Abstract
Background
Some of patients are suffered from pitch lowering of voice after thyroidectomy. We sought to identify factors predictive of a recovery from lowered pitch voice after thyroid surgery.
Methods
We retrospectively reviewed the records of 133 patients who underwent total thyroidectomy to treat papillary carcinoma between January 2012 and February 2013. Of these, we enrolled 78 who exhibited a lower-pitched voice (SFF fall > 12 Hz) at 2 weeks post-operatively than pre-operatively and investigated pitch recovery after 3 months. We subclassified patients into recovery and non-recovery groups and compared videostroboscopic findings, acoustic voice data, and thyroidectomy-related voice questionnaire scores pre-operatively and 2, 8, and 12 weeks post-operatively.
Results
Vocal cord asymmetry on videostroboscopic examination at 2 weeks post-operatively (odds ratio 19.056, p = 0.001*) was more frequent in the non-recovery group. In acoustic analysis, mean pre-operative SFF was higher in the non-recovery group than the recovery group (190.9 ± 27.5 and 180.9 ± 24.6 Hz, respectively; p = 0.030*). Also, a reduction in the SFF of > 19.6 Hz, at 2 weeks post-operatively versus pre-operatively, predicted non-recovery of pitch-lowering in patients with reduced SFF within post-operative 3 months, with 72.0% sensitivity and 71.2% specificity. After 6 months of follow-up, no patient who exhibited an SFF fall > 19.6 Hz recovered to within 10 Hz of the pre-operative value.
Conclusion
A reduction in the speaking fundamental frequency (SFF) > 19.6 Hz at 2 weeks post-operatively predicted persisting lowering of voice pitch after thyroidectomy among those with lower-pitched voices after surgery. Pre-operative high SFF and post-operative stroboscopic findings including vocal cord asymmetry at 2 weeks post-operatively also predicted persisting lowering of voice pitch for 3 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Voice problems after thyroid surgery are well-known and may be temporary or permanent. Early detection and management can improve patient outcomes and quality-of-life [1]. Recurrent laryngeal nerve (RLN) injury has been considered to be one of the main causes of voice change after thyroidectomy; the incidence is 0.3–15.4% [2]. However, many other factors also contribute to voice change, including injury to the external branch of the superior laryngeal nerve (EBSLN), changes in lymphatic drainage, laryngeal trauma following intubation, and psychogenic factors [3]. It is thus difficult to identify the exact cause of voice alteration after thyroidectomy because many factors affect vocal outcomes [4]. The most common symptom is pitch-lowering, which reduces vocal frequency, range, and intensity; and increasing perturbations such as shimmer, jitter, and the noise-to-harmonic ratio (NHR). [5,6,7,8,9,10]. According to various reports, 37% [9] to 87% [11] of patients experience vocal changes, including pitch-lowering, soon after surgery, but many recover with time [9]. We previously reported that 18% of patients experienced subjectively lowered pitch at 2 weeks after thyroidectomy [12], and that vocal exercises and indirect voice therapy were helpful [13] in reducing the recovery time. However, 10% of patients did not attain their pre-operative status. Thus, we examined patients who exhibited prolonged lower pitch after surgery and identified predictive factors.
Materials and methods
Patients
We retrospectively reviewed the records of 133 consecutive patients who underwent total thyroidectomy to treat papillary carcinoma of the thyroid between January 2012 and February 2013 at Seoul St. Mary’s Hospital, Catholic University of Korea. We selected only female patients. Patients meeting any of the following criteria were excluded: (1) a history of head-and-neck surgery; (2) scheduled for modified radical neck dissection; (3) scheduled for partial laryngeal or tracheal resection; (4) scheduled for lobectomy only; (5) abnormal findings (vocal nodules, polyps, or paralysis) evident on pre-operative laryngeal examination; and/or (6) vocal cord paralysis developing after surgery.
Thyroidectomy technique
All patients were operated on by one general surgeon using the same surgical technique and under the same conditions. During surgery, the strap musculature was retracted laterally from the midline but was not completely divided in any of the patients. Total thyroidectomy was performed by extracapsular dissection to remove both thyroid lobes and the pyramidal lobe (when present). All recurrent laryngeal nerves were identified and the superior thyroid artery and vein were individually ligated on the thyroid capsule to avoid injury to the external branch of the superior laryngeal nerve. When the external branch of the superior laryngeal nerve could not be readily identified, no further dissection was performed. In endoscopic surgery, transaxillary endoscopic surgery was performed. A vertical incision in axilla was made, and subcutaneous dissection was done to avascular space of the sternocleidomastoid muscle(SCM) branches and thyroid gland beneath the strap muscle. After exposure of thyroid gland, all the surgical procedure was same as open thyroidectomy.
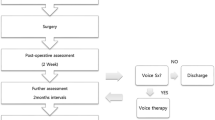
Study design
All patients underwent pre- and post-operative voice evaluation, including videostroboscopy, acoustic analysis [fundamental frequency (F0), speaking fundamental frequency (SFF), jitter, shimmer, and the NHR], and completion of the thyroidectomy-related voice questionnaire (TVQ; developed in our institution). Post-operative examinations were performed at 2, 8, 12, and 24 weeks after surgery.
We used the SFF to evaluate pitch. The SFF is the average F0 (the lowest frequency of a complex periodic sound) measured during performance of a vocal or speech task and is a basic acoustic measure used for clinical evaluation of voice disorders. To identify patients with lower-pitched voices, the SFFs were compared before and after surgery. Changes in all patients were calculated (post-operative change in SFF, ΔSFF: pre-operative SFF minus post-operative SFF).
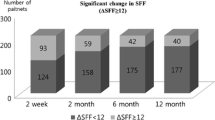
We defined pitch-lowered patients by reference to the post-operative SFF. Debruyne et al. reported that post-operative SFF was decreased by an average of 11.59 Hz at 4 days and the reduction in SFF was resolved(less than 5 Hz) within 15 days [6]. Above that research, Soylu et al. [9] reported that mean 11.0 Hz drop of F0 was observed through 3 months after surgery in thyroidectomy patients. They also revealed that patients who complained subjective voice disturbance showed 12.86 Hz of F0 drop at post-operative 3 months. According to those previous data, we set a reference value for defining pitch-lowered group as patients who exhibited pitch lowering of SFF(ΔSFF) > 12 Hz until 2 weeks after thyroidectomy. Patients who exhibited SFF decrease more than 10 Hz were categorized as non-recovery group through follow-up period (Fig. 1). Previously reported literatures suggested that most of patients who had voice problem after thyroidectomy were gradually restored after 3 months [3, 9], so we observed and assessed recovery from pitch lowering during 3 months.
No patient engaged in vocal exercises or underwent indirect voice therapy during follow-up. All subjects were informed of the nature of the study and gave written informed consent. The Institutional Review Board of Seoul St. Mary's Hospital approved this retrospective review of medical records.
Acoustic analysis
Patients were instructed to produce the vowel ‘a’ at a comfortable volume and constant pitch for at least 3 s. Each pronunciation was recorded at a constant mouth-to-microphone distance of 5 cm using a Computerized Speech Lab (CSL) (model 4150; KayPENTAX, Lincoln Park, NJ, USA). The task was repeated at least four times, and the fourth trial was commonly used for analysis by the Multi-Dimensional Voice Program platform (MDVP) (model 5105, ver. 3.1.7; KayPENTAX). We analyzed the F0 and perturbations of F0 (jitter), amplitude (shimmer), glottal noise (the NHR), and the SFF. To analyze SFF, all the patients were instructed to read “Sanchaek” (“A Walk”) sentences at a comfortable volume and rate.
Videostroboscopy
Pre-operatively, and 2 weeks after surgery, we examined the entire larynx employing videolaryngostroboscopy (model 9200C; KayPENTAX). Any diagnosis of disease was made, and any abnormal finding was noted, by two speech therapists and one otolaryngologist working in consensus. Post-operative vocal asymmetry, gap, edema, injection, tension, mucus presence, and subglottic edema were carefully recorded.
The TVQ
The TVQ was designed in our institution to assess vocal function. As reported previously [14], the TVQ comprises 20 questions; each response is scored from 0 (no voice alteration or symptom) to 80 (highest voice impairment with multiple vocal symptoms). The TVQ is a self-assessment tool measuring voice quality. We earlier showed that the questionnaire simply and effectively detected pre- and post-thyroidectomy voice-related disorders.
Statistical analysis
Statistical analyses were performed using SPSS for Windows software (ver. 25.0; SPSS Inc., Chicago, IL, USA). First, univariate analysis was used to identify factors significantly associated with recovery of lowered pitch. The paired t-test was employed to compare acoustic and stroboscopic data between the recovery and non-recovery group. Fisher’s correlation analysis was used to identify stroboscopic findings that significantly affected recovery from lowered pitch. Factors that were potentially prognostic in univariate analyses were entered into multivariate logistic regression analysis. A ΔSFF cutoff at the first visit predictive of recovery of lowered pitch was chosen to maximize the sensitivity and specificity of receiver operation characteristic (ROC) curve analysis. A p-value < 0.05 was considered to reflect statistical significance.
Results
Among 133 patients, 3 patients showed post-operative vocal cord paralysis and were thus excluded. Any other abnormal laryngeal condition was not found by stroboscopic examination. In total, 78 patients out of the 130 who exhibited a fall in pitch of > 12 Hz at 2 weeks after surgery were included and followed-up for 3 months. Of the 78 patients, 53 (67.9%) recovered and 25 (32.1%) did not; we divided these patients into two groups. Table 1 shows a summary of the results. The mean age of all 78 patients, and that of the recovery and non-recovery group, was 53.2, 52.2, and 55.2 years, respectively, and did not differ significantly (p = 0.260). TNM status, smoking history, current smoking status, site of the lesion, and mean lesion size did not differ significantly between the two groups (Table 1).
Videostroboscopic findings and recovery
On videostroboscopy performed at 2 weeks after surgery, vocal cord asymmetry and edema, and decreased tension were more frequent in the non-recovery group, with statistical significance (p = 0.001*, 0.045*, and 0.050*, respectively) (Table 2). We used Fisher’s exact test to explore the relationships between videostroboscopic findings and recovery of lowered pitch; the presence of vocal cord asymmetry significantly decreased the probability of recovery from pitch lowering (OR 19.06, p = 0.001*, Table 3). The presence of decreased vocal cord tension and vocal cord edema was also investigated, as potential risk factors for non-recovery of the voice after pitch lowering, but statistical significance was not attained (odds ratio, 5.95, p = 0.089; odds ratio, 2.857, p = 0.154, respectively).
Univariate analysis of acoustic parameters and the TVQ score
Acoustic parameters and TVQ results were compared between the recovery and non-recovery groups via univariate analysis (Table 4). The mean pre-operative SFF was higher in the non-recovery group than the recovery group (190.9 ± 27.5 and 180.9 ± 24.6 Hz, respectively; p = 0.030*). The ΔSFF at 2 weeks post-operatively differed significantly between the two groups. In the recovery group, the fall in pitch was 20.1 ± 7.4 Hz, but it was 31.3 ± 11.9 Hz in the non-recovery group; the difference was significant (p = 0.021*). At 8 weeks post-operatively, the difference remained significant (8.5 ± 2.7 Hz in the recovery group, 22.5 ± 8.9 Hz in the non-recovery group; p = 0.042*); this was also true at 12 weeks. The changes in F0 after surgery were similar to those in SFF, but the two groups did not differ significantly, except at 12 weeks post-operatively. None of jitter, shimmer, or the NHR differed between the groups. TVQ score also did not show statistical difference.
Multivariate analysis of acoustic parameters and the TVQ score
Univariate analysis showed that the pre-operative SFF and ΔSFF at post-operative day (POD) 2 weeks significantly predicted recovery from pitch-lowering after thyroidectomy at POD 3 months. We subjected these parameters including SFF at POD 2 weeks to logistic regression analysis (Table 5). The logistic regression analysis revealed that pre-operative SFF and ΔSFF at POD 2 weeks significantly predicted recovery (p = 0.024* and 0.001*, respectively). Thus, those with greater ΔSFFs at 2 weeks post-operatively were at the most risk.
Choice of screening parameters
Logistic regression indicated that the ΔSFF at 2 weeks post-operatively predicted recovery from pitch-lowering; we sought a suitable cutoff value. The ROC recovery curves (Fig. 2) revealed areas under the curve (AUCs) of 0.680, 0.466, and 0.752 for the pre-operative SFF, the post-operative SFF at 2 weeks, and the ΔSFF, respectively. Thus, the latter parameter exhibited the strongest correlation with recovery. The optimal cutoff was 19.6 Hz (72.0% sensitivity and 71.2% specificity).
Receiver operating characteristics (ROC) curves of recovery from lowered pitch. A. Blue line: change in speaking fundamental frequency (SFF); B. Green line: pre-operative SFF, C. Grey line: post-operative SFF. The curve shows the changes in SFF as the voice recovered (area under curve [AUC] = 0.752, cutoff = 19.6 Hz)
Long-term results
Of all enrolled patients, nine were followed-up for 6 months after surgery. We divided the patients into two groups (Table 6) by reference to the ΔSFF cutoff and investigated F0 and SFF status. Figures 3 and 4 show the SFF data, and Table 6 the summarized results. Four patients exhibiting pitch-lowering of > 19.6 Hz at 2 weeks post-operatively (Group 2) recovered after 6 months but did not attain their pre-operative SFFs. The lowest difference between the pre-operative and 6-month values was 11 Hz, and the mean difference was 26.0 ± 9.7 Hz (Table 6). For those with ΔSFFs < 19.6 Hz at 2 weeks post-operatively (Group 1), the figures were 1 Hz (Fig. 4) and 12.1 ± 5.2 Hz (Table 6). Two of the five Group 1 patients recovered pitch of < 5 Hz by 6 months, but no Group 2 patient recovered. Because of small sample size, we could not get statistical significant p-value.
Discussion
Voice changes are both uncommon and uncomfortable after thyroidectomy. Previously, it was thought that the causes were neurogenic, including injury to the RLN and EBSNL. A thorough knowledge of anatomy and careful surgical technique reduces the incidence of injury [15,16,17]. However, even in the absence of such injury, voice problems may arise, caused by injury to the laryngeal or strap muscles, hormonal changes, emotional problems, or psychogenic issues [9, 11, 18, 19]. Also, endotracheal intubation may cause aerodynamic and acoustic changes, such as a decrease in maximal phonation time and increased vocal perturbation [20]. In terms of objective voice changes after thyroidectomy, pitch-lowering is one of the most common. We earlier found that this occurred in 18% patients, of whom many recovered with time, but 7.3% patients did not recover at 1 year [13, 21]. Van Lierde et al. [22] reported that the 1-week F0 reductions after thyroidectomy averaged 4.5 and 8.6 Hz in females and males, respectively; these gradually recovered to the pre-operative levels by 3 months post-operatively. In contrast, others found that although most patients recovered gradually from pitch-lowering and voice alterations after thyroidectomy, the pitch did not return to the pre-operative level by 6 months in some cases [11]. In the present study, 60% of patients (78/130) exhibited a ΔSFF > 12 Hz both at 2 weeks post-operatively and during the 3-month follow-up period; most patients recovered, but 19.2% (25/130) did not. Thus, we sought a predictive ΔSFF value. A ΔSFF > 19.6 Hz at 2 weeks post-operatively reliably predicted non-recovery (72.0% sensitivity and 71.2% specificity). All such patients did not recover after 6 months, and the mean ΔSFF at that time was 26.0 Hz. We used the data of 6 months to describe long-term voice outcomes after thyroidectomy in this study. More than 1 year follow-up is generally required to address long-term outcomes. However, we previously showed that significant SFF changes at 6 months were similar to those at the 1-year follow-up, and that voice pitch was restored by the 6-month follow-up [21]. Thus, we analyzed our follow-up data up to 6 months assuming that as long term result and predicted that the frequency gap between the recovery and non-recovery groups would be decreased. Against our expectation, we noticed that the frequency gap was maintained up to 6 months, so we have now included the 6-month follow-up results, despite the small patient sample.
Pre-operative high SFF was found to be another significant predictive factor for the SFF recovery in our study. SFF in non-recovery group showed statistically higher value than recovery group (190.9 ± 27.5, 180.9 ± 24.6, respectively, p-value = 0.030*). Similar result with current study was published by Musholt et al. [8], and they reported that pre-operative highest pitch of singing voice is the only strong factor to predict post-operative impairment of vocal performance after thyroid and parathyroid surgery. In other words, patients with excellent pre-operative vocal performances including professional voice users are more prone to usually transient performance reductions.
The etiology of pitch-lowering after thyroidectomy has been interpreted in a number of ways. Sinagra et al. [11] concluded that pitch-lowering might be attributable to a reduction in cord tension, caused by changes in the cricothyroid muscle or the EBSLN. Earlier, we found that reduced cord tension was the most common stroboscopic finding associated with pitch-lowering after thyroidectomy (86% of patients) [13]. In the present study, vocal cord asymmetry was significantly more common in the non-recovery group (odds ratio, 19.056, p = 0.001*). Although statistical significance was not observed, reduced vocal cord tension increased the risk of pitch-lowering (OR 5.950, p = 0.089). The present study was not able to demonstrate a statistically significant association; however, we carefully presumed from those findings that nerve injury by dissection or thermal injury in close proximity of EBSLN creating asymmetrical muscle tone may explain somewhat pitch-lowering after thyroidectomy. However, further studies including laryngeal electromyography (EMG) are required.
Apart from EBSLN injury, strap muscle injury [6, 7], mucosal swelling caused by endotracheal intubation [23], and vascular congestion may cause pitch-lowering after thyroidectomy. Sinagra et al. [11] emphasized the important role of the strap muscle; this constitutes the sole support of the laryngotracheal unit after thyroidectomy. The cited authors remarked that elongation and retraction of the muscle during surgery could produce a functional deficit even in the absence of sectioning. Also, post-operative laryngotracheal adhesion to the strap muscle might be one of the reasons of SFF lowering. Hong et al. [7] suggested that post-operative diminished SFF and frequency range might be the result of laryngotracheal fixation by post-operative scarring after thyroidectomy. They concluded that without injury to the neural structure, impaired vertical movement of larynx which was occurred from the adherence of laryngotrachea, strap muscle, and subcutaneous soft tissue would be resulted in impairment of pitch control after thyroidectomy. Lee et al. [24] recently reported that post-operative decreased SFF after thyroidectomy has been attributed to the impairment of vertical movement of larynx due to laryngotracheal fixation and they draw a conclusion that decreased SFF could be improved by wound massage. It could be one of the reasons for the frequency lowering in early period after thyroidectomy but considering most of those kinds of vocal symptoms are recovered within 3 months, it is not major cause of pitch lowering in our study.
Intraoperative neuromonitoring (IONM) has been increasingly applied to prevent vocal morbidity. The recurrent laryngeal nerve (RLN) IONM thyroidectomy technique was first described in the 1970s. IONM is a valuable tool for identifying the location of RLN and reducing post-operative RLN palsy in high-risk thyroidectomy patients [25]. A recent meta-analysis demonstrated the utility of IONM for lowering the rate of RLN palsy, including temporary palsy, during high-risk thyroidectomy (including cases of re-operation, malignancy, and thyrotoxicosis) [26]. However, other studies reported no benefit of IONM in high-risk thyroidectomies [27, 28]. Furthermore, based on VHI-10 scores, Engelsman et al. [29] failed to verify the usefulness of IONM for improving voice outcomes after thyroidectomy. Despite these equivocal findings, we expect that, with technical improvements in IONM, it will aid preservation of voice quality after thyroidectomy.
Another strategy for improving voice quality is vocal exercise. We previously reported the usefulness of post-operative voice therapy and showed that both indirect and direct voice therapy facilitated restoration of pitch after thyroidectomy [13]. Vocal function exercises, which were developed by Stemple et al. [30], combined with indirect voice therapy improved the pitch recovery rate, but 10% of non-gliding patients failed to regain their pre-operative voice function. To rule out any basis associated with therapeutic compliance, we did not include vocal exercises in the present study. However, voice therapy should be considered a useful option for the treatment of voice impairment after thyroidectomy.
Our study had the following limitations: (1) short follow-up period, (2) small sample size, and (3) lack of EMG data. Despite these limitations, we identified meaningful prognostic factors for recovery of pitch lowering after thyroidectomy. Recently, thyroid weight, post-operative hypocalcemia, vocal cord palsy, and the absence of IONM have been shown to predict poor voice outcomes after thyroidectomy [31]. However, no optimal prognostic factor has been reported yet. Here, we revealed that patients with ΔSFF > 19.6 Hz at 2-weeks POD tended not to show restoration of their pre-operative vocal pitch within 3 months. Future studies should expand these findings to determine the optimal prognostic factors for voice change after thyroidectomy.
Conclusion
From the result of the current study, we figured out that pre-operative high SFF, ΔSFF > 19.6 Hz at POD 2 weeks, and post-operative vocal cord asymmetry evident videostroboscopically could be used for the prediction of non-recovery from lower pitch after thyroidectomy. Thus, it is possible to identify patients who require more concerns about their voice during follow-up after thyroidectomy.
References
Chandrasekhar SS, Randolph GW, Seidman MD et al (2013) Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg 148:S1–37
Steurer M, Passler C, Denk DM et al (2002) Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope 112:124–133
Kuhn MA, Bloom G, Myssiorek D (2013) Patient perspectives on dysphonia after thyroidectomy for thyroid cancer. J Voice 27:111–114
Akyildiz S, Ogut F, Akyildiz M et al (2008) A multivariate analysis of objective voice changes after thyroidectomy without laryngeal nerve injury. Arch Otolaryngol Head Neck Surg 134:596–602
de Pedro NI, Fae A, Vartanian JG et al (2006) Voice and vocal self-assessment after thyroidectomy. Head Neck 28:1106–1114
Debruyne F, Ostyn F, Delaere P et al (1997) Acoustic analysis of the speaking voice after thyroidectomy. J Voice 11:479–482
Hong KH, Kim YK (1997) Phonatory characteristics of patients undergoing thyroidectomy without laryngeal nerve injury. Otolaryngol Head Neck Surg 117:399–404
Musholt TJ, Musholt PB, Garm J et al (2006) Changes of the speaking and singing voice after thyroid or parathyroid surgery. Surgery 140:978–988 discussion 988-979
Soylu L, Ozbas S, Uslu HY et al (2007) The evaluation of the causes of subjective voice disturbances after thyroid surgery. Am J Surg 194:317–322
Stojadinovic A, Shaha AR, Orlikoff RF et al (2002) Prospective functional voice assessment in patients undergoing thyroid surgery. Ann Surg 236:823–832
Sinagra DL, Montesinos MR, Tacchi VA et al (2004) Voice changes after thyroidectomy without recurrent laryngeal nerve injury. J Am Coll Surg 199:556–560
Chun BJ, Bae JS, Chae BJ et al (2012) Early postoperative vocal function evaluation after thyroidectomy using thyroidectomy related voice questionnaire. World J Surg 36:2503–2508. https://doi.org/10.1007/s00268-012-1667-0
Nam IC, Bae JS, Chae BJ et al (2013) Therapeutic approach to patients with a lower-pitched voice after thyroidectomy. World J Surg 37:1940–1950. https://doi.org/10.1007/s00268-013-2167-6
Nam IC, Bae JS, Shim MR et al (2012) The importance of preoperative laryngeal examination before thyroidectomy and the usefulness of a voice questionnaire in screening. World J Surg 36:303–309. https://doi.org/10.1007/s00268-011-1347-5
McIvor NP, Flint DJ, Gillibrand J et al (2000) Thyroid surgery and voice-related outcomes. Aust N Z J Surg 70:179–183
Cernea CR, Nishio S, Hojaij FC (1995) Identification of the external branch of the superior laryngeal nerve (EBSLN) in large goiters. Am J Otolaryngol 16:307–311
Cernea CR, Ferraz AR, Furlani J et al (1992) Identification of the external branch of the superior laryngeal nerve during thyroidectomy. Am J Surg 164:634–639
Jaffe V, Young AE (1993) Strap muscles in thyroid surgery: to cut or not to cut? Ann R Coll Surg Engl 75:118
Vilkman E, Sonninen A, Hurme P et al (1996) External laryngeal frame function in voice production revisited: a review. J Voice 10:78–92
Hamdan AL, Kanazi G, Rameh C et al (2008) Immediate post-operative vocal changes in patients using laryngeal mask airway versus endotracheal tube. J Laryngol Otol 122:829–835
Kim CS, Park JO, Bae JS et al (2017) Long-lasting voice-related symptoms in patients without vocal cord palsy after thyroidectomy. World J Surg 42:2109–2116. https://doi.org/10.1007/s00268-017-4438-0
Van Lierde K, D'Haeseleer E, Wuyts FL et al (2010) Impact of thyroidectomy without laryngeal nerve injury on vocal quality characteristics: an objective multiparameter approach. Laryngoscope 120:338–345
Chun BJ, Bae JS, Lee SH et al (2015) A prospective randomized controlled trial of the laryngeal mask airway versus the endotracheal intubation in the thyroid surgery: evaluation of postoperative voice, and laryngopharyngeal symptom. World J Surg 39:1713–1720. https://doi.org/10.1007/s00268-015-2995-7
Lee JS, Kim JP, Ryu JS et al (2018) Effect of wound massage on neck discomfort and voice changes after thyroidectomy. Surgery 164:965–971
Chan WF, Lang BH, Lo CY (2006) The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery 140:866–872 discussion 872-863
Wong KP, Mak KL, Wong CK et al (2017) Systematic review and meta-analysis on intra-operative neuro-monitoring in high-risk thyroidectomy. Int J Surg 38:21–30
Higgins TS, Gupta R, Ketcham AS et al (2011) Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope 121:1009–1017
Pisanu A, Porceddu G, Podda M et al (2014) Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. J Surg Res 188:152–161
Engelsman AF, Warhurst S, Fraser S et al (2018) Influence of neural monitoring during thyroid surgery on nerve integrity and postoperative vocal function. BJS open 2:135–141
Stemple JC, Lee L, D'Amico B et al (1994) Efficacy of vocal function exercises as a method of improving voice production. J Voice 8:271–278
Borel F, Tresallet C, Hamy A et al (2020) Self-assessment of voice outcomes after total thyroidectomy using the voice handicap index questionnaire: results of a prospective multicenter study. Surgery 167:129–136
Funding
The authors have no commercial interests related to the subject of the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no competing interest exists.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, SY., Park, JO., Bae, JS. et al. How Can We Predict the Recovery from Pitch Lowering After Thyroidectomy?. World J Surg 44, 3395–3404 (2020). https://doi.org/10.1007/s00268-020-05628-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05628-6