Abstract
Background
Robotic systems introduced new surgical and technical demands. Surgical flow disruptions are critical for maintaining operating room (OR) teamwork and patient safety. Specifically for robotic surgery, effects of intra-operative disruptive events for OR professionals’ workload, stress, and performance have not been investigated yet. This study aimed to identify flow disruptions and assess their association with mental workload and performance during robotic-assisted surgery.
Methods
Structured expert-observations to identify different disruption types during 40 robotic-assisted radical prostatectomies were conducted. Additionally, 216 postoperative reports on mental workload (mental demands, situational stress, and distractions) and performance of all OR professionals were collected.
Results
On average 15.8 flow disruptions per hour were observed with the highest rate after abdominal insufflation and before console time. People entering the OR caused most flow disruptions. Disruptions due to equipment showed the highest severity of interruption. Workload significantly correlated with severity of disruptions due to coordination and communication.
Conclusions
Flow disruptions occur frequently and are associated with increased workload. Therefore, strategies are needed to manage disruptions to maintain OR teamwork and safety during robotic-assisted surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The adoption of robotic-assisted surgery created new demands for operating room (OR) teams [1]. The spatial separation introduced new challenges in maintaining situational awareness, team coordination, and information exchange [2, 3]. The identification of process inefficiencies contributes to an enhanced understanding of system-related issues responsible for delivery of robotic-assisted surgery [4].
Surgical flow disruptions are events that potentially distract or momentarily interrupt OR team members from their tasks or stop operation flow [5]. They have been identified across a variety of surgical specializations [5,6,7,8,9,10]. Previous research suggested that flow disruptions during robotic surgery are related to coordination, equipment, and training [4, 11, 12]. Nonetheless, the current literature concerning specific effects of flow disruptions during robotic-assisted surgery is limited [13].
A key hallmark of surgical performance is coping with intra-operative workload and stress [14]. Research in non-robotic settings suggests that frequent intra-operative disruptions are associated with increased mental workload and stress for OR professionals [15,16,17,18]. Workload is defined as “cost incurred by a human operator to achieve a particular level of performance” and evolves from interactions between task demands, circumstances, skills, behavior, and perceptions [19]. High workload can result in higher stress levels, potentially deteriorating communication and decision making, and, subsequently, impacts surgical performance and safety [14, 20, 21]. It has also been argued that flow disruptions differ in their impact on process outcomes and human performance [5, 8]. On the other hand, previous investigations suggested that robotic-assisted surgery is less stressful, physically demanding, and complex [22, 23]. Partly, because surgeons are less distracted while being at the console [2, 22, 24]. Previous investigations on disruptions and workload during robotic surgery are mainly based on simulations and almost exclusively focused on surgeons, thus, ignoring the intra-operative demands of OR nurses and anesthetists [21, 22, 24,25,26].
We sought to identify frequencies and severities of flow disruptions during robotic-assisted surgery and assess concurrent mental workload and performance of all OR professionals. The main objective was to explore associations between flow disruptions and workload as well as surgical performance during robotic-assisted surgery.
Materials and methods
Study design, procedure, and sample
A prospective and multi-method design was established, combining structured observations of robot-assisted radical prostatectomies with OR professionals’ self-reports. This study was part of a research project about disruptions and teamwork in robot-assisted procedures [27]. Assessments were carried out in an Urological Department of an University Hospital in Southern Germany. All observed procedures were performed with the Si da Vinci model. Ethical approval was given by the Ethics Committee of the Faculty of Medicine, Munich University (539-11). OR team members were informed before observations and provided written informed consent.
Observations started when the patient arrived at the OR and stopped when the patient left the OR. During procedures, flow disruptions were identified in real time by a trained observer on-site (first author). The observer sat next to the assisting surgeon, being able to overlook the whole OR. At the end of each observed procedure, all OR team members were asked to fill out short questionnaires to report their perceived workload and intra-operative performance.
All OR professionals were eligible, when present in the OR for at least 1 h and actively involved in the procedure, including surgeons (operating and assisting surgeons), OR nurses (scrub nurse and rotating nurse), and anesthetists.
Identification of types and severity of surgical flow disruptions
Flow disruptions were defined as unforeseen events that potentially distract or momentarily interrupt one or more OR team members from their task [5]. An established observational tool was applied for identification of 12 pre-defined types of flow disruptions [4, 5] (see Table 1). Additionally, each disruptions was rated for its severity of interference using an established scale that ranges from 1 to 9 [5, 6]: 1 to 3 refer to the rotating nurse: (1) a disruption, which is potentially distracting, (2) a disruptions, which is noticed, and (3) a disruption, which the rotating nurse attends to; 4 to 6 refer to individual OR team members: (4) one team member is momentarily distracted, (5) one team member pauses the current task, and (6) one team member attends to disruptive event; 7 to 9 refer to more than one OR team member or the whole team: (7) OR team is distracted as whole, (8) OR team attends to the distraction, and (9) the operation flow is disrupted.
Inter-rater agreement was established in a stepwise procedure: First, five unsystematic pilot observations were conducted on-site for observer training, achieving familiarity with the OR team and robotic setting. Secondly to obtain inter-rater reliability, five operations during the study were observed by a second expert observer (last author). During those observations, 210 and 205 flow disruptions were identified by the two observers, respectively (total observation time: 14 h 34 min). As distribution of observed events per minute suggested a prevalence problem, Gwet’s AC1 statistic as a variant of the kappa coefficient was used for agreement per minute whether or not a disruption occurred [28]. Gwet’s AC1 statistic was .83, which indicates very good agreement [29]. To test inter-rater reliability for correct classification of disruption types, a two-way, absolute agreement, single-measure intra-class correlation (ICC) of .80 was calculated. Furthermore, agreement on flow disruption severity was determined: the two-way, consistency, single-measure ICC was .78. Both ICCs demonstrate high inter-observer agreement [29].
Procedure and patient characteristics
Four operative phases were determined [4]. Phase 1 started when the patient entered the OR until abdominal insufflation via port placement was prepared. Phase 2 commenced with abdominal insufflation, including robot-docking, until the surgeon sat down at the robotic console. Phase 3 covered the main surgical intervention time when the surgeon operated at the console. Phase 4 included the postoperative activities after the surgeon left the console, including robot-undocking, until the patient left the OR.
Additional information about patient and procedural characteristics were collected through department’s internal documentation and patient chart information. It included patient’s age, BMI and ASA score, experience of operating surgeon, training case, daytime, duration of the procedure, and number of OR team members.
OR professionals’ workload and performance ratings
At the end of the observed procedure, each OR team member was asked to fill in a survey. This comprised three items of the validated Surgery Task Load Index (SURG-TLX), namely mental demands (“How mentally fatiguing was the procedure?”), situational stress (“How anxious did you feel while performing the procedure?”), and distractions (“How distracting was the operating environment?”) [16]. Two further questions were included to assess intra-operative performance, namely productivity (“How productive have you been in your work during the operation?”) and perceived quality (“How do you evaluate the quality of your work during the operation?”) [30]. As internal consistency between both items was good (Cronbach’s α = .85), performance scores collated both ratings. All items were answered through a visual analogue scale ranging from 0 = very low to 10 = very high. Additionally, all OR members reported their profession (surgical nurse, surgeon, anesthesia) and professional tenure (<5 years, 5–10 year, >15 year).
Analyses
Rates were calculated as flow disruptions per hour to control for procedure and phase duration. When multiple members of an OR profession filled out a survey, ratings were aggregated per profession. Analyses of variance with repeated measures (ANOVA) were calculated for differences in disruption rate between phases and for differences in workload and performance ratings between OR professions. When the assumption of sphericity was violated, the p value of Greenhouse–Geisser was reported. For differences in severity between the 4 phases, an unpaired ANOVA was applied. Correlation analyses were used to determine associations between rate and severity of disruptions and OR professionals’ reports, i.e., intra-operative workload and performance. Finally, these associations were adjusted for patient and procedural characteristics (e.g., training case, patients’ BMI, size of OR team) with Pearson partial correlation analyses. Those analyses revealed similar results patterns and were therefore not further included to the results section. In addition, we also controlled for multiple testing using Bonferroni correction. For all analyses, R 3.3.1 was used.
Results
Forty robot-assisted procedures (radical prostatectomies) were observed with a total observation time of 146 h 55 min (Mean procedure time: 3 h 40 min, SD = 31 min; Range 2 h 40 min, 5 h 04 min). Of the observed procedures, eight were training cases. In seven cases, the main surgeon had low (<250 robotic cases), in 14 medium, and in 19 high (>700) experience. Patients’ medium age was 66 years and mean BMI = 27.4 kg/m2. Distribution of patients’ ASA score was: 1 = 3 patients, 2 = 22, 3 = 15.
Observed rates and severity of surgical flow disruptions
In total, 2285 flow disruptions were identified with an overall mean rate of 15.80 events per hour (SD = 2.18). Overall rates and especially disruption rates due to coordination issues were significantly the highest during robot-docking (cf. Table 2). Rates of disruption types varied, being the highest for people entering the OR, case-irrelevant communication, and procedural issues. The rates of observed disruptions are depicted in Fig. 1 (and reported per phase in Supplementary Material, Table A-1).
Concerning severity of disruptions, significant differences were found between all phases (F[df = 3,23] = 19.48, p < .001), with the highest interference during robot-docking (cf., Table 2). Disruptions due to instrument changes or equipment problems were rated with the highest severity. Disruptions due to people entering the OR as well due to telephone calls were least severe.
OR professionals’ intra-operative workload and performance
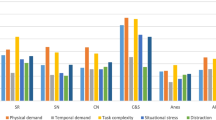
Overall, 216 staff reports were collected after the procedures (93 of nurses, 81 of surgeons, and 42 of anesthetists). The response rate was 90% of all eligible OR team members. Figure 2 reports perceived intra-operative workload and performance: anesthetists reported higher mental demands compared to surgeons (t[df = 36] = 4.27, p < .001) and nurses (t[df = 36] = 2.69, p = .011). Anesthetists also reported higher intra-operative distractions than surgeons (t[df = 36] = 4.25, p < .001). Mean performance ratings differed between professions (F[df = 2,72] = 51.30, p < .001) with higher values for surgeons (t[df = 36] = 9.66, p < .001) and nurses (t[df = 36] = 4.77, p < .001) compared to anesthetists.
Associations of flow disruptions and intra-operative workload and performance
Our main objective was to explore associations between flow disruptions and OR professionals’ experiences of intra-operative workload and performance. The mere count of flow disruption during the observed procedures was associated with increased intra-operative distractions perceived by anesthetists’ (r = .33, p = .046) and nurses (r = .38, p = .017). Higher disruption rates were also correlated with nurses’ intra-operative stress (r = .34, p = .036). Prospective associations of disruption rates with staff reports can be found in Supplementary material (see Table A-2). We further observed that higher severities were associated with increased distractions ratings by the whole OR team (r = .34, p = .030, cf., Table 3). For individual disruption types, high severity of case-relevant communication, case-irrelevant communication, and coordination were related to increased team distractions (cf., Table 3). Moreover, higher severity of case-irrelevant communication was linked to higher stress reports of anesthetists. Increased severity of surgeons’ decision making was correlated with inferior performance of anesthetists’ and nurses’ mental demands. Severe disruptions due to equipment issues were negatively correlated with anesthetists’ but positively correlated with nurses’ mental demands (cf., Table 3). Lastly, after adjusting for multiple testing, none of the above reported associations remained significant.
Discussion
We explored associations of surgical flow disruptions and intra-operative workload and performance during robotic-assisted surgery, suggesting that improved communication and team coordination could reduce workload and increase intra-operative performance.
Around 16 flow disruptions occurred per hour with variation across procedure phases. Our results show that particularly the docking phase is critical. Frequent disruptions due to coordination corroborate intense interaction and communication demands while moving the patient into a steep Trendelenburg position, rearranging the robot, and configuring monitors for assisting surgeon and scrub nurse [4, 31]. During console time, flow disruptions due to equipment issues indicate the extended use of complex technology [32]. Frequently, the camera had to be cleaned or a clip applicator was not working properly. Overall, most disruptions occurred due to people entering/exiting the OR [5, 6, 8].
Lower levels of workload and high-performance ratings of surgeons reflect the advantages in ergonomics, precision, and 3D-visualization due to the robotic system [22, 33]. In contrast, anesthetists reported higher workload and inferior performance. Younger age and less experience of anesthetists in this study could have been one reason. Secondly, robot-assisted radical prostatectomies pose additional strains for anesthetists including CO2-insufflation of the peritoneum, patients’ steep Trendelenburg position with increased risks of complications [34], and limited intra-operative access to patient’s head and lines [34,35,36].
Concerning our main objective, we observed that perceived distractions increased with higher overall disruption rate. This corroborates the validity of our observational approach. Furthermore, perceived distraction increased with more severe disruptions due to case-relevant communication, case-irrelevant communication, and coordination. Severe disruptions due to coordination often involved incorrect patient position, equipment being in the way, and difficulties in arranging the catheter during urethro-vesical anastomosis [31]. Severe case-relevant communication often comprised discussions about relaxation of the patient or pressure of gas insufflation, but also involved miscommunication, acoustic problems, or missing reactions to console surgeon’s instructions [2, 4]. It is difficult for team members to anticipate surgeon’s instructions due to spatial separation and due to impossibilities of non-verbal communication [2, 3, 32, 37]. In consequence, OR team members invest more effort into communication, which might deplete attention or awareness. Our results revealed that severe case-irrelevant communication increases anesthetists’ stress. Previous research suggested that case-irrelevant communication may serve as a strategy to reduce stress and that is more likely to occur during non-stressful cases [6, 8]. Our findings suggest that this is not true for all team roles [38, 39].
We found no significant association between flow disruptions and surgeons’ mental demands, situational stress or performance, suggesting that robotic systems create protective effects against disruptive events [22, 24]. It is conceivable that being immersed in the console reduces awareness of disruptions and consequently distractions, which is in line with low distraction ratings of surgeons in this study. Furthermore, performing on the robotic system has been shown to reduce surgeon’s mental and physical workload so that surgeons may have more cognitive resources left to cope with flow disruptions [22, 24].
Limitations
Like other observational studies, we cannot rule out observer bias [5, 6, 8]. Limited external validity should be considered since results are based on one department with high volume of robotic cases in Germany. Although we controlled for experience, it is reasonable to assume that flow disruptions occur more often, when OR teams have less robot experience. Our design of our study forbids inferences on causality between disruptions and individual outcomes [40]. Although interference and severity of disruption events was measured, it was not possible to capture potential positive effects, e.g., transmission of urgent information [41]. Our self-report approach among OR staff comprises risks of recall bias and omission of rapid workload changes during the surgery [6, 8]. Future studies on this topic should further delve into the impact of OR team roles [21], OR team familiarity [3], gender, and members’ strategies to deal with stress [42, 43]. In our study department, it is standard practice that the head surgeon is present during positioning and docking (phase 2). Nonetheless, within other institutions where junior residents perform docking and positioning, different disruptions frequencies may occur during this phase. We recommend future studies to further elucidate disruptions prior to docking, since we examined flow disruption frequencies before and after incision.
Implications
Our results show that system-based analyses and improvements are necessary that carefully take account of the complex inter-dependencies of surgical tasks and technology, OR environment, and the social system [4, 32]. In order to mitigate adverse consequences of disruptions, balanced and nuanced measures are advised to identify especially those flow disruptions that severely affect operation flow as well as OR professionals’ workload and performance (e.g., communication and coordination). Since flow disruptions often signify deeper system problems, OR management’s efforts to safeguard patient safety include development of an enhanced understanding of system-related issues responsible for safe surgery. Key drivers analyses facilitate an understanding of how high severity disruptions may curb surgical performance as well as how multiple, avoidable minor events may accumulate. Effective team training interventions and strategies to compensate for impossibilities of non-verbal communication could master demands on teamwork and communication [37]. Particularly during robot-docking, efforts for shared situation awareness, clear communication, and adaptive coordination problems are recommended [2, 31, 44]. Future interventions should especially target the docking and positioning of the robot and examine whether additional resources brought into the OR or a surgical pause facilitate smoothness of collaboration. Lastly, future studies shall include meaningful clinical outcomes and examine correlations of if or how disruptions during robotic procedures are deleterious for patients, e.g., for blood loss or intra-/postoperative complications.
Conclusions
Our results highlight the need for strategies improving shared situation awareness, communication and team coordination during robotic-assisted surgeries. Especially during critical steps involving increased interactions between OR team members and the robotic system, such as robot-docking, this is essential to mitigate flow disruptions and to establish a smooth and effective operation flow. Consequently this could reduce workload and improve performance of OR professionals.
References
H-y Yu, Hevelone ND, Lipsitz SR et al (2012) Use, costs and comparative effectiveness of robotic assisted, laparoscopic and open urological surgery. J Urol 187:1392–1399
Randell R, Honey S, Alvarado N et al (2016) Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work 18:423–437
Sexton K, Johnson A, Gotsch A et al (2018) Anticipation, teamwork and cognitive load: chasing efficiency during robot-assisted surgery. BMJ Qual Saf 27:148–154
Catchpole K, Perkins C, Bresee C et al (2016) Safety, efficiency and learning curves in robotic surgery: a human factors analysis. Surg Endosc 30:3749–3761
Antoniadis S, Passauer-Baierl S, Baschnegger H et al (2014) Identification and interference of intraoperative distractions and interruptions in operating rooms. J Surg Res 188:21–29
Weigl M, Schneider A, Hoffmann F et al (2015) Work stress, burnout, and perceived quality of care: a cross-sectional study among hospital pediatricians. Eur J Pediatr 174:1237–1246
Mentis HM, Chellali A, Manser K et al (2016) A systematic review of the effect of distraction on surgeon performance: directions for operating room policy and surgical training. Surg Endosc 30:1713–1724
Wheelock A, Suliman A, Wharton R et al (2015) the impact of operating room distractions on stress, workload, and teamwork. Ann Surg 261:1079–1084
Persoon MC, Broos HJ, Witjes JA et al (2011) The effect of distractions in the operating room during endourological procedures. Surg Endosc 25:437–443
Parker SH, Laviana A, Wadhera R et al (2010) Development and evaluation of an observational tool for assessing surgical flow disruptions and their impact on surgical performance. World J Surg 34:353–361. https://doi.org/10.1007/s00268-009-0312-z
Jain M, Fry BT, Hess LW et al (2016) Barriers to efficiency in robotic surgery: the resident effect. J Surg Res 205:296–304
Allers JC, Hussein AA, Ahmad N et al (2016) Evaluation and impact of workflow interruptions during robot-assisted surgery. Urology 92:33–37
Catchpole K, Bisantz A, Hallbeck MS et al (2018) Human factors in robotic assisted surgery: lessons from studies ‘in the Wild’. Appl Ergon. https://doi.org/10.1016/j.apergo.2018.02.011
Arora S, Sevdalis N, Nestel D et al (2010) The impact of stress on surgical performance: a systematic review of the literature. Surgery 147:318–330
Blikkendaal MD, Driessen SR, Rodrigues SP et al (2016) Surgical flow disturbances in dedicated minimally invasive surgery suites: an observational study to assess its supposed superiority over conventional suites. Surg Endosc 31:228–298
Wilson MR, Poolton JM, Malhotra N et al (2011) Development and validation of a surgical workload measure: the surgery task load index (SURG-TLX). World J Surg 35:1961–1969. https://doi.org/10.1007/s00268-011-1141-4
Weigl M, Antoniadis S, Chiapponi C et al (2015) The impact of intra-operative interruptions on surgeons’ perceived workload: an observational study in elective general and orthopedic surgery. Surg Endosc 29:145–153
Weigl M, Stefan P, Abhari K et al (2016) Intra-operative disruptions, surgeon’s mental workload, and technical performance in a full-scale simulated procedure. Surg Endosc 30:559–566
Hart SG, Staveland LE (1988) Development of NASA-TLX (task load index): results of empirical and theoretical research. Adv Psychol 52:139–183
Wetzel CM, Kneebone RL, Woloshynowych M et al (2006) The effects of stress on surgical performance. Am J Surg 191:5–10
Yu D, Dural C, Morrow MM et al (2017) Intraoperative workload in robotic surgery assessed by wearable motion tracking sensors and questionnaires. Surg Endosc 31:877–886
Moore LJ, Wilson MR, McGrath JS et al (2015) Surgeons’ display reduced mental effort and workload while performing robotically assisted surgical tasks, when compared to conventional laparoscopy. Surg Endosc 29:2553–2560
Heemskerk J, Zandbergen HR, Keet SW et al (2014) Relax, it’s just laparoscopy! a prospective randomized trial on heart rate variability of the surgeon in robot-assisted versus conventional laparoscopic cholecystectomy. Dig Surg 31:225–232
Moore LJ, Wilson MR, Waine E et al (2015) Robotically assisted laparoscopy benefits surgical performance under stress. J Robot Surg 9:277–284
Suh IH, Chien JH, Mukherjee M et al (2010) The negative effect of distraction on performance of robot-assisted surgical skills in medical students and residents. Int J Med Robot + Comput Assist Surg: MRCAS 6:377–381
Suh IH, LaGrange CA, Oleynikov D et al (2016) Evaluating robotic surgical skills performance under distractive environment using objective and subjective measures. Surg Innov 23:78–89
Weigl M, Weber J, Hallett E et al (2018) Associations of intraoperative flow disruptions and operating room teamwork during robotic assisted radical prostatectomy. Urology 114:105–113
Gwet K (2002) Kappa statistic is not satisfactory for assessing the extent of agreement between raters. Stat Methods Inter-rater Reliab Assess 1:1–6
Hallgren KA (2012) Computing inter-rater reliability for observational data: an overview and tutorial. Tutor Quant Methods Psychol 8:23–34
Grawitch MJ, Granda SE, Barber LK (2008) Do prospective workday appraisals influence end-of-workday affect and self-monitored performance? J Occup Health Psychol 13:331–344
Dru CJ, Anger JT, Souders CP et al (2017) Surgical flow disruptions during robotic-assisted radical prostatectomy. Can J Urol 24:8814–8821
Catchpole KR, Hallett E, Curtis S et al (2018) Diagnosing barriers to safety and efficiency in robotic surgery. Ergonomics 61:26–39
Lee GI, Lee MR, Clanton T et al (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28:456–465
Lee JR (2014) Anesthetic considerations for robotic surgery. Korean J Anesthesiol 66:3–11
Kakar P, Das J, Roy P et al (2011) Robotic invasion of operation theatre and associated anaesthetic issues: a review. Indian J Anaesth 55:18–25
Irvine M, Patil V (2009) Anaesthesia for robot-assisted laparoscopic surgery. Contin Educ Anaesth Crit Care Pain 9:125–129
Tiferes J, Hussein AA, Bisantz A et al (2018) Are gestures worth a thousand words?. Verbal and nonverbal communication during robot-assisted surgery, Appl Ergon
Widmer LW, Keller S, Tschan F et al (2018) More than talking about the weekend: content of case-irrelevant communication within the OR team. World J Surg. https://doi.org/10.1007/s00268-017-4442-4
Cavuoto LA, Hussein AA, Vasan V et al (2017) Improving teamwork: evaluating workload of surgical team during robot-assisted surgery. Urology 107:120–125
Weigl M, Muller A, Vincent C et al (2012) The association of workflow interruptions and hospital doctors’ workload: a prospective observational study. BMJ Qual Saf 21:399–407
Sevdalis N, Healey AN, Vincent CA (2007) Distracting communications in the operating theatre. J Eval Clin Pract 13:390–394
Gillespie BM, Chaboyer W, Fairweather N (2012) Interruptions and miscommunications in surgery: an observational study. AORN J 95:576–590
Hassan I, Weyers P, Maschuw K et al (2006) Negative stress-coping strategies among novices in surgery correlate with poor virtual laparoscopic performance. Br J Surg 93:1554–1559
Gillespie BM, Chaboyer W, Murray P (2010) Enhancing communication in surgery through team training interventions: a systematic literature review. AORN J 92:642–657
Acknowledgements
We thank all surgeons, nurses and anesthetists for their participation.
Funding
The study was supported by the Munich Centre for Health Sciences (MC-Health) and the Bavarian Research Alliance (BAYFOR).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Weber, J., Catchpole, K., Becker, A.J. et al. Effects of Flow Disruptions on Mental Workload and Surgical Performance in Robotic-Assisted Surgery. World J Surg 42, 3599–3607 (2018). https://doi.org/10.1007/s00268-018-4689-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4689-4