Abstract
Molecular balance between Angiopoietin-1 (Ang-1) and Angiopoietin-2 (Ang-2) has important effects in tumor angiogenesis. Ang-2 was shown to be elevated and proved to be a prognostic factor in acute myeloid leukemia (AML). To date studies revealed increased angiogenesis in bone marrows (BMs) of both myeloproliferative neoplasm (MPN) and AML patients. We conducted this study to demonstrate circulating levels of Ang-1 and Ang-2 in MPN patients since no data exists in literature. Thirty-three newly diagnosed MPN, 27 newly diagnosed AML patients and 25 controls (HC) were enrolled and Angiopoietin levels were determined with ELISA. We found that Ang-1 levels were higher whereas Ang-2 levels were lower in MPN and HC when compared to AML. Our results suggest that though angiogenesis is increased in both AML and MPN, angiopoietin serum level profile of the two diseases are different, and MPN patients have similar Ang-1 and Ang-2 levels as HC. We conclude that, according to our results Ang-1 and Ang-2 do not only regulate tumor angiogenesis and the difference between angiopoietin levels of acute and chronic myeloid neoplasms could be a reflection of other effects of these growth factors on tumor malignancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
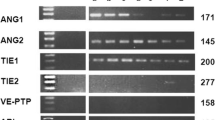
Malignant tumors are characterized by uncontrolled proliferation and metastasis to distant locations [1]. Angiogenesis has an important role in the growth, dissemination, and metastatic capacity of solid tumors [2]. However, it has also been shown that it may have a crucial pathophysiologic role in the development of hematologic malignancies [3]. Increased microvessel density (MVD) has been demonstrated in many hematologic disorders, such as acute and chronic leukemia, myelodysplastic syndrome, multiple myeloma and MPN [3–5]. Studies show that MVD is significantly increased in patients with newly diagnosed acute myeloid leukemia (AML) compared with control subjects, and returns to a normal level after complete remission (CR) is achieved [6, 7]. In literature, there are several studies demonstrating an increase in angiogenesis in myeloproliferative neoplasms (MPN) [3, 8, 9]. The article studying vascular density in BM samples of patients with MPN, revealed increased vascularity in polycythemia vera (PV), chronic myeloid leukemia (CML) and primary myelofibrosis (PMF) patients [4]. Alonci et al. demonstrated that serum VEGF levels were increased in MPN patients when compared to controls [8]. In the study conducted by Musolino et al. in which only CML and essential thrombocythemia (ET) patients were included, serum Angiogenin, another angiopoietic factor, was found to be increased in the patient group when compared to controls [10].
VEGF and the angiopoietins are among the most important growth factors in the tumor ecosystem. Angiopoietin-1 (Ang-1) and Angiopoietin-2 (Ang-2) and their Tie2 receptor tyrosine kinase have wide-ranging effects on tumor malignancy that includes angiogenesis, inflammation, and vascular extravasation. The regulatory role of Ang-1 and Ang-2 in tumor angiogenesis remains controversial due to the conflicting roles of both angiopoietins in angiogenesis [11]. Ang-1 activates Tie2 more strongly than does Ang-2; thus, some of the effects of Ang-2 could result from the inhibition of Ang-1 signaling [1, 12]. Ang-1–Tie2 signaling is thought to limit angiogenesis in mature vessels [1].
Ang-1, Ang-2 and Tie2 levels have been extensively studied in AML patients [12–15]. According to the results, Ang-2 was found to be elevated in AML patients as compared to controls and Ang-2 was proved to be an independent prognostic factor in AML [13]. To our knowledge, till now no data about circulating levels of Ang-1 and Ang-2 in MPN patients exists in literature. We decided to conduct this study in order to demonstrate serum levels of Ang-1 and Ang-2 in Ph(−) MPN patients and compare their serum level profiles both with AML patients and HC.
Materials and Methods
Thirty-three newly diagnosed Ph(−) MPN patients (13 ET, 16 PV, 4 PMF) and 27 newly diagnosed AML patients who admitted to Hematology Department from January 2011 to August 2012 were enrolled to this study. Twenty-five healthy individuals were included as the healthy control group. ET, PV and PMF patients were diagnosed according to 2008 World Health Organization (WHO) diagnostic criteria for MPNs [16]. AML patients were diagnosed according to 2008 WHO classification of acute leukemia [17]. Healthy controls were age and sex matched with the patient groups and they had no diagnosed disease which could interfere with the results of the study. Characteristics of MPN, AML patients and HC are shown in Table 1. Blood samples were collected from both the MPN and AML patients at the time of diagnosis before the initiation of therapy. Complete blood cell counts, biochemical test results of patients and HC were registered. Besides, splenomegaly (SM) and JAK2 V617F mutation status of MPN patients and cytogenetics of AML patients were also registered. However, in 40 % of in AML patients cytogenetic analysis results were undetermined due to a low number of metaphases (<20 metaphases). Characteristics of AML patients are shown in Table 2. After the samples were taken for the study, all of the AML patients received 3 + 7 remission induction therapy (Idarubicin 12 mg/m2, 3 days + Ara-C 100 mg/m2, 7 days). Patients who have normal complete blood counts and have a normocellular marrow and <5 % blasts in BM examination after the induction therapy were accepted as in CR. Patients who were in CR, received four courses of consolidation therapy with high-dose Ara-C (3 g/m2 every 12 h, 3 days). Patients who were refractory to therapy or relapsed received FLAG [Fluda-rabine (30 mg/m2, days 1–5), Ara-C (1 g/m2, over 3 h every 12 h, days 1–5) and G-CSF (5 μg/kg/day subcutaneously from day 0 until the white blood count was >20 × 109/l)] chemotherapy. Relapsed or refractory patients who were eligible for hematopoietic stem cell transplantation (HSCT) received HLA-identical, unrelated or haploidentical allogeneic transplantation. Samples collected from patients and HC were immediately centrifuged and the sera were stored at −80 °C. Serum Ang-1and Ang-2 levels were measured by commercial ELISA kits (ANG-2:R&D Systems, USA, ANG-1:RayBiotech Inc.,USA). The minimum detectable dose of Ang-1 was less than 30 pg/ml. While, intra-assay CV was <10 %, inter-assay CV was <12 % for Ang-1 ELISA kit. The minimum detectable dose of Ang-2 was 8.29 pg/mL. Intra-assay CV was 4.2–6.9 % and inter-assay CV was 7.4–10.4 % for Ang-2 ELISA kit. Only single measurement were performed for each sample. The study was approved by the Faculty Research Ethical Committee and informed consents from both the patients and healthy controls were taken.
SPSS 21.0 (IBM Statistics SPSS, USA) software was used for statistical analyses. Comparisons of non-parametric variables were performed with Kruskal–Wallis and Mann–Whitney U-tests. Correlation analyses were performed by using Spearman’s correlation. Survival curves were estimated using the Kaplan–Meier method, and the log-rank test was used to compare survival between groups. Overall survival (OS) was the primary outcome studied and was calculated from the date of first diagnosis to death from any cause. Univariate and multivariate Cox proportional hazards regression analyses were performed to evaluate the predictive effect of each factor. A p value of less than 0.05 was considered as a statistically significant result.
Results
Serum Ang-1 levels were significantly lower in AML patients [92.68 pg/ml (22.28–1946.5)] when compared to both MPN patients [6760.4 pg/ml (1593.6–9723.2)] and HC [6153.4 pg/ml (1699.5–7454)] (p < 0.0001). But there were no statistically significant difference between Ang-1 levels of MPN patients and HC (p = 0.15) (Fig. 1). On the other hand, serum Ang-2 levels were significantly increased in AML patients [3667.1 pg/ml (1167.6–1337.5)] when compared to both MPN patients [1263.5 pg/ml (749.2–1013.8)] and HC [1331.1 pg/ml (791.7–8227.7)] (p < 0.0001). Similar to Ang-1 levels, there were no statistically significant difference between Ang-2 levels of MPN patients and HC (p = 0.85) (Fig. 2).
In sub-group analysis, Ang-2 levels did not differ significantly between ET, PV, PMF patients and HC (p > 0.05). While, serum Ang-1 levels of PV patients were significantly higher in comparison to both PMF patients and HC, Ang-1 levels of PMF patients were significantly lower in comparison to HC (p = 0007, p = 0001, p = 0.05, respectively).
Ang-1 and Ang-2 levels didn’t differ significantly between JAK2 mutation positive and negative MPN patients (p = 0 27, p = 0.86, p = 0.79, respectively). Likewise, Ang-1 and Ang-2 levels were not significantly different between MPN patients with SM and without SM.
There were no statistically significant difference between Ang-1and Ang-2 levels of female and male subjects in any groups (p > 0.05). No correlation could be found between age and levels of Ang-1, Ang-2 in MPN, AML or HC (p > 0.05). Likewise, no correlation could be found between LDH, leukocyte count, thrombocyte count and levels of Ang-1, Ang-2 in MPN, AML patients or HC (p > 0.05).
When Ang-1and Ang-2 levels of AML patients who are in CR after induction therapy (13 patients) and who are refractory to induction therapy analysed, baseline Ang-2 levels were found to be significantly higher in non-responders (p = 0.03). However, there were no significant difference in responder and non-responder patients in terms of baseline Ang-1 levels (p > 0.05). In survival analysis, AML patients were divided into a low group (expression of angiogenic factor below the median) and a high group (above the median). Univariate analysis of factors associated with OS showed a significantly shorter survival in the patients with higher Ang-2 level (p = 0.020; Fig. 3). However, Ang-1 levels didn’t have any impact on survival (p = 0.588).
Discussion
The role of angiogenesis in solid tumors is well-established and there is also growing evidence about the role of angiogenesis in hematological malignancies [3, 4, 15]. In literature, there are several studies demonstrating an increase in angiogenesis in MPN and AML [3, 6, 8]. In our study, we determined serum Ang-1 levels were significantly lower, whereas serum Ang-2 levels were significantly higher in AML patients when compared to both MPN patients and HC. However, no significant difference in terms of serum Ang-1 or Ang-2 levels between MPN patients and HC existed. In sub-group analysis, Ang-1 levels of PMF patients were significantly lower in comparison to HC, similar to AML patients. This could be the result of inadequate number of PMF patients in our study or could be due to the higher probability of leukemic transformation feature of PMF.
To our knowledge, no data exists so far on blood levels of serum Ang-1 in MPN patients. There is only an article in literature demonstrating differential levels of soluble Ang-2 and Tie2 in patients with hematological malignancies, in which 25 ET patients were also enrolled. In this study, Ang-2 levels of ET patients were not significantly different from controls, similar to our study [18]. Our results suggest that, though there were several studies in literature demonstrating increased angiogenesis in MPN patients, Ang-1 and Ang-2 levels were not different from healthy controls.
In our study, Ang-1 and Ang-2 levels didn’t differ significantly between JAK2V617F mutation positive and negative MPN patients. This finding was in accordance with the literature. A study revealed that there was no association between JAK2-V617F mutational status and MVD and VEGF-expression in BM of MPN patients [19].
In the AML group of our study, we determined Ang-2 levels of AML patients significantly higher compared to HC and MPN patients. Baseline Ang-2 levels were found to be significantly higher in non-responder patients to induction chemotherapy when compared to responders. Moreover, OS of the AML patients with higher Ang-2 levels were shorter. In literature, there are several studies demonstrating the prognostic role of Ang-2 in AML patients. In a study, the authors have investigated the expression of Ang-1, Ang-2, Tie2, VEGF-A, and VEGF-C genes in BM mononuclear cells in newly diagnosed de novo AML and normal marrow donors. This study revealed that high pre-treatment levels of Ang-2 in the BM indicate an unfavorable prognosis in AML and it is an independent prognostic factors for overall survival [15]. In another study, marrow levels of Ang-1, Ang-2, and Tie2 were determined using ELISA in AML patients before chemotherapy and controls, revealing higher levels of Ang-2, Tie2 and lower levels of Ang-1 in AML patients. Moreover, patients with lower Tie2 and Ang-2 levels had a survival advantage [12].
There were no studies in literature comparing serum angiopoietin level profiles of AML and MPN patients in literature. Our study revealed that, Ang-1 and Ang-2 levels differ significantly between AML and MPN patients when compared to healthy controls. Mazzieri et al. revealed that Ang-2-Tie2 axis mediates cell-to-cell interactions between Tie2-expressing macrophages and endothelial cells that are important for tumor angiogenesis [20]. Although, increase in angiogenesis is a well-known fact both in AML and MPN, the increased tumorigenic potential in AML can be an explanation for the difference between serum level profiles of the two diseases. Besides, Scholz et al. demonstrated that Ang-1 and Ang-2 have regulatory roles on inflammation and while, Ang-1 seems to have an anti-inflammatory role, Ang-2 exerts a proinflammatory effect [21, 22]. These data reveal that Ang-1 and Ang-2 not only regulate tumour angiogenesis and there can be other factors affecting serum levels of Ang-1 and Ang-2.
Conclusion
In conclusion, our study revealed that MPN disease patients’ serum Ang-1 and Ang-2 levels were similar to HC. Moreover, Ang-1 and Ang-2 levels of AML patients were significantly different from both MPN patients and HC. Former studies revealed that Ang-1 and Ang-2 can both act as angiogenic or anti-angiogenic. Our study revealed that that molecular balance between Ang-1 and Ang-2 is the same as in HC, just the opposite to AML. Similar to studies in literature our study revealed higher Ang-2 level had a negative impact on response to remission induction therapy in AML patients. According to our results Ang-1 and Ang-2 do not only regulate tumour angiogenesis and the difference between angiopoietin levels of acute and chronic myeloid neoplasms could be a reflection of other effects of these growth factors on tumor malignancy and should be investigated in further more comprehensive studies. Moreover, considering that the leukemic transformation of myeloproliferative disorders and the significant difference between MPN and AML patients in terms of Ang-1 and Ang-2 levels, it may be speculated that serial measurements of their levels could be used for early prediction of leukemic transformation in MPN patients.
References
Saharinen P, Eklund L, Pulkki K, Bono P, Alitalo K (2011) VEGF and angiopoietin signaling in tumor angiogenesis and metastasis. Trends Mol Med 17:347–362
Khosravi Shahi P, Fernández Pineda I (2008) Tumoral angiogenesis: review of the literature. Cancer Invest 26:104–108
Gianelli U, Vener C, Raviele PR, Savi F, Somalvico F, Calori R, Iurlo A, Radaelli F, Fermo E, Bucciarelli P, Bori S, Coggi G, Deliliers GL (2007) VEGF expression correlates with microvessel density in Philadelphia chromosome-negative chronic myeloproliferative disorders. Am J Clin Pathol 128:966–973
Lundberg LG, Lerner R, Sundelin P, Rogers R, Folkman J, Palmblad J (2000) Bone marrow in polycythemia vera, chronic myelocytic leukemia, and myelofibrosis has an increased vascularity. Am J Pathol 157:15–19
Kvasnicka HM, Thiele J (2004) Bone marrow angiogenesis: methods of quantification and changes evolving in chronic myeloproliferative disorders. Histol Histopathol 19:1245–1260
Hussong JW, Rodgers GM, Shami PJ (2000) Evidence of increased angiogenesis in patients with acute myeloid leukemia. Blood 95:309–313
Dickson DJ, Shami PJ (2001) Angiogenesis in acute and chronic leukemias. Leuk Lymphoma 42:847–853
Alonci A, Allegra A, Bellomo G, Penna G, D’Angelo A, Quartarone E, Musolino C (2008) Evaluation of circulating endothelial cells, VEGF and VEGFR2 serum levels in patients with chronic myeloproliferative diseases. Hematol Oncol 26:235–239
Medinger M, Mross K (2010) Clinical trials with anti-angiogenic agents in hematological malignancies. J Angiogenes Res 2:10
Musolino C, Alonci A, Bellomo G, Loteta B, Quartarone E, Gangemi D, Massara E, Calabrò L (2004) Levels of soluble angiogenin in chronic myeloid malignancies: clinical implications. Eur J Haematol 72:416–419
Shim WS, Ho IA, Wong PE (2007) Angiopoietin: a TIE(d) balance in tumor angiogenesis. Mol Cancer Res 5:655–665
Lee CY, Tien HF, Hu CY, Chou WC, Lin LI (2007) Marrow angiogenesis-associated factors as prognostic biomarkers in patients with acute myelogenous leukaemia. Br J Cancer 9:877–882
Schliemann C, Bieker R, Thoennissen N, Gerss J, Liersch R, Kessler T, Büchner T, Berdel WE, Mesters RM (2007) Circulating angiopoietin-2 is a strong prognostic factor in acute myeloid leukemia. Leukemia 21:1901–1906
Kümpers P, Koenecke C, Hecker H, Hellpap J, Horn R, Verhagen W, Buchholz S, Hertenstein B, Krauter J, Eder M, David S, Göhring G, Haller H, Ganser A (2008) Angiopoietin-2 predicts disease-free survival after allogeneic stem cell transplantation in patients with high-risk myeloid malignancies. Blood 112:2139–2148
Hou HA, Chou WC, Lin LI, Tang JL, Tseng MH, Huang CF, Yao M, Chen CY, Tsay W, Tien HF (2008) Expression of angiopoietins and vascular endothelial growth factors and their clinical significance in acute myeloid leukemia. Leuk Res 32:904–912
Tefferi A, Vardiman JW (2008) Classification and diagnosis of myeloproliferative neoplasms: the 2008 World Health Organization criteria and point-of-care diagnostic algorithms. Leukemia 22:14–22
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, Harris NL, Le Beau MM, Hellström-Lindberg E, Tefferi A, Bloomfield CD (2009) The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 114:937–951
Quartarone E, Alonci A, Allegra A, Bellomo G, Calabrò L, D’Angelo A, Del Fabro V, Grasso A, Cincotta M, Musolino C (2006) Differential levels of soluble angiopoietin-2 and Tie-2 in patients with haematological malignancies. Eur J Haematol 77:480–485
Medinger M, Skoda R, Gratwohl A, Theocharides A, Buser A, Heim D, Dirnhofer S, Tichelli A, Tzankov A (2009) Angiogenesis and vascular endothelial growth factor-/receptor expression in myeloproliferative neoplasms: correlation with clinical parameters and JAK2-V617F mutational status. Br J Haematol 146:150–157
Mazzieri R, Pucci F, Moi D, Zonari E, Ranghetti A, Berti A, Politi LS, Gentner B, Brown JL, Naldini L, De Palma M (2011) Targeting the ANG2/TIE2 axis inhibits tumor growth and metastasis by impairing angiogenesis and disabling rebounds of proangiogenic myeloid cells. Cancer Cell 19:512–526
Scholz A, Lang V, Henschler R, Czabanka M, Vajkoczy P, Chavakis E, Drynski J, Harter PN, Mittelbronn M, Dumont DJ, Plate KH, Reiss Y (2011) Angiopoietin-2 promotes myeloid cell infiltration in a β2-integrin-dependent manner. Blood 118:5050–5059
Kim H, Koh GY (2011) Ang2, the instigator of inflammation. Blood 118:4767–4768
Conflict of interest
The authors report no declarations of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Atesoglu, E.B., Tarkun, P., Mehtap, O. et al. Serum Angiopoietin Levels are Different in Acute and Chronic Myeloid Neoplasms: Angiopoietins do not only Regulate Tumor Angiogenesis. Indian J Hematol Blood Transfus 32, 162–167 (2016). https://doi.org/10.1007/s12288-015-0548-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12288-015-0548-8