Abstract
Background
Advances in surgical techniques have significantly improved the safety of thyroidectomy. Quality of life issues, such as voice changes, however continue to be important considerations. This study evaluated the prevalence and determinants of voice changes following thyroidectomies for non-malignant goiters in a Nigerian Hospital.
Methodology
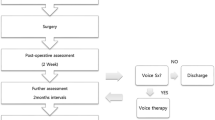
Consecutive adults who had thyroidectomy for non-malignant goiters were evaluated. Preoperatively, each participant had laryngoscopy and voice assessment using the Voice Handicap Index-10. At surgery, the intubation difficulty score, size of endotracheal tubes, and duration of operation were recorded. Laryngoscopy and VHI-10 assessments were repeated 1 week, 1 month, and 3 months after surgery. Pre and postoperative assessments were compared.
Result
Fifty-four patients completed the study. Subtotal thyroidectomy was the commonest operation performed in 17 patients (31.48%), with 14 (25.93%) having total thyroidectomy. Baseline median VHI-10 score was 6.5(IQR-10). Five patients had abnormal preoperative laryngoscopy findings (benign vocal cord lesions). Postoperatively, seven patients had endoscopic evidence of vocal cord paralysis, six were unilateral while one was bilateral. Ten patients (18.5%) had early voice changes. Median VHI-10 score at one week was significantly higher than baseline (10 vs. 6.5, p = 0.01). At 3 months, VHI-10 reverted back to baseline in five of the ten patients while five patients (9.3%) had persistent voice changes. Abnormal endoscopic findings predicted the occurrence of early postoperative voice changes.
Conclusion
Thyroidectomy for non-malignant goiters is associated with transient voice changes, many of which revert to normal over time. Abnormal endoscopic findings predict its occurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Improvements in surgical and anesthetic techniques coupled with the advent of precise electrosurgical and monitoring devices have significantly revolutionized surgical practice in general [1, 2]. Thyroidectomy has particularly benefited immensely from these innovations with excellent outcomes reported globally. Over the years, outcomes such as mortality have significantly reduced to near negligible rates making thyroidectomy a relatively safe operation to perform. Most discussions around thyroidectomy, therefore, focus on its effects on quality of life issues such as recurrent laryngeal nerve injury and voice changes.
When it occurs, voice changes can be associated with significant social, emotional, and in some instances, economic challenges [3]. Beyond inadvertent injury to the nerves during operation, other factors such as intubation trauma and pressure injuries to the recurrent laryngeal nerves by the endotracheal tube have been described as possible mechanisms for developing postoperative voice disorders [4, 5].Traditionally, preoperative indirect laryngoscopy is often performed to document the preoperative state of the vocal cords as a marker of the integrity of the laryngeal nerves. This practice although recommended is not routinely practiced by all thyroid surgeons worldwide [6, 7]. Where these practices are not routine, the true incidence of recurrent laryngeal nerve injury cannot be determined, given the possibility of asymptomatic nerve injury. Similarly, routine voice assessment post-thyroidectomy is not often conducted except when there are major voice changes. It is therefore possible for some forms of vocal dysfunction following thyroidectomy to remain undiagnosed or unreported. These postoperative events are not frequently evaluated, particularly in non-specialized centers where the majority of thyroid operations are performed [8]. Their effect on quality of life has also not been comprehensively evaluated.
In Nigeria, where goiter is endemic and often ignored until they assume enormous sizes [9], it will be ideal to evaluate the pattern of morbidities associated with thyroid operations. This study was conducted to evaluate the pattern and determinants of post-thyroidectomy voice changes in a Nigerian cohort.
Patients and methods
Study design
This was a cohort study of patients undergoing thyroidectomy for benign goiters at a Nigerian tertiary health hospital (Obafemi Awolowo University Teaching Hospital, Ile-Ife) between January 2019 and December 2020.
Consecutive adults scheduled for thyroidectomies on account of benign goiters were included in the study. Patients undergoing revision thyroid surgery were excluded. All patients with postoperative diagnosis of incidental thyroid malignancy were retrospectively excluded from the study.
Preoperative assessment
Preoperatively, each participant completed the Vocal handicap index-10 (VHI-10) questionnaire which is a validated tool for voice assessment. Preoperative fiber-optic laryngoscopy was performed in all patients within 1 week of surgery.
Intra-operative assessment
Intra-operatively, the ease of endotracheal intubation was assessed using the intubation difficulty score. Other details such as duration of surgery (taken as time interval from the commencement of skin incision to the point at which the last skin suture is completed), duration of thyroidectomy, duration of anesthesia and type of thyroidectomy were recorded. Type of thyroidectomy was classified as partial (lobectomy + isthmusectomy), subtotal thyroidectomy (removal of the thyroid gland leaving about 4–5 g on each side), near total thyroidectomy (removal of all the thyroid gland leaving only a little amount of thyroid tissue, estimated at about 1 g) and total thyroidectomy (removal of all thyroid tissue).
Postoperative assessment
Repeat VHI-10 and laryngoscopy were done at 1 week, 1 month, and 3 months post-thyroidectomy. Patients who had persistent nerve injuries at 3 months had additional laryngoscopies up to one year.
Data analysis
All collected data were entered into a computer for analysis using SPSS 22.
Variables of interest included socio-demographic details, VHI scores, IDS, Endotracheal tube sizes and intra-operative events such as type of thyroidectomy, duration of anesthesia and duration of surgery.
A 6-point change in VHI-10 score from baseline was considered to be clinically significant [10]. Median VHI-10 score was calculated and the significance of any change between the preoperative and postoperative scores was determined using Wilcoxon signed test. The relationship between change in baseline VHI-10 score and anesthetic considerations such as intubation difficulty and size of endotracheal tube was determined by Chi square test, while the relationship between change in VHI-10 and duration of surgery and anesthesia were determined using the two-sample t test with equal variance and the level of significance set at p < 0.05. Multivariate analysis was carried out to determine the factors associated with abnormal voice changes. Selection of variables included in the multivariate model was based on result of the univariate analysis. Only factors which were significant in the univariate analysis were included in the multivariate analysis.
Ethical issues
Ethical approval was obtained from the institutional ethics committee before commencement of the study.
Results
Baseline characteristics
A total of 54 participants made up of six males and 48 females completed the study. The median duration of symptoms before presentation was 5 years. Subtotal thyroidectomy was the most common form of thyroidectomy (17, 31.5%), 14 patients (25.9%) had total thyroidectomy, 12 (22.2%) had near total while 11 patients (20.4%) had partial thyroidectomy. The majority (90.7%) had normal baseline endoscopic findings with five patients having vocal cord abnormalities, mainly benign vocal cord lesions (Table 1). The median baseline VHI-10 score for the entire cohort was 6.5. There was no significant difference in the baseline VHI-10 between participants with normal and abnormal preoperative laryngoscopic findings (p = 0.94) (Table 1). The median duration of surgery was 60 min, with about one-third of the patients having moderate to severe difficulty with intubation (Table 2).
One week post-surgery assessment
VHI-10 scores
Ten participants (18.5%) had clinically significant change in their VHI-10 values (≥ 6 points increase from baseline) at 1 week. Median postoperative VHI-10 at 1 week was 10 (IQR 12) which was statistically higher than the baseline score of 6.5, p = 0.01.
Laryngoscopy findings
Seven patients (12.9%) had endoscopic features of vocal cord paralysis. Six of these were unilateral while one was bilateral. Of these, four (57.1%) had significant change in their VHI scores while 3 (42.86%) did not.
Factors associated with abnormal voice changes at 1 week
Abnormal postoperative laryngoscopy at one week was significantly associated with change in VHI-10 score (p ≤ 0.01). Extent of thyroidectomy was also associated with clinically significant change in VHI-10 score with total thyroidectomy being more frequently associated with voice changes (p = 0.03) (Table 3). Neither duration of surgery (p = 0.99), anesthesia (p = 0.98), size of endotracheal tube (p = 0.71) nor intubation difficulty showed any significant association with voice changes observed at one week post-surgery.
One month post-surgery assessment
VHI-10 scores
At one month post-surgery, two of the ten patients with significant VHI-10 change had reverted to baseline while eight still had significant changes from their baseline VHI-10 values.
Laryngoscopy findings
One patient (1.85%) was noticed to have a large vocal cord mass at laryngoscopy (Fig. 1). The patient had clinically significant change from baseline VHI-10 score. The VHI-10 score in this patient reverted to normal after excision of the mass. Histology of the mass confirmed the suspicion of a vocal cord granuloma.
Three months post-surgery assessment
VHI-10 scores
An additional three patients had reverted to baseline VHI-10 score leaving five patients (9.3%) with persistent change in VHI-10 score at 3 months. Overall median VHI-10 score at 3 months was not significantly different from baseline [8 (IQR-10) vs 6.5(10)].
Laryngoscopy findings
Endoscopy at 3 months revealed the persistence of preoperative vocal cord lesions in the five patients with abnormal vocal cord findings at baseline. Forty-four patients (81.5%) had normal laryngoscopy findings while two of the seven patients with vocal cord paralysis at 1 week had reverted to normal. Five patients (9.3%) however had vocal cord paralysis persisting till the third month. Of the five, four were unilateral, of which three were asymptomatic while one had hoarseness of voice. One patient had bilateral vocal cord paralysis (Table 4). At all time points, abnormal endoscopy finding was associated with significant change in VHI-10.
Endoscopic evaluation of patients with persistent vocal cord paralysis
Further evaluation of patients with vocal cord paralysis at about one year post-surgery showed that two of the five patients with abnormal vocal cord findings had reverted to normal, leaving three with endoscopic features of vocal cord paralysis (5.6%). Of the three, two were asymptomatic while one patient (1.8%) had symptomatic vocal cord paralysis.
Predictors of abnormal VHI-10 score
On univariate analysis, abnormal endoscopic findings at 1 week, 1 month and 3 months and the type of thyroidectomy were significantly associated with early postoperative voice changes. On multivariate analysis, abnormal endoscopic finding at 1 week was the only predictor of early postoperative voice change (Table 5). Persistent voice change at 3 months was significantly associated with abnormal endoscopic findings at 1 week, 1 month and 3 months. None of these was however significant on multivariate analysis (Table 6).
Discussion
This study established the presence of early postoperative voice changes in about one-fifth of patients with a steady decline over time. At three months, half of those with voice changes had reverted to normal highlighting the transient nature of some of the voice abnormalities. The extent of thyroidectomy and the presence of abnormal postoperative endoscopic findings were found to be associated with voice changes but only the former correctly predicted the occurrence of voice changes on multivariate analysis.
Voice assessment post-thyroidectomy has been evaluated in various settings using different tools. This accounts for the wide range of outcomes reported across various studies [11, 12]. Our study utilized the VHI-10 tool and reported prevalence of 9.3% at 3 months. Kovatch et.al in a review of 2325 patients using the same tool reported an incidence of 12.7% at 3 months [13] while Borel et.al in another study of 203 patients reported an incidence of 5.7% [14]. The assessment of voice changes post-thyroidectomy using this tool is novel in Nigeria, and therefore serves as a reference for further studies in the locality.
A spectrum of post-thyroidectomy voice changes ranging from vague symptoms to weakened vocal strength to severe hoarseness has been described [5, 15]. The decline in the prevalence of voice changes with gradual restoration of voice quality over time has also been reported by other studies. Among those with persistent voice changes, however, it is necessary to carefully seek for possible reasons as this may have resulted from an underlying nerve injury. The possibility of this resulting from other causes should also be borne in mind. In this study, a vocal cord granuloma was observed in one of the patients in this study, with restoration of voice quality after excision. A similar finding has been reported by a few studies [16, 17]
This study showed that clinically detectable voice changes were significantly associated with surgical complexity. Understandably, patients undergoing more extensive thyroid surgeries involving bilateral dissections have a higher risk of voice changes. Such operations involve a greater amount of dissection with more postoperative edema and subsequent fibrosis which may potentially change the aerodynamic quality of the larynx resulting in voice changes. Furthermore, such extensive dissections also put the laryngeal nerves at risk on both sides with higher chances of injuries [18]. Meticulous dissection and careful identification of the laryngeal nerve at surgery help to reduce the rate of nerve damage during thyroidectomy [19,20,21]. In our practice, the safety and speed of thyroidectomy has continued to improve with the advent of electrosurgical devices such as the Ligasure© vessel sealing device [2, 22, 23]. With the use of this device, complex dissections can be rapidly accomplished in a relatively bloodless field.
Of the factors associated with early voice changes, abnormal postoperative endoscopy was the only significant predictor identified on multivariate analysis. This pattern indicates the significant contribution of vocal cord paralysis to the occurrence of voice changes. This association was no longer seen at 3 months, apparently due to the recovery of some of the early postoperative vocal cord palsies. It should be noted however that voice changes may sometimes occur in the absence of nerve injury [24, 25].
This study found no association between abnormal preoperative laryngoscopy and postoperative voice changes. Although about 9.3% of patients had various benign vocal cord lesions, this did not reflect in the VHI-10 values preoperatively or after surgery. It is noteworthy; however, that the VHI-10 being a self-reporting tool may be insensitive in detecting subtle long-standing voice changes that an individual might have adjusted to. Consequently, patients with subtle long-standing voice changes may return normal scores.
Although this study focused primarily on voice changes, its interrelatedness with nerve injury and the clinical significance of nerve paralysis makes it an important subject. Serial endoscopic assessment of the vocal cords as performed in this study is quite novel for a Nigerian series. The proportion of patients who were asymptomatic despite having endoscopic evidence of nerve injury highlights the importance of objective vocal cord assessment in order to avoid under-reporting. Earlier studies in Nigeria on outcomes of thyroidectomy have reported varying rates of recurrent laryngeal nerve injury, ranging from 2.8 to 9.7% [26, 27]. The majority of these are however retrospective in design, with limited description of the methodology used in determining the occurrence of nerve injury. None of these also reported performing routine endoscopic assessment of the vocal cords postoperatively. These differences in study design limit the comparability of our findings with local data. Relative to high income countries, however, the nerve injury rate reported in this study is higher than the 0.3–3% reported in some series [28]. Although the majority were temporary, the proportion of patients with persistent nerve injury at one year (5.5%) exceeds the threshold. While the data in this study are not robust enough to adequately determine the predictors of nerve injury, factors such as operative volume, gland size and the practice of routine nerve identification are important factors to consider. In this study, of the three patients with persistent nerve injury at one year, two were operated by less experienced surgeons. In our setting, goiters tend to assume enormous sizes before patients present to the hospital for treatment. In an earlier series from our institution, the mean thyroid weight was 120 g which exceeds reports from high income countries [2, 29]. Furthermore, routine identification of the recurrent laryngeal nerve, which is an important step in the operation was not standardized in this study. All these factors have been associated with nerve injury and their contribution to nerve injury in our practice needs to be evaluated [30,31,32]. Building on our findings, another study which is evaluating the predictors of recurrent nerve injury, incorporating these variables is currently underway.
Findings from this study must be interpreted within its limits. The use of the VHI-10, though validated is based on patients’ self-report which is subjective. Other variables such as the size of the gland and degree of fibrosis and lifestyle behaviors such as smoking which may affect outcomes were not included in the analysis. Follow-up of patients with voice changes in this study was limited to three months. A longer follow-up period could have helped determine the long-term voice profile of patients in this study. This study only documented the occurrence of voice changes but did not evaluate its impact on everyday life. This would have been of greater clinical significance. Multivariate analysis in this study was carried out on a limited sample, a more robust analysis with a larger sample size will certainly shed more light on the subject.
Within these limits however, we conclude that post-thyroidectomy voice changes are commoner in the early postoperative period with a steady decline over time. Abnormal endoscopic finding is a predictor of its occurrence.
References
Cheng H, Soleas I, Ferko NC, Clymer JW, Amaral JF (2015) A systematic review and meta-analysis of harmonic focus in thyroidectomy compared to conventional techniques. Thyroid Res 8:15
Arowolo OA, Olasehinde O, Adisa AO, Adeyemo A, Alatise OI, Wuraola F (2019) Early experience with ligasure thyroidectomy in a Nigeria teaching hospital. Niger J Surg Off Publ Niger Surg Res Soc 25:64
Ruben RJ (2000) Redefining the survival of the fittest: communication disorders in the 21st century. Laryngoscope 110:241
Mencke T, Echternach M, Kleinschmidt S, Lux P, Barth V, Plinkert PK et al (2003) Laryngeal morbidity and quality of tracheal intubation a randomized controlled trial. J Am Soc Anesthesiol 98:1049–1056
de Pedro NI, Fae A, Vartanian JG, Barros APB, Correia LM, Toledo RN et al (2006) Voice and vocal self-assessment after thyroidectomy. Head Neck 28:1106–1114
Lee CY, Long KL, Eldridge RJ, Davenport DL, Sloan DA (2014) Preoperative laryngoscopy in thyroid surgery: Do patients’ subjective voice complaints matter? Surgery 156:1477–1483
Schlosser K, Zeuner M, Wagner M, Slater EP, Fernández ED, Rothmund M et al (2007) Laryngoscopy in thyroid surgery––essential standard or unnecessary routine? Surgery 142:858–864
BAETS (2007) British association of endocrine surgeons second national audit report. Dendrite Clinical Systems, Oxford
Chuhwak E, Ohwovoriole AE (2005) Clinical features of goitres on the Nigerian Plateau. Niger Postgrad Med J 12(4):2
Misono S, Yueh B, Stockness AN, House ME, Marmor S (2017) Minimal important difference in voice handicap index-10. JAMA Otolaryngol Head Neck Surg 143(11):1098–1103
Tedla M, Chakrabarti S, Suchankova M et al (2016) Voice outcomes after thyroidectomy without superior and recurrent laryngeal nerve injury: VoiSS questionnaire and GRBAS tool assessment. Eur Arch Otorhinolaryngol 273:4543–4547. https://doi.org/10.1007/s00405-016-4163-6
Shin Y, Hong K, Hong Y, Oh J, Yoon Y, Lee H (2014) Aerodynamic analysis of voice in patients with thyroidectomy. J Korean Thyroid Assoc 7(1):77–82
Kovatch KJ, Reyes-Gastelum D, Hughes DT, Hamilton AS, Ward KC, Haymart MR (2019) Assessment of voice outcomes following surgery for thyroid cancer. JAMA Otolaryngol Head Neck Surg 145:823–829
Borel F, Christou N, Marret O, Mathonnet M, Caillard C, Bannani S et al (2018) Long-term voice quality outcomes after total thyroidectomy: a prospective multicenter study. Surgery 163:796–800
Chun BJ, Bae JS, Chae BJ, Hwang YS, Shim MR, Sun DI (2012) Early postoperative vocal function evaluation after thyroidectomy using thyroidectomy related voice questionnaire. World J Surg 36(10):2503–2508. https://doi.org/10.1007/s00268-012-1667-0
Liang TJ, Wang NY, Liu SI et al (2021) Vocal cord granuloma after transoral thyroidectomy using oral endotracheal intubation: two case reports. BMC Anesthesiol 21:170. https://doi.org/10.1186/s12871-021-01393-8
Echternach M, Maurer C, Mencke T, Schilling M, Verse T, Richter B (2009) Laryngeal complications after thyroidectomy: Is it always the surgeon? Arch Surg 144(2):149–153
Hermann M, Keminger K, Kober F (1991) Risk factors of recurrent nerve palsy: a statistical analysis of 7566 thyroid operations. Chirurgie 62:182–188
Rathi PK, Shaikh AR, Shaikh GA (2010) Identification of recurrent laryngeal nerve during thyroidectomy decreases the risk of nerve injury. Pak J Med Sci 26(1):148–151
Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W (2002) Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope 112(1):124–133
Kim SY, Kim GJ, Lee DH, Bae JS, Lee SH, Kim JS, Hwang YS, Shim MR, Park YH, Sun DI (2020) Voice change after thyroidectomy without vocal cord paralysis: analysis of 2,297 thyroidectomy patients. Surgery 168(6):1086–1094
Moran K, Grigorian A, Elfenbein D, Schubl S, Jutric Z, Lekawa M et al (2020) Energy vessel sealant devices are associated with decreased risk of neck hematoma after thyroid surgery. Updat Surg 72:1135–1141
Cheng H, Soleas I, Ferko NC, Clymer JW, Amaral JF (2015) A systematic review and meta-analysis of harmonic focus in thyroidectomy compared to conventional techniques. Thyroid Res 8:1–13
Sinagra DL, Montesinos MR, Tacchi VA, Moreno JC, Falco JE, Mezzadri NA, Debonis DL, Curutchet HP (2004) Voice changes after thyroidectomy without recurrent laryngeal nerve injury. J Am Coll Surg 199(4):556–560. https://doi.org/10.1016/j.jamcollsurg.2004.06.020
Akyildiz S, Ogut F, Akyildiz M, Engin EZ (2008) A multivariate analysis of objective voice changes after thyroidectomy without laryngeal nerve injury. Arch Otolaryngol Head Neck Surg 134(6):596–602. https://doi.org/10.1001/archotol.134.6.596
Afolabi AO, Ayandipo OO, Afuwape OO, Ogundoyin OA (2016) A fifteen year experience of total thyroidectomy for the management of simple multinodular goitres in a low medium income country. S Afr J Surg 54(4):40–45
Samuel SA, Rebecca SH (2019) Complications of thyroidectomy at a tertiary health institution in Nigeria. Sub Sahar Afr J Med 6(1):1
Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R (2009) Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract 63(4):624–629
Gardiner KR, Russell CF (1995) Thyroidectomy for large multinodular colloid goitre. J R Coll Surg Edinb 40(6):367–370
Tsuzuki N, Wasano K, Kawasaki T, Sasaki SI, Ogawa K (2019) Thyroid lobe size predicts risk of postoperative temporary recurrent laryngeal nerve paralysis. Laryngosc Investig Otolaryngol 4(6):708–713
Godballe C, Madsen AR, Sørensen CH, Schytte S, Trolle W, Helweg-Larsen J, Barfoed L, Kristiansen L, Sørensen VZ, Samuelsen G, Pedersen HB (2014) Risk factors for recurrent nerve palsy after thyroid surgery: a national study of patients treated at Danish departments of ENT head and neck surgery. Eur Arch Otorhinolaryngol 271(8):2267–2276
Zakaria HM, Al Awad NA, Al Kreedes AS, Al-Mulhim AM, Al-Sharway MA, Hadi MA, Al Sayyah AA (2011) Recurrent laryngeal nerve injury in thyroid surgery. Oman Med J 26(1):34
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author’s declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Adeyemo, A., Olasehinde, O., Owojuyigbe, A.M. et al. Prevalence and Predictors of Post-Thyroidectomy Voice Dysfunction in a Nigerian Cohort. World J Surg 47, 682–689 (2023). https://doi.org/10.1007/s00268-022-06858-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-022-06858-6