Abstract
Purpose
The purpose of this article is to report the results of a prospective single-center study analyzing the long-term clinical and angiographic outcomes of subintimal angioplasty (SIA) for the treatment of chronic total occlusions (CTOs) of the femoropopliteal artery.
Materials and Methods
Patients with severe intermittent claudication or critical limb ischemia (CLI) were enrolled in the study. All lesions were treated with SIA and provisional stenting. Primary end points were technical success, patient survival, limb salvage, lesion primary patency, angiographic binary restenosis (>50%), and target lesion revascularization (TLR). Regular clinical and angiographic follow-up was set at 6 and 12 months and yearly thereafter. Study end points were calculated with life-table survival analysis. Proportional-hazards regression analysis with a Cox-model was applied to adjust for confounding factors of heterogeneity.
Results
Between May 2004 and July 2009, 98 patients (105 limbs, patient age 69.3 ± 9.9 years) were included in the study. Technical success rate was 91.4% with a lesion length of 121 ± 77 mm. Limb-salvage and survival rates were 88.7% and 84.1% at 3 years, respectively. After 12, 24, and 36 months, primary patency was 80.1%, 42.3%, and 29.0%, angiographic binary restenosis was 37.2%, 68.6%, and 80.0%, and TLR was 84.8%, 73.0%, and 64.5%, respectively. CLI was the only adverse predictor for decreased primary patency (hazard ratio [HR] 0.36; 95% confidence interval [CI] 0.16–0.80, p = 0.012), whereas significantly less restenosis was detected after spot stenting of the entry and/or re-entry site (HR 0.31; 95% CI 0.10–0.89, p = 0.01 and HR 0.20; 95% CI 0.07–0.56, p = 0.002, respectively).
Conclusions
Subintimal angioplasty is a safe and effective revascularization technique for the treatment of CTOs of the femoropopliteal artery. Provisional stenting may have a role at the subintimal entry or true lumen re-entry site.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The last decade has been marked by a rapid increase in endovascular management of obstructive arterial disease of the lower limbs, especially in the femoropopliteal segment. Several modern techniques, such as subintimal angioplasty (SIA), allow employment of endovascular recanalization procedures even in patients in whom, until recently, surgical bypass was the only feasible solution. Since its first description by Bolia in 1989, the use of SIA has rapidly expanded, and it is nowadays considered as an acceptable alternative technique for revascularization of totally occluded lesions, especially in the superficial femoral artery (SFA) and/or popliteal artery (PA) [1–3].
Data regarding primary patency rates at 1 year after SIA vary widely [1, 4–6]. Two recent regression meta-analyses of several SIA studies, including 1549 and 2810 limbs, respectively, estimated that 1-year primary patency rate was approximately 50% and that limb salvage varied from 80% to 90% [7, 8]. Albeit the not-so-favorable 1-year patency rates, SIA achieves encouraging limb-salvage rates, especially in patients with critical limb ischemia (CLI). Although surgical bypass demonstrates equally favorable limb salvage and even greater vessel patency rates, the abovementioned data make SIA a good alternative to surgical bypass in patients who are unsuitable to undergo peripheral bypass surgery, such as CLI patients with multiple comorbidities or in the absence of a proper vein conduit [9]. Unfortunately, the current literature lacks any angiographic follow-up of SIA, and no objective data regarding angiographic restenosis rates are so far available about SIA-treated lesions.
Renal disease, smoking, diabetes mellitus (DM), occlusion length, distal SFA lesions, postprocedural ankle–brachial index, and number of runoff arteries are all factors that have been documented to adversely affect primary patency and long-term SIA outcomes [9–11]. However, predictors for better angiographic patency after SIA have not been adequately investigated so far. In addition, the role of bare stent or stent-graft placement during subintimal recanalization of chronic total occlusions (CTOs) has been only touched on [12–15]. The investigators herein report the results of a prospective single-center registry with the aim to investigate the immediate result as well as the long-term clinical and angiographic outcome of SIA plus bail-out stenting for the treatment of chronic total occlusive atherosclerotic disease of lesions located in the SFA and/or PA. In addition, multivariable Cox proportional-hazards regression analysis was applied to adjust for confounding factors of heterogeneity and identify any independent predictors of favorable clinical or angiographic outcome of treated lesions.
Materials and Methods
Study Design
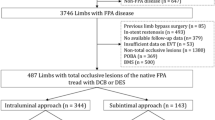
This was a prospective single-arm registry including individuals with either severe, life style–limiting intermittent claudication (IC) or CLI (Rutherford categories 3 to 6) presenting with at least one CTO of the SFA and/or popliteal (PA) artery as documented on preprocedural digital subtraction angiography (DSA). Clinical severity of limb ischemia was defined according to the Rutherford classification [16]. Patients were included in the study provided that they fulfilled all inclusion criteria as listed in Table 1. All patients were informed about the study’s nature and goal as well as its long-term design, to include angiographic follow-up, and they signed the appropriate informed consent form before undergoing the procedure. Lesions with heavy vessel-wall calcifications (by visual estimation), although this is considered a relative contraindication for SIA, were also included in the study. In all cases, the subintimal approach was performed after a failed attempt at intraluminal revascularization to achieve reperfusion of the distal ischemic limb. Among the exclusion criteria were acute arterial occlusions, IC classified as Rutherford categories 1 to 2, successful intraluminal wire passage through the lesion, a history of severe contrast allergy or hypersensitivity, intolerance to aspirin and/or clopidogrel, and systemic coagulopathy or other hypercoagulation disorders. The study’s inclusion and exclusion criteria are listed in Table 1.
Procedure
All patients were premedicated with aspirin (100 mg/d) and clopidogrel (75 mg/d) for 3 days before the procedure. Diabetic patients treated with metformin were adequately hydrated and appropriately advised to adjust their therapy as proposed by international guidelines [17]. Subintimal angioplasty was performed as previously described by Bolia [2, 3]. In brief, an antegrade puncture was performed, even when the occlusion was in the proximal segment, due to the superior pushability accomplished by this approach. On rare occasions on which the antegrade approach was impossible, or if ipsilateral iliac artery lesions had to be treated, a retrograde approach was performed. Entry transition to the subintimal space and re-entry to the intraluminal space was performed using a soft angled tip or j-tip hydrophilic 0.035-in. guidewire (Terumo, Tokyo, Japan) with support of a 4F angled hydrophilic glidecatheter (Terumo). The guidewire was advanced with a looped shape through the subintimal space (Bolia loop technique). After confirmation of successful distal re-entry, standard dilatation of the target lesion was performed using conventional balloon angioplasty. Stenting was reserved as bailout to deal with cases of elastic recoil or significant residual stenosis (>30%). After treatment of the target lesion, infrapopliteal lesions, if any, were also treated accordingly [18]. During the procedure, 5000 IU heparin were administered after sheath placement and followed by infusion of 1000 IU heparin per hour during the procedure. After completion of the procedure, all patients were prescribed to dual antiplatelet therapy for 6 months (same as preprocedure) and instructed to receive solely clopidogrel for lifetime thereafter. Exceptions to this were patients on warfarin.
Definitions and End Points
Primary clinical end points included technical success, overall patient survival and limb salvage, minor amputation, and target lesion revascularization (TLR). Angiographic end points included primary patency and binary restenosis as assessed by follow-up DSA. Technical success was defined as successful transition of the target lesion through the subintimal space and re-entry into the true lumen, with provisional use of re-entry devices, resulting in <30% residual stenosis with or without bail-out stenting. Indications for bail-out stenting after PTA included elastic recoil or residual stenosis >30% or flow-limiting dissection of the treated lesion. Limb salvage was determined as survival without any event of major amputation. TLR was defined as any repeat surgical or endovascular recanalization procedure within the target lesion due to symptomatic lesion restenosis or reocclusion as documented by DSA. The rest of the clinical end points and complications were defined according to international published guidelines and reporting standards [19]. Primary patency was defined as lack of occlusion without any additional TLR procedure, either surgical or endovascular, of the previously treated lesion at follow-up. Binary restenosis was specified as a decrease of the treated segment’s lumen by >50% according to reference vessel diameter. Clinical follow-up was prospectively scheduled and included regular revisits at 1, 3, 6, and 12 months after intervention, and yearly thereafter, to evaluate patient mobility and general health status. Angiographic follow-up by standard selective DSA was performed at 6 and 12 months and every year thereafter unless clinical deterioration occurred earlier.
Data Collection
Two independent vascular interventional radiologists, who were blinded to any other data, reviewed and analyzed the DSA images of all procedures. Researchers recorded lesions’ initial characteristics, such as length, treatment modality (solely angioplasty and/or stent use), as well as lesion location and stent location (full lesion stent coverage, placement of stent in the entry and/or re-entry site). In addition, they elaborated the angiographic follow-up images. In cases of ambiguity, there was a consensus between the two radiologists regarding the final result. Patient’s demographics, clinical status before and after the procedure, and specific procedural details were recovered from our database. Below-the-knee tibial runoff at the end of the procedure was described with a simplified score of 0 to 3 as described elsewhere [18]. End-point cumulative proportion outcomes were determined by life-table analysis with Kaplan–Meier plots. Subjects were censored in case of death, major amputation, repeat surgical or endovascular procedure, or angiographically proven vascular occlusion or binary restenosis or at the time of the patient’s last follow-up visit or communication. Multivariable Cox proportional-hazards regression analysis was applied to adjust for confounding factors of heterogeneity as described later in the text.
Statistical Analysis
Discrete variables were expressed as counts and percentages, whereas continuous variables were calculated as medians and interquartile ranges or as means ± SEs if they passed the Kolmogorov-Smirnov goodness-of-fit test. Unpaired Student t test was used to test variables originating from normal distributions. Mann–Whitney nonparametric test was used to test variables that did not pass the normality test. Life-table analysis with the Kaplan–Meier method was employed to calculate proportional outcomes of end points ≤3 years. Stepwise regression analysis, with use of the Cox proportional-hazards regression model, during the total follow-up period was performed to identify independent risk factors affecting the predefined end points. Dependent variables included DM, serum creatinine level (>1.5 mg/dL), nicotine use (up to the past 12 months), hyperlipidemia (more than mild increase controlled with diet or drugs), baseline Rutherford category (severe IC or CLI), lesion length, stent use, site of stenting (at entry and/or re-entry site, stenting of the whole lesion), vessel-wall calcifications (none, mild, or heavy), and infrapopliteal runoff score at the end of the procedure. The covariates included major amputation-free survival, TLR-free survival, primary patency, and binary in-lesion restenosis. The results are provided as hazard ratios (HRs) with the associated 95% confidence intervals (CIs) and the relevant level of statistical significance. The adjusted curves of the identified covariate are graphically illustrated only in cases of statistically significant results. Statistical analysis was performed with use of the SPSS/PASW statistical software package (version 17.0; SPSS/PASW, Chicago, IL). The threshold of statistical significance was set at 5% (i.e., α = 0.05).
Results
From May 2004 to July 2009, a total of 98 patients (105 limbs) fulfilled the study’s inclusion criteria and were included in the analysis. Mean age was 69.3 ± 9.9 years (range 42 to 85). Patient demographics and baseline clinical characteristics are listed in Table 2. Almost 50% of the patients had DM, and 70.4% had hyperlipidemia. Most of the patients included in the study reported symptoms of CLI (64.3%). Lesions were solely located in the SFA in 66.7% of the cases (70 of 105). The majority of the treated lesions were heavily calcified (75 of 105). The mean overall treated lesion length was 12.1 ± 7.7 cm, and bail-out stenting had to be employed in 70.5% of the cases (74 of 105). In 23.8% of cases (25 of 105), the whole lesion was stented (full lesion stenting). In 46.7% of cases (49/105), a stent was implanted at the level of the subintimal entry and/or re-entry site. Procedural details are analytically listed in Table 3.
Overall technical success of SIA was 91.4%, and in 7 cases (6.6%) a re-entry device (Outback re-entry catheter; Cordis, Miami Lakes, FL) was employed to successfully re-enter the true lumen. There were no procedure-related deaths, and complications were limited to two cases of retroperitoneal hemorrhage. One of those was self-limited and did not require any blood transfusion, whereas the other necessitated 2 U red blood cells. Local hematoma was noted at the puncture site in 2.9% of the treated limbs and required no further treatment. Other adverse events related to the procedure were noted in 8.6% (9 of 105) of the treated limbs. More specifically, accidental perforation of the artery occurred in 4 (3.8%) of cases. In one case, coil embolization was performed; in another, a diverse route was used to cross the subintimal space; and the remaining two were treated conservatively without any sequelae. In three cases (2.9%), distal embolization occurred; two of them being were treated by mechanical thrombectomy and adjunctive local thrombolysis. In the remaining case, application of a distal filter-protection device prevented distal thromboembolism. Finally, one acute thrombosis of the whole lesion occurred and was treated successfully by Angiojet rheolytic thrombectomy.
The mean clinical follow-up period was 24.5 ± 15.1 months (range 0.2 to 93.9), and the respective angiographic follow-up period was 17.1 ± 14.1 months (range 1.6 to 93.0). According to Kaplan–Meier analysis, the 3-year cumulative proportional mortality rate was 84.1%. The respective cumulative outcomes at 1 and 2 years were 93.0% and 88.8%, respectively. Cumulative proportional limb-salvage rates at 1, 2, and 3 years were estimated at the level of 95.7%, 91.3% and 88.7%, respectively (Fig. 1A and B). Estimated TLR-free survival was 84.8%, 73.0%, and 64.5%, at 12, 24, and 36 months, respectively (Fig. 1C). No statistically significant difference was noted between cases of IC and CLI. The Cox proportional regression model did not identify any favorable independent predictive factor for patient survival or limb salvage. Overall minor amputations were recorded in 6 treated cases (5.7%, 6 of 105). Focusing on angiographic end points, Kaplan–Meier plotting showed an estimated primary patency rate of 80.1% at 1 year, which decreased to 42.3% and 29.0% at 2 and 3 years, respectively (Fig. 2A). Angiographic binary restenosis of SIA-treated lesions was estimated at 37.2% at 1 year, which increased to 68.6% and 80.0% at 2 and 3 years, respectively (Fig. 2B).
Application of multivariable analysis using Cox proportional-hazards regression model to adjust for the previously reported confounding factors of heterogeneity identified spot stenting of the entry (HR 0.31; 95% CI 0.10–0.89, p = 0.03) and/or re-entry site (HR 0.20; 95% CI 0.07–0.56, p = 0.002) as positive predictors of significantly less in-lesion binary restenosis. In contrast, the Cox model showed that “full-lesion metal jacket” was a highly significant predictor of increased lesion restenosis (HR 5.88; 95% CI 1.64–20.00, p = 0.007). In addition, angiographic binary restenosis of SIA-treated lesions was negatively affected by increased initial CTO length (HR 4.55; 95% CI 1.41–14.29, p = 0.011 for lesions > 200-mm long) and initial CLI symptoms (HR 2.78; 95% CI 1.25–6.67, p = 0.03). In contrast, the only significant adverse predictor of decreased primary patency was CLI (HR 0.36; 95% CI 0.16–0.80, p = 0.012) (Table 4 and Figs. 3 and 4).
Discussion
Management of long CTOs remains the last frontier in endovascular treatment of peripheral obstructive arterial disease. Until recently, surgical bypass seemed the only feasible solution for such lesions. Since its first description by Bolia, SIA has gained recognition and is today considered a good alternative to surgical methods, especially in patients ineligible to undergo open surgery [9]. Although SIA is currently widely used and worldwide experience with the technique is growing, there is still considerable skepticism regarding the method and its results. This is mainly due to lack of evidence from randomized clinical trials comparing SIA with traditional surgical bypass. However, SIA is known to yield high percentages of technical success and acceptable long-term clinical patency and limb-salvage rates [7, 8].
The present report describes a prospective registry aimed to assess the long-term angiographic and clinical outcomes of SIA in CTOs of the superficial femoral and/or PA. Stents were used in a bailout manner after suboptimal and/or complicated angioplasty result, and the site of implantation was recorded. Of note, a high proportion of treated lesions (71.43%, 75 of 105) were initially heavily calcified, which may be the reason for the relatively high percentage of bail-out stenting in the present study (70.5%). The main contribution of the present study is the angiographic follow-up documentation of SIA-treated lesions to evaluate not only limb salvage but also angiographic vessel restenosis. Thus far, published studies have provided no angiographic data whatsoever regarding neointimal hyperplasia and vessel restenosis after SIA. In our opinion, clinical primary patency rates that are used as an end point in most published series fall short of providing an objective end point of SIA outcomes over time. Although limb salvage is the most widely accepted clinical outcome measure in the CLI population, angiographic binary vessel restenosis (>50%), along with TLR events, are more suitable end points for revascularization studies in patients with life style-limiting IC.
Technical success of SIA with the loop technique was 84.8% in our series and increased to ≤91.4% with the use of re-entry devices, which correlates well with data published thus far [7]. Thus far, reported primary patency outcomes have varied widely and are mostly documented at 1-year follow-up. In contrast, long-term results are scarce. London et al. reported a 46% hemodynamic patency at 3 years on an intention-to-treat basis, whereas the respective rate per treatment received was 58% [1]. In the study by Treiman et al., routine full-lesion stenting after SIA resulted in poor vessel patency, e.g., as low as 18% after 3 years [13]. In contrast, Scott et al. showed improved long-term primary patency rates using selective stenting, approximately 45% to 55% at 1 year and approximately 25% at 3 years [20, 21]. In our series, by using stenting selectively as bail-out strategy, cumulative proportional primary patency was calculated at 80.1%, 42.3%, and 29.0% at 12, 24, and 36 months, respectively. The main reason for the relatively lower primary patency rate at 3 years was the high incidence of angiographic reocclusion, which has not been incorporated into any of the studies published to date.
Provisional stenting has been known to improve the immediate procedural success of SIA. However, to date, either selective stenting or full-lesion stenting (i.e., “full-metal jacket”) has not proved its superiority compared with plain balloon angioplasty [13, 21]. Of interest, in a recent study by Boufi et al., there was no primary patency benefit by employment of a covered stent to treat the whole subintimal tract [15]. In our series, stenting was deemed necessary in 70.5% of the cases, all of which resulted in excellent initial outcome. However, after extensive multivariate statistical analysis, full-lesion stenting was recognized as an independent predictor associated with almost 6-fold greater binary restenosis as calculated by Cox regression analysis. In contrast, selective implantation of stents either in the subintimal entry or true lumen re-entry site was linked to decreased rates of restenosis. Specifically, stenting of the entry site was related to 3.3 times less angiographic restenosis, whereas stenting of the re-entry site was associated with almost 5 times less restenosis. Of note, Cox proportional-hazards analysis highlighted the adverse impact of CLI as initial clinical presentation on both primary patency and binary restenosis. Patients who initially presented with severe claudication exhibited a 2.7-fold better primary patency compared with CLI individuals. Again, claudicant patients demonstrated favorable restenosis rates compared with patients having CLI. Finally, the Cox model confirmed the adverse effect of increased lesion length on long-term SIA outcomes.
Limitations
Admittedly, the present analysis is limited by the fact that this was a single-center prospective study with a small cohort of patients. In addition, there was no follow-up treadmill testing to objectively evaluate functional outcomes, such as walking distance in case of claudicants, nor wound healing outcomes were assessed in case of CLI. Stenting was a priori reserved as bail-out strategy, and the principle of primary stenting as a CTO treatment was not explored. Despite the absence of definite evidence but taking into consideration the relatively poor medium-term patency rates of the procedure, we prescribed clopidogrel for life in all of our patients who underwent SIA.
Conclusion
In conclusion, SIA is a safe and effective revascularization technique for the treatment of CTOs of the femoropopliteal arteries. Based on our results, provisional stenting may have a role when cautiously used. Further studies are necessary to justify their use.
References
London NJ, Srinivasan R, Naylor AR et al (1994) Subintimal angioplasty of femoropopliteal artery occlusions: the long-term results. Eur J Vasc Surg 8(2):148–155
Bolia A, Miles KA, Brennan J, Bell PR (1990) Percutaneous transluminal angioplasty of occlusions of the femoral and popliteal arteries by subintimal dissection. Cardiovasc Intervent Radiol 13(6):357–363
Bolia A, Brennan J, Bell PR (1989) Recanalisation of femoro-popliteal occlusions: improving success rate by subintimal recanalisation. Clin Radiol 40(3):325
Bolia A, Bell PR (1995) Femoropopliteal and crural artery recanalization using subintimal angioplasty. Semin Vasc Surg 8(3):253–264
Lipsitz EC, Veith FJ, Ohki T (2005) Subintimal angioplasty in the management of critical lower-extremity ischemia: value in limb salvage. Perspect Vasc Surg Endovasc Ther 17(1):11–20
Lipsitz EC, Ohki T, Veith FJ et al (2003) Does subintimal angioplasty have a role in the treatment of severe lower extremity ischemia? J Vasc Surg 37(2):386–391
Bown MJ, Bolia A, Sutton AJ (2009) Subintimal angioplasty: meta-analytical evidence of clinical utility. Eur J Vasc Endovasc Surg 38(3):323–337
Met R, Van Lienden KP, Koelemay MJ, Bipat S, Legemate DA, Reekers JA (2008) Subintimal angioplasty for peripheral arterial occlusive disease: a systematic review. Cardiovasc Intervent Radiol 31(4):687–697
Markose G, Miller FN, Bolia A (2010) Subintimal angioplasty for femoro-popliteal occlusive disease. J Vasc Surg 52(5):1410–1416
Keeling AN, Khalidi K, Leong S et al (2009) Subintimal angioplasty: predictors of long-term success. J Vasc Interv Radiol 20(8):1013–1022
Kim SJ, Kim W, Kim JB, Hong MJ, Kang WY, Hwang SH (2010) Determinants of procedural success and patency following subintimal angioplasty in patients with TASC C and D femoropopliteal arterial disease. Circ J 74(9):1959–1964
Schmieder GC, Richardson AI, Scott EC, Stokes GK, Meier GH III, Panneton JM (2008) Selective stenting in subintimal angioplasty: analysis of primary stent outcomes. J Vasc Surg 48(5):1175–1181
Treiman GS, Treiman R, Whiting J (2006) Results of percutaneous subintimal angioplasty using routine stenting. J Vasc Surg 43(3):513–519
Kim JS, Kang TS, Ahn CM et al (2006) Efficacy of subintimal angioplasty/stent implantation for long, multisegmental lower limb occlusive lesions in patients unsuitable for surgery. J Endovasc Ther 13(4):514–521
Boufi M, Dona B, Orsini B, Auquier P, Hartung O, Alimi YS (2010) A comparison of the standard Bolia technique versus subintimal recanalization plus Viabahn stent graft in the management of femoro-popliteal occlusions. J Vasc Surg 52(5):1211–1217
Rutherford RB, Baker JD, Ernst C et al (1997) Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 26(3):517–538
Thomsen HS (2006) European Society of Urogenital Radiology (ESUR) guidelines on the safe use of iodinated contrast media. Eur J Radiol 60(3):307–313
Siablis D, Karnabatidis D, Katsanos K et al (2007) Sirolimus-eluting versus bare stents after suboptimal infrapopliteal angioplasty for critical limb ischemia: enduring 1-year angiographic and clinical benefit. J Endovasc Ther 14(2):241–250
Sacks D, Marinelli DL, Martin LG, Spies JB (2003) Reporting standards for clinical evaluation of new peripheral arterial revascularization devices. J Vasc Interv Radiol 14(9 Pt 2):S395–S404
Scott EC, Biuckians A, Light RE, Burgess J, Meier GH 3rd, Panneton JM (2008) Subintimal angioplasty: our experience in the treatment of 506 infrainguinal arterial occlusions. J Vasc Surg 48(4):878–884
Scott EC, Biuckians A, Light RE et al (2007) Subintimal angioplasty for the treatment of claudication and critical limb ischemia: 3-year results. J Vasc Surg 46(5):959–964
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siablis, D., Diamantopoulos, A., Katsanos, K. et al. Subintimal Angioplasty of Long Chronic Total Femoropopliteal Occlusions: Long-Term Outcomes, Predictors of Angiographic Restenosis, and Role of Stenting. Cardiovasc Intervent Radiol 35, 483–490 (2012). https://doi.org/10.1007/s00270-011-0244-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-011-0244-5