Abstract
Purpose
Different types of drug-eluting beads have been proposed for hepatocellular carcinoma (HCC) treatment, but long-term results are not well known. We report safety, efficacy and long-term overall survival of HCC patients not amenable of curative therapies treated with transcatheter arterial chemoembolization (TACE) using drug-eluting beads sized 70–150 micron.
Materials and Methods
This single-center retrospective study included 125 patients with Barcelona Clinic Liver Cancer stage A (80), B (45) and compensated cirrhosis. TACE was executed injecting drug-elutings microparticles loaded with 75 mg of Doxorubicine and was repeated in patients with partial response or stable disease after one month. Adverse events, response according to modified Response Evaluation Criteria in Solid Tumors and overall survival were assessed.
Results
Chemoembolization with 70–150 micron beads revealed an objective response rate of 88% according to mRECIST criteria and complete response was 60%. After a median follow-up of 53.3 months, overall survival was 36.6 months. Data were censored at the date of liver transplantation in 35 patients. 33 on 125 patients (26,4%) experienced at least one adverse event. We recorded a total of 102 adverse events and 18 were of a high grade (G3–G4). 30 day mortality was 0%.
Conclusion
Chemoembolization with very small particles (70–150 µm) is an effective and safe treatment in unresectable HCC both as a primary therapy or as bridge to transplantation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to Barcelona Clinic Liver Cancer (BCLC) staging system, transcatheter arterial chemoembolization (TACE) is the recommended treatment for patients with intermediate-stage hepatocellular carcinoma (HCC). Even patients with a disease that can potentially be treated radically (early stage disease A) but who are not eligible for surgery or ablation can benefit from TACE [1,2,3,4,5,6,7,8,9].
In a liver transplant perspective, TACE is effective as a bridge therapy in order to keep eligibility or as a downstaging therapy.
Transcatheter arterial chemoembolization with drug-eluting beads (DEBTACE) uses embolic microparticles able to bind chemotherapeutic agents via an ion exchange mechanism.
A wide range of beads diameters is available but which one is the best in terms of effectiveness and safety is still a matter of debate. Several scientific papers proved that efficacy and safety of DEBTACE increases using smaller beads, in particular 100–300 μm [10,11,12]. Interest in developing very small beads (i.e., 40 μm or 70–150 μm) is growing with the aim of increase drug penetration and obtains a more homogeneous distribution in the nodule. Different studies [6, 13, 14] have shown efficacy and safety of very small beads for the treatment of HCC, but there is currently a lack of data in the literature, especially regarding long-term survival.
The purpose of this study is to evaluate long-term overall survival (OS) of patients with unresectable and nonablatable HCC treated with drug eluting beads sized 70–150 μm. The long-term clinical tolerability profile of this treatment will also be evaluated.
Material and Methods
This was a single-center retrospective study. In order to obtain a prolonged OS times, we considered only patients who underwent DEBTACE with 70–150 μm particles from May 2012 to June 2015. Each patient was discussed during multidisciplinary meetings.
Inclusion criteria were: age > 18 years, diagnosis of HCC obtained according to non-invasive radiological criteria [15] or histology, early or intermediate stage HCC according to BCLC not amenable to curative treatments or HCC which failed/recurred after resection or ablation, compensated cirrhosis with Child–Pugh (CP) score not above B7, Performance Status score 0 according to Eastern Cooperative Oncology Group [16] (PS-ECOG 0), adequate clotting profile and adequate renal function.
Exclusion criteria were previous TACE treatments carried out in the previous three years, main or segmental portal vein thrombosis or extra-hepatic tumor spread.
Patients were premedicated with 20 mg of pantoprazole (Pantorc, Takeda, Osaka, Japan), 8 mg of ondasentron (Ondasentron, Hikma, Fervença, Portugal) and 2 g of cefazolin (Cefamizin, Pfizer, New York, NY, United States); during the procedure 1 g of paracetamol (Paracetamolo, S.A.L.F. S.p.A., Bergamo, Italy) was administered.
A 5F diagnostic angiographic catheter was inserted through a transfemoral access. Selective catheterization of tumor feeder arteries was performed as selectively as possible using a coaxial 2.8F microcatheter (Progreat, Terumo, Japan).
DEBTACE was performed injecting 2 mL of DCBeads M1 70–150 μm particles (Boston Scientific, Massachussets, MA, United States) loaded with 75 mg of doxorubicin (Adriblastina, Pfizer, New York, NY, USA) (DEBDOX), without adjustment for body surface.
An attempt was made to treat all nodules in a super-selective way but, if not possible, the treatment was performed including up to a maximum of three segments.
If flow stagnation was not achieved after DEBDOX injection, non-loaded microparticles of different size where injected until stagnant blood flow lasting for three cardiac cycles. This was accomplished by infusing Bead block (Boston Scientific, Massachussets, MA, United States) 100–300 micron and eventually shifting to 300–500 micron.
The treatment strategy was conducted “on demand” by means of one or more rounds each of which consists of one or more sessions of debTACE. The round ends with the achievement of complete radiological tumor response (CR), best achievable response (i.e., partial response or stable disease) or progressive disease (PD).
Patients were hospitalized and observed until discharge for 48–72 h. Clinical evaluation and laboratory values were recorded the day before and 24, 48 h, 7 days and 4 weeks after DEBTACE, then every three months.
Adverse events were defined treatment-related if occurred within 30 days from DEBTACE and were classified according to the Common Terminology Criteria for Adverse Events 5.0 (CTCae) [17].
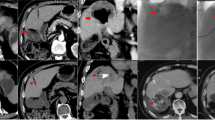
Radiological response was assessed by CT or MRI 4–6 weeks after treatment according to modified RECIST criteria (mRECIST) [18] then every three months thereafter. For analytical purposes we have taken into account the best radiological response of patients at the end of each round of treatment since initial response is considered a better predictor of survival [19].
Patients overall survival (OS) was computed from the date of the first DEBTACE session to the day of death censoring at the date of last follow-up for patients still alive and censoring at the date of transplant for those transplanted.
Statistical Analysis
Survival rates and curves were determined using Kaplan-Meyer method and compared using nonparametric log-rank test. Univariate analysis was performed on each variables to examinate their influence on patient’s survival and radiologic response and are reported with log-rank test for categoric variables and Cox regression analysis for continuous variables.
Eventually, all variables found to be significant in univariate analysis were included in Cox multivariate analysis to identify independent predictors of outcome.
A conventional p value less than 0.05 was considered significant.
All calculations were carried out using SPSS package version 26 (IBM, Armonk, NY, United States).
Results
From the 142 consecutive patients with documented HCC, 125 were analyzed, while 17 were lost at follow-up. The main baseline characteristics observed in the 125 patients are summarized in Table 1.
All patients were asymptomatic (PS-ECOG 0) at time of DEBTACE with a modest prevalence of BCLC A (64%) compared to BCLC B (36%). Forty-three patients underwent DEBTACE as a “neoadjuvant” or a "bridging to transplant" scenario and were subsequently treated radically with liver resection (4 patients), thermoablation (4 patients) or orthotopic liver transplant (35 patients). Causes of precluding curative treatments in patients in BCLC stage A were a combination of comorbidities, portal hypertension or difficult tumor location.
Fifty-three patients (42,4%) had previous curative treatments for HCC such as surgery, thermoablation or liver transplant but relapsed.
At baseline, the median number of nodules per patient was 2 (2–10) with mean tumor burden of 44 mm (8–207 mm), intended as sum of diameters. The baseline median size of the main nodule was 27 mm (8–144 mm).
A total number of 311 DEBTACE procedures were performed. The median number of treatments per patients was 2 (1–8).
Seventy (22.5%) nodules were treated in a superselective manner, seventy-nine (25.4%) DEBTACE were performed segmentally, eighty-eight (28.3%) were bisegmental and the remaining (23,8%) were performed on three right segments or the whole left lobe.
Eighty-one (64.8%) patients underwent one round of DEBTACE, thirty-six (28,8%) patients underwent two rounds and eight (6.4%) patients underwent three or more rounds.
Over a total of 311 DEBTACE sessions 33 on 125 patients (26,4%) experienced an adverse event. We recorded a total of 102 adverse events and 18 were of a high grade (G3–G4) according to CTCae v5.0 (Table 2). High-grade adverse events were mostly related to altered laboratory values: 10 was related to elevation of alanine or aspartate aminotransferases, 1 was related to elevation of bilirubin, 2 were cases of elevation of serum amylase with pancreatitis related symptoms, 1 case was related to anemia and 1 case was related to thrombocytopenia. One high grade clinical adverse event that led to hospitalization was a case of oesophageal varices bleeding 30 days after treatment most likely related to the worsening of the portal hypertension.
Two high grade adverse events were related to post-embolic syndrome: one G3 post embolic epigastric pain and one post embolic vomiting both requiring medical therapy and observation. Adverse events are summarized in Table 2.
Seventy-five patients experienced a CR (60%) and 36 a PR (28.8%) accounting for 88.8% of objective response rate (ORR). Since SD was obtained in 5 (4%) patients the total disease control rate (DCR) reached 92.8%.
Over the follow-up period crossover to Sorafenib was prescribed in 38 patients.
After a median follow-up of 53.3 months (range 46.5–60.1 mo), 75 patients died and 35 underwent liver transplantation.
The 1, 3, 5 year survival of our cohort was 90.7%, 48% and 30.8% with a median overall survival (OS) of 36.6 months (95%CI: 25.96–41.24) (Fig. 1). The 1, 3, 5 year survival of the BCLC-A cohort was 97%, 55% and 39% with a median survival of 40.2 months. The 1, 3, 5 year survival of the BCLC-B cohort was 77%, 33% and 12% with a median survival of 28.6 months (Fig. 2).
79 patients had been treated upon progression disease (PD) with a median time to PD of 21.5 months (range 2.1–60.9 mo).
For overall survival baseline categoric variables BCLC and CP score met criteria for statistic significance at univariate analysis and baseline continuous variables bilirubin ≤ 1.1 mg/dL, albumin ≥ 4.1 g/dL, MELD < 10 points, alfaphetoprotein < 100 ng/mL and tumor burden (< 75 mm in sum) were significant for a better survival.
These variables were then included in a multivariate analysis and α-fetoprotein (AFP), tumor burden and Child–Pugh (CP) score resulted as independent predictors of survival among our population.
Results of univariate and multivariate analysis are summarized in Tables 1 and 3, respectively.
Discussion
DEBTACE is widely accepted in clinical practice to treat patients with liver-confined HCC, but current literature lacks data about long-term results, especially regarding small caliber DEB.
Scientific evidence shows that DEBTACE has a better safety profile and greater efficacy in terms of local response than conventional TACE, with non-inferior survival rates [7, 20,21,22,23,24,25]. In particular, smaller particles reach the pathologic microcirculation more deeply obtaining a better occlusion of the tumor feeding vessels with increased surface for drug release [26]. The uniform intratumoral distribution achieved by smaller beads is associated with higher necrosis rates as confirmed by pathologically studies in animals and on explanted liver after transplant [27].
A number of clinical series have been published using different kinds of very small drug eluting beads with solid results in terms of safety and efficacy [13, 28,29,30,31].
In this retrospective study, we analyzed almost 6 years of experience using very small particles 70–150 µm on 125 patients affected by liver-confined HCC not amenable of curative treatments.
Datas about tumoral best response show interesting results with 75 patients (60%) who achieved CR as best response with a total ORR in 111 patients over 125 (88.8%).
In our study, after a median follow-up of 53.3 months, OS for the entire cohort was 36.6 months. Fifty-three patients (42,4%) were not treatment naïve but relapsed after previous curative treatments for HCC such as surgery, thermoablation or liver transplant.
OS in our cohort may be influenced by the relevant number of transplanted patients: censoring follow-up at the liver transplant date occurred for 35 patients. Transplantation occurred for early stage patients with a hypothetical better survival than patients outside the transplant criteria.
Aliberti et al. [14] found a median overall survival of 42.0 months and a ORR slightly larger than ours (94.5% vs 94.0%). Our study confirms these datas providing that very small beads are promising also in terms of OS.
Balli et al. [32] have compared DEBTACE using particles > 100 µm (28 patients) vs particles < 100 µm (30 patients). After 24 months of median follow-up, they found an OS of 10 and 32 months, respectively, without reaching statistical significance in the two cohorts.
In terms of safety, DEBTACE with very small particles is well tolerated and present a low incidence of adverse effects in our series. Similar findings were obtained in the safety study on microspheres smaller than 100 microns, reported by Malagari et al. [12, 30], Richter et al. [13] as well as Greco et al. [33]. Deipolyi et al. [34] in their comparison between 70–150 microns and 100–300 microns sized microspheres showed that 70–150 microns sized microspheres caused more hepatobiliary side effects but in their report DEBTACE procedures were performed non-selectively in 69% of patients.
We found baseline AFP, tumor burden and CP score acting as independent predictive features of OS on multivariate analysis. A patient with a compensated liver function (Child–Pugh score A), AFP level < 100 ng/mL and a tumor baseline burden (sum of the maximum diameter of HCC nodules) < 75 mm is significantly associated with longer survival in our cohort.
The main limitations of the study are the retrospective nature and non-comparative design. Other limitations of the study include a relatively small number of patients, that 57% of patients were treatment-naïve, the nature of a single-center study. Prospective studies with randomized allocation to different DEB particle sizes or formulations and stratification by baseline patient or tumor characteristics, could help to identify subgroups of patients who would gain the most benefit from chemoembolization with small DEB.
In conclusion, this paper shows that DEBTACE with very small particles (70–150 µm) is an effective and safe treatment in unresectable HCC both as a primary therapy or in a bridge to transplant scenario.
References
Corrigendum to ‘EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma’ [J Hepatol 69 (2018) 182–236],” J. Hepatol., 2019;70:(4). https://doi.org/10.1016/j.jhep.2019.01.020.
Llovet JM, Bruix J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology. 2003. https://doi.org/10.1053/jhep.2003.50047.
Bruix J, Sherman M. Management of hepatocellular carcinoma: an update. Hepatology. 2011. https://doi.org/10.1002/hep.24199.
Llovet JM, et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet. 2002. https://doi.org/10.1016/S0140-6736(02)08649-X.
Facciorusso A. Drug-eluting beads transarterial chemoembolization for hepatocellular carcinoma: current state of the art. World J Gastroenterology. 2018. https://doi.org/10.3748/wjg.v24.i2.161.
Varela M, et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J Hepatol. 2007. https://doi.org/10.1016/j.jhep.2006.10.020.
Vogl TJ, et al. Liver, gastrointestinal, and cardiac toxicity in intermediate hepatocellular carcinoma treated with PRECISION TACE with drug-eluting beads: results from the PRECISION V randomized trial. Am J Roentgenol. 2011. https://doi.org/10.2214/AJR.10.4379.
Reyes DK, et al. Single-Center phase II trial of transarterial chemoembolization with drug-eluting beads for patients with unresectable hepatocellular carcinoma: initial experience in the United States. Cancer J. 2009. https://doi.org/10.1097/PPO.0b013e3181c5214b.
Lo CM, et al. Randomized controlled trial of transarterial Lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology. 2002. https://doi.org/10.1053/jhep.2002.33156.
Padia SA, et al. Safety and efficacy of drug-eluting bead chemoembolization for hepatocellular carcinoma: comparison of small-versus medium-size particles. J Vasc Interv Radiol. 2013. https://doi.org/10.1016/j.jvir.2012.11.023.
Prajapati HJ, et al. Survival, efficacy, and safety of small versus large doxorubicin drug-eluting beads TACE chemoembolization in patients with unresectable HCC. Am J Roentgenol. 2014. https://doi.org/10.2214/AJR.13.12308.
Malagari K, et al. Chemoembolization of hepatocellular carcinoma with hepasphere 30–60 μm. Safety and efficacy study. Cardiovasc Interv Radiol. 2014. https://doi.org/10.1007/s00270-013-0777-x.
Richter G, et al. Safety and feasibility of chemoembolization with doxorubicin-loaded small calibrated microspheres in patients with hepatocellular carcinoma: results of the MIRACLE I prospective multicenter study. Cardiovasc Interv Radiol. 2018;41(4):587–93. https://doi.org/10.1007/s00270-017-1839-2.
Aliberti C, et al. Transarterial chemoembolization with small drug-eluting beads in patients with hepatocellular carcinoma: experience from a cohort of 421 patients at an Italian center. J Vasc Interv Radiol. 2017. https://doi.org/10.1016/j.jvir.2017.07.020.
Llovet JM, et al. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012. https://doi.org/10.1016/j.jhep.2011.12.001.
Oken MM, Creech RH, Davis TE. Toxicology and response criteria of the eastern cooperative oncology group. Am J Clin Oncol Cancer Clin Trials. 1982. https://doi.org/10.1097/00000421-198212000-00014.
National Institute of Health, “National Cancer Institute Common Terminology Criteria for Adverse Events ( CTCAE ) version 5.0,” NIH Publication, 2017.
Lencioni R, Llovet JM. Modified recist (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010. https://doi.org/10.1055/s-0030-1247132.
Kim BK, et al. Complete response at first chemoembolization is still the most robust predictor for favorable outcome in hepatocellular carcinoma. J Hepatol. 2015. https://doi.org/10.1016/j.jhep.2015.01.022.
Malagari K, et al. Prospective randomized comparison of chemoembolization with doxorubicin-eluting beads and bland embolization with BeadBlock for hepatocellular carcinoma. Cardiovasc Interv Radiol. 2010. https://doi.org/10.1007/s00270-009-9750-0.
Lammer J, et al. Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION v study. Cardiovasc Interv Radiol. 2010. https://doi.org/10.1007/s00270-009-9711-7.
Van Malenstein H, et al. A randomized phase II study of drug-eluting beads versus transarterial chemoembolization for unresectable hepatocellular carcinoma. Onkologie. 2011. https://doi.org/10.1159/000329602.
Sacco R, et al. Conventional versus doxorubicin-eluting bead transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol. 2011. https://doi.org/10.1016/j.jvir.2011.07.002.
Golfieri R, et al. Randomised controlled trial of doxorubicin-eluting beads vs conventional chemoembolisation for hepatocellular carcinoma. Br J Cancer. 2014. https://doi.org/10.1038/bjc.2014.199.
Poon RTP, et al. A phase I/II trial of chemoembolization for hepatocellular carcinoma using a novel intra-arterial drug-eluting bead. Clin Gastroenterol Hepatol. 2007. https://doi.org/10.1016/j.cgh.2007.04.021.
Lewis AL, et al. DC BeadM1TM: towards an optimal transcatheter hepatic tumour therapy. J Mater Sci Mater Med. 2016. https://doi.org/10.1007/s10856-015-5629-6.
Spreafico C, et al. Transarterial chemoembolization for hepatocellular carcinoma with a new generation of beads: clinical-radiological outcomes and safety profile. Cardiovasc Interv Radiol. 2015. https://doi.org/10.1007/s00270-014-0907-0.
Aal AKA, et al. Survival outcomes of very small drug-eluting beads used in chemoembolization of unresectable hepatocellular carcinoma. J Vasc Interv Radiol. 2019;30(9):1325-1334.e2. https://doi.org/10.1016/j.jvir.2019.05.006.
Urbano J, et al. Multicentre prospective study of drug-eluting bead chemoembolisation safety using tightly calibrated small microspheres in non-resectable hepatocellular carcinoma. Eur J Radiol. 2020. https://doi.org/10.1016/j.ejrad.2020.108966.
Malagari K, et al. Five-years outcome analysis of 142 consecutive hepatocellular carcinoma patients treated with doxorubicin eluting microspheres 30–60 μm: results from a single-centre prospective phase II trial. Cardiovasc Intervent Radiol. 2019;42(11):1551–62. https://doi.org/10.1007/s00270-019-02260-3.
Kang YJ, et al. Conventional versus small doxorubicin-eluting bead transcatheter arterial chemoembolization for treating barcelona clinic liver cancer stage 0/A hepatocellular carcinoma. Cardiovasc Interv Radiol. 2020;43(1):55–64. https://doi.org/10.1007/s00270-019-02349-9.
Balli H, Aksungur E, Khalatai B, Aikimbaev K. Super-selective transarterial chemoembolization with doxorubicin-loaded drug-eluting beads sized below and above 100 microns in hepatocellular carcinoma: a comparative study. J Belgian Soc Radiol. 2019. https://doi.org/10.5334/JBSR.1841.
Greco G, et al. Transarterial chemoembolization using 40 µm drug eluting beads for hepatocellular carcinoma. World J Radiol. 2017;9(5):245. https://doi.org/10.4329/wjr.v9.i5.245.
Deipolyi AR, Oklu R, Al-Ansari S, Zhu AX, Goyal L, Ganguli S. Safety and efficacy of 70–150 μm and 100–300 μm drug-eluting bead transarterial chemoembolization for hepatocellular carcinoma. J Vasc Interv Radiol. 2015. https://doi.org/10.1016/j.jvir.2014.12.020.
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Consent for Publication
Consent for publication was obtained for every individual person’s data included in the study.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cascella, T., Garanzini, E.M., Lanocita, R. et al. Long Term Survival Analysis in a Cohort of 125 Patients with Hepatocellular Carcinoma Treated with Transarterial Chemoembolization Using Small Drug Eluting Beads. Cardiovasc Intervent Radiol 45, 54–61 (2022). https://doi.org/10.1007/s00270-021-02991-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-021-02991-2