Abstract
Purpose
Anastomosis of an acutely obstructed colon is associated with an increased risk of dehiscence. In experimental models, acute obstruction decreases collagen in the colonic wall, but the time course and propagation along the colon of the biochemical changes are unknown. Furthermore, there is a paucity of information on the correlation between these biochemical changes and histological features.
Methods
Forty male Sprague Dawley rats were subjected to partial obstruction by placing a silicone ring around the left colon 30 mm above the reflection. Obstruction was maintained for 0, 1, 2, 3 or 4 days. Samples from five different locations along the colon were analysed on circumference, tissue water content, collagen concentration and histomorphology. Neutrophil and macrophage infiltration was characterized immunohistochemically.
Results
The colonic circumference and water content increased (p < 0.001), while the collagen concentration decreased by 48 % (p < 0.01) proximal to the obstruction already after 1 day. The degree of dilation and collagen reduction did not change significantly over the subsequent 3 days of obstruction, whereas the water content normalized by day 3. Mucosal and submucosal oedema and the relative neutrophil infiltration were highest after 1 day in the colonic segment proximal to the stenosis while the macrophage population continued to increase to day 4. Muscular necrosis in addition to ganglionitis and neuritis in the nervous plexus increased with duration of obstruction.
Conclusions
The pronounced and rapid changes of the composition of cells and the extracellular matrix of the colonic wall following acute obstruction may be of guidance for present surgical treatments and future pharmacological interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer is one of the most frequent malignancies worldwide with over 1.2 million new cases annually [1]. Approximately 15 % present as acute obstructing tumours interrupting the bowel continuity [2] and require prompt treatment. These emergency operations are high-risk procedures [3, 4]. Despite progress in surgical techniques, moving from the staged procedures to resection with construction of a primary anastomosis [4, 5], the presence of colonic obstruction is associated with an increased risk of anastomotic leakage [6, 7] and mortality [8]. Unfortunately, Hartmann's procedure [9, 10] and endoscopic placement of a self-expandable metal stent [11–13] are both associated with drawbacks as well. Regardless of surgical technique, a detailed knowledge of the biochemical and structural changes in the obstructed colonic wall is crucial to better understand the pathophysiology behind and the association with increased anastomotic leakage.
In a non-obstructed colon, anastomotic healing comprises a cascade of events, aiming to restore the function and biomechanical strength in the bowel. The submucosal collagen constitutes the suture-holding tissue and ensures anastomotic integrity in the first postoperative week [14]. During this period, collagen degradation predominates over collagen synthesis resulting in decreased concentration of collagen and reduced anastomotic biomechanical strength [15]. In the obstructed colonic wall, reduced collagen has been observed in rodents [16–19], but the time course as well as propagation of changes along the colon following obstruction has not been addressed previously.
The purpose of the present study was to examine the dimensional, biochemical and morphological changes in the colonic wall following 0 to 4 days of obstruction using an established acute model in rats [17–19].
Methods
Forty male Sprague Dawley rats (Taconic M&B, Ry, Denmark) weighing 348 ± 61 g (mean ± SD) were acclimatized for a minimum of 7 days prior to surgery with free access to standard pellets and tap water [15, 17]. The rats were randomized into five groups of eight rats in each group and subjected to partial colonic obstruction for 0, 1, 2, 3 or 4 days. After surgery, four rats were kept per cage. The study was approved by the local ethics committee for animal studies at Lund University (M174-04).
Anaesthesia and analgesics
Anaesthesia was induced with a mixture of 0.14 mg/kg fentanyl citrate and 4.4 mg/kg fluanisone (Hypnorm®; Janssen-Cilag, Beerse, Belgium), and 2.2 mg/kg midazolam (Dormicum®; F. Hoffmann-La Roche, Basel, Switzerland) given subcutaneously. After the surgery was completed, 0.02 mg/kg buprenorphine (Temgesic®; Schering-Plough, Brussels, Belgium) was injected subcutaneously. This regimen was also used for postoperative analgesia.
Surgery
The abdominal cavity was exposed through a 30-mm midline incision. Partial colonic obstruction was established using a 5-mm-wide silicone ring (6.5 mm inner diameter) placed around the left colon between two marginal veins 30 mm above the peritoneal reflection [17–19]. The ring was closed with single 7-0 polypropylene suture (Ethilon®; Ethicon, Johnson & Johnson, Brussels, Belgium). The abdomen was closed in two separate layers using continuous 4.0 sutures (Vicryl®; Ethicon).
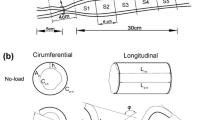
The rats were killed by asphyxiation in a carbon dioxide chamber after 0, 1, 2, 3 or 4 days of colonic obstruction. Five-millimetre-wide segments of the colon were excised at five predefined anatomical locations. Segment A was located 10 mm distal to the ileocolonic junction; segment B was 15 mm and segment C 5 mm proximal to the stenotic silicone ring, both segments 5 mm apart, and segment D 5 mm and segment E 15 mm distal to the ring as detailed in Fig. 1. The segments were cut open at the antimesenterial border, and the colonic circumference was measured in millimetres using a slide caliper. Each segment was bisected for determination of water and collagen contents (segments A, B, C, D and E) and for histopathological (segments C, D and E) and immunohistochemical examination (segments C and D).
Water content and collagen (hydroxyproline) analyses
Tissues were weighed (m Fresh), dried to constant weight at 100 °C and weighed (m Dry). Tissue water content was calculated as: (1 − (m Dry/m Fresh)) × 100 %.
Tissues were hydrolyzed in 6 M hydrochloric acid for 18 h at 110 °C. The acid hydrolysates were evaporated and the washed, acid-free residues dissolved in acetate–citrate buffer [19]. The hydroxyproline content was determined colourimetrically [19].
Histological evaluation
Colonic specimens were fixed in 4 % phosphate-buffered paraformaldehyde for 24 h and embedded in paraffin. Sections (5 μm) were stained with haematoxylin–eosin. A consultant specialised in gastrointestinal pathology evaluated the sections without prior knowledge of group affiliation. Oedema was graded as no, slight or pronounced. The degree of inflammatory cell infiltration was evaluated on a four-graded scale [20].
Immunohistochemical double labelling of neutrophils and macrophages
Tissue sections (5 μm) were deparaffinized, rehydrated and microwaved for 10 min in Tris–ethylenediaminetetraacetic acid (pH 9.0). Double labelling of neutrophils and macrophages was performed using reagents and protocols from Vector Laboratories (Burlingame, CA, USA) unless stated otherwise. Each incubation step was carried out at ambient temperature and was followed by washing in phosphate-buffered saline (pH 7.2) for 5 min.
Endogenous peroxidase activity was quenched with 3 % hydrogen peroxide for 5 min. Sections were then incubated with 2.5 % normal horse serum for 20 min. The rabbit anti-rat neutrophil adsorbed antiserum (AIAD51140; Accurate Chemical & Scientific Corporation, Westbury, NY, USA) [21] was diluted 1:10,000 in 1 % bovine serum albumin (Sigma-Aldrich, St. Louis, MO, USA) and applied for 60 min. The section was then incubated with the anti-mouse/rabbit Ig ImmPRESS peroxidase universal reagent for 30 min. The bound antibody complex was visualized with 3,3′-diaminobenzidine supplemented with nickel chloride for 4 min resulting in grey/black-labelled neutrophils. The tissue section was blocked again with 2.5 % normal horse serum for 20 min. The mouse monoclonal anti-rat CD68 antibody (clone ED1; Serotec, Oxford, UK) [22] was applied at 1:400 dilution in 1 % bovine serum albumin for 60 min. Following 30-min incubation with the anti-mouse/rabbit Ig ImmPRESS peroxidase universal reagent, ImmPACT NovaRED was applied to the section for 2 min resulting in red-labelled macrophages. Sections were counterstained with Mayer's haematoxylin (blue) for 40 s, cleared and mounted using Pertex mounting medium (Histolab Products, Göteborg, Sweden).
Statistics
Hydroxyproline levels were log-transformed to obtain normal distribution. One-way ANOVA with Newman–Keuls was applied for comparisons with day 0. A p < 0.05 was considered statistically significant. Hydroxyproline data are given as geometric mean ± back-transformed standard error (SE) and the other variables as mean ± SD.
Results
We have characterized the temporal and histological changes in the colonic wall following acute mechanical obstruction using a model developed in our laboratory [17–19]. There were no differences in preoperative body weight (p = 0.45) among the five groups. One day-3 rat died during recovery from anaesthesia leaving 39 rats for the analyses. The partially obstructed colon allowed passage of flatus but not faeces, and animals continuously lost weight throughout the study period from 8 ± 9 g after day 1 to 33 ± 6 g after 4 days of obstruction.
Colonic circumference
After 1 day of obstruction, the colonic circumference increased in segment B from 8 ± 1 to 17 ± 2 mm (p < 0.001) and in segment C from 8 ± 2 to 19 ± 2 mm (p < 0.001) (Fig. 2). The colonic dilation did not increase further with duration of obstruction. The colonic circumference of segment A increased from 6 ± 1 mm before obstruction to 12 ± 3 mm (p < 0.01) after 4 days of obstruction. The circumference of distal segment D did not change significantly over time whereas the circumference of segment E decreased after 2 days of obstruction from 11 ± 3 day 0 to 8 ± 1 mm on day 4 (p < 0.01).
Colonic inner circumference (red curves, mean ± SD), tissue water in percent (blue curves, mean ± SD) and hydroxyproline concentration (bars, geometric mean ± back-transformed SE) in the five segments of the colonic wall (see Fig. 1) after 0 to 4 days of obstruction. *p < 0.05, **p < 0.01, ***p < 0.001 compared to day 0
Colonic water content and collagen
The percentage of water in the colonic wall of segment B increased from 80 ± 2 % on day 0 to 86 ± 3 % on day 1 (p < 0.001) and to 83 ± 1 % on day 2 (p < 0.05) but returned to day-0 levels days 3 and 4 (Fig. 2). A similar pattern was observed in segment C, whereas the water content in segments A, D and E did not change with time.
The collagen concentration decreased in segment B after 1 day of obstruction by 39 % from 11.3 ± 1.4 to 6.9 ± 0.9 μg hydroxyproline/mg dry weight (p < 0.01) (Fig. 2). The corresponding value for segment C was 48 % from 12.5 ± 1.3 to 6.5 ± 0.9 μg/mg dry weight (p < 0.01). The collagen concentration did not significantly change further after day 1 in either segment B or C. In segment E, collagen levels increased from days 0 to 3 by 58 % from 11.2 ± 1.7 to 17.7 ± 2.5 μg/mg dry weight (p < 0.05) and from days 0 to 4 by 102 % to 22.7 ± 2.0 μg/mg dry weight (p < 0.01). The collagen levels did not change significantly with duration of obstruction in segment A or D.
Histological and immunohistochemical examinations
These analyses are presented in relation to day 0 (Fig. 3a). Immunohistochemical staining was applied to specifically identify neutrophils and CD68-positive macrophages in selected sections (Fig. 4a and b).
Morphologic changes of the proximal segment of the colon with time of obstruction from day 0 (a), 1 (b), 3 (c) and to day 4 (d). Note mucosal and submucosal oedema with inflammatory cell infiltrate on day 1 (b), while at day 3 (c), inflammation was severe in the submucosa with serosal peritonitis but with less submucosal oedema. d Pronounced ganglionitis was observed on day 4. A artery with adjoining extravasated neutrophils, G ganglionitis, LM/CM longitudinal/circular layers of the tunica muscularis, SM submucosa. Original magnifications: a ×100; b and c ×200; d ×600. Haematoxylin–eosin stain
Immunohistochemical double labelling of neutrophils (black) and macrophages (red) in rat colon proximal (a–d) and distal (e, f) to the obstructive ring applied for 1 day (a–c, e) or for 4 days (d, f). a, b High-resolution (oil) images of adjacent tissue sections treated with (a) or without (b) the primary antibodies directed against neutrophils (a black arrows) and macrophages (a red arrow). b Submucosa (SM) and mucosa (M) are indicated for the purpose of orientation. c–f Note the apparent sparse cellularity on day 1 due to extensive oedema but increased cell density in proximal versus distal segments. Original magnifications: a and b ×1,000, c–f ×400. Mayer's haematoxylin counterstain. g Differential counts of neutrophils, macrophages and other cells (endothelial cells excluded). Cells were counted manually in digital images (×400) of representative areas of the entire thickness of the submucosa in comparison with day 0. C and D above bars refer to the proximal and distal segments to the obstruction
Day 1
The mucosa of the proximal segment C was slightly oedematous and infiltrated with neutrophils. The CD68 immunoreactivity in the mucosa did not change appreciably with obstruction. The muscularis mucosa was thickened with scattered necroses. The submucosa exhibited a pronounced oedema and a moderate infiltrate composed mostly of neutrophils with fewer macrophages, lymphocytes and plasma cells (Figs. 3b and 4c). The submucosa of distal segment D was slightly oedematous but less populated by neutrophils than the C segment (Fig. 4e and g).
Day 2
The mucosal oedema had diminished, while the inflammation persisted. In the submucosa, the oedema was unaltered from day 1, and the inflammatory cell infiltration was moderate. At this stage of obstruction, scattered fibrinoid necroses and thrombosed arteries were apparent. The longitudinal layer of the tunica muscularis was moderately inflamed with scattered necroses. In the myenteric plexus of Auerbach, lymphocytes were found in the ganglions. Ganglionitis was evident in the proximal segment C and, to a lesser degree, in the distal segment D.
Days 3 and 4
Occasional neutrophils were observed in the mucosa of the proximal segment. The submucosal oedema decreased leading to apparently increased cell densities. The inflammatory cell infiltrate peaked on day 3 (Fig. 3c). Although the proportional number of neutrophils declined progressively proximally to the stenosis, it still exceeded that of the distal D segment on day 4 (Fig. 4g). In contrast, the proportion of CD68-positive macrophages was increased and encompassed about half of the cell count in the submucosa both above and below the obstruction on day 4 (Fig. 4d, f and g). Pronounced neuritis with neutrophils and lymphocytes in close vicinity to the neurons in the circular layer of the tunica muscularis was noted on either side of the stenosis. Ganglionitis persisted, and the neurons began to degenerate although necrotic neurons were only demonstrated in the proximal segment C (Fig. 3d). Severe peritonitis was present in the serosa of segment C. There were no obvious histological changes with time in segment E.
Discussion
The collagen-rich submucosa of the colonic wall constitutes the suture-bearing capacity and is paramount for the biomechanical strength of an anastomosis [14]. The present experimental study demonstrates that acute colonic obstruction dramatically and rapidly decreases collagen levels within the first day of obstruction. Interestingly, the kinetics of this collagen loss is analogous to that of the rat uterus during postpartum involution [23]. The early changes in the colon correlated with bowel dilation and pronounced oedema proximal to the obstruction.
Furthermore, neutrophils accumulated proximal as opposed to distal to the stenosis in the submucosa. We did not anticipate this rapid cellular response, and it is possible that the influx of neutrophils peaked even before 1 day of obstruction. On the other hand, the finding is consistent with the significantly higher myeloperoxidase levels previously demonstrated in the colonic wall proximal to the stenosis on day 4 [17].
Collagen degradation is accomplished by the action of one or more matrix metalloproteinases (MMPs). We have previously shown that the reduced collagen in an obstructed colon correlates with MMP activity [17], which tended to increase with the degree of colonic dilation [19]. Neutrophils primarily express MMP-8 and MMP-9, which collectively degrade the colon and type I collagens synergistically [24]. Neutrophils were probably the major cellular sources of MMPs here. To test this hypothesis, the recruitment of neutrophils could be blocked experimentally by giving specific antibodies against the adhesion molecule CD18 [25] or perhaps against responsible chemoattractants such as lipopolysaccharide-induced CXC chemokine [26]. Intuitively, the high mechanical load would increase the susceptibility of collagen to degradation by MMPs, although the opposite has been reported in vitro [27].
We suggest that the colonic wall proximal to an obstructing lesion is depleted of collagen, which impairs the healing conditions of anastomoses [14, 28]. Broad-spectrum MMP inhibition restores anastomotic integrity in a non-obstructive colon [15, 20], but it remains to be demonstrated whether this therapeutic approach is beneficial for anastomotic repair in the obstructed colon as well.
With time, the macrophage infiltration increased in the submucosa of the stenotic area. This may reflect an increased demand for macrophages in protective and reparative processes [29].
It is striking that, after the initial reduction, the collagen concentration proximal to the stenosis was maintained at the same low level. This finding suggests that degraded collagen was compensated for by the synthesis of new collagen molecules. In general, mechanical tension induces a synthetic fibroblast phenotype [30] under experimental conditions that mimic the increased strain exerted on the fibroblasts and myofibroblasts in the dilated colon.
Colonic dilation progressed to the most proximal segment of the colon after 4 days of obstruction. In contrast, the circumference of the most distal segment examined decreased, resulting in increased collagen concentration. The mechanisms are elusive because, in experimental studies on diverting stoma, the collagen concentration in the offloaded colon did not change [31]. Moreover, the chronically obstructed small intestine exhibits increased collagen levels and muscle hypertrophy [32], none of which was demonstrated in the present study.
We did not investigate the ultrastructural arrangements of the collagen fibrils [33] or the specific types of collagen although the submucosa is composed primarily of type I and III collagens [34, 35]. Apart from collagen, hydroxyproline is also found in elastin, but the contribution of elastin-derived compared with collagen-derived hydroxyproline is negligible [36]. It would be interesting to study the changes of other extracellular components such as fibronectin and laminin during colonic obstruction [34].
The scattered necroses observed after 4 days of obstruction in the muscular layer of the colonic wall might inhibit the return of bowel function as we have previously observed [19]. Neural damage including neuritis and ganglionitis in the tunica muscularis, shown here, may impair bowel peristaltic movement and prolong postoperative ileus.
In conclusion, the early and dramatic loss of structural collagen in the large bowel may hint that caution should be taken regarding primary anastomosis, also in patients with only a short history of colonic obstruction. Moreover, our results indicate that it would be worthwhile to test if the loss of connective tissue elements is preventable by pharmacologic means to reduce the risk of anastomotic leakage.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA Cancer J Clin 61:69–90
Deans GT, Krukowski ZH, Irwin ST (1994) Malignant obstruction of the left colon. Br J Surg 81:1270–1276
Waldron RP, Donovan IA (1986) Mortality in patients with obstructing colorectal cancer. Ann R Coll Surg Engl 68:219–221
Runkel NS, Hinz U, Lehnert T, Buhr HJ, Herfarth C (1998) Improved outcome after emergency surgery for cancer of the large intestine. Br J Surg 85:1260–1265
Baccari P, Bisagni P, Crippa S, Sampietro R, Staudacher C (2006) Operative and long-term results after one-stage surgery for obstructing colonic cancer. Hepatogastroenterology 53:698–701
Jex RK, van Heerden JA, Wolff BG, Ready RL, Ilstrup DM (1987) Gastrointestinal anastomoses. Factors affecting early complications. Ann Surg 206:138–141
Golub R, Golub RW, Cantu R Jr, Stein HD (1997) A multivariate analysis of factors contributing to leakage of intestinal anastomoses. J Am Coll Surg 184:364–372
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91:605–609
Wong RW, Rappaport WD, Witzke DB, Putnam CW, Hunter GC (1994) Factors influencing the safety of colostomy closure in the elderly. J Surg Res 57:289–292
Nugent KP, Daniels P, Stewart B, Patankar R, Johnson CD (1999) Quality of life in stoma patients. Dis Colon Rectum 42:1569–1574
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Holzik MF, Grubben MJ et al (2011) Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 12:344–352
Kim JS, Hur H, Min BS, Sohn SK, Cho CH, Kim NK (2009) Oncologic outcomes of self-expanding metallic stent insertion as a bridge to surgery in the management of left-sided colon cancer obstruction: comparison with nonobstructing elective surgery. World J Surg 33:1281–1286
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99:469–476
Halsted WS (1887) Circular suture of the intestine—an experimental study. Am J Med Sci 188:436–460
Syk I, Ågren MS, Adawi D, Jeppsson B (2001) Inhibition of matrix metalloproteinases enhances breaking strength of colonic anastomoses in an experimental model. Br J Surg 88:228–234
Aguilar-Nascimento JE, Mathie RT, Man WK, Williamson RC (1998) Collagen variation during experimental acute obstruction of the left colon. Dig Surg 15:252–255
Syk I, Mirastschijski U, Jeppsson BW, Ågren MS (2003) Experimental colonic obstruction increases collagen degradation by matrix metalloproteinases in the bowel wall. Dis Colon Rectum 46:1251–1259
Törnqvist A, Blomquist P, Ahonen J, Jiborn H, Zederfeldt B (1988) The effect of stenosis on collagen metabolism in the colonic wall. Studies in the rat. Acta Chir Scand 154:389–393
Rehn M, Ågren MS, Syk I (2011) Collagen levels are normalized after decompression of experimentally obstructed colon. Colorectal Dis 13:e165–e169
Ågren MS, Andersen TL, Andersen L, Schiodt CB, Surve V, Andreassen TT et al (2011) Nonselective matrix metalloproteinase but not tumor necrosis factor-alpha inhibition effectively preserves the early critical colon anastomotic integrity. Int J Colorectal Dis 26:329–337
Andrews FJ, Malcontenti-Wilson C, O'Brien PE (1994) Polymorphonuclear leukocyte infiltration into gastric mucosa after ischemia–reperfusion. Am J Physiol 266:G48–G54
Damoiseaux JG, Dopp EA, Calame W, Chao D, MacPherson GG, Dijkstra CD (1994) Rat macrophage lysosomal membrane antigen recognized by monoclonal antibody ED1. Immunology 83:140–147
Harkness RD, Moralee BE (1956) The time-course and route of loss of collagen from the rat's uterus during post-partum involution. J Physiol 132:502–508
Ågren MS, Andersen TL, Mirastschijski U, Syk I, Schiødt CB, Surve V et al (2006) Action of matrix metalloproteinases at restricted sites in colon anastomosis repair: an immunohistochemical and biochemical study. Surgery 140:72–82
Törkvist L, Månsson P, Raud J, Larsson J, Thorlacius H (2001) Role of CD18-dependent neutrophil recruitment in skin and intestinal wound healing. Eur Surg Res 33:249–254
Van Den Steen PE, Wuyts A, Husson SJ, Proost P, Van Damme J, Opdenakker G (2003) Gelatinase B/MMP-9 and neutrophil collagenase/MMP-8 process the chemokines human GCP-2/CXCL6, ENA-78/CXCL5 and mouse GCP-2/LIX and modulate their physiological activities. Eur J Biochem 270:3739–3749
Chang SW, Flynn BP, Ruberti JW, Buehler MJ (2012) Molecular mechanism of force induced stabilization of collagen against enzymatic breakdown. Biomaterials 33:3852–3859
Cronin K, Jackson DS, Dunphy JE (1968) Changing bursting strength and collagen content of the healing colon. Surg Gynaecol Obstet 126:747–753
Murray PJ, Wynn TA (2011) Protective and pathogenic functions of macrophage subsets. Nat Rev Immunol 11:723–737
Kessler D, Dethlefsen S, Haase I, Plomann M, Hirche F, Krieg T et al (2001) Fibroblasts in mechanically stressed collagen lattices assume a “synthetic” phenotype. J Biol Chem 276:36575–36585
Törnqvist A, Blomquist P, Jiborn H, Zederfeldt B (1990) The effect of diverting colostomy on anastomotic healing after resection of left colon obstruction. An experimental study in the rat. Int J Colorectal Dis 5:167–169
Storkholm JH, Zhao J, Villadsen GE, Hager H, Jensen SL, Gregersen H (2007) Biomechanical remodeling of the chronically obstructed Guinea pig small intestine. Dig Dis Sci 52:336–346
Gabella G (1987) The cross-ply arrangement of collagen fibres in the submucosa of the mammalian small intestine. Cell Tissue Res 248:491–497
Braskén P, Lehto M, Renvall S (1990) Fibronectin, laminin, and collagen types I, III, IV and V in the healing rat colon anastomosis. Ann Chir Gynaecol 79:65–71
Klein L, ChandraRajan J (1977) Collagen degradation in rat skin but not in intestine during rapid growth: effect on collagen types I and III from skin. Proc Natl Acad Sci U S A 74:1436–1439
Vaos GC, Lister J (1987) Elastic fibers in musculature of rectosigmoid colon: normal findings in children and changes in Hirschsprung's disease—a preliminary report. J Pediatr Surg 22:252–256
Acknowledgment
Eygló Gisladóttir, Histocenter AB, Västra Frölunda, Sweden, carried out the immunohistochemical stainings.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Krarup, PM., Rehn, M., Sand-Dejmek, J. et al. Rapid morphological changes and loss of collagen following experimental acute colonic obstruction. Int J Colorectal Dis 28, 341–347 (2013). https://doi.org/10.1007/s00384-012-1548-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-012-1548-x