Abstract
In actuality, chronic lymphocytic leukaemia (CLL) remains an incurable haematopoietic malignancy of high prevalence amongst elderly populations in the West. Malignant CLL cells characteristically accumulate in the peripheral blood, bone marrow, lymph nodes, and spleen of CLL patients. There is evidence that CLL cells express Ang2 and Tie1, two central components of the Ang-Tie2 pro-angiogenic pathway. Central to blood vessel development and maintenance, at present it remains unclear how the Ang-Tie2 pathway modulates CLL pathophysiology. Here we evaluate the status of the Ang-Tie2 pathway in CLL cells and assess Ang1 levels in plasma/cell medium from CLL samples. To understand how angiopoietins in the microenvironment regulate the components of Ang-Tie2 pathway, survival, migration, and metabolic fitness of CLL cells, we exposed CLL cells to recombinant angiopoietins. CLL plasma and CLL cells in culture present significant lower levels of Ang1. CLL cells simultaneously express Ang1, Ang2, and Tie1 mRNA, but lack that of Tie2 and its regulator, VE-PTP. Exposure to Ang1 confers survival advantage in the long-term, whereas Ang2 and trebananib, an angiopoietin blocker, proved detrimental. Angiopoietins differentially modulate expression of Ang1, Ang2, and Tie1 transcripts. Ang2, but not Ang1, induces the concomitant and transient expression of Tie2 and VE-PTP mRNA. Both angiopoietins, particularly Ang2, increase CLL-Tie1 expression and Ang1 clearly induces chemotaxis and transendothelial-like migration of CLL cells. Besides, changes in caspase and ATP content corroborate the sensitivity of CLL cells to angiopoietin exposure. Altogether, this work shows that angiopoietins regulate the fate of CLL cells in a Tie2-independent manner and highlights the potential of the Ang-Tie2 pathway as a therapeutic target in CLL research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pathological angiogenesis is a dreadful biological process linked to the disproportionate development of blood vessels that support growth and proliferation of solid tumours. However, participation of pathological angiogenesis in chronic lymphocytic leukaemia (CLL), as well as in other haematopoietic malignancies, is difficult to envision, mainly because leukaemia cells do not depend directly on a network of vessels and capillaries to support basic physiological requirements. Nonetheless, it is widely accepted that pathological angiogenesis supports blood cancers [1, 2]. CLL remains an incurable and highly prevalent haematopoietic malignancy amongst the elderly in western societies [3]. Patients diagnosed with CLL present a heterogeneous collection of clinical, cellular, chromosomal, molecular, and genetic traits, all of which medical practitioners evaluate to accurately diagnose the disease and to administer the optimal treatment. Whilst the average age of patients diagnosed with CLL is between 67 and 72 years, available diagnostic tools allow early diagnosis in patients as young as 40 years of age [3]. Notably, younger CLL patients display the most severe symptoms attributed to this malignancy [3, 4]. As quality of life and life expectancy increase amongst the general world population, the morbidity and mortality rates due to CLL cases will likewise increase in the upcoming years [3]. Therefore, the necessity of alternative therapeutic avenues to circumvent resistance and relapses attributed to current treatments prompt us to study the molecular mechanics of CLL-related angiogenic signalling pathways.
Peterson et al. provided the first strong evidence linking angiogenic signalling pathways with CLL pathophysiology by showing increased microvessel density in bone marrow (BM) biopsies and detecting elevated secretion levels of basic fibroblast growth factor (bFGF) in the urine of CLL patients [5]. Researchers also detected high levels of vascular endothelial growth factor (VEGF) in CLL patients [2] and together with bFGF, VEGF is one of the most studied angiogenic factors in cancer research. Similar to the overexpression of VEGF and bFGF, recent research describing the overexpression of angiopoietin-2 (Ang2) in CLL cases highlights the relevance of angiopoietins in the CLL microenvironment [6–8]. There is a correlation between high plasma levels of Ang2 with disease progression, and in addition, isolated CLL cells abundantly secrete Ang2 in culture. Due to the absence of Tie2 receptor in CLL cells, scientists considered the Ang-Tie2 pathway as inactive on these leukemic lymphocytes [2]. Whilst CLL cells fail to express Tie2 receptor [2], they express Tie1 receptor; its expression correlates with CLL disease stages [9]. These leukemic lymphocytes abundantly secrete Ang2 into the microenvironment, probably contributing to the high plasma levels of Ang2 detected in CLL patients [6, 7]. The constitutive expression of Ang2 and Tie1 and their correlation with disease progression certainly arouses the interest of CLL research on this particular angiogenic signalling pathway.
Together with pro-angiogenic Ang1, receptors Tie1 and Tie2, and VE-PTP, Ang2 comprises the Ang-Tie2 pathway, which regulates vessel assembly and maturation during embryogenesis and secures quiescence of the vascular tissue during adult life [10]. Ang1 and Ang2 are agonist and antagonist ligands respectively, which modulate angiogenesis by binding to Tie2. Receptors Tie1 and Tie2 are type I transmembrane protein receptor tyrosine kinases (RTKs) of homologous structures involved in proliferation, migration, and survival of endothelial cells (EC) [11]. Pro-angiogenic Ang1 promotes EC survival in a dose-dependent manner, supports EC network formation and stabilization, and reduces apoptosis in EC models, an effect increased in the presence of VEGF [12]. Most importantly, Ang1 maintains quiescent blood vessels [13], decreases vascular permeability [14], and repairs damaged and leaky vessels [15]. Besides, Ang1 overexpression results in varying degrees of reduced tumour growth and surprisingly, healthy adults present relatively high levels of Ang1 (40–50 ng/ml) [10]. In contrast, Ang2 destabilizes and remodels vascular endothelium [16] and its secretion dramatically increases during vasculogenesis and inflammation [17]. Overexpression of Ang2 induces severe discontinuities in vessel development [18] and high levels of Ang2 associate with the degree of severity of the malignancy, making Ang2 an attractive prognostic marker of neoplasias [10]. At a pathological level, Ang-Tie2 signalling is strongly associated with inflammation [14] and tumour-related angiogenesis [19].
Not long ago, molecular biology could neither explain the precise mechanisms of action of agonist Ang1 and antagonist Ang2, the detailed function of Tie1 and Tie2 receptors, nor the precise interactions between ligands and receptors. Early models overexpressing Ang1 and Ang2 in vivo [20] proved that Ang1 activates and Ang2 blocks signalling events downstream of Tie2 [18]. Today biochemical evidence provides us with a more unified model of Ang-Tie2 signalling, depicting clear roles and interactions between ligands and receptors [11, 19, 21, 22]. Tie1 and Tie2 interact through their ectodomains forming a complex detected even prior to angiopoietin recognition, and here kinase domains play no role in Tie2 clustering or Tie2 relocalization [11]. This Tie1-Tie2 complex inhibits Tie2-dependent signalling transduction and both angiopoietins differentially modulate the Tie1-Tie2 complex. Whilst Ang1 binds to Tie2 inducing dissociation of Tie1 from Tie2, clustering of Tie2, and activation of Tie2-dependent signal transduction, Ang2 fails to induce a similar effect and prevents Ang1 from binding to Tie2 [11]. Both Ang1 and Ang2 bind by complementary surface interaction to the same site on Tie2 [19] and each angiopoietin possesses specific amino acid residues on their surface that clearly define their contrasting cell-signalling roles [22]. Moreover, Ang1 activation of Tie2 shows an evident association of VE-PTP to Tie2 and VE-PTP dissociation enhances Tie2 activation by Ang1 [23]. VE-PTP negatively regulates Tie2-dependent proliferation during embryonic development and blood vessel remodelling [23], binds and dephosphorylates activated Tie2, attenuates Tie2 activity, and resensitizes Tie2 to new angiopoietin stimuli [24]. Whilst the role of Tie2 is well characterized, the molecular and physiological contributions of Tie1 beyond its association with Tie2 are rather unclear [11] and those of VE-PTP are just being uncovered [23, 25–27]. To our knowledge, no attempts to describe the role of VE-PTP or to understand the impact that Ang1 has on the CLL microenvironment exist.
The full contributions of the Ang-Tie2 pathway and its components to CLL pathophysiology at the molecular and cellular level remain to date a complete mystery. In this report, we explore the parallel expression pattern of the components of the Ang-Tie2 signalling pathway in CLL cells. Additionally, we measure Ang1 levels in plasma from CLL patients and Ang1 levels secreted by CLL cells in media. To assess the impact of Ang1 and Ang2 on CLL cell survival, we mimic angiopoietin microenvironmental availability by exposing CLL cells to recombinant human Ang1 and Ang2. We monitor survival advantage for short and long periods and analyse fold changes in relative mRNA levels of Ang1, Ang2, and Tie1 in CLL cells. In addition, we explore whether exposure to angiopoietins could trigger Tie2 and VE-PTP expression as well as changes on Tie1 expression on CLL cells. We also assess the ability of angiopoietin to modulate chemotaxis and transendothelial-like migration of CLL cells. To further asses the sensitivity of CLL cells to angiopoietins, we evaluate changes in contents of caspase and ATP in these leukemic lymphocytes upon angiopoietin exposure. Our results point toward a dynamic role of angiopoietins in regulating the fate of CLL cells in a Tie2-independent manner at the molecular and cellular level.
Materials and Methods
Compliance with Ethical Standards
Our research was performed in accordance with the declaration of Helsinki and approved by the internal revision board of the University Hospital, Cologne. CLL patients signed a consent form and all had confirmed CLL status prior to the time of peripheral blood collection. Processing of peripheral blood and isolation of CLL cells was carried by personal of the Biobank Center for Integrated Oncology (CIO) Cologne/Bonn, at the University Hospital, Cologne.
Isolation of CLL Cells and Healthy PBMCs
Peripheral blood from CLL and healthy patients was collected in EDTA-treated tubes. PB from CLL patients was incubated with the RosetteSep® B-cell enrichment antibody cocktail (StemCell Technologies) and CLL cells were isolated by the Ficoll gradient (PAA Biotech). Quality check by flow cytometry analysis (FACS-Gallios, Beckman Coulter) showed that the isolated CLL cells have a purity ≥ 99.1 % of CD5/CD19 double positive cells, confirming that the CLL samples are free from other cellular entities. Additionally, CLL viability was ≥99 % as assessed by tryptan-blue staining using an automated cell counter (Beckman Coulter) and by flow cytometry (FACS-Gallios, Beckman Coulter) using FITC-Annexin-V/7-AAD (Biolegend) viability staining assay. Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll gradient.
Cell Culture
PBMCs and CLL cells were processed immediately after isolation and cultured under standard humidified atmosphere at 37 °C/5 % CO2. Throughout our experiments, we employed RPMI 1640-Glutmax (Gibco) medium, supplemented with 1 %-penicillin/streptomycin (PAA Biotech) and 10 % foetal calf serum (PAA Biotech). Quality controls by light microscopy demonstrated that no cells with the typical morphology of ECs or that of any adherent cell line were present in either PBMC or CLL cell cultures, further confirming flow cytometry quality control. Conditioned RPMI media is designed to support primary cells and fails to supports the growth of ECs as tested using human umbilical vein endothelial cells (HUVECs).
Assessment of Survival Upon Stimulation with Ang1, Ang2, and Neutralizing Peptibody
CLL cells were stimulated with either recombinant human Ang1, Ang2 (Prepotech), or trebananib (AMG386, kindly provided by AMGEN) at concentrations of 50, 100, 200, 500 ng/ml and cultured in 96-well plates (1×10^7 cells/ml) for 1 and 4 days. Cell viability was assessed by flow cytometry (FACS-Gallios, Beckman Coulter) using FITC-Annexin-V/7-AAD viability assay.
Concentration of Ang1 Secretion in Plasma and Cell Medium
For plasma collection, we depleted cells from peripheral blood of healthy and CLL patients by centrifuging 3000 g/20 min/4 °C. To measure Ang1 in cell media, healthy PBMCs and CLL cells (1×10^7cells/ml) were cultured for 24 h and depleted of media by centrifuging 1000 g/15 min/4 °C. To assess the concentration of Ang1 we employed a Quantikine ELISA Human Angiopoietin-1 kit (R&D) following the provided protocol and the plate was analysed photometrically (μQuant Bio-TEK instruments) with the suggested OD correction (OD450–OD565).
Primer Design
The mRNA sequences Ang1, Ang2, Tie1, Tie2, and VE-PTP were obtained from NCBI Reference Sequence and primer pairs picked from the Basic Local Alignment Search Tool (BLAST) query for primer pairs exclusively expanding exon-exon junctions. Identity and product size were further verified using In-Silico PCR available from the University of California at Santa Cruz (UCSC) Genome Browser. All primers were purchased from TIB MOLBIOL (Berlin, Germany) and solved in DEPC-treated water (Roth, Germany).
RNA Extraction and cDNA Synthesis
In all cases, cells were harvested 800 g/10 min/4 °C, washed with PBS-3x, lysed with RLT buffer (Qiagen), snap frozen in liquid nitrogen, and stored at −80 °C. At time of processing, lysates were allowed to thaw on ice and brought to room temperature with alternate vortexing. RNA material was extracted as suggested by the Rneasy Plus Mini Kit (Qiagen). RNA integrity was verified by electrophoresis on a 1.5 % agarose gel in parallel with a 1000 bp DNA ladder (Thermo Scientific). RNA concentration and purity were assessed photometrically (NanoPhotometer® P-Class, Implem). cDNA was synthesised with a RevertAid First Strand cDNA synthesis kit (Thermo Scientific) and reverse transcribed (Mastercycler, Eppendorf) as follows: 10 min/25 °C, 50 min/50 °C, 5 min/80 °C, cooling to 4 °C.
Qualitative Polymerase Chain Reaction (PCR)
For qualitative PCR, we employed 2xFastStart PCR Master Mix (Roche). To calculate working melting temperature (Tm, X°C= optimal primer pair Tm), all primer pairs were subjected to gradient PCR (96 Universal Gradient, peqLAB) using all available cDNAs and non-template controls (NTC). The standard PCR program was comprised of initial denaturation of 10 min/95 °C, followed by 40 cycles of denaturation 30 s/95 °C, amplification at 30 s/X°C, and elongation at 30 s/72 °C, followed by final elongation 2 min/72 °C and cooling to 4 °C. PCR product sizes were verified on 1 % agarose gel in parallel with a 100 base pair (bp) DNA ladder (ThermoScientific) as a molecular marker.
Semi-quantitative Real Time-PCR
To determine changes in the expression of Ang1, Ang2, and Tie1, CLL cells were stimulated with 500 ng/ml of Ang1 and Ang2 for 1 h and RNA/cDNA processed as in 3.7. We employed Maxima SYBR Green qPCR 2xMaster Mix (ThermoScientific) to run 20 μl rt-PCR reactions using a Light Cycler System 2.0 (Roche, Mannheim, Germany) and its accompanying software. In order to validate primer efficiency and empirical Tm, primer pairs were tested at parallel 10-fold serial dilutions over a range of five magnitudes using all available cDNAs as template and respective non-template control. All RT-PCR reactions were run with a denaturation of 15 min/95 °C, 40 cycles of denaturation 30 s/95 °C, amplification 30 s/X°C, and elongation 30 s/72 °C, followed by a final elongation of 1 min/72 °C and melting curve analysis to confirm identity of rt-PCR products. Relative gene expressions were calculated by the ΔΔCt method [28] and normalized to the reference gene ABL (Abelson murine leukaemia viral oncogene homolog-1).
Detecting Transient Expression of Tie2 and VE-PTP
CLL cells (1×10^7 cells/ml) were stimulated with 500 ng/ml Ang1 or Ang2, and collected after 30 min and 6 h. The corresponding non-stimulated samples were collected prior to stimulation, and at 30 min and 6 h post-stimulation. RNA/cDNA were processed as described in 2.7. As a possible control of Tie2 and VE-PTP expression, we utilized cDNA extracted from HUVEC cells (PromoCell). Due to suspected low expression, PCR products were analysed by capillary gel electrophoresis to confirm expression. ABL reference gene was visualized by classical electrophoresis.
Assessment of Tie1 and Tie2 Expression by Flow Cytometry
CLL cells (1×10^7 cells/ml) were stimulated with 500 ng/ml of Ang1 or Ang2 for 24 h, washed with PBS-3x and conditioned with Human TruStain FcX™ Fc-receptor blocker (Biolegend). Cells were stained with polyclonal antibodies against either Tie1, Tie2, or corresponding isotype, all conjugated to phycoerythrin (R&D, USA) and analyzed by flow cytometry (FACS-Gallios, Beckman Coulter).
Assessment of Chemotaxis and Transendothelial-Like Migration Activity
To test the chemotactic effect of angiopoietins on CLL cells, we employed Transwell Permeable Support (Corning Inc) inserts with a pore size of 5 μm adapted for 24-well plates. To test the transendothelial-like migration effect, we employed ThinCert (Greiner Bio-One) inserts with a pore size of 3 μm adapted for 24-well plates. Wells and inserts were preconditioned with cell culture media for 12 h at standard cell culture conditions. CLL cells were seeded at 1×10^7 cells/ml and volumes processed as suggested by the manufacturer. Media in the bottom chamber was supplemented with either 500 ng/ml of Ang1 and Ang2, and in combination with trebananib as angiopoietin blocker. CLL cells were incubated for 24 h, cells were retrieved from the bottom chamber, and counted with a haemocytometer.
Caspase Relative Content Assay
Caspase activity was assessed with Cell Meter™ Caspase 3/7 Activity Apoptosis Assay Kit (AAT Bioquest, Inc.) employing black-wall 96-well plates (Greiner Bio) with transparent bottom, which were pre-coated with poly-d-lysine (50 μg/ml, Sigma-Aldrich) for 24 h/4 °C with constant shaking, washed with PBS-3x, and allowed to air-dry in a sterile environment with complementary UV-treatment. CLL cells were seeded at the concentration suggested by the manufacturer in parallel with corresponding caspase content dilution curves of untreated cells for all measurements. Cells were stimulated with Ang1, Ang2, or trebananib at concentrations ranging from 5 fg/ml to 500 ng/ml for 24 h. Changes in fluorescence were monitored with a Paradigm Detection Platform connected to Multimode Analysis Software (Beckman Coulter).
ATP Relative Content Assay
ATP relative content was assessed using CellTiter-Glo® Luminescent Cell Viability Assay (Promega). CLL cells were seeded as suggested with a corresponding ATP content dilution curve of untreated cells. Cells were stimulated with Ang1, Ang2, or trebananib at concentrations ranging from 5 fg/ml to 500 ng/ml in white-wall 96-well plates (Sarsted, Germany) and incubated for 24 h. Plates were analysed with a microplate luminometer (EG&G Berthold).
Statistics and Graph Design
Results are shown as mean ± bars of standard error of the mean (SEM). Significance was calculated using Windows Microsoft Excel 2010 with a two-tailed student t-test and minimal statistical significance was set at p ≤ 0.05. Graphs were processed using GraphPad Prism Version 5.
Results
CLL Cells Express in Parallel Ang1, Ang2, Tie1, but not Tie2 or VE-PTP
To understand the extend to which the Ang-Tie2 pathway is active in CLL cells, we analysed in parallel the expression of Ang1, Ang2, Tie1, Tie2, and VE-PTP at the mRNA level in CLL cells and healthy PBMCs by qualitative PCR. CLL cells express Ang1, Ang2, and Tie1 transcripts (Fig. 1) and lack Tie2 and VE-PTP transcripts. Besides expressing Ang1, Ang2, and Tie1, the healthy PBMC population expresses Tie2. We failed to detect the regulator of Tie2 activity, VE-PTP, in both, CLL and healthy PBMC samples. Previously Kay et al. analysed the expression of some angiogenic factors and receptors in CLL patients, detecting expression of Tie1 and Ang1 and similarly failed to detect Tie2 transcripts [2]. Ang2 expression in CLL and its correlation with disease progression has been extensively described in the literature [6, 8, 28]. Furthermore, Aguayo et al. described Tie1 expression [29] in CLL samples and its correlation with CLL disease stage.
Expression patterns of the components of the Ang-Tie2 pathway in CLL cells and healthy PMBCs. Agarose gel electrophoresis showing the detection of Ang1, Ang2, Tie1, Tie2, VE-PTP and reference gene ABL. a-e CLL samples. 1–2 Healthy PMBCs samples. NTC; non-template controls, BP; size in base pairs. MM; molecular marker
According to our preliminary test readings, B-cells extracts appear to be positive for Ang1, Ang2, Tie1, and negative for Tie2 and VE-PTP, but unlike the samples shown in Fig. 1, these B-cells come from buffy coats derived from several blood donors. There is one important point that must be considered when dealing with these kinds of samples. Reports based on highly sensitive detection (1 in 105 cells) of cells positive for CD5, CD19, CD20, and CD79b reveal that up to 3 % of healthy individuals show a detectable population of lymphocytes with a malignant profile, that is, a profile identical to that of CLL cells [30]. Patients, however, lack lymphadenopathy or organomegaly and may never progress into a full CLL [31]. Thus, B-cell preparations isolated from buffy coats probably contain CLL-like cells. Development of powerful cell sorting techniques in haematology is necessary to help researcher to work with highly pure CLL-cell free B-cell fractions and to define the true profile of B-cells on the Ang-Tie2 pathways context.
The low expression of Tie2 in the PBMC population possibly derives from Tie2 expressing monocytes (TEMs), which comprise approximately 2–7 % of the total PBMCs population of healthy patients [32], therefore they represent an integral part of the PBMC population. Furthermore, we discard the presence of ECs in PMBCs or CLL cell extracts, because no VE-PTP was detected in PMBCs (ECs are positive for VE-PTP) and because ECs also represent an insignificant minority of 0.01 to 0.0001 % of mononuclear cells in complete normal peripheral blood [33]. This renders their contribution in angiopoietins secretion or mRNA detection, if any, as insignificant. Whilst the number of EC may rise in the case of vascular damage seen in other malignancies (e.g. melanoma, glioma, breast, colonic, gastric, oesophageal, renal, ovarian, cervical, carcinoid, testicular, prostate, and head and neck cancer patients) [33], there is to date no evidence of a similar issue in CLL.
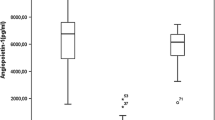
Downregulation of Ang1 in CLL is Evident in Both Plasma and Cell Media
We evaluated plasma of healthy and CLL patients, as well as culture media from PBMCs and CLL cells after 24 h in culture to determine concentration of Ang1 (Fig. 2). Here, we detected a significant (p = 0.04) downregulation of Ang1 levels in plasma (Fig. 2b) of CLL patients (2336 pg/ml) when compared to healthy patients (4414 pg/ml). Cells in culture show a similar discrepancy (Fig. 2b). PBMCs secrete significantly (p = 0.002) higher levels of Ang1 (632 pg/ml) when compared with CLL cells (67 pg/ml). This downregulation of Ang1 in CLL patients is rather remarkable. Tie2-expressing cells, such as ECs, require Ang1 to support the quiescent state of blood vessels and capillaries. The observed downregulation of Ang1 could lead to a leaky state of vessels and capillaries, facilitating perfusion of leukemic lymphocytes between organs, tissues, and the blood stream.
Ang1 levels in plasma and cell media in healthy and CLL samples. a Ang1 levels as detected in plasma from healthy and CLL patients. b Ang1 levels secreted by PMBCs and CLL cells (1×10^7 cells/ml) after 24 h in culture. Plasma samples; healthy n = 10, CLL n = 10. Cell culture, PMBCs n = 10 and CLL samples n = 25. Significance set at p ≤ 0.05 (*) and p ≤ 0.005 (**)
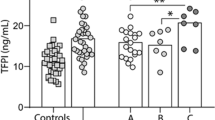
Angiopoietins Modulate the Survival of CLL Cells
We stimulated CLL cells with recombinant human Ang1 and Ang2 for short (1 day) and long (4 day) intervals to examine whether angiopoietins present in the microenvironment modulate CLL cell survival. Because CLL cells constitutively express and secrete Ang1 (Fig. 2) and Ang2 [7] at a basal level, we blocked endogenous Ang1 and Ang2 with trebananib to monitor angiopoietins autocrine role in CLL cell survival. At 1 day post-stimulation, Ang1 shows no impact on survival (Fig. 3a), Ang2 (Fig. 3b) induces a slight reduction in survival (50 ng/ml not significant (n.s.), 100 ng/ml −4.2 % p = 0.05, 200 ng/ml -7.1 % p = 0.05, 500 ng/ml -10.% p = 0.005), and trebananib appears to have no effect (Fig. 3c). Nevertheless, long-term culture shows interesting changes in survival advantage. At 4 d Ang1 (Fig. 3a) stimulation confers significant survival advantage in a dose dependent manner (50 ng/ml +4.4 % p = 0.048, 100 ng/ml +6.7 % p = 0.01, 200 ng/ml + 7.9 % p = 0.02, 500 ng/ml +11.5 % p = 0.003,), whilst Ang2 (Fig. 3b) significantly decreases CLL survival (50 ng/ml n.s., 100 ng/ml n.s., 200 ng/ml -8.2 % p = 0.04, 500 ng/ml -9.0 % p = 0.04) also in a dose dependent manner. The pro-survival effect of Ang1 and the detrimental one of Ang2 in a long-term analysis suggests that early angiopoietin interaction with CLL cells is sufficient to regulate long-term survival advantage. In addition, trebananib strongly and specifically binds both Ang1 and Ang2, blocking their interaction with their targets. After 4 days of trebananib stimulation (Fig. 3c) we observed an unexpected and significant detriment in CLL cell survival (50 ng/ml n.s., 100 ng/ml n.s., 200 ng/ml n.s., 500 ng/ml -12.3 % p = 0.01), suggesting that CLL-derived Ang1 and Ang2 confer survival advantage to CLL cells. Due to the significant effect on survival advantage, we employed 500 ng/ml of Ang1, Ang2, or trebananib in subsequent stimulation procedures.
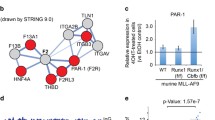
Ang1 and Ang2 Regulate mRNA Expression of Ang1, Ang2, and Tie1
The presence of Ang1, Ang2, and Tie1 mRNA in CLL samples is a suggestive indicator of Ang-Tie2 signalling activity in CLL cells. We stimulated CLL cells with angiopoietins to determine whether microenvironmentally available Ang1 and Ang2 modulate expression of Ang1, Ang2, and Tie1 transcripts. Interestingly, when evaluating changes in the relative levels of mRNA expression 1 h post angiopoietin stimulation, we observed that both angiopoietins differentially induce changes in the expression of Ang1, Ang2, and Tie1 (Fig. 4). With respect to non-stimulated control (1.00), Ang1 stimulation induces a slight and significant increase to 1.14 fold (p = 0.018) of Ang2 mRNA, and slight and significant increase to 1.31 fold (p = 0.029) of Tie1 mRNA. Ang2 stimulation only induces a slight and significant increase of 1.55 fold (p = 0.042) of Ang2 mRNA. The ability of angiopoietins to modulate the relative mRNA contents of Ang1, Ang2, and Tie1 on CLL cells illustrates the sensitivity of CLL cells to angiopoietins present in the microenvironment. Taking in consideration that CLL cells from peripheral blood lack Tie2 receptor, we could infer that angiopoietins recognize alternate receptors on the surface of CLL cells, which in turn regulate angiopoietins and Tie1 mRNAs.
Ang2 Stimulation Induces Transient Expression of Tie2 and VE-PTP mRNA
Qualitative PCR showed that CLL samples express Ang1, Ang2, and Tie1, yet CLL cells from peripheral blood do not express Tie2 supporting previous works [2] nor they express VE-PTP (Fig. 1). To assess whether angiopoietins trigger expression of either VE-PTP or Tie2 in CLL cells, we stimulated CLL cells with 500 ng/ml of Ang1 or Ang2 and collected samples at 30 min and 6 h. Interestingly, we detect the transient and concomitant expression of both VE-PTP and Tie2 transcripts only after 30 min of Ang2 stimulation (Fig. 5). These transcripts are not detectable upon Ang1 stimulation and neither detectable at 6 h post-stimulation with either angiopoietin. We could infer from this observation that CLL cells actively react to externally available angiopoietins to transiently control transcription of the components of the Ang-Tie2 pathway.
Electrophoresis showing the transient expression of Tie2 and VE-PTP transcripts. After 30 min, stimulation with Ang2 induces expression of Tie2 and VE-PTP. After 6 h, these transcripts are no longer detectable. Tie2 and VE-PTP transcripts were visualised on capillary electrophoresis. HUVEC cells used as positive control for Tie2 and VE-PTP expression. Reference gene ABL was run on regular gel electrophoresis. BP; base pairs, NTC; non-template control, NSC; non-stimulated control
Angiopoietins Modulate Patterns of Tie1 Expression on CLL cells
Since CLL cells from peripheral blood express Tie1 and fail to express Tie2 [2] we wondered whether Ang1 and Ang2 were capable of modulating Tie1 expression of CLL cells. Our flow cytometer analysis shows expression of Tie1 (Fig. 6a), but we failed to detect Tie2 (Fig. 6b), backing qualitative PCR findings. In addition, our analysis shows that stimulating CLL cells with Ang1 significantly increases the CLL-Tie1 relative expression (Fig. 6c) by 7.7 % (p = 0.014) and stimulation with Ang2 significantly increases the CLL-Tie1 expression to 12.5 % (p = 0.006). This observation suggest that varying concentration of angiopoietins encountered in the microenvironment differentially control Tie1 expression on CLL cells.
Tie1 and Tie2 detection by flow cytometry on CLL cells upon angiopoietin exposure. a Histogram shows the shift in detecting Tie1-relative fluorescence. b Histogram shows the lack of Tie2-positive CLL cells. c Graph shows the relative increase in Tie1-relative expression in non-treated control (Set to 100 %), and Ang1 and Ang2 stimulated samples. n = 6. Significance set at p ≤ 0.05
Angiopoietins Modulate Chemotaxis and Transendothelial-Like Migration of CLL Cells
In order to explore the impact of angiopoietins and their blockage in chemotaxis, we employed inserts with a 5.0 μm/pore. Stimulation with Ang1 but not Ang2 (Fig. 7a) induced robust chemotaxis of CLL cells (p = 0.0006). Blocking Ang1 and Ang2 by adding trebananib to the media significantly abrogates homing-like migration (Ang1 + Tre p = 0.01, Ang2 + Tre p = 0.03). To test whether angiopoietins are capable of inducing transendothelial-like migration of CLL cells, we employed inserts of 3.0 μm/pore. Interestingly, Ang1 induces significant transendothelial-like migration (Fig. 7b, Ang1 p = 0.0008, Ang2 n.s.). In this instance, trebananib significantly abrogates CLL movement through the membrane (Ang1 + Tre p = 0.048, Ang2 + Tre p = 0,044). Apparently, Ang1 not only supports CLL cell survival advantage, but also angiopoietin-mediated migration and, strikingly, transendothelial-like movement.
Chemotactic and transendothelial-like migration activity of CLL cells upon angiopoietin stimulation and angiopoietin blockage. a) Ang1 has a strong effect on homing-like activity on CLL cells and Ang2 display a pattern similar to that of the untreated control (UTC). b) Ang1, but not Ang2, has a strong effect inducing transendothelial-like migration. Trebananib blocks Ang1 in both a) and b), bringing relative values close to a basal level, which are also comparable those of Ang2 stimulation. n = 6. n.s.; non-significant. Significance set at p ≤ 0.05
Angiopoietins Differently Regulate Caspase and ATP Relative Contents
We evaluated the impact of angiopoietins on the metabolic fitness of CLL cells by assessing caspase and ATP relative content. First, stimulation with Ang1 and Ang2 after 24 h induces a constant reduction of caspase relative content in CLL cells (Fig. 8). When comparing to non-stimulated control (Set as 100 % reference), stimulation with as low as 5 fg/ml of Ang1 (Fig. 8a) induces a decrease of caspase content, remaining relatively steady as concentration increased (5 fg/ml 70.4 %, 50 fg/ml 65.4 %, 500 fg/ml 73.2 %, 5 pg/ml 68.8 %, 50 pg/ml 77.4 %, 500 pg/ml 73.8 %, 5 ng/ml 71 %, 50 ng/ml 76.8 %, and 500 ng/ml 71.1 %). Stimulation with Ang2 (Fig. 8b) also results in a decrease of caspase content (5 fg/ml 71.5 %, 50 fg/ml 72.5 %, 500 fg/ml 72 %, 5 pg/ml 67.6 %, 50 pg/ml 73 %, 500 pg/ml 65.6 %, 5 ng/ml 68.2 %, 50 ng/ml 67.5 %, and 500 ng/ml 56.4 %). Interestingly, stimulation with trebananib (Fig. 8c) triggers an increase of caspase activity only on CLL cells (5 fg/ml 99.3 %, 50 fg/ml 97.2 %, 500 fg/ml 86 %, 5 pg/ml 106.3 %, 50 pg/ml 110.3 %, 500 pg/ml 110.3 %, 5 ng/ml 122.3 %, 50 ng/ml 120.5 %, and 500 ng/ml 127.8 %). Second, slight reduction of ATP relative content remains constant upon Ang1 (Fig. 9a) stimulation (5 fg/ml 67.5 %, 50 fg/ml 67.5 %, 500 fg/ml-67.4 %, 5 pg/ml 66.3 %, 50 pg/ml 66.8 %, 500 pg/ml 68 %, 5 ng/ml 64.1 %, 50 ng/ml 71.8 %, and 500 ng/ml 72.7 %). Ang2 stimulation (Fig. 9b) induces a large decrease in ATP content, decreasing as the concentration of Ang2 approaches 500 ng/ml (5 fg/ml 68.6 %, 50 fg/ml 67.2 %, 500 fg/ml 65.1 %, 5 pg/ml 61.8 %, 50 pg/ml 63.3 %, 500 pg/ml 62.6 %, 5 ng/ml 58.1 %, 50 ng/ml 55.9 %, 500 ng/ml 46.7 %). Exposure to trebananib (Fig. 9c) shows larger decrease of activity than that of Ang1 and Ang2 (5 fg/ml 56.3 %, 50 fg/ml 55.3 %, 500 fg/ml 56.6 %, 5 pg/ml 57.4 %, 50 pg/ml 49.5 %, 500 pg/ml 49.3 %, 5 ng/ml 45.9 %, 50 ng/ml 42 %, and 500 ng/ml 35.8 %). The decrease in ATP detection indicates the sensitivity of CLL cells toward the presence of Ang1 and Ang2 (Fig. 9a and b). Therefore, reduction of ATP activity induced by Ang1 indicates that CLL cells possibly profit from lowering their metabolic activity to preserve cellular energy. Reduction of ATP activity by Ang2 could correlate with apoptosis induction, which also becomes significant after 4 days in culture (Fig. 3b). In both assays, PBMCs appear without change in caspase and ATP relative contents after stimulation, indicating that the observed changes specifically affect CLL cells.
Caspase relative contents in CLL cells upon exposure to Ang1, Ang2, and trebananib. Relative changes in fluorescence are expressed as per cent change relative to non-stimulated CLL cells. Cells were stimulated with Ang1, Ang2, or trebananib at increasing concentration of a Ang1 b Ang2 and c trebananib. n = 6
Discussion
Some bystander (or accessory) cells in the microenvironment are secretors of angiopoietins. The first evidence of Ang1 and Ang2 expression in BM microenvironment showed that up to 75 % of all osteoblasts and osteoclasts express Ang1, and 25 % of these weakly express Ang2 [34]. Mural cells, fibroblasts and non-vascular cells are secretors of Ang1, whilst Ang2 secretion is attributed mainly to ECs [14]. Fibroblasts, which lack Tie2, adhere and spread in the presence of Ang1 but not Ang2, suggesting that migration and adhesion processes induced by Ang1 are Tie2-independent [35]. CLL researchers report a concomitant overexpression of Ang2 and pro-angiogenic VEGF in CLL patients [7]. Ang2 negatively impacts the CLL disease course [8] correlating not only with Binet staging, but also with high β-2-microglobulin levels, unmutated IgVH, elevated CD38-ZAP70 status, and intermediate-to-high risk cytogenetic profiles [6]. What is more, Ang2 levels also correlate with shorter time to first treatment (TTFT), disease aggressiveness, and rapid disease progression [36]. Regardless, the role of Ang1 in CLL pathophysiology is unclear. Here we report that when compared to healthy patients and healthy PBMCs, Ang1 levels in plasma from CLL patients (Fig. 2a) and in CLL cell culture medium (Fig. 2b) are significantly lower. Pericytes are essential in angiogenesis and vascular integrity and deficiency in pericyte coverage strongly associates with numerous diseases and uncontrolled angiogenesis [37]. Ang-2 treatment results in severe disassociation of pericytes and loss of pericyte coverage from tumour vessels, thus inducing vascular permeability [14, 38]. Lower Ang1 levels could possibly induce a pathological and transient state of compromised pericyte coverage, leaky vessels, and higher trafficking rates of leukemic lymphocytes between peripheral blood and the microenvironments.
The Ang1 levels in plasma from healthy and CLL patients dependent on contributions made by mononuclear cells (PBMCs and CLL cells), other accessory cells, and tissues. Since CLL patients display lower Ang1 level, we could infer that accessory cells in the CLL microenvironment, which normally secrete Ang1 and maintain quiescent Ang-Tie2 signalling, or CLL themselves, have lost their Ang1 secretion ability. Since increased expression of Ang2 [28] is associated with changes in the Ang2 promoter methylation pattern [8], a similar scenario could explain the lower Ang1 levels detected in CLL samples. Further research is necessary to identify the specific cell populations with compromised Ang1-expressing capabilities in the CLL microenvironments.
In the BM, LN, and spleen CLL microenvironments, CLL cells allegedly recirculate between peripheral blood and tissue compartments, dynamically interacting with healthy lymphocytes, accessory cells [39], surrounding tissues, and other CLL cells. Niches in BM have a perivascular localization, adjacent to blood vessels, and located in close proximity to trabecular bone [40]. Haematopoietic stem cells (HSC) are often observed in transit or migrating through vascular barriers [40] supporting the idea that CLL cells may similarly recirculate and transiently reach a perivascular position to benefit from a fast and efficient exchange of nutrients with blood capillaries, a cellular behaviour denominated as co-option [41]. Our migration assays demonstrate that CLL cells are capable of undergoing angiopoietin-mediated chemotaxis and transendothelial-like migration by traveling towards areas of high Ang1 concentration.
We show here that upon Ang2 stimulation, there is transient and concomitant expression of VE-PTP at the mRNA level (Fig. 5) 30 min post stimulation, which disappears within hours. VE-PTP binding to Tie2 prevents downstream signalling events and the disassociation of VE-PTP from Tie2 negatively affects EC proliferation and compromises vascular remodelling [23]. This emphasises the important function of VE-PTP in balancing Tie2 activity [23]. Observing a transient and concomitant expression of both Tie2 and VE-PTP upon Ang2 exposure in CLL cells is intriguing. We suspect that this transient expression could be present in only a small sub-clonal population of CLL cells, inducing a transiently active Ang-Tie2 pathway only in some of the CLL cells as a strategy to promote proliferation, survival, and evasion from efficient immunological elimination.
The Tie1 receptor is essential in angiogenesis processes during embryogenesis and development and is mainly expressed by ECs and hematopoietic lineage cells [42]. Its expression correlates with Rai stages and becomes a predictor of an aggressive disease course and a marker of shorter survival in CLL patients [29]. Besides presenting high Ang2 plasma levels, CLL patients also display increased Tie2-expressing monocytes (TEMs) counts in peripheral blood, which strongly associates with a high-risk cytogenetic profile, such as 17p deletion [36]. Apparently, Ang2 induces a homing-like effect on TEMs [32] and Ang1 stimulation triggers aggregation of Tie-2 expressing cells by Tie2-dependent trans-association at cell-cell contacts in a bridge-like manner [43]. Since the Tie1-Tie2 association has an inhibitory character [11], we could infer that Tie1-positive CLL cells interact and associate with Tie2-expressing cells in the microenvironment, such as ECs and TEMs (Fig. 10a). The direct interaction of CLL-Tie1-positive with Tie2-positive cells in the microenvironment is a putative strategy for the regulation of Ang-Tie2 signalling, since interaction of Tie-Tie2 is inhibitory and only Ang1 is capable of inducing its disassociation (Fig. 10b). Under high Ang2 concentration, the inhibitor Tie1-Tie2 complex possibly remains stable, not only preventing Ang1 from dissuading this complex (Fig. 10c), which may compromise the constitutively active Ang-Tie2 activity on ECs, but also leading to instability of the EC layer and affecting permeability and perfusion (Fig. 10c).
Interaction of Tie1-expressing CLL cells with ECs and TEMs. a Tie1-expressing CLL cells adhere to Tie2-expressing cells such as ECs and TEMs, supporting a Tie1-Tie2 inhibitory complex. b Exposure to Ang1 (Green), dissuades Tie1-Tie2 complex in resulting in activation Ang-Tie2 signalling in Tie2-expressing cells. b Under Ang2 (red) exposure, are the Ang-Tie2 inhibitory complex remains stable and Ang2 binds to the active site of Tie2 preventing Ang1 binding
Cancer cells impair energy homeostasis of healthy tissues and cells in the microenvironment, allowing tumour cells to acquire protective and pro-survival characteristics [44]. Mitochondrial functions, such ATP production, strongly regulate metabolism, apoptosis, necrosis, autophagy, cell migration, gene expression, and cell differentiation [45]. Even in the presence of oxygen, most cancers, including CLL, rely on glycolysis as the main energy-generating pathway (i.e. the Warburg effect) and as a source of building blocks for proteins, nucleotides, and lipids [44]. In models of porcine acute myocardial infarction, the concomitant expression VEGF and Ang1 correlates with neovascularization, reduced caspase-3, and reduced apoptosis [46]. Furthermore, Ang1 promotes survival of human skeletal myocytes (HSM) and freshly isolated rat neonatal cardiac myocytes (NCM) and prevents taxol-induced apoptosis (caspase-3) [47]. In our assays, both angiopoietins reduce the content of caspase, but only Ang1 offers a clear survival advantage to CLL cells. It interesting to observe that whilst Ang2 appears to reduce the survival advantage of CLL cells in culture (Fig. 3b) it also triggers a reduction of caspase content (Fig. 8b). A plausible explanation for this is that Ang2 exposure may activate a pro-survival mechanism in CLL cells to reduce caspase activity in an effort either to restore the fitness of the cell or to lessen pro-apoptotic signalling. In addition, it is possible to infer that Ang2 activates alternative pro-apoptotic pathways that cannot be rescued or blocked by reducing caspase activity, hence the decrease in both survival advantage and caspase activity. The unchanged ATP and caspase levels in the PBMC population upon exposure to Ang1, Ang2, and trebananib indicates that, unlike CLL cells, healthy PBMCs possess a strong mechanism to compensate bioenergetics stresses.
In our assays, we employed trebananib as a blocker of constitutively secreted and recombinant angiopoietins. Trebananib is an anti-angiogenic cancer drug that specifically binds Ang1 and Ang2 preventing interaction with target receptors [48], resulting in the inhibition and reversion of EC proliferation and tumour growth [49]. By exposing CLL cells to trebananib, we detect a detrimental effect on CLL survival advantage (Fig. 3c) and a successful inhibition of Ang1-mediated migration (Fig. 7). Furthermore, trebananib exposure induces an increase in caspase relative content (Fig. 8c), which indicates a putative cytotoxic effect of trebananib on leukemic lymphocytes. Trebananib exposure also influences the relative ATP content (Fig. 9c), suggesting that blocking endogenously expressed angiopoietins from interacting with CLL cells is detrimental to their survival.
CLL cells from peripheral blood lack Tie2 receptors, yet react to Ang1 and Ang2 exposure resulting in changes of mRNA expression of Ang1, Ang2, and Tie1 (Fig. 4), strongly suggesting that angiopoietins recognize alternate receptors expressed by CLL cells other than Tie2. Integrins putatively recognize angiopoietins [19] and research indicates that Ang1 binds to integrins inducing cell adhesion [35]. Employing different myocyte cell lines, which lack Tie2, Dallabrida et al. demonstrate that Ang1 and Ang2, together with laminin, fibronectin, vitronectin, and collagen-I, -III, and –IV, induce cell adhesion [47]. In addition, Ang1 also induces EC spread, adherence, and migration, an effect apparently ablated by Ang2 [35]. Further biochemical evidence is necessary to accurately identify the alternate binding partners to Ang1 and Ang2 on CLL cells and to tease out the molecular pathways they modulate, which regulate survival, migration, and metabolism in a Tie2-independent fashion in these malignant lymphocytes.
Conclusion
Our report shows that Ang1 and Ang2 dynamically modulate essential physiological aspects of CLL cells, such as survival and migration. Besides detecting a significant downregulation of Ang1 in plasma of CLL patients, we also observed that CLL cells in culture secrete significant lower levels of Ang1 when compared to healthy PBMCs. Detection of survival advantage in the long-term suggests that early interaction of Ang1 and Ang2 with CLL cells triggers signal transduction events that regulate survival in a Tie2-independent manner. Furthermore, interaction with angiopoietins, particularly Ang2, induces notable modulation of Tie1 expression on CLL cells. Chemotaxis and transendothelial-like migration assays demonstrate the activity of Ang1 in mediating CLL cell migration. Using trebananib to block the interaction of constitutively secreted and recombinant angiopoietins demonstrates the efficacy of this agent as an angiopoietin blocker. Regardless of their Tie2 deficiency, stimulation with angiopoietin modulates the relative expression of Ang1, Ang2, and Tie1 mRNA in CLL cells. The transient and concomitant expression of Tie2 and VE-PTP under the influence of Ang2 indicates that CLL cells putatively benefit from a fully functional Ang-Tie2 system, yet we are far from fully understanding the implications of this observation. To our knowledge, this is the first time that a report describes a link between CLL cells from the peripheral blood and expression of Tie2 and VE-PTP. In addition, angiopoietin exposure induces changes in the relative content of caspases and ATP, showing Ang1 and Ang2 present in microenvironment impact the metabolic fitness of leukemic lymphocytes. Since CLL cells lack Tie2 receptors, these cells become a suitable model for CLL researchers to understand the alternative molecular mechanism that angiopoietins activate. Together, our results highlight the relevance of ligands and receptors comprising the Ang-Tie2 angiogenesis pathway in CLL pathophysiology.
Abbreviations
- Ang1/Ang2:
-
Angiopoetin-1 and angiopoietin -2
- bFGF:
-
Basic fibroblast growth factor
- CLL:
-
Chronic lymphocytic leukaemia
- PBMC:
-
Peripheral blood mononuclear cells
- Tie1/Tie2:
-
Tyrosine kinase with immunoglobulin and endothelial growth factor domain-1 and -2
- VEGF:
-
Vascular endothelia growth factor
- VE-PTP:
-
Vascular endothelial-protein tyrosine phosphatase
References
Folkman J (2001) Angiogenesis. In: Brenner S, Miller JH (eds) Encyclopedia of genetics. Academic, New York, pp 66–73
Kay NE, Bone ND, Tschumper RC et al (2002) B-CLL cells are capable of synthesis and secretion of both pro- and anti-angiogenic molecules. Leukemia 16(5):911–919
Hallek M (2013) Chronic lymphocytic leukemia: 2013 update on diagnosis, risk stratification and treatment. Am J Hematol 88(9):803–816
Mauro FR, Foa R, Giannarelli D et al (1999) Clinical characteristics and outcome of young chronic lymphocytic leukemia patients: a single institution study of 204 cases. Blood 94(2):448–454
Peterson L, Kini AR, Kay N (2001) Angiogenesis is increased in B-cell chronic lymphocytic leukemia. Blood 97(8):2529–2530
Maffei R, Martinelli S, Santachiara R et al (2010) Angiopoietin-2 plasma dosage predicts time to first treatment and overall survival in chronic lymphocytic leukemia. Blood 116(4):584–592
Maffei R, Martinelli S, Castelli I et al (2010) Increased angiogenesis induced by chronic lymphocytic leukemia B cells is mediated by leukemia-derived Ang2 and VEGF. Leuk Res 34(3):312–321
Martinelli S, Kanduri M, Maffei R et al (2013) ANGPT2 promoter methylation is strongly associated with gene expression and prognosis in chronic lymphocytic leukemia. Epigenetics 8(7)
Aguayo A, Kantarjian H, Manshouri T et al (2000) Angiogenesis in acute and chronic leukemias and myelodysplastic syndromes. Blood 96(6):2240–2245
Augustin HG, Young Koh G, Thurston G, Alitalo K (2009) Control of vascular morphogenesis and homeostasis through the angiopoietin–Tie system. Nat Rev Mol Cell Biol 10(3):165–177
Seegar TCM, Eller B, Tzvetkova-Robev D et al (2010) Tie1-Tie2 interactions mediate functional differences between angiopoietin ligands. Mol Cell 37(5):643–655
Papapetropoulos A, García-Cardeña G, Dengler TJ, Maisonpierre PC, Yancopoulos GD, Sessa WC (1999) Direct actions of Angiopoietin-1 on human endothelium: evidence for network stabilization, cell survival, and interaction with other angiogenic growth factors. Lab Invest J Tech Methods Pathol 79(2):213–223
Jeansson M, Gawlik A, Anderson G et al (2011) Angiopoietin-1 is essential in mouse vasculature during development and in response to injury. J Clin Invest 121(6):2278–2289
Huang H, Bhat A, Woodnutt G, Lappe R (2010) Targeting the ANGPT–TIE2 pathway in malignancy. Nat Rev Cancer 10(8):575–585
Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J (2000) Vascular-specific growth factors and blood vessel formation. Nature 407(6801):242–248
Kawaguchi M, Sugaya M, Suga H et al (2013) Serum levels of Angiopoietin-2, but not Angiopoietin-1, are Elevated in Patients with Erythrodermic Cutaneous T-cell Lymphoma. Acta Derm Venereol
Moss A (2013) The angiopoietin:Tie 2 interaction: a potential target for future therapies in human vascular disease. Cytokine Growth Factor Rev
Maisonpierre PC, Suri C, Jones PF et al (1997) Angiopoietin-2, a natural antagonist for Tie2 that disrupts in vivo angiogenesis. Science 277(5322):55–60
Barton WA, Tzvetkova-Robev D, Miranda EP et al (2006) Crystal structures of the Tie2 receptor ectodomain and the angiopoietin-2–Tie2 complex. Nat Struct Mol Biol 13(6):524–532
Reiss Y, Droste J, Heil M et al (2007) Angiopoietin-2 impairs revascularization after limb ischemia. Circ Res 101(1):88–96
Barton WA, Tzvetkova D, Nikolov DB (2005) Structure of the Angiopoietin-2 receptor binding domain and identification of surfaces involved in Tie2 recognition. Structure 13(5):825–832
Yu X, Seegar TCM, Dalton AC et al (2013) Structural basis for Angiopoietin-1–mediated signaling initiation. Proc Natl Acad Sci 110(18):7205–7210
Winderlich M, Keller L, Cagna G et al (2009) VE-PTP controls blood vessel development by balancing Tie-2 activity. J Cell Biol 185(4):657–671
Fachinger G, Deutsch U, Risau W (1999) Functional interaction of vascular endothelial-protein-tyrosine phosphatase with the angiopoietin receptor Tie-2. Oncogene 18(43):5948–5953
Nawroth R, Poell G, Ranft A et al (2002) VE-PTP and VE-cadherin ectodomains interact to facilitate regulation of phosphorylation and cell contacts. EMBO J 21(18):4885–4895
Shen J, Frye M, Lee BL et al (2014) Targeting VE-PTP activates TIE2 and stabilizes the ocular vasculature. J Clin Invest 124(10):4564–4576
Nottebaum AF, Cagna G, Winderlich M et al (2008) VE-PTP maintains the endothelial barrier via plakoglobin and becomes dissociated from VE-cadherin by leukocytes and by VEGF. J Exp Med 205(12):2929–2945
Martinelli S, Maffei R, Castelli I et al (2008) Increased expression of Angiopoietin-2 characterizes early B-cell chronic lymphocytic leukemia with poor prognosis. Leuk Res 32(4):593–597
Aguayo A, Manshouri T, O’Brien S et al (2001) Clinical relevance of Flt1 and Tie1 angiogenesis receptors expression in B-cell chronic lymphocytic leukemia (CLL). Leuk Res 25(4):279–285
Kay NE, Hamblin TJ, Jelinek DF et al (2002) Chronic lymphocytic leukemia. ASH Educ Program Book 2002(1):193–213
Parikh SA, Kay NE, Shanafelt TD (2013) Monoclonal B-cell lymphocytosis: update on diagnosis, clinical outcome, and counseling. Clin Adv Hematol Oncol 11(11):720–729
Venneri MA, Palma MD, Ponzoni M et al (2007) Identification of proangiogenic TIE2-expressing monocytes (TEMs) in human peripheral blood and cancer. Blood 109(12):5276–5285
Goon PKY, Lip GYH, Boos CJ, Stonelake PS, Blann AD (2006) Circulating endothelial cells, endothelial progenitor cells, and endothelial microparticles in cancer. Neoplasia 8(2):79–88
Horner A, Bord S, Kelsall AW, Coleman N, Compston JE (2001) Tie2 ligands Angiopoietin-1 and Angiopoietin-2 are coexpressed with vascular endothelial cell growth factor in growing human bone. Bone 28(1):65–71
Carlson TR, Feng Y, Maisonpierre PC, Mrksich M, Morla AO (2001) Direct cell adhesion to the angiopoietins mediated by integrins. J Biol Chem 276(28):26516–26525
Maffei R, Bulgarelli J, Fiorcari S et al (2013) The monocytic population in chronic lymphocytic leukemia shows altered composition and deregulation of genes involved in phagocytosis and inflammation. Haematologica 98(7):1115–1123
Stapor PC, Sweat RS, Dashti DC, Betancourt AM, Murfee WL (2014) Pericyte dynamics during angiogenesis: new insights from new identities. J Vasc Res 51(3):163–174
Cao Y, Sonveaux P, Liu S et al (2007) Systemic overexpression of Angiopoietin-2 promotes tumor microvessel regression and inhibits angiogenesis and tumor growth. Cancer Res 67(8):3835–3844
ten Hacken E, Burger JA (2014) Molecular pathways: targeting the microenvironment in chronic lymphocytic leukemia—focus on the B-cell receptor. Clin Cancer Res 20(3):548–556
Morrison SJ, Scadden DT (2014) The bone marrow niche for haematopoietic stem cells. Nature 505(7483):327–334
Eikesdal HP, Kalluri R (2009) Drug resistance associated with antiangiogenesis therapy. Semin Cancer Biol 19(5):310–317
Woo KV, Baldwin HS (2011) Role of Tie1 in shear stress and atherosclerosis. Trends Cardiovasc Med 21(4):118–123
Fukuhara S, Sako K, Minami T et al (2008) Differential function of Tie2 at cell–cell contacts and cell–substratum contacts regulated by Angiopoietin-1. Nat Cell Biol 10(5):513–526
Prezma T, Shteinfer A, Admoni L et al (2013) VDAC1-based peptides: novel pro-apoptotic agents and potential therapeutics for B-cell chronic lymphocytic leukemia. Cell Death Dis 4(9), e809
Kasahara A, Scorrano L (2014) Mitochondria: from cell death executioners to regulators of cell differentiation. Trends Cell Biol
Tao Z, Chen B, Tan X et al (2011) Coexpression of VEGF and Angiopoietin-1 promotes angiogenesis and cardiomyocyte proliferation reduces apoptosis in porcine myocardial infarction (MI) heart. Proc Natl Acad Sci 108(5):2064–2069
Dallabrida SM, Ismail N, Oberle JR, Himes BE, Rupnick MA (2005) Angiopoietin-1 promotes cardiac and skeletal myocyte survival through integrins. Circ Res 96(4):e8–e24
Coxon A, Bready J, Min H et al (2010) Context-dependent role of Angiopoietin-1 inhibition in the suppression of angiogenesis and tumor growth: implications for AMG 386, an Angiopoietin-1/2-neutralizing peptibody. Mol Cancer Ther 9(10):2641–2651
Herbst RS, Hong D, Chap L et al (2009) Safety, pharmacokinetics, and antitumor activity of AMG 386, a selective angiopoietin inhibitor, in adult patients with advanced solid tumors. J Clin Oncol 27(21):3557–3565
Acknowledgments
We would like to thank Keri Elizabeth Parsons Mattaliano, MLIS, for kindly revising the manuscript. We would like to thank Thomas Landwehr and Lukas Heukamp from the biobank, Center for Integrated Oncology, for their kind support in providing CLL specimens.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflicts of interest. In addition, the authors declare that they have no disclosures to make.
Funding
This work was made possible by a grant (No. 2011.101.02) from to the Wilhelm Sander-Foundation, Munich, Germany.
Rights and permissions
About this article
Cite this article
Aguirre Palma, L., Flamme, H., Gerke, I. et al. Angiopoietins Modulate Survival, Migration, and the Components of the Ang-Tie2 Pathway of Chronic Lymphocytic Leukaemia (CLL) Cells In Vitro. Cancer Microenvironment 9, 13–26 (2016). https://doi.org/10.1007/s12307-016-0180-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12307-016-0180-7