Abstract
Purpose
To compare bacterial cultures from three sterilization methods immediately before and after cataract surgery.
Design
A prospective randomized open-label group-comparison study.
Methods
We investigated 75 eyes in 73 consecutive patients undergoing cataract surgery. After swabbing the eyelid and surrounding area, patients were randomly assigned to one of 3 eye-washing methods: patients administered one drop of 5 % povidone–iodine (Group A); patients whose conjunctival sac was washed with 0.02 % chlorhexidine while everting the eyelid (Group B); or 0.02 % chlorhexidine as above but without eyelid eversion (Group C). In each group, specimens were collected from the conjunctival sac immediately before and after eye washing and again at completion of surgery, along with aqueous humor. The post-surgical condition of the corneal epithelium and the severity of anterior chamber inflammation were assessed by use of a slit-lamp microscope.
Results
In Groups A and C, the percentage of eyes with conjunctival bacteria decreased significantly from immediately before to immediately after washing (Group A, p = 0.008; Group C, p = 0.016), but there was no significant decrease in Group B (p = 0.125). Slit-lamp microscopy showed that inflammation of the anterior chamber 1 day after surgery was significantly milder in Group C than in Group B (p = 0.032).
Conclusion
Eye-washing methods without eyelid eversion are more effective in reducing conjunctival bacteria before surgery and anterior chamber inflammation after surgery than those with eyelid eversion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There have been remarkable technical advances in cataract surgery, and many patients enjoy good postoperative visual acuity. At the same time, patients are demanding greater safety and expect an active approach to preventing complications that may affect postoperative visual function. Endophthalmitis is a potentially serious postoperative complication of cataract surgery; even with appropriate treatment, the final visual acuity is unfavorable, with one study reporting acuity of ≤20/200 in 35.7 % and 20/200 to 20/40 in 36.7 % [1].
Reports show that the incidence of endophthalmitis after cataract surgery is 0.03 % [2] to 1.02 % [3], with a mean incidence of 0.1 % [2–5]. As such, endophthalmitis after cataract surgery remains a persistent problem warranting further investigations into prevention. Speaker et al. [6] report that bacteria on either the eyelid or conjunctiva may invade the eye and cause postoperative endophthalmitis. This suggests that thorough preoperative sterilization of the cornea, conjunctiva, and eyelid is critical in preventing postoperative endophthalmitis. Accordingly, eye washing before surgery should involve more thorough sterilization. Considering that current methods vary greatly among medical institutions, a method that sterilizes the eye efficiently is needed. Several studies that report both the prophylactic administration of antibiotics and growing evidence of the efficacy of preoperative sterilization, mainly with preoperative povidone–iodine eyewash [7–12].
However, no reports compare post-cataract surgery results after application of different methods of eye washing.
In this evidence-based analysis, we assessed the effects on bacterial growth in the conjunctival sac and clinical findings after cataract surgery for three different methods of preoperative eye washing, using both povidone–iodine and chlorhexidine and administering with both eversion and non-eversion of the eyelid. Because there is no evidence that 0.02 % chlorhexidine gluconate can prevent postoperative endophthalmitis, we established a povidone–iodine group for which such evidence exists.
Subjects and methods
The study included 75 eyes of 73 consecutive patients who underwent phacoemulsification (Infinity; Alcon Surgical, Fort Worth, TX, USA) and intraocular lens implantation via a temporal corneal incision, at St Luke’s International Hospital in Tokyo, Japan, between 1 June 2008 and 31 July 2009. A total of 34 eyes in 33 male patients and 41 eyes in 40 female patients aged 41–93 years (mean age ± SD 71.5 ± 10.7 years) were observed for 1 month after surgery in a prospective randomized open-label group-comparison study. The study included patients with senile cataracts, patients who underwent cataract surgery alone, and patients with virgin eyes. We excluded patients with atopy, patients who had used antibiotics within 1 week before surgery, patients with inflammatory diseases of the external eye, and patients with known hypersensitivity to the iodine agent used in the study. The study was approved by the clinical review board of our hospital, and informed consent was obtained from each patient.
Levofloxacin ophthalmic eye drops (0.5 %) (Santen Pharmaceutical, Osaka, Japan) were instilled 4 times daily starting 3 days before surgery, and approximately 30 ml 10 % povidone–iodine (Meiji Seika, Tokyo, Japan) was administered to the eyelid and the surrounding area including the lid margin. The eyes were then washed using one of the following 3 eye-sterilization methods to which patients were randomly assigned.
-
In Group A, one drop of 5 % povidone–iodine was instilled on the surface of the cornea and conjunctiva, which was subsequently washed with 100 ml physiological saline solution without eyelid eversion.
-
In Group B, the eye and surrounding area were washed with 100 ml 0.02 % chlorhexidine gluconate, followed by 100 ml physiological saline solution wash while the eyelid was everted.
-
In Group C, the eye and surrounding area were washed with 100 ml 0.02 % chlorhexidine gluconate, followed by 100 ml physiological saline solution wash without eyelid eversion.
For each patient, culture specimens were collected from the conjunctival sac immediately before and after eye washing and again at the completion of surgery, at which time culture specimens from the anterior chamber were also obtained. Samples from the conjunctival sac were collected by inserting a sterile cotton swab into the inferior conjunctival fornix, after instillation of 0.4 % oxybuprocaine, and sliding it forward and backwards once. Aqueous humor culture was obtained through the surgical wound by use of a 27 G needle with a 0.1 ml syringe, with collection in “seed cube” specimen containers (Mitsubishi Chemical Medience, Tokyo, Japan). Refrigerated specimens were transported to the laboratory (Mitsubishi Chemical Medience) for direct isolation culture or enrichment culture under either aerobic or anaerobic conditions. Specimens from 3 groups were compared for the presence and type of bacteria detected. For isolation culture, samples were inoculated on plates of sheep’s blood agar (Eiken Kagaku, Tokyo, Japan), chocolate agar (Becton Dickson, Tokyo, Japan), CHROM agar (Becton Dickson), and Anaero Columbia agar with rabbit blood (Becton Dickson). Samples were inoculated on plates of GAM semisolid agar (Nissui Seika, Tokyo, Japan) for enrichment culture.
Phacoemulsification and intraocular lens insertion were performed in the standard fashion by two surgeons with 31 and 10 years of surgical experience in ophthalmology, respectively. Incisions were made on the temporal side. At the end of cataract surgery, 1.0 mg (0.3 ml) dexamethasone was injected under the conjunctiva in all cases. Slit-lamp microscopy was performed to assess corneal condition on postoperative day 1 and inflammatory cells in the anterior chamber on postoperative days 1, 3, 7, and 1 month. Inflammatory cells in the anterior chamber were graded as 0, ±, 1+, 2+, or 3+. Patients’ clinical features and duration of surgery were analyzed for each group. Statistical analysis was performed by one-way layout analysis of variance and the chi-squared test using SPSS 15.0J (SPSS Japan, Tokyo, Japan), with significance accepted at p < 0.05.
Results
Patients’ profiles
Clinical characteristics and duration of surgery in Groups A, B, and C are shown in Table 1. Of 75 eyes in 73 patients, 24 eyes (32 %) were assigned to Group A, 24 eyes (32 %) to Group B, and 27 eyes (36 %) to Group C. Mean age was 71.8 (SD ±10.5) years in Group A, 71 (±9.6) years in Group B, and 71.8 (±12.2) years in Group C. One-way layout analysis of variance detected no significant difference in either age or duration of surgery between the 3 groups. Similarly the chi-squared test showed no significant difference in the prevalence of diabetes between the 3 groups.
Results of bacterial culture
Percentage of bacteria-positive eyes
Table 2 shows the percentage of eyes with a bacteria-positive conjunctival sac immediately before and after eye washing and after surgery, and eyes with postoperative bacteria-positive anterior chamber fluid in each group. The chi-squared test detected no significant differences among the groups. McNemar’s chi-squared test revealed a significant decrease in the percentage of bacteria-positive eyes immediately after versus immediately before eye washing in Groups A (p = 0.008) and C (p = 0.016), whereas there was no significant decrease in Group B (p = 0.125).
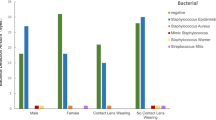
Bacterial isolates
Table 3 shows all bacterial isolates for all groups. A total of 39 bacterial strains were detected from the conjunctival sac immediately before washing the eye. Coagulase-negative staphylococci (CNS) including Staphylococcus epidermidis (S. epidermidis) were the most common (13 eyes, 33.3 %), followed by Corynebacterium species (11 eyes, 28.2 %) and Propionibacterium acnes (P. acnes) (10 eyes, 25.6 %). For all groups, S. epidermidis, Corynebacterium species, and P. acnes were detected at high frequency in the conjunctival sac immediately before washing the eye.
CNS (including S. epidermidis) in the conjunctival sac immediately after washing was noted in 1 eye (4.16 %) from Group A, 4 eyes (16.7 %) from Group B, and 0 eyes from Group C. Chi-squared analysis showed that CNS was detected immediately after washing in significantly more eyes from Group B than in those from the other groups (p = 0.049).
Slit-lamp microscopic findings after surgery
Postoperative corneal findings
Corneal epithelial edema was noted in 1 eye (4.16 %) from Group A, 1 eye (4.16 %) from Group B, and 3 eyes (11.1 %) from Group C. Folding of Descemet’s membrane was noted in 1 eye (4.16 %) from Group A, 5 eyes (20.8 %) from Group B, and 4 eyes (14.8 %) from Group C. No significant differences among the groups were found by chi-squared analysis.
Severity of anterior chamber inflammation
A difference of 1+ or more for inflammation of the anterior chamber on slit-lamp microscopy was defined as significant. Anterior chamber inflammation of ≥1+ on slit-lamp microscopy was noted in 16 eyes (66.6 %) from Group A, 18 eyes (75 %) from Group B, and 11 eyes (40.7 %) from Group C. Inflammation of the anterior chamber 1 day after surgery was significantly milder in Group C than in the other groups (p = 0.032). There were no significant differences among the groups with regard to severity of anterior chamber inflammation on days 3 (p = 0.336) or 7 (p = 0.113). No patients had anterior chamber inflammation at 1 month after surgery.
Complications
Within 1 month of follow-up, no obvious complications, for example endophthalmitis, posterior capsule rupture, or Zinn’s zonular dialysis, were noted for any of the 75 eyes examined in this study.
Discussion
Although cataract surgery has become less invasive with the use of small incisions and is associated with fewer complications today, postoperative endophthalmitis remains a serious problem. A variety of preoperative countermeasures, for example instillation or infusion of antimicrobial drugs, eyelash removal, and eye washing with povidone iodine, are used to prevent postoperative endophthalmitis. Ciulla et al. [4] report an evidence-based assessment of these measures, which were assigned a recommendation level of either A (crucial to clinical outcome), B (moderately important to clinical outcome), or C (possibly relevant, but not definitely related to clinical outcome). Only sterilization with povidone iodine was assessed as level B; all other measures remained at recommendation level C. Thus, washing the eye to prevent contamination of the operating field is the most fundamental method of preventing infections. Therefore, to better utilize preoperative eye washing methods, we examined whether positivity for bacterial culture in the conjunctival sac and anterior chamber fluid changed after eye washing and after surgery, whether the findings differed depending on the method of eye washing, and whether these had any effect on postoperative slit-lamp microscopic findings.
Hara et al. [2] reported conjunctival bacteria in 37 % of unwashed eyes before cataract surgery; in our study the number was slightly higher at 42.7 %. In previous reports, bacterial positivity of the conjunctival sac was seen in 0.06 % [6] to 27.6 % [7] of eyes immediately after washing, and anterior chamber fluid was positive in 1.7 % [2] to 43 % [13] of eyes at completion of surgery. In our study, the conjunctival sac was positive in 17.3 % of eyes immediately after washing, and the anterior chamber fluid was positive in 2.7 % at completion of surgery. Detection in the conjunctival sac immediately after washing the eye was slightly higher than previously reported. This difference may be because of detection bias, because we performed enrichment culture, anaerobic culture, and direct culture. In addition, both the method of washing and the disinfectants used vary widely among institutions, compounded further by different surgical procedures.
As shown in Table 2, the conjunctival sac was positive for bacteria immediately before washing in 50 % of Group A, 41.6 % of Group B, and 37.0 % of Group C. Immediately after washing positive cultures were obtained in 16.7 % of Group A, 25 % of Group B, and 11.1 % of Group C. Compared with immediately before washing, McNemar’s chi-squared test revealed a significant decrease in bacterial positivity in the conjunctival sac immediately after washing the eye in Groups A (p = 0.008) and C (p = 0.016), whereas no significant difference was found in Group B (p = 0.125). When the eye was washed without everting the eyelid, bacterial positivity of the conjunctival sac was lower.
The Endophthalmitis Vitrectomy Study Group reports that CNS (including S. epidermidis) are a common cause of postoperative endophthalmitis [14]. In recent years, late-onset endophthalmitis caused by P. acnes, generally occurring approximately 1 month after cataract surgery, has attracted particular attention. Patients may recover after either topical or oral administration of antibiotics, but recurrence is common [15]. Although in our study 0.5 % levofloxacin was instilled four times daily from 3 days before surgery, a total of 39 bacterial strains were detected in the conjunctival sac immediately before eye washing (Table 3). S. epidermidis, Corynebacterium species, and P. acnes were prominent in the conjunctival sac immediately before washing of the eye. The conjunctival sac seems to be an environment in which bacteria are unlikely to be detected, because of the administration of antimicrobial drugs. Because P. acnes and S. epidermidis are bacteria present in the deep structure of the skin (hair follicles), these microorganisms are likely to emerge on the skin surface and be easily detected in the setting of eyelid eversion.
Some S. epidermidis strains may have been detected as CNS. Accordingly, each group was examined for CNS (including S. epidermidis) in the conjunctival sac immediately after eye washing. Significantly more bacteria were detected in Group B, suggesting that many bacteria from the hair follicles spread into the conjunctiva by lid eversion during eye washing, resulting in detection of more bacteria and a potentially greater risk of endophthalmitis.
The Japanese Association for Ocular Infection (JAOI) recommended preoperative administration of antibiotics for cataract surgery in 1995 [16]. In 2008, Inoue et al. [7] instilled levofloxacin for 3 days and washed the eyes with a dilute iodine solution. Yet, even after these procedures bacteria, including P. acnes and S. epidermidis, were detected. These findings suggest that, in practice, complete removal of bacteria from the conjunctival sac by washing is not possible. Yet, although complete removal may not be possible, an optimum method of eye washing is clinically important in minimizing the number of bacteria in the surgical field.
That significantly milder inflammation of the anterior chamber was noted 1 day after surgery in Group C compared to Group B suggests that everting the eyelid during preoperative washing may promote an environment for endophthalmitis. One reason may be that eyelid eversion before surgery may cause minor trauma to the cornea and anterior chamber. Because there was no significant difference in immediate postoperative bacterial detection between Groups B and C, either in the aqueous humor or conjunctival sac, conjunctival contamination is not likely to be a large contributing factor to the different postoperative inflammation between the two groups.
This prospective randomized study has some limitations. Because the sample size was small (75 eyes), only cataract surgery via a temporal corneal incision was examined and only three of the many methods of eye washing were analyzed. Although this study suggests an optimum method for eye washing, further investigation with larger sample sizes are warranted to corroborate these results. Larger studies may be necessary to more clearly assess the relationship between optimum eye washing methods and the occurrence of endophthalmitis.
References
Lindstrom M, Weide G, Stenevi U, Thorburn W, Montan P. Endophthalmitis after cataract surgery: a nationwide prospective study evaluating incidence in relation type and location. Ophthalmology. 2007;114:866–70.
Hara T, Hoshi N, Hara T. Changes in bacterial strains before and after cataract surgery. Ophthalmology. 1996;103:1876–9.
Leong JK, Shah R, McCluskey PJ, Benn RA, Taylor RF. Bacterial contamination of the anterior chamber during phacoemulsification cataract surgery. J Cataract Refract Surg. 2002;28:826–33.
Ciulla TA, Starr MB, Masket S. Bacterial endophthalmitis prophylaxis for cataract surgery. An evidenced-based update. Ophthalmology. 2002;109:13–24.
Mamalis N. Endophthalmitis. J Cataract Refract Surg. 2002;28:729–30.
Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone–iodine. Ophthalmology. 1991;98:1769–75.
Inoue Y, Usui M, Ohashi Y, Shiota H, Yamazaki T. Preoperative Disinfection Study Group: preoperative disinfection of the conjunctival sac with antibiotics and iodine compounds: a prospective randomized multicenter study. Jpn J Ophthalmol. 2008;52:151–61.
Seal DV, Barry P, Gettinby G, Lees F, Peterson M, Revie CW, et al. ESCRS Endophthalmitis Study Group: ERCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: case for a European multicenter study. J Cataract Refract Surg. 2006;32:396–406.
Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW. ESCRS Endophthalmitis Study Group: ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: preliminary report of principal results from a European multicenter study. J Cataract Refract Surg. 2006;32:407–10.
Hori Y, Nakazawa T, Maeda N, Sakamoto M, Yokokura S, Kubota A, et al. Susceptibility comparisons of normal preoperative conjunctival bacteria to fluoroquinolones. J Cataract Refract Surg. 2009;35:475–9.
Shimada H, Arai S, Nakashizuka H, Hattori T, Yuzawa M. Reduction of anterior chamber contamination rate after cataract surgery by intraoperative surface irrigation with 0.25 % povidone–iodine. Am J Ophthalmol. 2011;151:11-7.
Fernandez-Rubio E, Urcelay JL, Cuesta-Rodriquez T. The antibiotic resistance pattern of conjunctival bacteria: a key for designing a cataract surgery prophylaxis. Eye. 2009;23:1321–8.
Dickey JB, Thompson KD, Jay WM. Anterior chamber aspirate cultures after uncomplicated cataract surgery. Am J Ophthalmol. 1991;112:278–82.
Endophthalmitis Vitrectomy Group. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113:1479–96.
Meisler DM, Mandelbaum S. Propiobacterium-associated endophthalmitis after extracapsular cataract extraction. Review of reported cases. Ophthalmology. 1989;96:54–61.
Kitano S. Preoperative administration of antibiotics for cataract surgery. Jpn J Ophthalmic Surg. 1995;8:717–9.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Inagaki, K., Yamaguchi, T., Ohde, S. et al. Bacterial culture after three sterilization methods for cataract surgery. Jpn J Ophthalmol 57, 74–79 (2013). https://doi.org/10.1007/s10384-012-0201-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-012-0201-0