Abstract
Background
Assessment of preoperative physiological status is crucial for optimizing clinical outcomes in patients undergoing surgery for esophageal carcinoma (EC). We aimed to evaluate the prognostic impact of pulmonary dysfunctions and their relationships with other physiological factors, especially sarcopenia, in EC patients receiving esophagectomy.
Methods
In total, 411 EC patients who underwent esophagectomy between 2006 and 2016 were retrospectively reviewed. Preoperative pulmonary functions were evaluated based on %vital capacity (%VC) and forced expiratory volume (FEV) 1.0%. The thresholds were set as the lowest quartile (99% for %VC and 68.6% for FEV1.0%) in this cohort.
Results
One hundred and two patients (24.8%) had low %VC (%VC < 99%), which was significantly associated with age, comorbidity, sarcopenia and postoperative complications, while not correlating with pathological variables. The overall survival (OS) of patients in the low %VC group was significantly poorer than that of those in the high %VC group (P < 0.001), especially in those with pStage 0–II diseases (P < 0.001). In contrast, survival was not stratified by FEV1.0% (P = 0.80). Notably, patients with both low %VC and sarcopenia showed very poor 5-year OS (30.3%). Multivariate analysis revealed low %VC to be independently associated with poor OS (P = 0.03). In the cause-specific survival analyses, low %VC was an independent predictor of deaths from non-EC-related causes (P = 0.03).
Conclusions
Preoperative low %VC was independently associated with poor survival outcomes, especially when present in combination with sarcopenia, due to an increased risk of death from non-EC-related causes. Preoperative spirometry testing is useful for predicting long-term outcomes in EC patients undergoing esophagectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal carcinoma (EC) is the sixth most common cause of death from cancer worldwide, despite improvements in survival outcomes due to advances in multimodal treatment strategies [1]. Although histopathological findings are the most powerful prognostic determinants for patients with EC [2, 3], assessment of preoperative physiological status is also crucial for optimizing clinical outcomes in EC patients undergoing esophaegectomy, which is a highly invasive procedure involving considerable morbidity [4]. In fact, prior studies have suggested impaired physiological functions, which are characterized by advanced age [3], low-performance status [1] or comorbidities [5], to be associated with poor short- and long-term outcomes in EC patients treated by esophagectomy.
Preoperative evaluation of pulmonary functions using spirometry testing is widely employed to select surgical candidates and predict the development of postoperative pulmonary complications [6]. In patients undergoing esophagectomy, decreased vital capacity (VC) [7], low forced expiratory volume (FEV) [8] and reduced lung diffusing capacity [9] are reportedly associated with postoperative pulmonary complications. Poor lung functions apparently represent a state of poor physical fitness including comorbidities. Especially, preoperative pulmonary dysfunctions reportedly show correlations with sarcopenia [7], and these two factors are independent predictors for poor survival outcomes in patients undergoing hepatectomy [10].
Some institutions have suggested low pulmonary functions to be associated with high mortality in the general population [11, 12] and in a cohort comprised of patients with gastric carcinoma [13]. Since the long-term survival impact of preoperative pulmonary dysfunctions has not as yet been investigated in patients undergoing esophagectomy, we focused on these factors in the present study.
This study aimed to evaluate the prognostic impact of pulmonary dysfunctions and their relationships with other possible prognostic factors, especially sarcopenia, in EC patients undergoing radical surgery.
Patients and methods
Patients
Between 2006 and 2016, a total of consecutive 468 patients with esophageal malignancies underwent esophagectomy in the University of Tokyo Hospital. Forty-four patients undergoing salvage esophagectomy and 13 lacking data on preoperative pulmonary functions and/or sarcopenia were excluded. The clinical records of the remaining 411 patients were retrospectively reviewed from a prospectively maintained database. At the time of the final follow-up (April 2019), the median follow-up period was 60.8 months for the survivors. This retrospective study was approved by the local ethics committee of the faculty of medicine at the University of Tokyo (ID: 3962).
Evaluation of preoperative pulmonary function
Pulmonary functions were measured using spirometry before surgery under the supervision of a respiratory physician. When patients received neoadjuvant treatment, the tests were performed before neoadjuvant therapy. Vital capacity (VC) of predicted (%VC) and forced expiratory volume in one second (FEV1.0)/forced VC ratio (FEV1.0%) were employed to evaluate ventilatory functions [12]. The cutoff values for %VC and FEV1.0% were set as the lowest quartile (99% for %VC and 68.6% for FEV1.0%) in this cohort.
The definition of sarcopenia
The skeletal muscle index (SMI) was calculated as previously described [14]. In brief, the cross-sectional area of total skeletal muscle (cm2) was assessed at the third lumbar vertebra. Skeletal muscle was identified and quantified based on Hounsfield unit (HU) thresholds (−29 to +150). SMI (cm2/m2) was calculated by the following formula: SMI (cm2/m2) = [total skeletal muscle at the third lumbar vertebra (cm2)]/[height (m)2]. The cutoff values for SMI were set as the sex-specific lowest quartile of SMI (42.7 cm2/m2 for men and 34.3 cm2/m2 for women) in this cohort [15].
Surgical treatment
Our standard procedures consisted of subtotal esophagectomy with mediastinal lymphadenectomy via right thoracotomy (transthoracic esophagectomy; TTE) either by the Ivor Lewis’ or McKeown’s standard procedure. We usually employed 3-field lymphadenectomy for the upper- and middle-thoracic EC and 2-field lymphadenectomy for lower-thoracic and abdominal EC. For patients participating in our previous study on robot-assisted esophagectomy [16], we used a non-transthoracic esophagectomy combining transcervical video-assisted and transhiatal approaches (transmediastinal esophagectomy, TME [16]).
Studied criteria
Patient characteristics included age, sex and charlson comorbidity index (CCI) [17]. Histological staging of tumors was based on the TNM classification (AJCC, 7th edition) [2]. The PNI, an immunonutritional marker, was calculated based on the following equation: [(10 × serum albumin (g/dL)) + (0.005 × total lymphocyte count (/mm3))]. The Clavien–Dindo (C–D) scale was used to grade the severity of all postoperative morbidities [18]. Adjuvant chemotherapy was basically employed for patients with metastatic lymph nodes, unless the patient’s general status made the procedure unlikely to be tolerable [19].
Statistical analysis
Categorical variables were compared using Fisher’s exact test or the Chi-squared test, as appropriate. Continuous variables were compared using Wilcoxon’s rank-sum test. Overall survival (OS) was calculated from the operation date. Cancer-specific survival (CSS) was defined as the period from the date of surgery until death due to EC. Non-EC-related deaths included those from both non-malignant diseases and malignancies other than EC. Survival curves were constructed using the Kaplan–Meier method, and we used the log-rank test for making comparisons. Clinically relevant factors with P < 0.1 in a Cox proportional hazard model with univariable analysis were regarded as potential risk factors and were further analyzed by applying a multivariable Cox model. Multivariable Cox proportional splines model for each spirometric parameter was constructed to investigate the association between %VC or FEV1.0% and the risk of overall death, with adjustment for potential prognostic factors including age, comorbidity, sarcopenia, complications, pStage II/III and non-curative resection. Statistical analyses were carried out using JMP 13.0.0 (SAS Institute, Cary, NC).
Results
Patient characteristics
One hundred and two patients (24.8%) had a low %VC (%VC < 99%, the low %VC group), and the remaining 309 patients (75.2%) had a high %VC (%VC ≥ 99%, the high %VC group). Low %VC was significantly associated with age (P < 0.001), CCI (P = 0.005) and sarcopenia (P < 0.001) (Table 1). The value of PNI, FEV1.0%, tumor location, surgical procedure and pathological findings did not, however, differ significantly between the two groups. One hundred and three patients (25.1%) had low FEV1.0% (FEV1.0% < 68.56%), which was significantly associated with age (P = 0.009) and male gender (P = 0.001), while showing no association with CCI or sarcopenia.
Short-term outcomes according to %VC and FEV1.0%
Overall postoperative complications (C–D classification ≥ Grade II) developed more frequently in the low %VC than in the high %VC group (P = 0.02, Table 2). Patients with low %VC had a higher incidence of pulmonary complications than those with a high %VC, but the difference did not reach statistical significance (P = 0.09). In-hospital deaths were more prevalent in the low %VC group than in the high %VC group (P = 0.002). In contrast, low FEV1.0% was not significantly associated with poor short-term outcomes.
Impact of low %VC and low FEV1.0% on survival
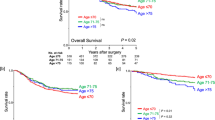
The OS of patients in the high %VC group was significantly better than that of patients in the low %VC group (3-year OS; 75.7% vs. 59.3%, 5-year OS; 67.6% vs. 47.7%, P < 0.001, Fig. 1a). In marked contrast, OS in our cohort could not be stratified according to FEV1.0% (P = 0.80, Fig. 1b). Subdivision into pStage 0–II and III showed a significant survival difference according to %VC to be present only in pStage 0–II patients (3-year OS; 90.0% vs. 68.5%, 5-year OS; 80.8% vs. 53.8%, P < 0.001, Fig. 1c), while no increase was evident in pStage III patients (P = 0.35, Fig. 1d).
The prognostic impacts of low %VC and low FEV1.0%. a The OS of patients in the high %VC group was significantly better than that of patients in the low %VC group (P < 0.001). b FEV 1.0% did not stratify OS (P = 0.80). Survival by %VC was c notably higher in patients with pStage 0–II EC (P < 0.001), while d there was no increase in patients with pStage III EC (P = 0.35).
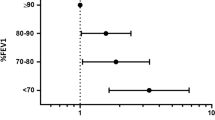
We further employed the Cox proportional splines model for each parameter adjusting for potential prognostic factors identified by the univariable Cox proportional model (age, comorbidity, sarcopenia, complications, pStage II/III and non-curative resection, Table 3) to describe the nonlinear relationships between pulmonary functions and survival time. Adjusted hazard risks of overall death significantly increased as %VC decreased (Fig. 2a), whereas no increase was detected according to a decline in FEV1.0% (Fig. 2b).
Association between %VC or FEV1.0% and the risk of overall death hazard ratios is shown for the association between a %VC or b FEV1.0% and the risk of overall death. The analyses were adjusted for age, comorbidity, sarcopenia, complications, pStage II/III and non-curative resection,. The dotted lines show 95% confidence intervals.
Impact of low %VC with sarcopenia on survival
Patients with sarcopenia had significantly lower %VC [100.0% (69.0–136.0)] than those without sarcopenia [108.0% (80.0–155.0)] (P < 0.001). In contrast, FEV1.0% showed no significant association with sarcopenia (sarcopenic patients; 73.9% (57.8–96.4), non-sarcopenic patients; 73.6% (45.5–96.6), P = 0.74).
Subsequently, we evaluated the prognostic impact of low %VC in combination with sarcopenia. Patients with both low %VC and sarcopenia showed markedly poor OS (5-year OS; 30.3%, Fig. 3), which was significantly poorer than that of patients with either low %VC or sarcopenia (both P < 0.05). Survival outcomes of patients with either low %VC or sarcopenia were essentially equivalent (5-year OS; 55.5%, 53.0%, respectively), while being significantly worse than that of patients with neither low %VC nor sarcopenia (5-year OS; 71.5%) (Fig. 3).
Survival according to low %VC and sarcopenia patients with both low %VC and sarcopenia showed strikingly poor OS (5-year OS; 30.3%). Survival outcomes of patients with either low %VC or sarcopenia were essentially equivalent (5-year OS; 55.5%, 53.0%, respectively), while being significantly worse than that of patients with neither low %VC nor sarcopenia (5-year OS; 71.5%). Survival was analyzed by Kaplan–Meier method using the log-rank test (*, P < 0.05; **, P < 0.01; ns, not significant).
Causes of death
Patients with low %VC had poorer cancer-specific survival than those with high %VC, although the difference was not statistically significant (P = 0.06, Fig. 4a). Of note, low %VC was associated with significantly increased non-EC-related deaths as compared to high %VC (P < 0.001, Fig. 4b). Univariable analysis and subsequent application of the multivariable Cox proportional hazards model revealed low PNI (<45), low %VC, non-TME procedure, pStage III disease and non-curative resection to be independently associated with poor OS outcomes (Table 3). Notably, multivariate Cox hazards model analysis focusing on non-EC-related deaths showed low %VC to be an independent predictor of non-EC-related deaths (HR 1.80, 95% CI 1.01–3.22, P = 0.04), as were age (HR 1.04 per 1-unit increase, 95% CI 1.00–1.08, P = 0.04), low PNI (HR 2.51, 95% CI 1.40–4.49, P = 0.002) and high CCI (≥2) (HR 1.97, 95% CI 1.10–3.52, P = 0.02) (Table 3). There were no distinct patterns among non-cancer causes in either group.
Cancer-specific survival and non-EC-related deaths according to low %VC. a Patients with low %VC had poorer cancer-specific survival than those with high %VC, although the difference was not statistically significant (P = 0.06). b Low %VC was associated with significantly increased non-EC-related deaths as compared to high %VC (P < 0.001).
Discussion
Lung functions gradually deteriorate after 20–25 years of age due to diminishing lung elasticity and reduced intercostal muscle mass [20]. The presence of impaired lung functions, especially reduced VC, is reportedly associated with mortality in the large general population [11, 21]. Our study highlighted a difference in survival impact between %VC and FEV1.0%; preoperative low %VC significantly worsened survival in patients undergoing esophagectomy, while low FEV1.0% did not affect long-term outcomes.
As previously demonstrated [10, 12], our investigation showed reduced %VC to be closely related to impaired physiological conditions such as high comorbidity, advanced age and sarcopenia, all of which negatively affect survival outcomes after esophagectomy [3, 5, 22]. Of note, multivariable analyses including all of the possible prognostic factors revealed low %VC to be independently associated with poor survival outcomes, which underscored the powerful prognostic significance of low %VC itself. Importantly, the negative survival impact of low %VC was due mainly to increased deaths from non-EC-related causes. Only a few studies have focused on non-cancer-related deaths in EC patients [23], although this is a highly relevant issue from a public health perspective [24]. Given that non-cancer deaths generally influence survival in patients with early-stage cancer [24], our observation of a significant survival difference according to %VC only in pStage 0–II patients is consistent with earlier findings.
In line with prior results [7, 10, 20], low %VC significantly correlated with sarcopenia characterized by decreased skeletal muscle mass in our cohort. It is noteworthy that patients with both low %VC and sarcopenia exhibited quite poor survival outcomes, and the survival difference according to %VC was highly apparent in sarcopenic patients. These results allow us to hypothesize that the concomitant presence of low %VC and sarcopenia strongly reflects the vicious cycle of ever-worsening frailty, as suggested by a recent study showing the combination of high comorbidity and sarcopenia to clearly result in quite poor survival outcomes for patients with gastric carcinoma [15].
In contrast, the presence of low FEV1.0% did not affect short- and long-term outcomes, a finding consistent with those of some past studies [10]. The prognostic significance of low FEV1.0% alone remains to be determined in large general populations [11, 21]. Given that FEV1.0% itself showed no correlation with either low muscle mass or muscle quality [10, 20], low %VC, but not low FEV1.0%, might affect general status and secondary comorbidities.
In this study, we employed the lowest quartiles of %VC and FEV1.0% as the cutoff values, rather than the thresholds commonly used in clinical settings (%VC < 80% or FEV1.0% < 70%) [12]. In our cohort, the proportion of patients with %VC < 80% was very small (n = 17, 4.1%), which was consistent with prior findings [25] because thoracic surgery is not feasible for patients with extremely poor pulmonary functions. Furthermore, we employed the Cox proportional splines model for each parameter and revealed adjusted hazard risks of overall death to significantly increase as %VC decreased, while showing no increase according to a decline in FEV1.0%. These findings highlight the robust survival impact of decreased %VC in various statistical approaches, although how to make use of our findings in clinical practice remains to be fully addressed in this study.
Our study has limitations. First, we employed only general spirometric parameters, such as VC and FEV1.0, for preoperative pulmonary evaluations. Further, the survival impact of postoperative changes in pulmonary functions merits scrutiny given that impaired physiological status after esophagectomy, such as decreased SMI, reportedly affects the long-term outcome [26]. Second, we evaluated only the cross-sectional area of skeletal muscle mass on computed tomography, rather than precise muscle strength or physical performances, to determine whether or not sarcopenia was present. In addition, the optimal cutoff values for diagnosing sarcopenia remain controversial. We employed the sex-specific lowest quartile of SMI as the cutoff value, which was lower than the Prado et al. proposal [14], because our cohort was comprised mainly of esophageal squamous cell carcinoma (ESCC) patients, in whom low body muscle mass is much more prevalent than in those with other types of cancer [22]. Considering that adenocarcinoma is a common histological type in western countries, further studies are warranted to verify whether our conclusions are applicable to western populations. Finally, the number of patients given neoadjuvant therapy was limited in our institution during this study period. Our findings thus need to be validated in patients undergoing neoadjuvant chemotherapy.
In conclusion, preoperative low %VC is independently associated with poor survival outcomes in EC patients, especially when present in combination with sarcopenia. In addition to oncological variables, preoperative patient physiological factors should be underscored to optimize the survival outcomes of EC patients. Less invasive approaches such as minimally invasive esophagectomy reportedly contribute to maintaining postoperative pulmonary functions [27] and improving short-term outcomes [28], thus might provide survival benefits for such high-risk patients. Further, definitive chemoradiotherapy might be beneficial for vulnerable patients with ESCC [29]. It might also be very interesting to determine whether preoperative rehabilitation and intervention would improve not only pulmonary functions [30] but also long-term survival outcomes after esophagectomy.
Abbreviations
- EC:
-
Esophageal carcinoma
- VC:
-
Vital capacity
- FEV:
-
Forced expiratory volume
- SMI:
-
Skeletal muscle index
- HU:
-
Hounsfield unit
- TTE:
-
Transthoracic esophagectomy
- TME:
-
Transmediastinal esophagectomy
- VATS:
-
Video-assisted transthoracic surgery
- CCI:
-
Charlson comorbidity index
- PNI:
-
Prognostic nutritional index
- C–D:
-
Clavien–Dindo
- OS:
-
Overall survival
- CSS:
-
Cancer-specific survival
- COPD:
-
Chronic obstructive pulmonary disease
- ESCC:
-
Esophageal squamous cell carcinoma
References
Lagergren J, Smyth E, Cunningham D et al (2017) Oesophageal cancer. Lancet 390:2383–2396
Rice TW, Blackstone EH, Rusch VW (2010) 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol 17:1721–1724
Chen SB, Weng HR, Wang G et al (2013) Prognostic factors and outcome for patients with esophageal squamous cell carcinoma underwent surgical resection alone: evaluation of the seventh edition of the American Joint Committee on Cancer staging system for esophageal squamous cell carcinoma. J Thorac Oncol 8:495–501
Takeuchi H, Miyata H, Gotoh M et al (2014) A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web-based database. Ann Surg 260:259–266
Backemar L, Lagergren P, Johar A et al (2015) Impact of co-morbidity on mortality after oesophageal cancer surgery. Br J Surg 102:1097–1105
Smetana GW (1999) Preoperative pulmonary evaluation. N Engl J Med 340:937–944
Ida S, Watanabe M, Yoshida N et al (2015) Sarcopenia is a predictor of postoperative respiratory complications in patients with esophageal cancer. Ann Surg Oncol 22:4432–4437
Ferguson MK, Celauro AD, Prachand V (2011) Prediction of major pulmonary complications after esophagectomy. Ann Thorac Surg 91:1494–1500 (discussion 1500–1491)
Goense L, Meziani J, Bulbul M et al (2019) Pulmonary diffusion capacity predicts major complications after esophagectomy for patients with esophageal cancer. Dis Esophagus. https://doi.org/10.1093/dote/doy082
Shirai H, Kaido T, Hamaguchi Y et al (2018) Preoperative low muscle mass and low muscle quality negatively impact on pulmonary function in patients undergoing hepatectomy for hepatocellular carcinoma. Liver Cancer 7:76–89
Burney PG, Hooper R (2011) Forced vital capacity, airway obstruction and survival in a general population sample from the USA. Thorax 66:49–54
Godfrey MS, Jankowich MD (2016) The vital capacity is vital: epidemiology and clinical significance of the restrictive spirometry pattern. Chest 149:238–251
Feng F, Tian Y, Zang Y et al (2017) Low forced vital capacity predicts poor prognosis in gastric cancer patients. Oncotarget 8:28897–28905
Prado CM, Lieffers JR, McCargar LJ et al (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9:629–635
Kuwada K, Kuroda S, Kikuchi S et al (2018) Sarcopenia and comorbidity in gastric cancer surgery as a useful combined factor to predict eventual death from other causes. Ann Surg Oncol 25:1160–1166
Mori K, Yamagata Y, Aikou S et al (2016) Short-term outcomes of robotic radical esophagectomy for esophageal cancer by a nontransthoracic approach compared with conventional transthoracic surgery. Dis Esophagus 29:429–434
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Kuwano H, Nishimura Y, Oyama T et al (2015) Guidelines for diagnosis and treatment of carcinoma of the esophagus edited by the Japan esophageal society. Esophagus 12:1–30
Jeon YK, Shin MJ, Kim MH et al (2015) Low pulmonary function is related with a high risk of sarcopenia in community-dwelling older adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008–2011. Osteoporos Int 26:2423–2429
Guerra S, Sherrill DL, Venker C et al (2010) Morbidity and mortality associated with the restrictive spirometric pattern: a longitudinal study. Thorax 65:499–504
Nakashima Y, Saeki H, Nakanishi R et al (2018) Assessment of sarcopenia as a predictor of poor outcomes after esophagectomy in elderly patients with esophageal cancer. Ann Surg 267:1100–1104
Ichikawa H, Kosugi SI, Kanda T et al (2016) Surgical and long-term outcomes following oesophagectomy in oesophageal cancer patients with comorbidity. Int J Surg 36:212–218
Cho H, Mariotto AB, Mann BS et al (2013) Assessing non-cancer-related health status of US cancer patients: other-cause survival and comorbidity prevalence. Am J Epidemiol 178:339–349
Ohi M, Toiyama Y, Omura Y et al (2019) Risk factors and measures of pulmonary complications after thoracoscopic esophagectomy for esophageal cancer. Surg Today 49:176–186
Nakashima Y, Saeki H, Hu Q et al (2020) Skeletal muscle loss after esophagectomy is an independent risk factor for patients with esophageal cancer. Ann Surg Oncol 27:492–498
Kosumi K, Yoshida N, Okadome K et al (2018) Minimally invasive esophagectomy may contribute to long-term respiratory function after esophagectomy for esophageal cancer. Dis Esophagus. https://doi.org/10.1093/dote/dox153
Yoshida N, Yamamoto H, Baba H et al (2019) Can minimally invasive esophagectomy replace open esophagectomy for esophageal cancer? Latest analysis of 24,233 Esophagectomies from the Japanese National Clinical Database. Ann Surg. https://doi.org/10.1097/SLA.0000000000003222
Faiz Z, van Putten M, Verhoeven RHA et al (2019) Impact of age and comorbidity on choice and outcome of two different treatment options for patients with potentially curable esophageal cancer. Ann Surg Oncol 26:986–995
Valkenet K, Trappenburg JCA, Ruurda JP et al (2018) Multicentre randomized clinical trial of inspiratory muscle training versus usual care before surgery for oesophageal cancer. Br J Surg 105:502–511
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sugawara, K., Mori, K., Okumura, Y. et al. Preoperative Low Vital Capacity Influences Survival After Esophagectomy for Patients with Esophageal Carcinoma. World J Surg 44, 2305–2313 (2020). https://doi.org/10.1007/s00268-020-05450-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05450-0