Abstract
Background and Objective
Chlorhexidine (CH) and povidone-iodine (PI) are the most commonly used preoperative skin antiseptics at present. However, the prevention of the surgical site infection (SSI) and the incidence of skin adverse events do not reach a consistent statement and conclusion. This meta-analysis aimed to evaluate the efficacy of chlorhexidine and povidone-iodine in the prevention of postoperative surgical site infection and the incidence of corresponding skin adverse events.
Method
Substantial studies related to “skin antiseptic” and “surgical site infection” were consulted on PUBMED, Web of Science, EMBASE, and CNKI. The primary outcome was the incidence of postoperative SSI. The secondary outcome was associated with skin adverse events. All data were analyzed with Revman 5.3 software.
Results
A total of 30 studies were included, including 29,006 participants. This study revealed that chlorhexidine was superior to povidone-iodine in the prevention of postoperative SSI (risk ratio [RR], 0.65; 95% confidence interval [CI], 0.55–0.77; p < 0.00001, I2 = 57%). Further subgroup analysis showed that chlorhexidine was superior to povidone-iodine in the prevention of postoperative SSI in clean surgery (risk ratio [RR], 0.81; 95% confidence interval [CI], 0.67–0.98; p = 0.03), I2 = 28%) and clean-contaminated surgery (risk ratio [RR], 0.58; 95% confidence interval [CI], 0.47–0.73; p < 0.00001, I2 = 43%). However, there was no statistically significant difference in the incidence of skin adverse events between CH and PI groups.
Conclusion
Chlorhexidine was superior to povidone-iodine in preventing postoperative SSI, especially for the clean-contaminated surgery. However, there was no statistically significant difference in the incidence of skin adverse events between CH and PI groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical site infection has attracted more and more attention. It is not only associated with delayed recovery and prolongation of hospitalization, but also adversely affects the patient’s mental health and endangers society [1]. The definition of postoperative surgical site infection is not clear, but SSI occurs within 30 days postoperation, including superficial and deep wound infections, which has reached a consensus [2, 3]. There are several ways to prevent postoperative surgical site infections, such as strict hand antiseptic, preoperative antibiotic, strict aseptic operation and so on. The World Health Organization (WHO) [4], Centers for Disease Control (CDC) [5], and the National Institute for Health and Care Excellence (NICE) [6] have also updated the guidelines for the prevention of postoperative surgical site infections, suggesting that preoperative skin antiseptic is one of the most critical factors for postoperative surgical site infection.
Povidone-iodine is the most commonly used preoperative skin antiseptic in clinical settings. However, in recent years, there are many studies which show that chlorhexidine provides better results than povidone-iodine for preoperative skin antiseptic. The choice of preoperative skin disinfectants is a puzzling problem for clinicians.
In order to obtain a relatively more objective, credible, and powerful evidence, the purpose of this meta-analysis was to evaluate the effects of chlorhexidine and povidone-iodine on the prevention of postoperative surgical site infection.
Materials
This research was in accordance with PRISMA and AMSTAR guidelines.
Systematic literature search
PUBMED, Web of Science, EMBSAE, and CNKI have been searched, respectively, from inception to September 2019. Language restriction is English. Retrieval strategy is a combination of keywords, free words, and subject words.
Search strategy
Use the following search strategies:(((“iodine” [MeSH Terms] OR “iodine” [All Fields] OR “iodides” [MeSH Terms] OR “iodides” [All Fields]) OR (“chlorhexidine” [MeSH Terms] OR “chlorhexidine” [All Fields])) OR ((“skin” [MeSH Terms] OR “skin” [All Fields]) AND (“antisepsis” [MeSH Terms] OR “antisepsis” [All Fields]))) AND (“surgical wound infection” [MeSH Terms] OR (“surgical” [All Fields] AND “wound” [All Fields] AND “infection” [All Fields]) OR “surgical wound infection” [All Fields] OR (“surgical” [All Fields] AND “site” [All Fields] AND “infection” [All Fields]) OR “surgical site infection” [All Fields]).
We have also manually searched the references of included studies and related reviews for additional eligible trials.
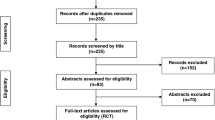
The process and results of literature retrieved are shown in Fig. 1.
Include criteria
-
1.
All patients involved in the surgery had no open wounds;
-
2.
Povidone-iodine and chlorhexidine as preoperative skin antiseptics, with or without alcohol;
-
3.
Reported the incidence of skin adverse events or postoperative surgical site infection;
-
4.
Included literature types: all RCTs (prospective or retrospective), observational studies, cohort studies, etc.;
Exclude criteria
-
1.
Non-surgical or patients who were intolerance to the surgeries, or patients who showered, scrubbed or irrigated the wounds before surgery;
-
2.
Those who were allergic to chlorhexidine or povidone-iodine;
-
3.
Animal experiments or in vitro experiences;
-
4.
The type of articles were either reviews or meta-analysis;
Selection of studies and extraction
The selection of studies was conducted by two independent authors (Chen jun wu, Guo bin). If the conclusions were inconsistent, the two authors will make further discussion to reach a consistent agreement. We extracted data on the following information: first author, year of publication, country, type of study, sample size of experimental and control groups, age, type of skin disinfectant, and side effects. (Details are shown in Table 1.)
The primary outcome was the incidence of postoperative surgical site infection, and the secondary was skin adverse events;
Assessment
The quality of all RCT studies was assessed by the Cochrane evaluation criteria [7], which includes the following domains: random sequence generation, allocation concealment, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias. All retrospective, observational and cohort studies were assessed based on the criteria of Newcastle–Ottawa Quality Assessment Scale (NOS).
Statistical analysis
Statistical analysis of this study was performed using Revman 5.3 (Cochrane Collaboration, Oxford, UK). The risk ratio (RR) was applied as the effect indicators for the dichotomous data of the two groups; In addition, the point estimated value and 95% CI were calculated for each effect indicators. The heterogeneity between the studies was analyzed according to the Chi-square test, and the size of heterogeneity was quantified by combining with I2.
Mild heterogeneity: I2 < 25%; moderate heterogeneity: 25% < I2 < 50%; high heterogeneity: I2 > 50% [8]. Meta-analysis was performed using a random effects model; if there was statistical heterogeneity between studies, the source of heterogeneity would be further investigated. Significant heterogeneity was handled using the following methods: subgroup analysis, sensitivity analysis, and only descriptive analysis.
Results
Literature search results
A total of 30 studies including 19 RCTs, 4 retrospective studies, 7 observational studies and cohort studies in this meta-analysis were conducted. A total of 29,006 patients including adult and pediatric were involved, of which 15,263 cases were in chlorhexidine group and 13,437 in povidone-iodine group. (The basic characteristics and risk assessment of bias in the included studies are shown in Fig. 2.)
Clean or clean-contaminated surgery definition
Cleaning surgery is a kind of sterile incision operation, such as a craniocerebral, visual organ, limb trunk, and thoracoabdominal incision, etc. There is no open cavity organ. A clean-contaminated surgery, in which the cavity organ must be cut or disconnected from the body surface during the surgery, including operations of the digestive tract, respiratory tract, urethra, vagina, scrotum, perineum, etc., in this cases, complete disinfection skin incision proves to be quite difficult [9].
Twenty-two of included studies identified the types of surgery: 10 [10,11,12,13,14,15,16,17,18,19] reported clean surgeries, and 12 studies [20,21,22,23,24,25,26,27,28,29,30,31] underwent clean-contaminated surgeries; five studies [32,33,34,35,36] included both clean surgeries and clean-contaminated surgeries. And the last three studies did not classify the type of surgeries [37,38,39].
Methodological quality assessment
We identified the design type of included study according to methodology evaluation analysis (RCT vs. non-RCT), and non-RCT included retrospective studies, observational studies, and cohort studies. (See Fig. 3 and Table 2 for details.)
Primary outcome
Surgical site infection (SSI) rate
All studies reported postoperative surgical site infection. Meta-analysis showed that the wound infection rate in chlorhexidine group was lower than that in povidone-iodine group (risk ratio [RR], 0.65; 95% confidence interval [CI], 0.55–0.77; p < 0.00001, I2 = 57%). (Figs. 4, 5).
Subgroup analysis based on the type of study design revealed that: RCT group (risk ratio [RR], 0.57; 95% confidence interval [CI], 0.47–0.70; p < 0.00001, I2 = 42%); non-RCT group (risk ratio [RR], 0.82; 95% confidence interval [CI], 0.66–1.02; p = 0.08, I2 = 49%). It indicated that the type of study design had an impact on the incidence of postoperative surgical site infection. (Figs. 6, 7).
Further subgroup analysis indicated that chlorhexidine were superior to povidone-iodine in the prevention of postoperative surgical site infection in both clean surgery subgroup (risk ratio [RR], 0.81; 95% confidence interval [CI], 0.67–0.98; p = 0.03, I2 = 28%) and clean-contaminated surgery subgroup (risk ratio [RR], 0.58; 95% confidence interval [CI], 0.47–0.73; p < 0.00001, I2 = 43%),especially for the clean-contaminated surgery subgroup. (Figs. 8, 9).
The results of funnel plot on the infection rate showed that the scatter points were substantially symmetrical, suggesting no significant publication bias.
Secondary outcomes
Nine of include studies [17, 19, 22, 25, 26, 30, 33, 35, 37] reported the incidence of skin adverse events. Four studies [12, 15, 29, 36] found no significant skin adverse events, and the remaining 17 studies reported no relevant skin adverse events.
Meta-analysis indicated no statistically significant difference in the incidence of skin adverse events between chlorhexidine and povidone-iodine group (risk ratio [RR], 0.89; 95% confidence interval [CI], 0.50–1.59; p = 0.69, I2 = 0%). (Figs. 10, 11).
Discussion
The occurrence of postoperative incision infection results from the interaction of many factors and is highly associated with the colonization of intraoperative bacteria. How to remove bacteria from incision to the maximum extent is a technical problem worthy of surgeons’ attention. It is an effective method to disinfect the skin before operation. The choice of disinfectant remains controversial in clinical practice.
Povidone-iodine plays a role in antibiosis, on the one hand, it can be attributed to covalently bonded hydrogen-containing groups, i.e., -OH, -NH, -SH, -CH; on the other hand, as a iodine carrier which can interact with oxygen-containing functional groups. It inhibits microbial protein synthesis by oxidizing sulfhydryl groups, making it quickly and extensively to tackle bacteria, viruses, and fungi [40]. It is the most widely used and lasting classic skin antiseptic in clinical practice.
Chlorhexidine is a kind of cationic biguanide; it combines with the anions on the surface of bacterial cell walls, which alters the permeability of cell wall, inducing apoptosis due to the leakage of cytoplasmic components [41]. It has the same bactericidal activity on both resistant and non-resistant bacteria and still effective even when exposed to body fluids. With alcohol as the medium, chlorhexidine dries faster when disinfecting and wait for surgery shorter. Therefore, some scholars suggest that chlorhexidine is better on disinfection effect and more suitable for clinical application.
Therefore, we conducted this meta-analysis to comprehensively evaluate the effectiveness of chlorhexidine or povidone-iodine for preventing postoperative surgical site infection.
The results of this study indicated that chlorhexidine as a main component of antiseptic was superior to povidone-iodine in reducing the incidence of overall postoperative wound infection. Further subgroup analysis showed that chlorhexidine was more conducive to prevent postoperative surgical site infections in clean-contaminated surgery.
Wu yan [39], Patrick [15], Guo [16], and Culligan et al. [20] investigated the effects chlorhexidine and povidone-iodine on local bacteria, and found that the inhibition of chlorhexidine on bacteria was significantly stronger than that of povidone-iodine; in addition, the disinfection effect of chlorhexidine on Staphylococcus was faster and more favorable. Given the diversity of bacterial infections and the complexity of the clinical research’s setting, none of the four researchers focused on specific bacteria. However, studies by Kulkarni and Awode [42] suggested that the effect of povidone-iodine was more persistent than chlorhexidine.
Comparison of side effects
The main skin adverse events of chlorhexidine and povidone-iodine are allergy and pruritus. However, the incidence of both has not been clearly and thoroughly investigated. Nine studies of included studies reported skin side effects, such as pruritus and mild to moderate allergy, had no serious life-threatening complications and can be alleviated by antiallergic or symptomatic treatment. Four studies found no corresponding skin adverse reactions, electrotome fire or other adverse events. Meta-analysis showed that there was no statistically significant difference in the incidence of skin adverse events between the two disinfectants.
However, adverse reactions related to chlorhexidine have also been reported.
As reported [43], chlorhexidine may penetrate into the patient’s eyes during the operation of cervical spine due to negligence in the process of disinfection, resulting in corneal damage and sometimes even corneal transplantation. In view of the damage of chlorhexidine to cornea, it is highly recommended to take eye protection measures in the process of skull and neck disinfection, and low concentration disinfectants during ophthalmic surgery; for instance, in a study of cataract surgery, the concentration of compound chlorhexidine used by researchers was only 0.02% [44].
One study [45] reported that when the chlorhexidine was not completely dry, there was a risk of electrotome fire; although the incidence was very low. Therefore, it is recommended to wait at least 3 min for the disinfectant to dry completely before operation. No electrotome fire caused by chlorhexidine was found in the literature.
Studies by Edmiston et al. [46] suggested that chlorhexidine was safe for use on intact skin. However, compound chlorhexidine has an irritation effect on the nerves on a certain degree. It is suggested that spinal cord surgery and open surgery with nerve exposure should avoid using compound chlorhexidine [47].
A study by Zhou and Carlson [48] showed that the cost of chlorhexidine was higher than that of povidone-iodine.
In the traditional sense, because chlorhexidine contains alcohol, it can lead to dryness and irritation to the mucous such as the urethra. Therefore, it shall be used with caution in the corresponding surgery. Instead, povidone-iodine in a water solvent was used as a replacement in urinary tract operation. However, in this study, Yeung [22] implied that chlorhexidine was more effective than povidone-iodine in disinfection of male urinary and prostate surgery. In addition, there was no statistically significant difference in skin and other related side effects. It is recommended that chlorhexidine should be used for disinfection in related urinary surgery. Culligan et al. [20] showed that chlorhexidine was superior to povidone-iodine, and no skin complications were found in the literature.
Limitation
There are certain deficiencies in this study: 1. Not all included studies were RCTs; on the contrary, it included retrospective studies, observational studies, and cohort studies. Although the subgroups analysis had been conducted, the results were not significantly biased. However, there were still certain deviations in the research design. 2. The surgery types varied between studies. Although the surgery type was divided into clean surgery and clean-contaminated surgery, and the corresponding subgroup analysis has been conducted, potential bias could not be ruled out. 3. The main components of the disinfectant used in the experimental and observation groups of this study were compound chlorhexidine and povidone-iodine. However, the concentrations of compound chlorhexidine, povidone-iodine, and solute (such as alcohol, polypropanol, and normal saline) were different, which might weaken the reliability of the results.
Highlight
Some researchers [49, 50] had conducted a meta-analysis of the skin antiseptic on chlorhexidine and povidone-iodine. However, this meta-analysis further integrated the latest research, with the longest duration and the largest number of studies, totaling 29,006 research objects. In addition, the skin adverse events of the chlorhexidine and povidone-iodine were analyzed systematically. Therefore, the conclusions of this meta-analysis have a strong guiding value for the development of clinical practices.
Conclusion
In summary, this study showed that chlorhexidine was superior to povidone-iodine in preventing postoperative surgical site infection, and in particular, for clean-contaminated surgery, the prevention effect was superior, which was worth clinical promotion to a certain degree. There was no statistically significant difference in the incidence of skin side effects between the two disinfectants. Given the limitation of included studies in quality and quantity, more high-quality randomized controlled trials are needed to further confirm the conclusion of this research.
References
Abbas M, Pittet D (2016) Surgical site infection prevention: a global priority. J Hosp Infect 93(4):319–322
Mangram AJ et al (1999) Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 20(4):250–278 (quiz 279-80)
Heal CF et al (2016) Topical antibiotics for preventing surgical site infection in wounds healing by primary intention. Cochrane Database Syst Rev 11:Cd011426
Allegranzi B et al (2016) New WHO recommendations on preoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 16(12):e276–e287
Berrios-Torres SI et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 152(8):784–791
Team NGU (2019) National Institute for Health and Care Excellence: clinical guidelines, in surgical site infections: prevention and treatment. 2019, National Institute for Health and Care Excellence (UK) Copyright (c) NICE 2019.: London
Higgins JP et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Higgins JP et al (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560
Hong X, Cheng Y, Dai Z (1997) Kunming General Hospital of Chengdu Military Region, correctly mastering the classification of surgical incision and the principle of healing grade identification. Chin Hosp Manag (01):41 1001-5329 23-1041 CNKI
Perek B et al (2013) Comparative analysis of the antiseptic effectiveness of two commercially available skin disinfectants in cardiac surgery—a preliminary report. Kardiochirurgia I Torakochirurgia Polska 10(2):177–181
Hannan MM et al (2015) The combined impact of surgical team education and chlorhexidine 2% alcohol on the reduction of surgical site infection following cardiac surgery. Surg Infect 16(6):799–805
Anirudh S et al (2015) Comparison of the efficacy of chlorhexidine gluconate versus povidone iodine as preoperative skin preparation for the prevention of surgical site infections in clean-contaminated upper abdominal surgeries. Surg Today 45(11):1378–1384
Davies BM, Patel HC (2016) Does chlorhexidine and povidone-iodine preoperative antisepsis reduce surgical site infection in cranial neurosurgery? Ann R Coll Surg Engl 98(6):405–408
Madej T et al (2016) Reducing mediastinitis after sternotomy with combined chlorhexidine-isopropyl alcohol skin disinfection: analysis of 3000 patients. Surg Infect 17(5):552–556
Patrick S et al (2017) Antisepsis of the skin before spinal surgery with povidone iodine-alcohol followed by chlorhexidine gluconate-alcohol versus povidone iodine-alcohol applied twice for the prevention of contamination of the wound by bacteria. Bone Joint J 99B(10):1354–1365
Sumei Guo, Lifeng Li (2017) Comparison of the effects of chlorhexidine gluconate and povidone iodine on preoperative skin preparation. Chin J Disinfect 34(07):684–686
Ghobrial GM et al (2018) Preoperative skin antisepsis with chlorhexidine gluconate versus povidone-iodine: a prospective analysis of 6959 consecutive spinal surgery patients. J Neurosurg Spine 28(2):209–214
Raja SG et al (2018) Impact of choice of skin preparation solution in cardiac surgery on rate of surgical site infection: a propensity score matched analysis. J Infect Prev 19(1):16–21
Peel TN et al (2019) Chlorhexidine-alcohol versus iodine-alcohol for surgical site skin preparation in an elective arthroplasty (ACAISA) study: a cluster randomized controlled trial. Clin Microbiol Infect
Culligan PJ et al (2005) A randomized trial that compared povidone iodine and chlorhexidine as antiseptics for vaginal hysterectomy. Am J Obstet Gynecol 192(2):422–425
Jonia A-A et al (2013) Can we reduce the surgical site infection rate in cesarean sections using a chlorhexidine-based antisepsis protocol? The journal of maternal-fetal & neonatal medicine: the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians 26(17)
Yeung LL et al (2013) A comparison of chlorhexidine-alcohol versus povidone-iodine for eliminating skin flora before genitourinary prosthetic surgery: a randomized controlled trial. J Urol 189(1):136–140
Ngai IM et al (2015) Skin preparation for prevention of surgical site infection after cesarean delivery: a randomized controlled trial. Obstet Gynecol 126(6):1251–1257
Kunkle CM et al (2015) Chlorhexidine gluconate versus povidone iodine at cesarean delivery: a randomized controlled trial. J Matern Fetal Neonatal Med 28(5):573–577
Salama FA et al (2016) Efficacy and safety of chlorhexidine versus povidone-iodine skin antisepsis in reducing surgical site infection in cesarean sections: a randomized, controlled clinical trial. Evid Based Womenʼs Health J 6(1)
Tuuli MG et al (2016) A randomized trial comparing skin antiseptic agents at cesarean delivery. N Engl J Med 374(7):647–655
Tuuli MG et al (2016) Chlorhexidine-alcohol compared with iodine-alcohol for preventing surgical-site infection at cesarean: a randomized controlled trial. Am J Obstet Gynecol 214(1):S3–S4
Danasekaran G, Rasu S, Palani M (2017) A study of comparative evaluation of preoperative skin preparation with chlorhexidine-alcohol versus povidone-iodine in prevention of surgical site infections. J Evid Based Med Healthcare 4(41)
Springel EH et al (2017) A randomized open-label controlled trial of chlorhexidine-alcohol vs povidone-iodine for cesarean antisepsis: the CAPICA trial. Am J Obstet Gynecol 217(4):463.e1–463.e8
Elshamy E et al (2018) Chlorhexidine-alcohol versus povidone-iodine for skin preparation before elective cesarean section: a prospective observational study. J Matern Fetal Neonatal Med 8:1–5
Xiaoxia Shou et al (2018) Clinical analysis of chlorhexidine and povidone-iodine in preventing postoperative wound infection. Chin J Nosocomiol 28(17):2702–2704
Swenson BR et al (2009) Effects of preoperative skin preparation on postoperative wound infection rates: a prospective study of 3 skin preparation protocols. Infect Control Hosp Epidemiol 30(10):964–971
Darouiche RO et al (2010) Chlorhexidine-alcohol versus povidone-iodine for surgical-site antisepsis. N Engl J Med 362(1):18–26
Luzia RA, Biondo SMdLP (2014) Incidence of surgical site infection with pre-operative skin preparation using 10% polyvidone-iodine and 0.5% chlorhexidine-alcohol. Revista do Colegio Brasileiro de Cirurgioes 40(6)
Bibi S et al (2015) Is chlorhexidine-gluconate superior than Povidone-Iodine in preventing surgical site infections? A multicenter study. J Pak Med Assoc 65(11):1197–1201
Li Lai et al (2017) A randomized controlled clinical trial comparing the efficacy of chlorhexidine and povidone-iodine in preventing surgical wound infection. J Sichuan Univ (Med Ed) 48(03):500–502
Paocharoen V, Mingmalairak C, Apisarnthanarak A (2009) Comparison of surgical wound infection after preoperative skin preparation with 4% chlorhexidine [correction of chlohexidine] and povidone iodine: a prospective randomized trial. J Med Assoc Thai 92(7):898–902
Hakkarainen TW et al (2014) Comparative effectiveness of skin antiseptic agents in reducing surgical site infections: a report from the Washington State Surgical Care and Outcomes Assessment Program. J Am Coll Surg 218(3):336–344
Yan Wu et al (2017) Effects of chlorhexidine combined with iodine-containing surgical membranes on orthopedic incisional wound infection in children. Chin J Nosocomiol 27(18):4216–4219
Fleischer W, Reimer K (1997) Povidone-iodine in antisepsis–state of the art. Dermatology 195(Suppl 2):3–9
Milstone AM, Passaretti CL, Perl TM (2008) Chlorhexidine: expanding the armamentarium for infection control and prevention. Clin Infect Dis 46(2):274–281
Kulkarni AP, Awode RM (2013) A prospective randomised trial to compare the efficacy of povidone-iodine 10% and chlorhexidine 2% for skin disinfection. Indian J Anaesth 57(3):270–275
Tabor E, Bostwick DC, Evans CC (1989) Corneal damage due to eye contact with chlorhexidine gluconate. JAMA 261(4):557–558
Inagaki K et al (2013) Bacterial culture after three sterilization methods for cataract surgery. Jpn J Ophthalmol 57(1):74–79
Briscoe CE, Hill DW, Payne JP (1976) Inflammable antiseptics and theatre fires. Br J Surg 63(12):981–983
Edmiston CE et al (2010) Evidence for using chlorhexidine gluconate preoperative cleansing to reduce the risk of surgical site infection. AORN J 92(5):509–518
Sviggum HP et al (2012) Neurologic complications after chlorhexidine antisepsis for spinal anesthesia. Reg Anesth Pain Med 37(2):139–144
Zhou S, Carlson A PIN5 a budget impact analysis of three presurgical skin antisepsis protocols
Jiang X, Qin Y, Cui D (2013) A meta-analysis of the preventive effects of two skin disinfectants on surgical site infection. Chin J Nosocomiol 23(19):4749–4750+4753
Privitera GP et al (2016) Skin antisepsis with chlorhexidine versus iodine for the prevention of surgical site infection: a systematic review and meta-analysis. AJIC Am J Infect Control
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that there is no conflict of interest with any individual/organization for the present work.
Ethical statement
All analyses in this systematic review and meta-analysis were based on previous published studies that met ethical guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, S., Chen, J.W., Guo, B. et al. Preoperative Antisepsis with Chlorhexidine Versus Povidone-Iodine for the Prevention of Surgical Site Infection: a Systematic Review and Meta-analysis. World J Surg 44, 1412–1424 (2020). https://doi.org/10.1007/s00268-020-05384-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-020-05384-7