Abstract
Background
Stoma reversal in patients with an incisional hernia represents a clinical dilemma, as it remains unknown whether hernia repair should be concomitantly employed. We aimed at examining postoperative complications and mortality in patients undergoing stoma reversal with or without concomitant hernia repair.
Methods
This study included all patients subjected to stoma reversal between 2010 and 2016 at our institution. Patients were grouped according to conductance of concomitant incisional hernia repair or not. The primary outcome was anastomotic leak (AL). Secondary outcomes were surgical site occurrences (SSO), overall surgical complications, 90-day mortality and overall survival.
Results
In total, 142 patients were included of whom 18 (13%) underwent concomitant hernia repair. The incidence of AL was significantly higher in patients subjected to concomitant hernia repair (four out of 18 [22.2%]) compared with patients undergoing stoma reversal alone (three out of 124 [2.4%], P = 0.002). Additional variables associated with AL were duration of surgery (P < 0.001) and ischemic heart disease (P = 0.039). Twenty-two patients (15.5%) developed a SSO: eight (44.4%) in the hernia repair group and 14 (11.3%) in the non-hernia repair group (P < 0.001). In the multivariable analysis, concomitant hernia repair remained significantly associated with development of postoperative complications (OR = 5.92, 95% CI = 1.54–25.96, P = 0.012).
Conclusions
Compared with stoma reversal alone, incisional hernia repair concomitant with stoma reversal was associated with a higher incidence of AL and other complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
One of the most frequent complications after laparotomy is incisional hernia, which is reported in up to 20% of patients [1]. Temporary intestinal stomas are often created during emergency surgery or as a protective measure after colorectal resection. Patients with a temporary stoma after emergency surgery are at an increased risk of incisional hernia formation [2]. Repair of the incisional hernia in conjunction with stoma reversal as a one-stage procedure is tempting because of potential optimized time- and cost-effectiveness, though a recent study only found a marginally lower cost of a single-stage procedure [3]. In contrast, a two-stage procedure with postponement of the hernia repair may be a safer choice. Spillage of bowel contents during stoma takedown and construction of the anastomosis could potentially contaminate the surgical field and increase the rate of complications [4]. The most severe complication after stoma reversal is anastomotic leak that leads to increased morbidity, length of hospital stay, need for intensive care and thirty-day mortality [5,6,7]. The incidence of AL after stoma reversal depends on the type of stoma.
A previous study reported a 65% wound morbidity rate after a single-stage approach for enterocutaneous fistula takedown combined with large complex abdominal wall reconstruction [8]. Kugler et al. [9] found a 53% rate of surgical site occurrences (SSO) after a dual-stage approach to ventral hernia repair in potentially contaminated fields.
Until recently, we have routinely performed stoma reversal and incisional hernia repair as a single-stage procedure at our institution. The aim of the present study was to investigate whether a concomitant incisional hernia repair influenced the incidences of AL, 90-day overall complications and 90-day mortality in patients undergoing stoma reversal.
Materials and methods
This retrospective cohort study was conducted and reported in accordance with the STROBE guidelines [10]. We included all patients undergoing elective reversal of an intestinal end-stoma between October 1, 2010 and May 10, 2016 at the Digestive Disease Center, Bispebjerg University Hospital, Denmark. Patients were identified in the administrative surgical database by their relevant International Classification of Diseases 10th version procedure codes (Table 1). All patients undergoing reversal of loop ostomies were excluded, because these procedures do not require a laparotomy. Data on patient characteristics, surgical history, intraoperative data and 90-day postoperative complications were assessed by medical chart review. The following patient characteristics were retrieved: age, gender, body mass index (BMI), tobacco use, excessive alcohol intake (defined as > 168 g/week for women and > 252 g/week for men), American Society of Anesthesiologists’ (ASA) score, ischemic heart disease, chronic obstructive pulmonary disorder, diabetes, the use of immunosuppressive medication, previous intraabdominal surgery, duration of surgery, other procedures in addition to the stoma reversal, previous AL, type of anastomosis (colo-colonic, colorectal, ileo-colonic or ileo-ileal), length of stay and readmission. We also recorded the size of the hernia defect, number of defects, mesh type, mesh placement, mesh size and lateral release procedures, in patients undergoing concomitant incisional hernia repair. Exclusively patients with incisional hernias undergoing mesh repair were included in the hernia repair group, because non-mesh hernia repair was not considered to technically differ significantly from standard laparotomy closure.
The primary outcome was AL, defined as a grade C leakage requiring reoperation [11]. The secondary outcomes were any complication, complications with a Clavien Dindo score ≥ III, 90-day mortality and 3-year cumulative survival. The severity of postoperative complications was graded according to the Clavien Dindo classification [12]. The outcome “any complication” included the following four subgroups (1) AL, (2) SSO (superficial or deep surgical site infection, fascial dehiscence, seroma, enterocutaneous fistula or late bleeding/hematoma [4]), (3) pulmonary complications (pneumonia, atelectasis, hydrothorax, hemothorax or pneumothorax) and (4) other complications. Next, patients with Clavien Dindo scores below III were compared to patients with a Clavien Dindo score above or equal to III, to assess the severity of complications with and without concomitant hernia repair. Data on overall survival were extracted from the Danish Civil Person Register [13].
Statistics
Univariable analysis was performed on the entire cohort, comparing the recorded variables between (a) patients with and without a concomitant hernia repair; (b) patients with and without AL; and (c) patients with and without any postoperative complication. Continuous and categorical variables were compared using Student’s t test after a normality test and Chi-square test, respectively. Only a univariable analysis was performed on the primary outcome due to the small number of cases with AL. Multivariable analysis was performed on the composite outcome “any complication.” Potential confounding variables included in the multivariable analysis were selected according to a P value < 0.1 in the univariable analyses. The three-year cumulative survival was compared between the two groups using the log-rank test.
The statistical software used for all analyses was R 3.2 (Foundation for Statistical Computing, Vienna, Austria). P values < 0.05 were considered statistically significant. The study was approved by the Danish Data Protection Agency (j. no. 2012-58-0004).
Results
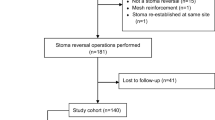
A total of 150 patients underwent stoma reversal during the study period. Eight patients were excluded from the cohort: Five patients underwent stoma reversal during an emergency procedure, two underwent loop colostomy reversal without laparotomy, and one patient was lost to follow-up, leaving 142 for analysis (Fig. 1).
The indications for the initial stoma formation were benign condition (n = 88), cancer (n = 45), trauma (n = 5) and iatrogenic surgical injury (n = 4). In total, 18 (13%) patients underwent stoma reversal and concomitant incisional hernia repair. This patient group had higher BMI, ASA score, number of previous abdominal procedures, time from primary surgery to stoma closure and operative time (Table 2). The median size of the fascial defect of the hernias was 5.6 cm (range: 2–20 cm) horizontally and 7.5 cm (range: 3–18 cm) vertically. The mesh placement was retromuscular in 10 patients, intraperitoneal in seven patients and onlay in one patient. Fourteen of the implanted meshes were synthetic and four were biological. Colorectal consultant surgeons performed all colo-colic and colorectal anastomoses, whereas general surgeons also performed ileo-colic anastomoses.
AL occurred in four of 18 (22.2%) patients in the hernia repair group and in three of 124 (2.4%) patients in the non-hernia repair group (P = 0.002) (Table 3). No patients in the cohort were diagnosed with a minor AL, which only required conservative treatment. The median time from stoma reversal to diagnosis of AL was 8 days (range 3–14). In the univariable analysis, increasing duration of surgery (mean 269 min vs. 174 min, P < 0.001), time from primary surgery to stoma closure (median 602 days [IQR 319–980] vs. 234 days [IQR 148–380], P = 0.018) and ischemic heart disease (2 out of 7 vs. 5 out of 135, P = 0.039) were significantly associated with AL. Detailed information about patients undergoing reoperation for AL is given in Table 4.
Thirteen out of 18 (72.2%) patients in the hernia repair group experienced at least one complication compared with 28 of 124 (22.6%) patients in the non-hernia repair group, P < 0.001 (Table 5). In the hernia repair group, five out of 18 (27.8%) patients had a Clavien Dindo class III complication or higher, compared with 12 out of 124 (9.7%) in the non-hernia group, P < 0.001. Eight (44.4%) patients in the hernia repair group developed a SSO compared to 14 (11.3%) in the non-hernia repair group (P < 0.001) (Table 6). Factors associated with the development of at least one complication included increasing age (P = 0.002), higher BMI (P = 0.008), higher ASA score (P = 0.035), concomitant hernia repair (P < 0.001) and greater number of previous surgeries (P = 0.001) (Table 5). After multivariable adjustment for potential confounders, concomitant hernia repair was the only variable that significantly associated with the development of any postoperative complication after elective stoma reversal (OR 5.92, 95% CI 1.54–25.69, P = 0.012) (Table 7). Patients with any complications had a significantly longer postoperative length of hospital stay (median 12 days [IQR 7–19] vs. 5 days [IQR 3–5], P < 0.001) and higher rate of readmission (8 [19.5%] vs. 5 [5.0%], P = 0.016) (Table 6).
No patients undergoing hernia repair concomitant to stoma reversal died during the 90-day follow-up, whereas three (2.5%) patients who only underwent stoma reversal died during this period. The fatalities occurred 13, 21 and 42 days postoperatively and were due to cerebral infarction, sepsis following AL and unknown reasons (no autopsy), respectively. The three-year cumulative survival for patients undergoing the combined procedure was 80.8% (56.8–100%) compared to 90.7% (84.7–96.7%) after stoma reversal only, P = 0.708.
Discussion
In the current study, we found concomitant hernia repair, longer duration of surgery, time to stoma closure and ischemic heart disease to be associated with AL. Further, concomitant hernia repair was associated with an increased risk of postoperative complications. To our knowledge, this is the first study to specifically evaluate the risks associated with stoma reversal and concomitant hernia repair.
Other studies have reported the risk factors for AL to include male gender, age beyond 60 years, obesity, duration of surgery > 180 min, ASA score ≥ 3, anastomosis close to the anal verge, excessive alcoholic intake, tobacco smoking, hypoalbuminemia, advanced tumor stage, emergency conditions, high intraoperative blood loss and transfusion therapy [14,15,16,17,18,19,20]. AL is relatively rare after stoma reversal and depends on the level of bowel segments joined in the anastomosis. The reported rates of AL vary from 0.4 to 2.9% after ileostomy reversal to 0.3–8.0% after colostomy reversal [5, 21,22,23]. Considering that the majority of anastomoses in our study were either colo-colonic or colorectal, the overall AL rate of 5% is low, whereas the 22% AL rate in patients undergoing concomitant hernia repair is unacceptably high.
The literature on the safety of combining stoma reversal with an additional procedure is limited. Lupinacci et al. [24] did not report an increased rate of AL after a combined surgical intervention with ostomy closure and liver resection in patients with hepatic metastatic disease from colorectal cancer. This finding is probably due to the exclusive inclusion of patients undergoing loop ileostomy closure as opposed to the present study, in which a majority of patients underwent colo-colonic or colorectal anastomoses and no patients underwent closure of a loop ostomy. It remains unknown whether incisional hernia repair in particular increases the incidence of AL. A combined approach induces a longer operative time and more pronounced perioperative stress, as hernia repair often entails wide parietal dissection and implantation of foreign body material. Interestingly, mesh repair increases the systemic inflammatory response compared to sutured repair of a hernia [25], and previous studies have demonstrated an association between the inflammatory activity and collagen turnover which might affect the strength of the anastomosis [26, 27]. Eight patients underwent repair of a fascial defect wider than 10 cm. An increase in intraabdominal pressure after large incisional hernia repair has previously been reported, potentially reducing anastomotic microcirculation [28].
The modified hernia grading scale predicts that the risk of a SSO is 46% in a grade 3 hernia (clean-contaminated, contaminated or dirty operative field) [4]. This is comparable to the 44% incidence of SSO in the present study, as all patients undergoing stoma reversal are categorized as grade 3. A previous study found that ventral hernia repair concomitant to another intraabdominal procedure more than double the risk of developing a SSO. This rate reached 86% in patients undergoing ventral hernia repair in combination with stoma reversal [29]. The incidence of SSO after hernia repair in the current study was rather low compared to studies reporting the results of ventral hernia repair in contaminated fields [8, 9, 29]. In contrast, a recent study examined the effects of prophylactic mesh on IH development at the former stoma site and the rate of SSOs after stoma takedown. Comparable rates of SSO and AL after ostomy takedown were found between patients with and without an additional retromuscular mesh [30]. This study differed from the present in that less than half of the patients had a midline IH present. Moreover, some of the patients only required a small peristomal incision rather than a full laparotomy.
The Ventral Hernia Working Group considers development of SSOs to be an important predictor of hernia recurrence [31], and we thus consider a 44% SSO rate in the hernia repair group to be unacceptably high. If patients require both stoma reversal and hernia repair undergoing a two-stage procedure, the hernia repair could be reduced from level 3 to a level 1 or 2, thus reducing the predicted SSO rate from 46 to 14–27% [4]. Furthermore, AL following stoma reversal and hernia repair including lateral release may require mesh removal and result in “burned bridges” in terms of future hernia repair. On the other hand, possible drawbacks of a dual-stage procedure are also potentially significant, including the risk of complications after exposure to two separate surgical and anesthesiologic procedures. Surgical site infection following mesh repair is a serious condition often requiring reoperation, mesh removal, prolonged hospitalization and higher healthcare expenses [32, 33]. Larger studies are required to evaluate whether a dual-stage approach is economically advantageous compared with a single combined approach.
There are limitations to this retrospective study. The distribution of patients into the two groups was prone to selection bias. Though this might be the case, the only significantly different demographic variables between the case and the control groups were BMI and number of previous surgeries, leaving the two groups relatively comparable. This particular study did not take into account the peri- and postoperative complications that could arise during a secondary hernia repair, nor did it address the issue of hernia-related complications in the waiting period of a dual-stage approach. Furthermore, the study lacked statistical power to allow for multivariable analysis on the risk of AL. Lastly, the low number of patients undergoing concomitant hernia repair in this study increases the risk of a type 1 error.
The findings of this study suggest that the risk of AL and overall complications after stoma reversal is increased by concomitant incisional hernia repair.
References
Sanders DL, Kingsnorth AN (2012) The modern management of incisional hernias. BMJ 344:e2843
Jensen KK, Krarup PM, Scheike T et al (2016) Incisional hernias after open versus laparoscopic surgery for colonic cancer: a nationwide cohort study. Surg Endosc 30:4469–4479
Madabhushi V, Plymale MA, Roth JS et al (2017) Concomitant open ventral hernia repair: what is the financial impact of performing open ventral hernia with other abdominal procedures concomitantly? Surg Endosc 32:1915
Kanters AE, Krpata DM, Blatnik JA et al (2012) Modified hernia grading scale to stratify surgical site occurrence after open ventral hernia repairs. J Am Coll Surg 215:787–793
Phang PT, Hain JM, Perez-Ramirez JJ et al (1999) Techniques and complications of ileostomy takedown. Am J Surg 177:463–466
Kaiser AM, Israelit S, Klaristenfeld D et al (2008) Morbidity of ostomy takedown. J Gastrointest Surg 12:437–441
van de Wall BJ, Draaisma WA, Schouten ES et al (2010) Conventional and laparoscopic reversal of the Hartmann procedure: a review of literature. J Gastrointest Surg 14:743–752
Krpata DM, Stein SL, Eston M et al (2013) Outcomes of simultaneous large complex abdominal wall reconstruction and enterocutaneous fistula takedown. Am J Surg 205:354–358 discussion 358–359
Kugler NW, Bobbs M, Webb T et al (2016) A dual-stage approach to contaminated, high-risk ventral hernia repairs. J Surg Res 204:200–204
Vandenbroucke JP, von Elm E, Altman DG et al (2014) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg 12:1500–1524
Rahbari NN, Weitz J, Hohenberger W et al (2010) Definition and grading of anastomotic leakage following anterior resection of the rectum: a proposal by the International Study Group of Rectal Cancer. Surgery 147:339–351
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Pedersen CB (2011) The Danish Civil Registration System. Scand J Public Health 39:22–25
Buchs NC, Gervaz P, Secic M et al (2008) Incidence, consequences, and risk factors for anastomotic dehiscence after colorectal surgery: a prospective monocentric study. Int J Colorectal Dis 23:265–270
Golub R, Golub RW, Cantu R Jr et al (1997) A multivariate analysis of factors contributing to leakage of intestinal anastomoses. J Am Coll Surg 184:364–372
Rullier E, Laurent C, Garrelon JL et al (1998) Risk factors for anastomotic leakage after resection of rectal cancer. BJS 85:355–358
Jannasch O, Klinge T, Otto R et al (2015) Risk factors, short and long term outcome of anastomotic leaks in rectal cancer. Oncotarget 6:36884–36893
Schrock TR, Deveney CW, Dunphy JE (1973) Factor contributing to leakage of colonic anastomoses. Ann Surg 177:513–518
Choi HK, Law WL, Ho JW (2006) Leakage after resection and intraperitoneal anastomosis for colorectal malignancy: analysis of risk factors. Dis Colon Rectum 49:1719–1725
Telem DA, Chin EH, Nguyen SQ et al (2010) Risk factors for anastomotic leak following colorectal surgery: a case-control study. Arch Surg 145:371–376 discussion 376
Fauno L, Rasmussen C, Sloth KK et al (2012) Low complication rate after stoma closure. Consultants attended 90% of the operations. Colorectal Dis 14:e499–e505
Nagell CF, Pedersen CR, Gyrtrup HJ (2005) Complications after stoma closure. A retrospective study of 11 years’ experience. Ugeskr Laeger 167:1742–1745
Wong RW, Rappaport WD, Witzke DB et al (1994) Factors influencing the safety of colostomy closure in the elderly. J Surg Res 57:289–292
Lupinacci RM, Agostini J, Chirica M et al (2015) Combined stoma reversal and liver resection: a matched case-control study. Am S Surg 210:501–505
Di Vita G, D’Agostino P, Patti R et al (2005) Acute inflammatory response after inguinal and incisional hernia repair with implantation of polypropylene mesh of different size. Langenbecks Arch Surg 390:306–311
Ågren MS, Andersen TL, Mirastschijski U et al (2006) Action of matrix metalloproteinases at restricted sites in colon anastomosis repair: an immunohistochemical and biochemical study. Surgery 140:72–82
Krarup PM, Rehn M, Sand-Dejmek J et al (2013) Rapid morphological changes and loss of collagen following experimental acute colonic obstruction. Int J Colorectal Dis 28:341–347
Angelici AM, Perotti B, Dezzi C et al (2016) Measurement of intra-abdominal pressure in large incisional hernia repair to prevent abdominal compartmental syndrome. G Chir 37:31–36
Berger RL, Li LT, Hicks SC et al (2013) Development and validation of a risk-stratification score for surgical site occurrence and surgical site infection after open ventral hernia repair. J Am Coll Surg 217:974–982
Warren JA, Beffa LR, Carbonell AM et al (2018) Prophylactic placement of permanent synthetic mesh at the time of ostomy closure prevents formation of incisional hernias. Surgery 163:839–846
Ventral Hernia Working G, Breuing K, Butler CE et al (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148:544–558
Govaert JA, Fiocco M, van Dijk WA et al (2015) Costs of complications after colorectal cancer surgery in the Netherlands: building the business case for hospitals. Eur J Surg Oncol 41:1059–1067
Fischer JP, Wes AM, Wink JD et al (2014) Analysis of perioperative factors associated with increased cost following abdominal wall reconstruction (AWR). Hernia 18:617–624
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Baastrup, N.N., Hartwig, M.F.S., Krarup, PM. et al. Anastomotic Leakage After Stoma Reversal Combined with Incisional Hernia Repair. World J Surg 43, 988–997 (2019). https://doi.org/10.1007/s00268-018-4866-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4866-5