Abstract
Purpose
To assess the technical success of GoBack™ crossing catheter in chronic total occlusion.
Materials and Methods
A retrospective review of chronic limb threatening ischemia (CLTI) patients treated for chronic total occlusions (CTO) with the application of the GoBack™ crossing catheter (Upstream Peripheral Technologies, Haifa, Israel) between May 2020 and January 2021 was performed. Sixteen GoBack catheters were applied in twelve limbs in 12 patients (ten men, average age 75.7 years). Treated limbs were classified as Rutherford Category 5 and 6 in ten patients and four in two patients. Average occlusion length was 287 mm (62–466). All occluded arteries were heavily calcified. Technical success was defined as successful application of the GoBack catheter for lesion crossing or luminal reentry.
Results
Successful application of the four French catheter was achieved in 11 of the 12 cases (92%) for reentry in external iliac (1), superficial femoral (2), popliteal (2) and posterior tibial (1) arteries in six out of six cases (100%) and lesion crossing in popliteal (4), peroneal (1) and posterior tibial arteries in five out of six cases (83%). The 2.9 Fr catheter was successfully applied once out of four (25%) in lesion crossing in the posterior tibial artery.
Conclusion
The GoBack™ 4 Fr crossing catheter in revascularization of CLI patients with CTO could be valuable when manual crossing or reentry is unsuccessful and is applicable from any access site.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The endovascular treatment of patients with chronic limb threatening ischemia (CLTI) has evolved dramatically in the recent years due to advances in endovascular techniques and equipment [1, 2]. Subintimal angioplasty of chronic total occlusions (CTOs) of the femoropopliteal segment is an accepted method to achieve recanalization in cases of failure of the endoluminal approach [3]. Due to the risk of distal extension of the dissection or interruption of collateral flow [4, 5] reentering devices were created and is used in some 12.2% of patients treated for CTO's [6]. The GoBack™ crossing catheter (Upstream Peripheral Technologies, Caesarea, Israel) is a new FDA and CE approved device consisting of a metal shaft and a retractable curved needle that allows crossing occluded segments. Contrary to existing devices [6], this device offers both endoluminal crossing and reentry capabilities, through which the wire is advanced to the distal true lumen. The operator can control the needle curvature by the degree of needle protrusion. The device has two sizes, each has two lengthens of 80 cm and 120 cm. The 4 Fr over 0.018" guidewire is dedicated for arteries larger than 3 mm and the 2.9 Fr over 0.014" guidewire for non-calcified, larger than 2 mm tibial arteries. The 4Fr device has three needle protrusion lengths, and the 2 Fr has 2 lengths. Together with the needle curve control and the metal shaft, there is excellent torque control and pushabilty (Fig. 1).
The purpose of this study is to report our early experience with the GoBack™ crossing catheter for treating CTOs in patients with CLTI.
Materials and Methods
This study was conducted under Institutional Review Board approval.
Patient Selection
The data were retrospectively evaluated with the aid of the hospital's radiology information system (RIS), picture archiving and communication system (PACS), HI-IQ dedicated interventional software (Lincoln, RI, USA) and an electronic medical records system (Chameleon, Elad Group, Israel). A retrospective review of CLTI patients who underwent arterial revascularization of limb and pelvic vasculature between May 2020 and January 2021 was conducted. During this time a total of 196 endovascular procedures were performed on CLI patients due to CTO of the affected limb. Most recanalization were performed with the conventional catheter and wire technique. When this technique was unsuccessful, the GoBack™ crossing catheters were applied. Age, gender, Rutherford and TASC classification, vascular access site (ipsilateral and contralateral femoral and retrograde via anterior tibial artery) were recorded alongside occlusion length and ankle-brachial index (ABI) prior to and after the procedure. TASC classification score was graded by using computerized tomography angiography (CTA) coronal reconstruction and assigned for both the treated arteries and reentry site. Calcification was assessed by two readers based on the angiographic images, where one reader was the operator and the other was not involved in the procedure. The extent of calcification was based on a score which published previously [7]. In case of disagreement, a consensus was reached. Arterial calcification were graded as follows: grade 0—none, grade 1—mild, grade 2—moderate and grade 3—severe.
Technical Procedure
All treated patients underwent a diagnostic preprocedural CTA. Based on this study, the access site was chosen according to patient's habitus, arterial tree patency and potential access site calcification. All procedures were performed in a dedicated angiography suite (Axiom Artis Zee, Siemens Healthcare, Germany) by a single interventional radiologist who performs primarily endovascular procedures. Following arterial access with 6 Fr vascular sheath (Terumo Europe, Leuven, Belgium), intravenous Heparin (Rotexmedica, Trittau, Germany) was administered to achieve activated clotting time values between 250 and 300 s.
In patients with ipsilateral antegrade access, a short 10 cm 6 Fr sheath was used. In patients with contralateral retrograde approach, the short sheath was exchanged to a curved 45 cm 6 Fr Destination sheath (Terumo Europe, Leuven, Belgium) over the aortic bifurcation. In patients treated via anterior tibial artery, access was gained with a 21 g echogenic tip needle, an 0.018" guidewire and a 3 Fr inner dilator of a micropunctur e set (Angiodynamics, Queensbury, NY, USA). The dilator was then exchanged over a 0.018" 300 cm Advantage wire (Terumo Europe, Leuven, Belgium) for a 3 Fr 150 cm Trailblazer Support Catheter (EV3 Inc, Plymouth, MN, USA), which was then advanced to the occlusion site. Intra-arterial vasodilators, such as verapamil or nitroglycerin, were not used. Regardless of the access, once the occlusion was reached, recanalization was attempted, either luminal or subintimal, using the 3 Fr TrailBlazer™ support catheter and 0.018 Advantage guidewire (Terumo Europe, Leuven, Belgium).
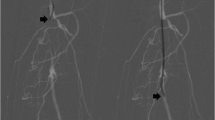
If crossing or reentry into the true lumen was not successful with these conventional maneuvers, a GoBack™ crossing catheter was advanced over the wire into the subintimal space or toward the part of the occlusion through which crossing was to be attempted. The needle was subsequently deployed and the guide wire was advanced into the post occlusion true lumen (Fig. 2a–d). The catheter was then removed. Balloon angioplasty (PTA) was routinely performed with the PowerCross™ 0.018" (ev3 Inc, Plymouth, MN, USA) balloon (chosen in accordance with the arterial diameter). Control angiography was performed to evaluate vascular patency. If it was deemed necessary, stent placement was performed with self-expandable stents, either Supera® (Abbott Vascular, Santa Clara, CA, USA), Complete SE (Medtronic, Minneapolis, MN, USA) or balloon-expandable Biotronik AG (Biotronik, Bülach, Switzerland). Procedural success was defined as recanalization of the occluded artery with residual stenosis less than 30% and improvement in ABI of at least 0.2 after 24 h. Technical success was defined as successful CTO recanalization by occlusion crossing or luminal reentry via the application of GoBack catheter and a patent treated artery on the completion angiogram.
Patient treated via tibial access due to previous surgical intervention to the common femoral artery. a GoBack catheter is placed at the subintimal space at the level of common femoral artery with the catheters tip (white arrow) oriented toward the lumen marked by the radiopaque marker (arrow). b Protrusion of the needle tip (arrow). c Introduction of 0.018" guidewire into the lumen via the needle. d Proximal advancement of the wire to the external iliac artery (arrow)
Results
Twelve limbs in 12 patients were treated (ten men, mean age 75.7 years (range 62–89 years)) with application of 16 GoBack™ crossing catheters. Six patients presented with Category 6 (Grade IV), four with Category 5 (Grade III) and two with Rutherford Category 4 (Grade II). All lesions were classified as TASC II class D (Table 1).
Technical success was achieved in all patients.
Average ABI improved from 0.34 prior to the endovascular procedure to 0.97 after the procedure. Access site for five procedures were ipsilateral femoral, four contralateral femoral and three retrograde via anterior tibial artery as a single access. Occluded arteries included four posterior tibial, one peroneal, five popliteal, eight superficial femoral, one common femoral and one external iliac arteries. Average occluded segment length was 287 mm (range 62–466). Both the treated arteries and reentry site arterial segment were graded 3—severely calcified (Table 2).
The 2.9 Fr catheter was used three times for occlusion crossing and once for reentry. It was applied in one peroneal and three posterior tibial arteries. Successful application was in only one out of four (25%) in the crossing attempt in the posterior tibial artery.
The 4 Fr catheter was used in 12 cases, six times for occlusion crossing and six time for reentry. It was applied six times in the popliteal, twice in the posterior tibial and superficial femoral, and once in peroneal and external iliac arteries. Successful application was achieved in 11 of the 12 patients (92%) for reentry in 6/6 (100%) and lesion crossing in 5/6 (83%).
In the single case with failed crossing at the popliteal artery with the 4 Fr catheter, additional access was done via the anterior tibial artery and crossing of the occlusion was done via the SAFARI technique [8]. The procedure was successful.
In the three failed cases with the 2.9 Fr catheter neither crossing nor reentry was successful due to heavy calcification of the tibial arteries. In these cases, the 4 Fr catheter was successfully applied.
On a few occasions, after crossing the heavily calcified lesion with a guidewire, no catheter could cross the lesion, so the calcified occlusion was off-labeled macerated with the needle in different directions which eventually allowed the balloon to cross the stubborn occlusion. This was done solely with the 4 Fr catheter.
Discussion
This study evaluates the feasibility and safety of the GoBack™ crossing catheter in severe arterial calcified occlusions in CLI patients with uncrossable lesions with the conventional 3F support catheter and 0.018" wire. This device assists the operator to directly cross the occlusion or indirectly by intraluminal reentry technique. Off-labeled it can be used for calcified occluded lesion maceration, helping crossing "stubborn" occlusions.
Advances in endovascular techniques and equipment, treatment of femoropopliteal lesions of TASC C and D has become feasible [1, 9,10,11] and are changing the vascular surgery field from extra-anatomic surgical bypasses to endovascular recanalization [bisdas]. This progress presents a challenge for endovascular treatment of long and calcified lesions. One approach in treatment CTO is the intentional dissection of the arterial wall using the loop technique [3]. The chances of a successful return of the wire into the true lumen are high [8, 12]. Failure to gain reentry to the true lumen result in procedural failure. In order to achieve a better reentry success rate, reentry devices were developed [8]. Those devices are stiff and have one angle needle [5].
The GoBack crossing catheter is a new novel device which its application has not been yet studied extensively. In contrast to reentry devices, it has a smaller shaft; it is relatively flexible compared to other available reentry devices and can be used to either cross the lumen directly or as a reentry device with its different needle angulation. We used it with different access sites including retrograde femoral contralateral over the aortic bifurcation, retrograde pedal access and antegrade femoral unilateral, without any problem to reach the occluded target artery of different sizes. We also used it off-labeled, as macerator for uncrossable calcified lesions. The results were better with the 4 Fr device, 92% success, which we used for all leg arteries, including the tibial arteries. The 2.9 Fr device is fine and cannot accommodate calcified occlusion. Our success rate with it was only 25%, so its application is less favorable (Table 3).
This study is limited by the small, selected, patient group from a single center and its retrospective, non-randomized nature. Moreover, all the procedures were conducted by a single operator. More experience should be gained, especially with the 2.9F device.
Conclusion
The GoBack™ 4 Fr crossing catheter in revascularization of CLI patients with CTO could be valuable when manual crossing or reentry is unsuccessful and is applicable from any access site.
References
Rabellino M, Zander T, Baldi S, et al. Clinical follow-up in endovascular treatment for TASC C-D lesions in femoro-popliteal segment. Catheter Cardiovasc Interv. 2009;73(5):701–5.
Bisdas T, Borowski M, Stavroulakis K, Torsello G, Collaborators CR. C. R. I. T. I. S. C. H. Endovascular therapy versus bypass surgery as first-line treatment strategies for critical limb ischemia: results of the interim analysis of the CRITISCH registry. JACC: Cardiovasc Interv. 2016;9(24):2557–65.
Bolia A, Miles KA, Brennan J, et al. Percutaneous transluminal angioplasty of occlusions of the femoral and popliteal arteries by subintimal dissection. Cardiovasc Intervent Radiol. 1990;13(6):357–63.
Met R, Van Lienden KP, Koelemay MJ, et al. Subintimal angioplasty for peripheral arterial occlusive disease: a systematic review. Cardiovasc Intervent Radiol. 2008;31(4):687–97.
Jacobs DL, Motaganahalli RL, Cox DE, et al. True lumen re-entry devices facilitate subintimal angioplasty and stenting of total chronic occlusions: initial report. J Vasc Surg. 2006;43(6):1291–6.
Kokkinidis DG, Katsaros I, Jonnalagadda AK, et al. Use, safety and effectiveness of subintimal angioplasty and re-entry devices for the treatment of femoropopliteal chronic total occlusions: a systematic review of 87 studies and 4,665 patients. Cardiovasc Revasc Med. 2020;21(1):34–45.
Shin SH, Baril D, Chaer R, et al. Limitations of the outback LTD re-entry device in femoropopliteal chronic total occlusions. J Vasc Surg. 2011;53(5):1260–4.
Gandini R, Pipitone V, Stefanini M, et al. The “Safari” technique to perform difficult subintimal infragenicular vessels. Cardiovasc Intervent Radiol. 2007;30(3):469–73.
Etezadi V, Benenati JF, Patel PJ, et al. The reentry catheter: a second chance for endoluminal reentry at difficult lower extremity subintimal arterial recanalizations. J Vasc Interv Radiol. 2010;21(5):730–4.
Baril DT, Chaer RA, Rhee RY, et al. Endovascular interventions for TASC II D femoropopliteal lesions. J Vasc Surg. 2010;51(6):1406–12.
Setacci C, Chisci E, De Donato G, et al. Subintimal angioplasty with the aid of a re-entry device for TASC C and D lesions of the SFA. Eur J Vasc Endovasc Surg. 2009;38(1):76–87.
Siablis D, Diamantopoulos A, Katsanos K, et al. Subintimal angioplasty of long chronic total femoropopliteal occlusions: long-term outcomes, predictors of angiographic restenosis, and role of stenting. Cardiovasc Intervent Radiol. 2012;35(3):483–90.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interests and neither received any funding.
Informed Consent
The study was approved by the institutional review board that waived informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raskin, D., Silverberg, D., Halak, M. et al. Technical Success of the GoBack™ Crossing Catheter in Chronic Total Occlusion in Patients with Chronic Limb Threatening Ischemia. Cardiovasc Intervent Radiol 45, 641–645 (2022). https://doi.org/10.1007/s00270-021-03033-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-021-03033-7