Abstract
Chronic inflammation has been identified in leukemias as an essential regulator of angiogenesis. B-chronic lymphocytic leukemia (CLL) cells secrete high levels of vascular endothelial growth factor (VEGF) and hypoxia inducible factor 1 alpha (HIF1α). The aim was to assess the role of inflammation in activation of angiogenic factors: endothelial nitric oxide synthase (eNOS), HIF1α and VEGF via proliferation related signaling pathways and VEGF autocrine control. We isolated mononuclear cells (MNC) and CD19+ cells from peripheral blood of 60 patients with CLL. MNC were treated with pro-inflammatory interleukin-6 (IL-6) and VEGF, in combination with inhibitors of JAK1/2 (Ruxolitinib), mTOR (Rapamycin), NF-κB (JSH23), SMAD (LDN-193189) and PI3K/AKT (Ly294002) signaling pathways, to evaluate eNOS, VEGF and HIF1α expression by immunoblotting, immunocytochemistry and RT-qPCR. Also, we investigated IL-6 dependent neovascularization in human microvascular endothelial cells (HMEC-1) in co-culture with MNC of CLL. The angiogenic factors eNOS, VEGF and HIF1α had significantly higher frequencies in MNC of CLL in comparison to healthy controls (p < 0.001) and CD19+ cells of CLL. IL-6 increased the quantity of HIF1α (p < 0.05) and VEGF positive cells in the presence of JSH23 (p < 0.01). VEGF increased HIF1α (p < 0.05), and decreased eNOS gene expression (p < 0.01) in MNC of CLL. VEGF significantly (p < 0.001) increased the number of HIF1α positive MNC of CLL, prevented by inhibitors of JAK1/2, PI3K and mTOR signaling pathways. VEGF stimulation of SMAD (p < 0.05) and STAT5 (p < 0.01) signaling has been prevented by inhibitors of JAK1/2, mTOR, PI3K and SMAD signaling, individually (p < 0.01) or mutually (p < 0.001). Also, we showed that MNC of CLL and IL-6 individually stimulate neovascularization in co-culture with HMEC-1, without a cumulative effect. We demonstrated elevated angiogenic factors in CLL, while VEGF and IL-6 independently stimulated HIF1α. VEGF stimulation of HIF1α was mostly mTOR dependent, while IL-6 stimulation was NF-κB dependent.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic lymphocytic leukemia (CLL) is a common and incurable hematological malignancy characterized by the clonal growth of malignant CD5+ B-lymphocytes with delayed apoptosis that accumulate in peripheral blood, bone marrow and lymph node [1, 2]. In severe inflammation process higher vascular permeability permits inflammatory mediators and immune response cells to intrude the site of damage, where vascular endothelial growth factor (VEGF) plays a dynamic role as a multifunctional molecule [3].
Our previous study has shown that the proinflammatory marker IL-6 stimulates the expression of S100A4 and S100A8 proteins in CLL, mediated by JAK1/2- and NF-κB signaling. These findings support the inflammation’s role in the overexpression of antiapoptotic protein BCL-2 and CLL progression [4]. It is widely accepted that angiogenesis contributes to the development and progression of CLL [5], but the molecular mechanism of angiogenic growth factors in the CLL is unclear. The three most widely studied angiogenic factors in the CLL are VEGF, hypoxia inducible factor 1 alpha (HIF1α) and endothelial nitric oxide synthase (eNOS) as potential targets to achieve tumor remission [6]. Several types of leukemic cells, including mononuclear cells (MNC) of CLL, produce and secrete VEGF which may control the malignancy of those cells by paracrine and autocrine effects [7, 8]. Previous study reported that specific mutations in the tumor-suppressor gene TP53 are associated with higher HIF1α levels in CLL [9]. HIF1α plays a critical role in the oncogene-dependent expression and autocrine regulation of VEGF in patients with CLL [10]. Angiogenic factors can become the essential targets of anti-CLL therapy because they modulate the cellular composition of the cancer microenvironment [11]. The inhibition of synthesis and physiological function of VEGF and it signaling pathway is a potential target for antiangiogenic therapy in CLL patients [9, 12].
The main hypothesis of our study is that inflammation aggravates angiogenesis in CLL. In accordance, we observed the interplay between angiogenic factors in MNC of CLL mediated by inflammation, proliferation and apoptosis related signaling pathways. We evaluated the regulation of angiogenic factors HIF1α, VEGF and eNOS by IL-6, as well as HIF1α and eNOS by VEGF, mediated by JAK1/2, PI3K /mTOR, SMAD, STAT5 and NF-κB signaling pathways in patients with CLL parallel with the observation of SMAD and STAT5 phosphorylation. The results of this study should reveal the interaction between inflammation and angiogenesis through proliferation-related signaling pathways in CLL.
Material and methods
CLL patients and treatment of MNC
Ten healthy individuals and 60 patients with CLL diagnosed according to the World Health Organization (WHO) classification provided peripheral blood samples. Patients and healthy controls provided their consent by signing the form approved by a local ethical commission following the guidelines of the Declaration of Helsinki. 30 ml of peripheral blood samples were collected in disodium EDTA and MNC were isolated using a lymphocyte separation medium (LSM, Capricorn Scientific GmbH, Ebsdorfergrund, Germany). The isolated MNC were washed in PBS and resuspended in RPMI-1640 medium (Biowest, Nuaillé, France). The MNC were preincubated for 1 h with 0.6 μM ruxolitinib (RUXO, JAK1/2 inhibitor, Cayman Chemical Company, Ann Arbor, MI, USA), 5 μM Ly294002 (PI3K inhibitor, Cell Signalling Technology, Inc, Danvers, MA, USA), 1.5 μM JSH23 (NF-κB inhibitor, Sigma-Aldrich, Darmstadt, Germany), 100 ng/mL Rapamycin (RAPA, mammalian target of rapamycin (mTOR) inhibitor, Calbiochem, EMD Millipore Corp., Billerica, MA, USA), or 10 ng/mL Low Dose Naltrexone (LDN-193189 Merck KGaA, Darmstadt, Germany), and treated 1 h with IL-6 (20 µg/ml Miltenyi Biotec, Bergisch Gladbach, Germany) or VEGF (10 µg/mL Elabscience, Wuhan, China) [13]. After these treatments, the MNC was washed in PBS, incubated in RIPA lysis buffer at 4 ºC for 60 min, and centrifuged at 12,000 × g at 4 ºC for 15 min.
Isolation of CD19+ cells
CD19 is a B cell–specific antigen expressed on CLL cells, while CD19 + B cells make up on average about 10% of the peripheral blood MNC population. CD19 + [14]. Using MACS cell separation and CD19+ Microbeads, B-lymphocyte antigen CD19+ cells were purified from MNC of CLL patients in accordance with Miltenyi Biotec's manufacturer's procedure. Following the manufacturer's instructions, a magnetic separation column (Super Macs II, Miltenyi Biotec) and a combination of magnetic microbeads conjugated with antibody against CD19 (Miltenyi Biotec) were used to separate the CD19+ cells from the collected MNC. We centrifuged cell suspension at 300 × g for 10 min and after that aspirated supernatant completely. The cell pellet was resuspended in 80 μL of buffer per 107 total cells. 20 μL of CD19 MicroBeads, human per 107 total cells were added, mixed well, and incubated for 15 min in the refrigerator (+ 2 to + 8 °C). Cells were washed by adding 1–2 mL of buffer per 107 cells and centrifuged at 300 × g for 10 min. The supernatant was aspirated completely. The cells were then resuspended up to 108 cells in 500 μL of buffer. Using the trypan-blue exclusion method, viable CD19+ cells were counted (Life Technologies, Bleiswijk, Netherlands).
Cell culture of HMEC-1
The HMEC-1 cells (ATCC, USA) were cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS, Biowest) and 1% penicillin–streptomycin (Biowest) at 37 °C in a 5% CO2 humidified environment. HMEC-1 cells were passaged using trypsinization when reaching 70–80% confluency. HMEC-1 cells were treated with IL-6 (20 µg/ml Miltenyi Biotec) and seeded on the Matrigel surface at a final density of 1,2 × 104 per well for 18 h in a 37 °C incubator containing 5% CO2.
Western blotting
Proteins from CLL‐derived MNC were isolated and processed as previously reported [15]. Isolated MNC were exposed to chilled radioimmunoprecipitation assay (RIPA) lysis buffer (50 mM Tris HCl pH 7.6, 150 mM sodium chloride, 1% Triton x-100, 1% sodium deoxycholate, 0.1% sodium dodecyl sulphate, 2 mM EDTA and 50 mM sodium fluoride) at a ratio of 1 ml of buffer on 1 × 108 cells. A protease inhibitor cocktail (Pierce, Thermo Fisher Scientific, Waltham, MA, USA) and sodium orthovanadate were added to the lysis buffer just prior to use. Lysates were incubated at 48 ºC for 25 min and then centrifuged at 10.000 g, 4 ºC, for 15 min. Protein concentration was determined by the bicinchoninic acid (BCA) Protein Assay Kit (Pierce, Thermo Fisher Scientific) and samples were stored at -70 °C. To examine activated HIF1α protein, we conducted separation of the nuclear and cytoplasmic fractions of granulocytes using NE-PER Kit (Pierce, Thermo Fisher Scientific). Equal amounts of protein (20 μg) were run on polyacrylamide gels and transferred to polyvinylidene difluoride membranes. The membranes were blocked with 4% milk (Serva Electrophoresis GmbH, Heidelberg, Germany) for 1 h at room temperature and probed with primary antibodies directed against HIF1α (Elabscience), VEGF (Elabscience), eNOS (Elabscience), phospho-STAT5 (R&D Systems, Inc, Minneapolis, MN, USA), STAT5 (R&D Systems), phospho-SMAD (R&D Systems) and β‐actin (R&D Systems). Peroxidase‐conjugated goat anti‐rabbit immunoglobulin (R&D Systems) was used as a secondary antibody, except goat anti‐mouse immunoglobulin (R&D Systems) for β‐actin. The HIF1 α, VEGF, eNOS, pSTAT5, STAT5, SMAD and β‐actin protein levels were imaged with ChemiDoc Imaging System (Bio‐Rad Laboratories, Hercules, CA, USA) and estimated by densitometric scanning of the blots using the Image Lab (Bio‐Rad Laboratories, Inc. Version 6.0.0.25) software tool and normalized to β‐actin.
Immunocytochemistry
For cytoplasm staining, we isolated circulating MNC and CD19+ cells from 10 healthy donors and 35 CLL patients. The MNC and CD19+ were collected onto microscope glass slides by cytospins (2 × 104 cells/each) and fixed by methanol at room temperature. Samples were treated with 3% H2O2 solution in distilled water to block endogenous peroxidase activity. Then, samples were immunostained with VEGF, HIF1α and eNOS (Elabscience) antibodies in a humidity chamber overnight at + 4 °C. Immunostaining was performed using the streptavidin‐biotin technique (LSAB+/HRP Kit, DAKO, Glostrup, Denmark). Immunoreactivity was visualized with DAKO Liquid DAB+ Substrate/Chromogen System counterstained with Mayer's hematoxylin (Merck, Whitehouse Station, NY, USA). For the negative control samples, normal serum, and PBS buffer (1:500) were pipetted without primary antibodies. Positive cells were analyzed and scored at five powered fields in each sample using a computer‐supported imaging system (Analysis Pro 3.1) connected to the light microscope (Olympus AX70, Hamburg, Germany) with an objective magnification of × 40.
Isolation of Total RNA and RT-qPCR
Total RNA from MNC of 40 CLL patients was isolated using TRIzol (Life Technologies, Thermo Fisher Scientific Inc). The concentration and integrity of total RNA were assessed using Ultrospec 3300 spectrophotometer (Amersham Pharmacia, Upsala, Sweden). Identical amounts of RNA from investigated samples were transcribed into cDNA using the Maxima First Strand cDNA Synthesis kit (Thermo Fisher Scientific Inc). Quantitative real-time PCR analyses of the human HIF1α gene and eNOS gene was performed on a Mastercycler EP RealPlex (Eppendorf AG, Hamburg, Germany) using the Maxima SYBR Green/ROX qPCR master mix (Thermo Fisher Scientific Inc) and adequate primers (Table 1). As internal control for normalization of the examined angiogenic factors was used β-actin.
In Vitro neovascularization and Tube Formation
In vitro neovascularization and Tube formation assay was performed using an angiogenesis assay kit (Angiogenesis Assay Kit, In Vitro, (ab204726)) (Abcam, Cambridge, UK). To investigate endothelial tube formation we co-cultured human microvascular endothelial cells (HMEC-1) cells and MNC from CLL patients in DMEM medium for 24 h. Briefly, 50 µL of liquid Matrigel (Merck, Darmstadt, Germany) was placed in 96 well plate and incubated at 37 °C for 30 min. HMEC-1 cells were treated with IL-6 (20 µg/ml Miltenyi Biotec) and seeded on the Matrigel surface at a final density of 1,2 × 104 per well for 18 h in a 37 °C incubator containing 5% CO2. Captured images were analyzed for mean mesh size, number of meshes, number of nodes, number of junctions, number of segments, number of master junctions and number of master segments using the image J-based Angiogenesis Analyzer tool.
Statistical analysis
Descriptive statistics were obtained from the outcome measures and expressed as means with standard deviations or as numbers and percentages, as appropriate. Differences between groups were analyzed using Student’s t-test. The results are expressed as means ± SEM. The one-way ANOVA and Dunnett’s posttest were applied using Prism 6 software (GraphPad Software Inc., San Diego, CA, USA). P < 0.05 was considered statistically significant.
Results
Proinflammatory effect of IL-6 on angiogenic factors in CLL
Our results confirmed that the number of VEGF, HIF1α and eNOS positive cells were significantly higher in MNC of CLL compared to healthy controls (Fig. 1A). The number of VEGF, eNOS and HIF1α positive cells were significantly lower in CD19+ cells than in MNC of CLL (Fig. 1A). Therefore, these angiogenic factors are produced at higher levels by non-B cell types of peripheral blood MNC, such as T cells, monocytes, or NK cells. In order to investigate the inflammatory effect on angiogenic factors in CLL, we treated isolated MNC with IL-6 and followed the level of angiogenic factors VEGF, HIF1α, and eNOS. Pro-inflammatory IL-6 did not significantly increase the expression of angiogenic factors in MNC of patients with CLL (Fig. 1B, C), except for the HIF1α expression (Fig. 1D. p < 0.05). In opposite with NF-κB inhibitor, IL-6 decreased the level of VEGF frequency in combination with JAK1/2 inhibitors compared to MNC cells treated with the IL-6 only (Fig. 1B, p < 0.05). Mutually with IL-6, NF-κB and JAK1/2 inhibition significantly reduced the eNOS expression (Fig. 1C, p < 0.05). The inhibitor of JAK1/2 signaling pathway significantly downregulated HIF1α expression that was prevented by IL-6 (Fig. 1D). In addition, IL-6 upregulation of HIF1α was NF-κB- and PI3K-mediated (Fig. 1D).
IL-6 induction of angiogenic factors in mononuclear cells (MNC) and CD19+ cells of peripheral blood of chronic lymphocytic leukemia (CLL). A) Percentage of VEGF, eNOS, and HIF1α in positive MNC and CD19 + cells of CLL and healthy controls (HC) determined by immunocytochemistry (n = 5–7). The MNC were treated 1 h by 20 µg/ml IL-6 with or without preincubation of 1 h with 0.6 nM JAK1/2 inhibitor Ruxolitinib (RUXO), 5 nM PI3K inhibitor LY294002 (LY) or 0.75 nM NF-κB inhibitor JSH23 and levels of B) VEGF, C) eNOS and D) HIF1α were determined. Immunocytochemistry images correspond to the Supplemental Fig. 1. Values mean ± SEM (n = 4). ***p < 0.001 vs. MNC from CLL (A); *p < 0.05, vs. IL-6 only treated MNC; #p < 0.05 vs. healthy control C (B-D)
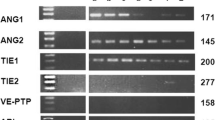
VEGF effect on angiogenic factors gene expression
After common treatment with VEGF and inhibitors of inflammation-related signaling pathways, the gene expression of HIF1α and eNOS was monitored in MNC of CLL patients (Fig. 2). VEGF stimulated HIF1α gene expression (p < 0.05), while inhibitor of mTOR signaling pathway decreased gene expression (p < 0.01) (Fig. 3A). VEGF significantly increased the gene expression of angiogenic factors HIF1α (p < 0.05, Fig. 2B) in contrast to eNOS (p < 0.01) which was decreased in the MNC of CLL patients (Fig. 2C). In addition, PI3K, JAK1/2 and mTOR inhibitors also significantly decreased VEGF-stimulated HIF1α (p < 0.05) and individually eNOS gene expression (p < 0.05, Fig. 2B, C). Moreover, the IL-6 prevented VEGF simulation of HIF1α (p < 0.05, Fig. 2A) and reduced eNOS gene expression (p < 0.01, Fig. 2C). VEGF transcriptional activation of the angiogenic factors had opposite trend for eNOS and HIF1α gene expression controlled by PI3K, JAK1/2 and mTOR signaling.
Vascular endothelial growth factor (VEGF) induction of angiogenic gene expression in mononuclear cells (MNC) of peripheral blood of chronic lymphocytic leukemia (CLL). Densitometry revealed gene expression determined by RT-PCR and presented as a ratio of angiogenic factors to β-actin levels. The MNC were treated 1 h by 10 µg/ml VEGF with or without preincubation of 1 h with 1 µM JAK1/2 inhibitor Ruxolitinib (RUXO), 5 µg/ml PI3K inhibitor LY294002 (LY) and 100 ng/ml mTOR inhibitor Rapamycin (RAPA, individually or combination of inhibitors) and levels of A) HIF1α and B) HIF1α (all samples treated with VEGF); and C) eNOS were determined. Values mean ± SEM (n = 6). #p < 0.05, ##p < 0.01 versus VEGF treated only (A, B), *p < 0.05, **p < 0.01 vs. Control MNC (C)
Vascular endothelial growth factor (VEGF) induction of angiogenic protein expression in mononuclear cells (MNC) of peripheral blood of chronic lymphocytic leukemia (CLL). Densitometry revealed protein expression determined by Western blotting and presented as a ratio of angiogenic factors to β-actin protein levels. The MNC were treated 1 h by 10 µg/ml VEGF with or without preincubation of 1 h with 1 µM JAK1/2 inhibitor Ruxolitinib (RUXO), 5 µg/ml PI3K inhibitor LY294002 (LY) and 100 ng/ml mTOR inhibitor Rapamycin (RAPA) levels of A) HIF1α, and B) eNOS were determined. Columns correspond to immunoblot images. Values mean ± SEM (n = 5). #p < 0.05, ##p < 0.01 vs. VEGF treated only (first column)
VEGF effect on angiogenic factors protein expression
As part of our study, we also investigated the changes in eNOS and HIF1α protein expression after the treatment of MNC of CLL with VEGF and inhibitors of JAK1/2, mTOR and PI3K signaling pathway. VEGF treatment of MNC of CLL significantly stimulated expression of HIF1α and eNOS protein expression (Fig. 3). JAK1/2, mTOR and PI3K inhibition decreased the VEGF stimulated HIF1α and eNOS protein expression (p < 0.05, Fig. 3A, B). The most significant decreased of HIF1α (p < 0.05) and eNOS (p < 0.01) protein expression was detected after combination of PI3K and mTOR inhibitors (Fig. 3A, B). Combination of two inhibitors for PI3K, mTOR and JAK1/2 additionally inhibited HIF1α and eNOS protein expression in MNC of CLL (Fig. 3A, B).
VEGF effect on angiogenic factors immunoreactivity in bone marrow
Since we already shown that the gene and protein levels of angiogenic factors are changed under the influence of VEGF we also wanted to examine the total degree of its expression in the MNC of CLL patients. Immunocytochemical analysis showed that VEGF significantly increased the number of HIF1α (p < 0.001, Fig. 4A, B) positive cells. PI3K inhibitor significantly inhibited VEGF increased number of HIF1α as well as eNOS positive cells (p < 0.001, Fig. 4A, C). Our results also showed that HIF1α and eNOS have opposite patterns of expression after inhibition of PI3K signaling pathway in comparison to non-treated MNC (Fig. 4A, C). Namely, HIF1α number of positive cells was increased (p < 0.001, Fig. 4A), while number of eNOS positive cells was decreased (p < 0.001, Fig. 4C) after those treatments in comparison to non-treated MNC of CLL. The same trend of changes in the number of HIF1α and eNOS positive cells was observed after the treatment of VEGF and its combination with inhibitors of JAK1/2 and mTOR signaling pathways (Fig. 4B, D). In both cases the number of positive cells was significantly decreased after those treatments in comparison to non-treated MNC or only VEGF treated MNC of CLL.
Vascular endothelial growth factor (VEGF) induction of angiogenic protein positive mononuclear cells (MNC) of peripheral blood of chronic lymphocytic leukemia (CLL). The MNC were treated 1 h by 10 µg/ml VEGF with or without preincubation of 1 h with 1 µM JAK1/2 inhibitor Ruxolitinib (RUXO), 5 µg/ml PI3K inhibitor LY294002 (LY) and 100 ng/ml mTOR inhibitor Rapamycin (RAPA, individually or combination of inhibitors) and levels of A, B) HIF1α, and C, D) eNOS were determined by immunocytochemistry. Immunocytochemistry images correspond to the Supplemental Fig. 2. Values mean ± SEM (n = 5). *p < 0.05, **p < 0.01, ***p < 0.001 vs. non-treated MNC (first column); ###p < 0.001 vs. VEGF treated only (second column)
VEGF activation of inflammation and proliferation signaling in MNC of CLL
VEGF caused phosphorylation and activation of pSTAT5 and pSMAD signaling pathways in MNC of CLL (Fig. 5). Phosphorylation and activation of the pSTAT5 signaling pathway were markedly reduced when treating MNC of CLL with VEGF and a combination of JAK1/2, PI3K, and mTOR inhibitors (p < 0.01) (Fig. 5A). Inhibitors for SMAD (p < 0.05), JAK1/2 (p < 0.01), and mTOR (p < 0.01) signaling pathways significantly blocked the VEGF-induced phosphorylation and activation of pSMAD in the study. When inhibitors were used in pairs, the inhibition of pSTAT5 and pSMAD signaling pathways was significantly more pronounced (p < 0.001) (Fig. 5).
Vascular endothelial growth factor (VEGF) activation of inflammation and proliferation signaling in mononuclear cells (MNC) of peripheral blood of chronic lymphocytic leukemia (CLL). Densitometry revealed protein expression determined by Western blotting and presented as a ratio of phosphorylated to total protein levels. The MNC were treated 1 h by 10 µg/ml VEGF with or without preincubation of 1 h with 1 µM JAK1/2 inhibitor Ruxolitinib (RUXO), 5 µg/ml PI3K inhibitor LY294002 (LY), 10 ng/mL LDN and 100 ng/ml mTOR inhibitor Rapamycin (RAPA, individually or combination of inhibitors) and activation of A) STAT5 and B) SMAD signaling was determined. Columns correspond to immunoblot images. Values mean ± SEM (n = 3–5). *p < 0.05, **p < 0.01, ***p < 0.001 vs. VEGF treated only (second column)
IL-6 induction of neovascularization in vitro
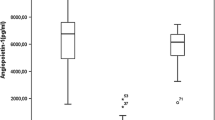
Our results showed that IL-6 induction of neovascularization of HMEC-1 in co-culture with MNC of peripheral blood of CLL (Fig. 6). The mean number of meshes (Fig. 6A), nodes (Fig. 6B), junctions (Fig. 6C), total length (Fig. 6D), master junctions (Fig. 6E), and master segments (Fig. 6F) was significantly higher in co-culture of HMEC-1 with MNC of peripheral blood of CLL. Proinflammatory marker IL-6 also stimulated neovascularization and significantly increased the number of nodes, junctions, and total length of blood vessels (Fig. 6B-D). IL-6 in combination with MNC of peripheral blood of CLL significantly increased the number of junctions, master junctions and master segments (Fig. 6C, E, F). Detection of constitutive elements of the network during neovascularization of human microvascular endothelial cells show extremities (arrowhead A), nodes, identified as pixels that had at least 3 branches, corresponding to a bifurcation (arrow B); twig (C1, D1), segment (C2, D2) delimited by two junctions (C3, D3) (note that this pointed junction is composed by several nodes) and branch (C4, D4) (Suppl. Figure 1). After incubation with IL-6, the number of junctions and total vessel length increased significantly compared to non-treated HMEC-1 (Suppl. Figure 2). IL-6 significantly increased the number of junctions and the total vessel length compared to non-treated HMEC-1 cells (Suppl. Figure 2).
IL-6 induction of neovascularization of human microvascular endothelial cells (HMEC-1) in co-culture with mononuclear cells (MNC) of peripheral blood of chronic lymphocytic leukemia (CLL). The quantity of A) meshes, B) nodes, C) junctions, D) total length, E) master junctions, and F) master segments during IL-6 induced neovascularization of HMEC-1 in the presence of peripheral blood derived MNC of patients with CLL. Values mean ± SEM (n = 4–8). *p < 0.05, **p < 0.01 vs. HMEC-1 only (first column). Description of the elements in neovascularization is presented in Supplemental Figs. 3 and 4
Discussion
According to the presented results, angiogenic factors VEGF, eNOS and HIF1α were increased in the CLL derived MNC. VEGF significantly increased gene expression and quantity of HIF1α positive cells in the CLL derived MNC, as well as the activation of STAT5 and SMAD signaling pathways. Inhibitors of PI3K, JAK1/2, and mTOR signaling pathways significantly prevented VEGF induced gene and protein expression of HIF1α, indicating their potential therapeutic effects. Moreover, inhibitors of PI3K and NF-κB, signaling pathways significantly blocked IL-6 induced quantity of HIF1α positive MNC. Inhibition of inflammatory JAK1/2 signaling decreased quantity of VEGF and HIF1α positive MNC, while inhibition of PI3K and NF-κB signaling decreased quantity of eNOS positive MNC. VEGF and IL-6 decreased eNOS gene expression. Furthermore, we showed that IL-6 and MNC of CLL individually, but not cumulatively, stimulated neovascularization of HMEC-1, indicating already increased IL-6 or inflammation factors in MNC of patients with CLL. It has been shown that plasma of CLL patients had increased levels of IL-6 that might be a therapeutic target [16].
CLL cells enhanced production of VEGF protein in hypoxia, while angiogenesis was stimulated by CLL cells [17]. It has been reported greater angiogenesis in CLL, with augmented MVD and increased VEGF and HIF1α, in addition to presence of VEGF receptors on CLL cells. [18]. CLL can be affected by angiogenesis due to the strong interaction of cytokines with the bone marrow microenvironment in bone marrow where VEGF exposed endothelial cells increased translation of various hematopoietic growth factors, such as IL-6, with an autocrine stimulation of the proliferation and migration of endothelial cells [19]. Bevacizumab, as a monoclonal antibody for VEGF, in addition to chemoimmunotherapy of CLL, is generally well-tolerated and appears to prolong progression-free survival and treatment-free survival [20].
As a key determinant of disease outcome, the proliferative drive of CLL cells was linked to the activation of mTOR-MYC-oxidative phosphorylation [21]. A rapamycin analog showed a weak effect in the clinical trial of patients with relapsed CLL [22]. The simultaneous inhibition of all PI3K isoforms combined with the inhibition of mTOR destroyed CLL cells more potently and overcame the positive feedback look via mTOR complex 2 (mTORC2) [23]. Results of our study showed that mTOR and PI3K are involved in VEGF mediated stimulated expression of HIF1α gene and protein expression in MNC of CLL patients. Hypoxia acts through the activation of the PI3K/AKT pathway, whereas the HIF1α inhibitor BAY87-2243 exerts cytotoxic effects toward leukemic cells and has anti-tumor activity in mouse model of aggressive B-cell lymphoma [9].
In our study IL-6 induced significantly higher level of expression only for HIF1α in MNC of CLL, while the number of positive cells for all three angiogenic markers was significantly lower in CD19+ cells. Treatment with proinflammatory IL-6, in combination with inhibitor of NFκB signaling pathway induced higher number of VEGF positive cells, while the number of eNOS and HIF1α positive cells were significantly lower in comparison to IL-6 only treated MNC of CLL. Wnt5a/ROR1-dependent signaling contributed to CLL cell activation of NF-κB and increased expression of IL-6, while cirmtuzumab (humanized monoclonal antibody that targets ROR1) could inhibit leukemia cell activation of NF-κB in patients with CLL [24].
CLL derived MNC synthetized strong angiogenic factors such as VEGF which have an anti-apoptotic effect on the CLL cells [25]. The presented results also showed that VEGF and IL-6 significantly stimulated expression of HIF1α positive cells, prevented by inhibitors of PI3K, NFkB and mTOR signaling pathways. PI3K/AKT is the most important signaling pathway in the control of angiogenesis mediated by VEGF in many tumors including CLL [26]. PI3K/AKT pathway stimulated tumor expansion by expression of angiogenic factors and the inhibition of antiangiogenic factors [27]. PI3K/AKT also controlled angiogenesis by numerous downstream signaling pathways, such as mTOR, where they usually upregulated HIF1α expression which provoked VEGF expression [28].
In patients with CLL serum IL-6 and IL-10 levels were higher than in healthy controls and correlated with adverse disease features and short survival [29]. IL‐6 activated STAT3 and NF‐κB signaling pathway in CLL cells, while an amplified autocrine IL‐6 synthesis by CLL cells was linked to poorer quality of clinical outcome [6]. In accordance with our results, IL-6 activation of HIF1α was mediated by NF-κB signaling pathway, while inhibition of IL‐6 or its receptor could contribute to disabling the resistance of CLL cells to chemotherapy [6].
STAT5 and AKT were the main activators of oncogenesis in drug-resistant forms of chronic myeloid leukemia and systemic mastocytosis, and targeting STAT5 and AKT could be an interesting approach in therapy for these malignancies [30]. Our results also showed that VEGF significantly increased activation of STAT5 and SMAD signaling pathways, prevented by inhibition of PI3K, JAK1/2 and mTOR signaling pathways. STAT5 signaling pathway was inhibited in MNC of CLL patients, and that low level of the STAT5 was localized mainly in cytoplasm, indicating the absence of active transcriptional complexes in the nucleus of MNC [31]. It has been reported a significant correlation between expression of SMAD1/8 and SMAD4 proteins and poor prognosis of CLL patients [32]. In our study, phosphorylation of SMAD signaling was increased with VEGF treatment, but also inhibited with inhibitors for SMAD, JAK1/2 and mTOR signaling pathways, indicating potential association of several signaling pathways in the activation of the SMAD via VEGF.
Conclusions
In conclusion, we showed the increased angiogenic factors in complex interplay with proinflammatory markers and proliferation related signaling pathways in CLL. Results of the study showed that VEGF and IL-6 upregulated angiogenic HIF1α levels in MNC of CLL controlled mutually by PI3K signaling pathway as a potential therapeutic target. This study revealed that MNC of CLL already have inflammatory capacity for neovascularization, not further on supported by external IL-6. Our results suggest that combined inhibition of VEGF and IL-6 may have a potential benefit for patients with CLL as a new place for therapeutic approach.
Data availability
Data available on request by email to corresponding author.
References
Darwiche W, Gubler B, Marolleau JP (2018) Ghamlouch H (2018) Chronic Lymphocytic Leukemia B-Cell Normal Cellular Counterpart: Clues from a Functional Perspective. Front Immunol 9:683. https://doi.org/10.3389/fimmu.2018.00683
Strati P, Shanafelt TD (2015) Monoclonal B-cell lymphocytosis and early-stage chronic lymphocytic leukemia: diagnosis, natural history, and risk stratification. Blood 126(4):454–462. https://doi.org/10.1182/blood-2015-02-585059
Aguilar-Cazares D, Chavez-Dominguez R, Carlos-Reyes A, Lopez-Camarillo C, Hernadez de la Cruz ON, Lopez-Gonzalez JS (2019) Contribution of Angiogenesis to Inflammation and Cancer. Front Oncol 9:1399. https://doi.org/10.3389/fonc.2019.01399
MitrovićAjtić O, Subotički T, Diklić M, Đikić D, Vukotić M, Dragojević T, Živković E, Antić D, Čokić V (2022) Regulation of S100As Expression by Inflammatory Cytokines in Chronic Lymphocytic Leukemia. Int J Mol Sci 23(13):6952. https://doi.org/10.3390/ijms23136952
Han Y, Wang X, Wang B, Jiang G (2016) The progress of angiogenic factors in the development of leukemias. Intractable Rare Dis Res 5(1):6–16. https://doi.org/10.5582/irdr.2015.01048
Montemagno C, Pagès G (2020) Resistance to Anti-angiogenic Therapies: A Mechanism Depending on the Time of Exposure to the Drugs. Front Cell Dev Biol 8:584. https://doi.org/10.3389/fcell.2020.00584
Adams J, Carder PJ, Downey S, Forbes MA, MacLennan K, Allgar V, Kaufman S, Hallam S, Bicknell R, Walker JJ, Cairnduff F, Selby PJ, Perren TJ, Lansdown M, Banks RE (2000) Vascular endothelial growth factor (VEGF) in breast cancer: comparison of plasma, serum, and tissue VEGF and microvessel density and effects of tamoxifen. Cancer Res 60:2898–2905
Kay NE, Bone ND, Tschumper RC, Howell KH, Geyer SM, Dewald GW, Hanson CA, Jelinek DF (2002) B-CLL cells are capable of synthesis and secretion of both pro- and anti-angiogenic molecules. Leukemia 16:911–919. https://doi.org/10.1038/sj.leu.2402467
Griggio V, Vitale C, Todaro M, Riganti C, Kopecka J, Salvetti C, Bomben R, Bo MD, Magliulo D, Rossi D, Pozzato G, Bonello L, Marchetti M, Omedè P, Kodipad AA, Laurenti L, Del Poeta G, Mauro FR, Bernardi R, Zenz T, Gattei V, Gaidano G, Foà R, Massaia M, Boccadoro M, Coscia M (2020) HIF-1α is over-expressed in leukemic cells from TP53-disrupted patients and is a promising therapeutic target in chronic lymphocytic leukemia. Haematologica 105(4):1042–1054. https://doi.org/10.3324/haematol.2019.217430
Ghosh AK, Shanafelt TD, Cimmino A, Taccioli C, Volinia S, Liu CG, Calin GA, Croce CM, Chan DA, Giaccia AJ, Secreto C, Wellik LE, Lee YK, Mukhopadhyay D, Kay NE (2009) Aberrant regulation of pVHL levels by microRNA promotes the HIF/VEGF axis in CLL B cells. Blood 113(22):5568–5574. https://doi.org/10.1182/blood-2008-10-185686
Lopes-Coelho F, Martins F, Pereira SA, Serpa J (2021) Anti-Angiogenic Therapy: Current Challenges and Future Perspectives. Int J Mol Sci 22(7):3765. https://doi.org/10.3390/ijms22073765
Rafii S, Lyden D, Benezra R, Hattori K, Heissig B (2002) Vascular and haematopoietic stem cells: novel targets for anti-angiogenesis therapy? Nat Rev Cancer 2:826–835. https://doi.org/10.1038/nrc925
Subotički T, MitrovićAjtić O, Živković E, Diklić M, Đikić D, Tošić M, Beleslin-Čokić B, Dragojević T, Gotić M, Santibanez JF, Čokić V (2021) VEGF Regulation of Angiogenic Factors via Inflammatory Signaling in Myeloproliferative Neoplasms. Int J Mol Sci 22(13):6671. https://doi.org/10.3390/ijms22136671
Darwiche W, Gubler B, Marolleau JP, Ghamlouch H (2018) Chronic Lymphocytic Leukemia B-Cell Normal Cellular Counterpart: Clues From a Functional Perspective. Front Immunol 9:683. https://doi.org/10.3389/fimmu.2018.00683
Hoermann G, Greiner G, Valent P (2015) Cytokine Regulation of Microenvironmental Cells in Myeloproliferative Neoplasms. Mediat Inflamm 2015:869242. https://doi.org/10.1155/2015/869242
Zhu F, McCaw L, Spaner DE, Gorczynski RM (2018) Targeting the IL-17/IL-6 axis can alter growth of Chronic Lymphocytic Leukemia in vivo/in vitro. Leuk Res 66:28–38. https://doi.org/10.1016/j.leukres.2018.01.006
Maffei R, Martinelli S, Castelli I, Santachiara R, Zucchini P, Fontana M, Fiorcari S, Bonacorsi G, Ilariucci F, Torelli G, Marasca R (2010) Increased angiogenesis induced by chronic lymphocytic leukemia B cells is mediated by leukemia derived Ang2 and VEGF. Leuk Res 34(3):312–321. https://doi.org/10.1016/j.leukres.2009.06.023
Frater JL, Kay NE, Goolsby CL, Crawford SE, Dewald GW, Peterson LC (2008) Dysregulated angiogenesis in B-chronic lymphocytic leukemia: morphologic, immunohistochemical, and flow cytometric evidence. Diagn Pathol 3:16. https://doi.org/10.1186/1746-1596-3-16
Ribatti D, Vacca A, De Falco G, Ria R, Roncali L, Damacco F (2001) Role of hematopoietic growth factors in angiogenesis. Acta Haematol 106:157–161. https://doi.org/10.1159/000046611
Kay NE, Strati P, LaPlant BR, Leis JF, Nikcevich D, Call TG, Pettinger AM, Lesnick CE, Hanson CA, Shanafelt TD (2016) A randomized phase II trial comparing chemoimmunotherapy with or without bevacizumab in previously untreated patients with chronic lymphocytic leukemia. Oncotarget 7(48):78269–78280. https://doi.org/10.18632/oncotarget.13412
Lu J, Cannizzaro E, Meier-Abt F, Scheinost S, Bruch PM, Giles HA, Lütge A, Hüllein J, Wagner L, Giacopelli B, Nadeu F, Delgado J, Campo E, Mangolini M, Ringshausen I, Böttcher M, Mougiakakos D, Jacobs A, Bodenmiller B, Dietrich S, Oakes CC, Zenz T, Huber W (2021) Multi-omics reveals clinically relevant proliferative drive associated with mTOR-MYC-OXPHOS activity in chronic lymphocytic leukemia. Nat Cancer 2(8):853–864. https://doi.org/10.1038/s43018-021-00216-6
Zent CS, LaPlant BR, Johnston PB, Call TG, Habermann TM, Micallef IN, Witzig TE (2010) The treatment of recurrent/refractory chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL) with everolimus results in clinical responses and mobilization of CLL cells into the circulation. Cancer 116:2201–2207. https://doi.org/10.1002/cncr.25005
Blunt MD, Carter MJ, Larrayoz M, Smith LD, Aguilar-Hernandez M, Cox KL, Tipton T, Reynolds M, Murphy S, Lemm E, Dias S, Duncombe A, Strefford JC, Johnson PW, Forconi F, Stevenson FK, Packham G, Cragg MS, Steele AJ (2015) The PI3K/mTOR inhibitor PF-04691502 induces apoptosis and inhibits microenvironmental signaling in CLL and the Eμ-TCL1 mouse model. Blood 25:4032–4041. https://doi.org/10.1182/blood-2014-11-610329
Chen Y, Chen L, Yu J, Ghia EM, Choi MY, Zhang L, Zhang S, Sanchez-Lopez E, Widhopf GF 2nd, Messer K, Rassenti LZ, Jamieson C, Kipps TJ (2019) Cirmtuzumab blocks Wnt5a/ROR1 stimulation of NF-κB to repress autocrine STAT3 activation in chronic lymphocytic leukemia. Blood 134(13):1084–1094. https://doi.org/10.1182/blood.2019001366
Farahani M, Treweeke AT, Toh CH, Till KJ, Harris RJ, Cawley JC, Zuzel M, Chen H (2005) Autocrine VEGF mediates the antiapoptotic effect of CD154 on CLL cells. Leukemia 19(4):524–530. https://doi.org/10.1038/sj.leu.2403631
Okumura N, Yoshida H, Kitagishi Y, Murakami M, Nishimura Y, Matsuda S (2012) PI3K/AKT/PTEN Signaling as a Molecular Target in Leukemia Angiogenesis. Adv Hematol 843085. https://doi.org/10.1155/2012/843085
Ellis L, Hammers H, Pili R (2009) Targeting tumor angiogenesis with histone deacetylase inhibitors. Cancer Lett 280(2):145–153. https://doi.org/10.1016/j.canlet.2008.11.012
Li Q, Michaud M, Canosa S, Kuo A, Madri JA (2011) GSK-3β: a signaling pathway node modulating neural stem cell and endothelial cell interactions. Angiogenesis 14(2):173–185. https://doi.org/10.1007/s10456-011-9201-9
Khodashenas M, Rajabian A, Attaranzadeh A, Lavi Arab F, Allahyari N (1992) Allahyari A (2022) Evaluation of cytokine levels as possible predicting elements in patients with chronic lymphocytic leukemia. Rev Assoc Med Bras 68(10):1364–1368. https://doi.org/10.1590/1806-9282.20220260
Bibi S, Arslanhan MD, Langenfeld F, Jeanningros S, Cerny-Reiterer S, Hadzijusufovic E, Tchertanov L, Moriggl R, Valent P, Arock M (2014) Co-operating STAT5 and AKT signaling pathways in chronic myeloid leukemia and mastocytosis: possible new targets of therapy. Haematologica 99(3):417–429. https://doi.org/10.3324/haematol.2013.098442
Matvieieva AS, Kovalevska LM, Ivanivska TS, Klein E, Kashuba EV (2019) The STAT5 transcription factor in B-cells of patients with chronic lymphocytic leukemia. Biopolym Cell 30–38. https://doi.org/10.7124/bc.000993
Witkowska M, Majchrzak A, Cebula-Obrzut B, Wawrzyniak E, Robak T, Smolewski P (2017) The distribution and potential prognostic value of SMAD protein expression in chronic lymphocytic leukemia. Tumour Biol 39(3):1010428317694551. https://doi.org/10.1177/1010428317694551
Funding
This research was supported by The Ministry of Science, Technological Development and Innovation of the Republic of Serbia grant number 451–03-66/2024–03/200015.
Author information
Authors and Affiliations
Contributions
Conceptualization, V.Č., D.A. and O.M.A.; methodology, T.S., O.M.A., M.D. and D.Đ.; formal analysis, T.S., O.M.A., E.Ž. and M.D.; investigation, T.S., O.M.A., M.V., T.D. and D.Đ.; data curation, O.M.A. and M.V., writing—original draft preparation, O.M.A., T.S., V.V., and V.Č.; writing—review & editing, O.M.A. and V.Č.; visualization, O.M.A. and E.Ž.; supervision, V.Č.; project administration, V.Č. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Institutional review board Statement
The study was approved by the Ethics Committee of the University Clinical Centre of Serbia, Belgrade (decision number 187/4) and the Ethics Committee of the Institute for Medical Research, Belgrade (decision number EO 117/2016).
Conflicts of Interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mitrović-Ajtić, O., Živković, E., Subotički, T. et al. Inflammation mediated angiogenesis in chronic lymphocytic leukemia. Ann Hematol 103, 2865–2875 (2024). https://doi.org/10.1007/s00277-024-05781-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-024-05781-1