Abstract
The purpose of this study was to describe the efficacy of planned combined subintimal arterial flossing with antegrade–retrograde intervention (SAFARI) to obtain the precise recanalization of the patent portion of a distal runoff vessel in critical limb ischemia (CLI) patients presenting long occlusions involving the popliteal trifurcation. Four patients at risk of limb loss due to long occlusions involving the leg vessel tree and not suitable for a surgical bypass were treated by the subintimal antegrade and retrograde (posterior tibial or anterior tibial artery) approach. The patent portion of the runoff vessel was previously assessed by magnetic resonance angiography (MRA) and directly punctured under Doppler ultrasound (US) guidance. A subintimal channel rendezvous was performed to allow snaring of the guidewires. Subsequently, a balloon dilatation was performed without stent deployment. All patients were successfully recanalized and had complete healing of the limb lesions. At the 12-month follow-up all patients showed clinical improvement with no major complications related to the procedure. This combined antegrade and retrograde subintimal approach is currently an excellent endovascular option in patients with long occlusions extending onto the leg vessels trifurcation and at risk of limb loss.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Lower-limb ischemia is one of the most common complications in patients with long-term diabetes mellitus. It can be classified into subcritical limb ischemia (SLI), with rest pain and ankle pressure >40 mm Hg, and critical limb ischemia (CLI), with chronic rest pain, tissue loss, and/or ankle pressure <40 mm Hg [1]. In this latter group, the amputation rate is very high, with diabetics forming 40–45% of all amputees [1].
Subcritical limb ischemia patients generally respond to medical treatment alone and allow a delay of the surgical therapy. Medically treated CLI patients undergo limb amputation in 95% of cases within a year, and surgical bypass treatment often fails because they are referred to the surgeon in a late phase of their pathology when coexisting diseases, mainly cardiovascular or renal, and vessel occlusions require difficult surgical management [2].
The percutaneous endovascular recanalization approach, consisting of the intraluminal or the subintimal technique, represents a valid alternative to the surgical bypass in patients at risk of limb loss and not suitable for surgery [3–5].
The intraluminal approach consists in reaching the distal patent lumen by pushing a hydrophilic guidewire through the obstructed tract. This technique is a good option in the case of a short superficial femoral artery (SFa) obstructions, but since the first experience of Bolia et al. [6], the subintimal technique is often preferred, especially in long occlusions (>5 cm), because of the poor patency of the intraluminal revascularization [7–9].
The subintimal recanalization consists of creating a new lumen between the media and the intimal layer by advancing a guidewire until a reentry site at the distal patent tract of the vessel. However, problems are often encountered in advancing the catheter or in reentering the patent lumen in the case of long occlusions or calcified vessels. These problems have been successfully overcome by either using a stiff guidewire or entering the vessel distally [10, 11].
In the case of long occlusions with involvement of the leg trifurcation showing a single patent distal runoff vessel, the wire tends to enter the vessel and offering less resistance to the antegrade progression but not necessarily better patency [12]. Therefore, the precise and successful direct recanalization toward the patent vessel of the leg remains to date the main technical problem to overcome [13].
We applied a subintimal revascularization technique by the combined simultaneous proximal antegrade and distal retrograde approach by entering the common femoral artery (CFa) on one side and the patent leg vessel on the other side.
We present four cases of femoro-popliteal obstruction extending onto the popliteal trifurcation of the leg that were successfully treated at our department applying the above-mentioned procedure.
Materials and Methods
Patients
From September 2002 to October 2003, 104 diabetic patients, candidates for amputation, underwent limb salvage by endovascular recanalization. Four of these patients (two females, two males;mean age: 64 years; range: 61–67 years) presented with femoro-popliteal leg vessels obstruction. Two of them (patients 1 and 2) were ASA III and had a coronary bypass and two (patients 3 and 4) were ASA IV because of unstable angina.
Two of these patients were referred for endovascular recanalization because of their clinical condition (patients 3 and 4) and the other two because of the lack of venous vessels suitable to perform a surgical bypass.
-
Patient 1 was a 63-year-old male with hypercholesterolemia, a 35-year history of smoking, an 18-year history of type II diabetes mellitus, and a triple coronary by-pass performed 7 months prior to admission. Rest pain on his right leg and trophic lesions with loss of the distal phalanx of his second toe had begun 3 months prior to admission. Doppler ultrasound (US) revealed tight stenosis of the proximal tract of the SFa (VPS 310 cm/s) and obstruction at its distal third. Several calcified lesions of the arterial wall were noted along the femoro-popliteal tract, with no flow signal at the popliteal level. A typical “parvus et tardus” postobstructive flow pattern was found at the distal third of the posterior tibial artery (PTa), behind the malleolus. Moreover, feeble postocclusive flow at the distal third of the anterior tibial artery (ATa) was also noted. Magnetic resonance angiography (MRA) confirmed a 45-cm-long occlusion running from the distal third of the right SFa to the distal third of the PTa, with multiple stenoses on the SFa obstruction and collateral vessels from the profunda. The images also showed a low flow signal on the distal portion of the ATa.
-
Patient 2 was a 65-year-old male with a 40-year history of smoking, a 15-year of type II diabetes mellitus, a previous coronary bypass, and a single episode of stroke, referred to our department because of trophic lesions in his third, fourth, and fifth left toes. Doppler US revealed flow signal absence from the distal third of the SFa to the popliteal branches, showing multiple collateral vessels from the profunda. A feeble flow was noted at the ATa. Color-Doppler showed a postobstruction flow at the distal third of the PTa. The subsequent MRA confirmed the long obstruction of the femoro-popliteal axis, with involvement of the popliteal branches and refilling of the PTa at its distal portion.
-
Patient 3 was a 61-year-old female, overweight (164 cm tall, 80 kg), with a history of hypertension, end-stage renal disease (ESRD), type II diabetes mellitus, and unstable angina for 5 years, referred to our department after being conservatively treated for 3 months for her right heel ulceration. Doppler US revealed a calcified obstruction of the SFa above the knee with involvement of the popliteal branches and with refilling of the PTa at the distal third, where a feeble flow acceleration as sign of stenosis of this tract was noted. No flow signal was observed in either the ATa or the dorsalis pedis artery. MRA confirmed an 18-cm obstruction of the popliteal artery and multiple preobstructive stenosis of the PTa with normal flow at the distal third. A precocious venous signal was also noted because of distal arterial-venous shunts. No flow signal in the ATa and peroneal artery was detected.
-
Patient 4 was a 67-year-old female with unstable angina, a 12-year history of type II diabetes mellitus, 2 months of right calf and foot rest pain, and ulceration of her first and second toe. Doppler US demonstrated no flow signal extending onto the femoro-popliteal tract and the infrapopliteal vessels, with postobstructive flow in the distal portion of the ATa. Flow absence in the PTa could not be documented but was suspected. MRA confirmed the long occlusion (about 30 cm) of the femoro-popliteal axis with involvement of all three distal runoff vessels at the origin. The middle-distal portion of the ATa seemed retrogradely refilled by collateral vessels.
Technique
All patients were preprocedurally administered ticlopidine 500 mg + aspirin 100 mg for 3 days and postprocedurally treated with ticlopidine 500 mg for 6 weeks followed by Ticlopidine 250 mg + aspirin 100 mg quoad vitam.
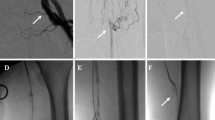
Each patient underwent a diagnostic angiography (Figs. 1 and 2) of the affected lower limb by antegrade puncture of the right CFa using the Seldinger technique and a 6F, 25-cm Terumo vascular sheath. A combined antegrade and retrograde subintimal recanalization was subsequently planned. The occluded tract of the SFa to the popliteal artery above the knee was recanalized by subintimal antegrade dissection as described by Bolia et al. [6], using a 180-cm, 0.035-in. Terumo stiff guidewire (Boston Scientific, Natick, MA) and a 5F Van Handel catheter (Cook, Bloomington, IN). The technique we used has been recently described by Spinosa et al. [14] and named “subintimal arterial flossing with antegrade-retrograde intervention (SAFARI).” Room for the subsequent snaring at the popliteal level was created by PTA advanced into the SFa (Fig. 3a).The percutaneous retrograde dissection of the best distal runoff vessel from the ankle mortise to the popliteal tract was then performed to obtain the most effective revascularization (Fig. 3b).
Antegrade subintimal recanalization and dilation at 6 mm of the femoro-popliteal tract (A) in order to create room for the subsequent snaring of the 0.035-in. guidewire advanced from the retrograde transposterior tibial approach. Retrograde road mapping performed to follow the progression of the catheter (B ).
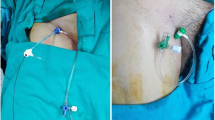
The target vessel was punctured using a 20-gauge needle under Doppler guidance and a 0.018-in. guidewire was retrogradely advanced in the patent vessel. After removing the needle, the external and internal cannula of the micropuncture system (Cook) was advanced over the guidewire. Then the internal cannula and guidewire were gently removed and a Terumo 0.035-in. guidewire was advanced into the external cannula, which was subsequently substituted by a 4F short Terumo sheath.
Retrograde subintimal dissection was started by gently pushing a 4F, 100-cm beacon tip catheter (Cook) over a 260-cm Glidewire, until the antegrade dissection in the popliteal artery was reached. After subintimal rendezvous, obtained by advancement of the distal Glidewire into a 25-mm-diameter Snare-Loop device inserted into the subintimal space from the antegrade access, the 260-cm, 0.035-in. Terumo Glidewire was pulled out of the transfemoral long sheath (Fig. 4a). Subsequently, the beacon tip catheter was retrieved and readvanced into the patent distal vessel mounted on the floppy tip of the wire. The beacon tip catheter, because of its hard and angled distal tip, permitted one to punch a hole in the intima, to start the recanalization, to reduce the guidewire loop, and to keep it within a size unable to damage the vessel. Therefore, after exchanging the guidewire with a 300-cm, 0.014-in. Choice (Boston Scientific) metallic wire, the subintimal angioplasty of the PTa and tibio-peroneal trunk or of the ATa was performed, distally to proximally, by inflating a (2.5–3.5)-mm × 100/120-mm over-the-wire balloon catheter (Symmetry, Boston Scientific; Bard, Tempe, AZ) (Fig. 4b). The SFa and the popliteal artery were subintimally dilated between 5 and 6 mm using a 0.035-in. over-the-wire balloons (Wanda, Boston Scientific). After the entire reconstitution of the femoro-popliteal and PTa or ATa tract, we attempted the subintimal recanalization and angioplasty of other occluded vessels (patient 1), carefully inflating the balloon without damaging the tibio-peroneal trunk at the origin and, consequently, obstructing the previously recanalized vessel.
The balloon advancement encountered resistance in the subintimal channel; therefore, the guidewire had to be kept in tension at the femoral and malleolar level by two operators to ease the progression of the balloon. At the level of the femoro-popliteal obstruction, the guidewire loop was maintained sufficiently large to create a subintimal pocket rather than just a subintimal canal and then an intraprocedural dilation of 5–6 mm was performed to reduce the resistance of the guidewire and to create room for the snaring of the guidewire advanced retrogradely. All interventional procedures were performed after intra-arterial injection of a bolus of 5000 U/L heparin and with frequent flushing of the sheaths with heparinized saline.
Intraprocedural and postprocedural angiographic studies (Fig. 4c) were performed with simultaneous aspiration by the 4F sheath at the ankle mortise-dorsalis pedis, thus avoiding a false stop-flow effect as a result of occlusive position of the sheath into these small arteries.
Results
Patient 1
The entire femoro-popliteal tract was recanalized, with optimal reestablishment of patency along the tibio-peroneal trunk and the PTa. Recanalization of the ATa was subsequently attempted and a good flow was detected immediately after the procedure, but the artery appeared occluded at the 1-month follow-up. At the 1-, 3-, 6-, and 12-month Doppler US follow-ups, the femoro-popliteal tract showed a 50% stenosis in the middle portion of the SFa.
The PTa demonstrated a good flow, but with diastolic flow-wave hypertrophy and absence of postsystolic flow inversion resulting from artero-venous shunts patency and peripheral vessels sclerosis, respectively. The ATa was patent at its origin, but a postobstructive flow was noted at its distal portion.
The patient showed total healing of the lesions at 4 months.
Patient 2
The obstructed tract of the PTa had good recanalization with unmodified findings at the 1-, 6-, and 12-month Doppler US follow-ups, showing a wall irregularity at the proximal end of the subintimal channel of no hemodynamic significance.
Rest pain disappeared shortly after the procedure and toes were healed at 3 months.
Patient 3
The PTa had optimal flow at the 1-, 6-, and 12-month Doppler US follow-ups, showing peak systolic velocity of 50 cm/s but lacking the typical morphology of the flow wave. The patient did not undergo amputation and showed healing of her heel ulcer.
Patient 4
No pathologic findings were noted at the 1-, 6-, and 12-month Doppler US follow-ups. There was evidence of parietal irregularity at the proximal and distal ends of the subintimal channel without hemodynamic irregularities of the vessel cavity. The patient experienced a disappearance of ischemic symptoms and healing of his ulcers at 3 months. No evidence of other foot ulceration or onset of rest pain at a 12-month clinical examination was found.
Discussion
In the medium term, the outcome after bypass surgery or angioplasty is comparable. In the short term, however, surgery is associated with a higher rate of morbidity [5]. This is because of the frequent presence of comorbidities at the time of intervention, occlusions extending below the knee, and limb tissue loss [1, 15]. In addition, many of these patients often already had previous bypasses because of the characteristic multiregional location of the atherosclerotic pathology, therefore hampering the use of leg veins as grafts for long femoro-tibial bypasses.
Percutaneous angioplasty, because of the progress of the intraluminal and the extraluminal techniques and the availability of new materials, has demonstrated great efficacy in the treatment of CLI in terms of success rate, clinical outcome, and procedure-related complications [4, 5, 16].
In CLI, the aim of the treatment is to avoid limb loss, trying to obtain an optimal clinical patency (relief of symptoms, lesions healing) even if without a stable main vessel patency. The intraluminal recanalization in the treatment of a femoral occlusion longer than 5 cm is poor (45–55% at 12–24 months) [17–19], compared with the vein graft patency of 82% at 1 year [9] or 66–81% at 5 years [19–22]. The subintimal procedure is therefore preferable. However, as previously reported [3], the subintimal recanalization alone is associated with a high percentage of technical failure (13–24%) that too often leads to amputation and death. The first cause of failure is the difficulty to precisely guide the dissection into the best distal runoff vessel. In fact, the guidewire–catheter because of the obstruction of the trifurcation tends to proceed into the straighter pathway, thus risking to damage the ostium of the previously assessed runoff artery.
A second cause of failure in long transfemoral extraluminal recanalization is both the intense force necessary for the progression of the guidewire–catheter system and the related difficulty in modeling the loop formed in the femoral artery to reenter the lumen. Because of these potential problems, in selected patients we applied an antegrade–retrograde approach. The best distal runoff vessel was first evaluated by US or MRA and then after angiographic confirmation directly punctured under color US guidance using a micropunture kit (Cook) at its most distal end. The use of the 4F Terumo introducer allowed us to advance into the ATa or the PTa with the guidewire–catheter without friction at the entry zone, to push more effectively, and to remove possible thrombi, contemporarily performing angiographies through the introducer. However, thrombi formation was prevented by the preprocedural administration of ticlopidine 500 mg + aspirin 100 mg and by the use of heparinized saline.
The spasm effect that the movement of the devices inside such small vessels could have caused was one of our concerns, but the reduced reaction of such sclerosed arteries in fact has kept confined this event. The presence of ulcers at the entry zone is unfortunately a limitation to the performance of this type of procedure.
Previous authors have already used this type of limb salvage approach [10, 11]. In particular, Spinosa et al. have recently presented a very interesting retrospective study showing a limb salvage rate of 90% at 6 months by applying the above-mentioned technique [14]. Similarly, but at 12 months, in our small group of patients we had a 100% limb salvage rate. In addition to this, in our group of patients the antegrade and retrograde approach was planned and performed without attempting an antegrade approach alone.
The involvement of the popliteal trifurcation is at too high risk of hampering the secure direction of the wire toward the patent distal runoff vessel; moreover, repeated attempts to reenter the true lumen or prolonged maneuver of the wire could lead to vessel damage or thrombus formation and subsequent failure of the recanalization. Therefore, because the risk involved is too high for the patient, this technique should be adopted as a standard procedure in CLI cases showing long occlusions involving the trifurcation and presenting risk of amputation.
Although a larger number of cases would strengthen the case, nonetheless we think that this type of planned combined antegrade and retrograde subintimal recanalization approach is an excellent first choice of endovascular option in cases of long femoro-popliteal obstructions involving the trifurcation.
References
Dormandy J, Heeck L, Vig S (1999) Major amputations: Clinical patterns and predictors. Semin Vasc Surg 12:154–161
Wolfe JH, Wyatt MG (1997) Critical and subcritical ischaemia. Eur J Vasc Endovasc Surg 13:578–582
Yilmaz S, Sindel T, Yegin A, et al. (2003) Subintimal angioplasty of long superficial femoral artery occlusions. J Vasc Intervent Radiol 14:997–1010
Stanley B, Teague B, Raptis S, et al. (1996) Efficacy of balloon angioplasty of the superficial femoral artery and popliteal artery in the relief of leg ischemia. J Vasc Surg 23:679–685
Adam DJ, Beard JD, Cleveland T, et al. (2005) BASIL trial participants. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet 366(9501):1925–1934
Bolia A, Miles KA, Brennan J, et al. (1990) Percutaneous transluminal angioplasty of occlusion of femoral and popliteal arteries by subintimal dissection. Cardiovasc Intervent Radiol 13:357–363
Reekers JA, Kromhout JG, Jacobs JHM (1994) Percutaneous intentional extraluminal recanalisation of the femoropopliteal artery. Eur J Vasc Surg 8:723–728
London NJM, Srinivasan R, Naylor AR, et al. (1994) Subintimal angioplasty of femoropopliteal artery occlusions: The long term results. Eur J Vasc Surg 8:148–155
van der Zaag ES, Legemate DA, Prins MH, et al. (2004) Angioplasty or bypass for superficial femoral artery disease? A randomised controlled trial. Eur J Vasc Endovasc Surg 28:132–137
Spinosa DJ, Leung DA, Harthun NL, et al. (2003) Simultaneous antegrade and retrograde access for subintimal recanalization of pheripheral arterial occlusion. J Vasc Intervent Radiol 14:1449–1454
Botti CF, Ansel GM, Silver MJ, et al. (2003) Percutaneous retrograde tibial access in limb salvage. J Endovasc Ther 10:614–618
Ingle H, Nasim A, Bolia A, et al. (2002) Subintimal angioplasty of isolated infragenicular vessels in lower limb ischemia: long-term results. J Endovasc Ther 9(4):411–416
Nasim A, Sayers RD, Dunlop P, et al. (1996) Intentional extraluminal recanalisation of the femoropopliteal segment following perforation during percutaneous transluminal angioplasty. Eur J Vasc Endovasc Radiol 12:246–249
Spinosa DJ, Harthun NL, Bissonette EA, et al. (2005) Subintimal arterial flossing with antegrade-retrograde intervention (SAFARI) for subintimal recanalization to treat chronic critical limb ischemia. J Vasc Intervent Radiol 16:37–44
Reekers JA (2002) Percutaneous intentional extraluminal (subintimal) revascularization (PIER) for critical lower limb ischemia: too good to be true? J Endovasc Ther 9:419–421
Bray PJ, Robson WJ, Bray AE (2003) Percutaneous treatment of long superficial femoral artery occlusive disease: Efficacy of the hemobahn stent-graft. J Endovasc Ther 10:619–628
Conroy RM, Gordon IL, Tobis JM, et al. (2000) Angioplasty and stent placement in chronic occlusion of the superficial femoral artery: Technique and results. J Vasc Intervent Radiol 11:1009–1020
Bolia A, Sayers RD, Thompson MM, et al. (1994) Subintimal and intraluminal recanalisation of occluded crural arteries by percutaneous balloon angioplasty. Eur J Vasc Surg 8:214–219
Alback A, Biancari F, Schmidt S, et al. (1998) Haemodynamic results of femoropopliteal percutaneous transluminal angioplasty. Eur J Vasc Endovasc Surg 16:7–12
Allen BT, Reilly JM, Rubin BG, et al. (1996) Femoropopliteal bypass for claudicatio: vein vs PTFE. Ann Vasc Surg 10:178–185
Hunink MG, Wong JB, Donaldson MC, et al. (1994) Patency results of percutaneous and surgical revascularization for femoropopliteal arterial disease. Med Decis Making 14:71–81
Shah DM, Darling RC, Chang BB, et al. (1995) Long term results of in situ saphenous vein bypass: analysis of 2058 cases. Ann Surg 222:438–446
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gandini, R., Pipitone, V., Stefanini, M. et al. The “Safari” Technique to Perform Difficult Subintimal Infragenicular Vessels. Cardiovasc Intervent Radiol 30, 469–473 (2007). https://doi.org/10.1007/s00270-006-0099-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-006-0099-3