Abstract
While the benefits of robotic surgery for the patient have been relatively well established, little is known about the benefits for the surgeon. This study examined whether the advantages of robotically assisted laparoscopy (improved dexterity, a 3-dimensional view, reduction in tremors, etc.) enable the surgeon to better deal with stressful tasks. Subjective and objective (i.e. cardiovascular) responses to stress were assessed while surgeons performed on either a robotic or conventional laparoscopic system. Thirty-two surgeons were assigned to perform a surgical task on either a robotic system or a laparoscopic system, under three stress conditions. The surgeons completed self-report measures of stress before each condition. Furthermore, the surgeons’ cardiovascular responses to stress were recorded prior to each condition. Finally, task performance was recorded throughout each condition. While both groups reported experiencing similar levels of stress, compared to the laparoscopic group, the robotic group displayed a more adaptive cardiovascular response to the stress conditions, reflecting a challenge state (i.e. higher blood flow and lower vascular resistance). Furthermore, despite no differences in completion time, the robotic group performed the tasks more accurately than the laparoscopic group across the stress conditions. These results highlight the benefits of using robotic technology during stressful situations. Specifically, the results show that stressful tasks can be performed more accurately with a robotic platform, and that surgeons’ cardiovascular responses to stress are more favourable. Importantly, the ‘challenge’ cardiovascular response to stress displayed when using the robotic system has been associated with more positive long-term health outcomes in domains where stress is commonly experienced (e.g. lower cardiovascular disease risk).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite some equivocal findings [1], clinical studies have generally demonstrated that robotic surgery can benefit patients in terms of reduced blood loss, post-operative pain, and length of stay in hospital compared to conventional laparoscopy [2]. Despite this research, little is known about whether robotic technology benefits the surgeon. Indeed, traditional laparoscopy causes unique challenges for the surgeon, with reduced dexterity of elongated tools, limited freedom of movement within the abdomen, and a two-dimensional field of view generating high physical and mental demands [3, 4]. These limitations mean that dealing with operative stress in laparoscopic procedures can be difficult. By addressing these limitations and reducing the demands placed upon the surgeon, robotic technology may help surgeons cope better with stress. However, despite research showing that robotic techniques are associated with better training task performance as well as less mental and physical workload [5, 6], limited research has examined if robotic techniques are more beneficial during stressful surgical tasks than laparoscopic techniques.
The impact of stress on surgical performance has received increasing research interest [7], with findings demonstrating that stressors such as time pressure and multi-tasking can cause laparoscopic tasks to be performed slower and with more errors [8, 9]. Despite recent research implying that surgeons experience less self-reported stress during tasks performed on a robotic rather than laparoscopic platform [10–12], there is a lack of research using objective markers of stress. This is surprising given that objective measures such as cardiovascular responses allow stress to be recorded online continuously and covertly, making them impervious to the biases associated with self-report measures (e.g. social desirability bias). One theory that outlines two specific cardiovascular responses to stress that can influence task performance is the biopsychosocial model (BPSM) of challenge and threat developed by Blascovich and colleagues [13, 14].
According to the BPSM, a surgeon can respond to a stressful surgical task via a challenge state or a threat state [13, 15]. These states are characterized by different cardiovascular responses and can be assessed objectively. Specifically, while both states are associated with increases in heart rate, reflecting active engagement with the stressful task, a challenge state is accompanied by greater blood flow (i.e. higher cardiac output) and less resistance in the vasculature (i.e. lower total peripheral resistance) [13, 15]. This ‘challenge’ cardiovascular response is considered a more adaptive reaction to stress than the ‘threat’ response, as blood flow, and thus energy (glucose and free fatty acids) delivery to the brain and muscles, is greater (higher cardiac output) and less restricted (lower total peripheral resistance) [13, 15]. Importantly, recent research has demonstrated that a challenge state also results in better surgical performance than a threat state [16, 17]. Moreover, it has been suggested that when frequently experienced, a threat state can lead to deleterious health outcomes, including depression, cardiovascular disease, and cellular aging [18, 19].
This study aimed to examine surgeons’ cardiovascular responses to, and performance during, a surgical task performed either on a robotic system or a laparoscopic system, under three stressful conditions (time pressure, multi-tasking, and evaluative pressure). The suggested benefits of the robotic system (i.e. 3-dimensional field of view, improved dexterity, reduction in tremors, etc.) were predicted to result in surgeons assigned to the robotic system reporting less stress before all conditions. Furthermore, due to the purported benefits of the robotic system, the surgeons assigned to the robotic system were also hypothesized to display a ‘challenge’ cardiovascular response (i.e. higher blood flow and lower vascular resistance) before all stress conditions compared to surgeons allotted to the laparoscopic system. Finally, surgeons assigned to the robotic system were predicted to perform better (i.e. fewer errors and faster completion times) in all stress conditions compared to surgeons allocated to the laparoscopic system.
Methods
Participants
Thirty-two, right-hand dominant, qualified, and trainee surgeons (24 qualified surgeons and 8 trainee surgeons; 27 male, 5 female; mean age = 39.91 years, SD = 8.96) participated in the study. On average, the surgeons had greater laparoscopic experience than robotic experience (mean number of procedures = 384.03, SD = 906.11 vs. 7.56, SD = 28.83). This information was gathered via a brief demographic questionnaire. All surgeons declared that they did not smoke, were free of illness or infection, had normal or corrected vision, had no known family history of cardiovascular or respiratory disease, had not performed vigorous exercise or ingested alcohol for 24 h prior to testing, and had not consumed food and/or caffeine for 1 h prior to testing. The study was approved by the institutional ethics committee and written informed consent was obtained from all surgeons before each individual testing session.
Surgical systems and task
A da Vinci Si robotic system (Intuitive Surgical Ltd., Sunnyvale, California) consisting of a control and viewing console and a moveable cart with three articulated robot arms was used in this study. The surgeon sat at the console and viewed a three-dimensional image of the scene while moving a handle that controlled a robotic arm fitted with a single laparoscopic instrument. A second arm was fitted with an endoscope, which the surgeons did not need to manipulate, because the task was always in full view. A 3-Dmed (3-Dmed, Franklin, OH) standard minimally invasive training system with a joystick SimScope (a manoeuvrable webcam) was also employed. The surgeon stood in front of the system and viewed the scene inside the system on a monitor (via a webcam) while manipulating a single laparoscopic instrument that was inserted through a single port. The task was also in full view on this system to ensure that surgeons did not need to manipulate the joystick at any stage.
A ball pick-and-drop task was completed on either the robotic system or the laparoscopic system. The task required the surgeons to move six foam balls from stems of varying heights into a cup, using a single instrument. The surgeons used their dominant hand to grasp the balls and drop them into the cup individually and in a pre-specified order. The surgeons were asked to complete the task as accurately (i.e. no dropped balls) and as fast as they could. Previous research has shown that this task can be used to improve laparoscopic skills [16, 17]. The experimental setup and task are displayed in Fig. 1.
Procedure
After arriving at the laboratory, the surgeons read an information sheet and provided written informed consent before completing a brief demographic questionnaire regarding their age, job title, and prior laparoscopic and robotic experience. Following this, the surgeons were randomly assigned to one of the two surgical systems (robotic or laparoscopic group). Importantly, a between-subjects design was employed, as previous research has shown that cardiovascular responses can be attenuated by prior exposure to a stressful task [20]. Due to their participation in a prior experiment, all surgeons were familiar with performing the ball pick-and-drop task on each system. Next, the surgeons were fitted with an impedance cardiograph device (Physioflow, PF05L1, Manatec Biomedical, France). The surgeons then sat still and quietly while 3 min of baseline cardiovascular data was recorded. Subsequently, the surgeons received instructions regarding the time pressure condition and a further minute of cardiovascular data was recorded while they sat quietly and reflected upon these instructions and the upcoming task. The surgeons then completed the self-report questionnaire before performing one trial on the ball pick-and-drop task under time pressure conditions. This process was then repeated for both the multi-tasking and evaluative pressure conditions. Performance data were recorded continuously during each condition. Finally, the surgeons were debriefed and thanked while the impedance cardiograph device was removed.
Stress conditions
The three stress conditions included experimental manipulations adapted from previous research [8, 21, 22]. In the time pressure condition, the surgeons were instructed to complete the task in a faster time than they had managed in a previous experiment (as when a patient might suffer from complications). In the multi-tasking condition, the surgeons were informed to complete a concurrent secondary tone-counting task while performing the surgical task (to assess the degree to which surgeons can apply cognitive resources to other tasks). The tone-counting task required the surgeons to listen for a target sound (bell ring) and count the number of times it was played while ignoring three other distracting sounds (buzzer, ping, and tone). Participants were played a 30-s example of the sounds for familiarization purposes. Finally, in the evaluative pressure condition, the surgeons were informed that their performance on the next trial would be videotaped and compared against the surgeons who had already participated (via a published leader board). The surgeons were told that based on their performance to date, they would be placed in the bottom 30 % compared to these surgeons (non-contingent feedback).
Measures
Stress
Stress was assessed via the short version of the State–Trait Anxiety Inventory (STAI) [23]. The STAI consists of six items (e.g. I feel tense, I feel calm) that are rated on a four-point Likert scale anchored between not at all (=1) and very much (=4). A score was calculated by reversing the ratings for the positively framed items and then summing the ratings from all six items so that a higher score reflected greater stress (range 6–24). This measure has been used in previous research examining stress in surgery [8].
Cardiovascular response
Cardiovascular data were recorded using an impedance cardiograph device (Physioflow, PF05L1, Manatec Biomedical, France) [24]. The Physioflow measures impedance changes in response to a high-frequency (75 kHz) and low-amperage (3.8 mA) electrical current emitted via electrodes. Following preparation of the skin, six spot electrodes (Blue Sensor R, Ambu, Ballerup, Denmark) were positioned on the thorax: two on the supraclavicular fossa of the left lateral aspect of the neck, two near the xiphisternum at the midpoint of the thoracic region of the spine, one on the middle of the sternum, and one on the rib closest to V6. After entering the surgeons’ details (height, weight, etc.), the Physioflow was calibrated over 30 heart cycles while the surgeons sat still and quiet in an upright position. Three resting systolic and diastolic blood pressure values were taken (one prior to the 30 heart cycles, one during this time period, and another immediately after this time period) manually by a trained experimenter using an aneroid sphygmomanometer (ACCOSON, London, UK) and stethoscope (Master Classic II, Littmann, 3 M Health Care, St. Paul, USA). The mean blood pressure values were entered into the Physioflow to complete the calibration procedure.
The surgeons’ cardiovascular responses were estimated continuously during baseline (3 min) and post-instruction (1 min) time periods for each stress condition while the surgeons remained seated, still, and quiet. Heart rate, the number of times the heart beats per minute, was estimated directly by the Physioflow. Heart rate reactivity (the difference between the final minute of baseline and the minute post-instruction) was used to assess task engagement; with greater increases in heart rate reflecting greater task engagement, a pre-requisite for challenge and threat states [15]. Cardiac output, the amount of blood in litres pumped by the heart per minute, was estimated directly by the Physioflow. Furthermore, total peripheral resistance, a measure of net constriction versus dilation in the arterial system, was calculated using the formula: (mean arterial pressure × 80/cardiac output) [25]. Mean arterial pressure was calculated using the formula: [(2 × diastolic blood pressure) + systolic blood pressure/3] [26]. Cardiac output and total peripheral resistance were used to differentiate challenge and threat states, with a challenge state characterized by higher cardiac output and lower total peripheral resistance [15].
Surgical task and tone-counting performance
Performance on the ball pick-and-drop task was assessed in terms of the number of errors made during each trial (number of balls dropped and/or knocked off) and time taken to complete each trial [27]. Additionally, tone-counting performance in the multi-tasking condition was assessed by calculating an error score (participants’ estimate of the number of target tones played during the task minus the actual number of target tones played) [22].
Statistical analyses
Dependent t tests were conducted on the heart rate reactivity data to establish that the surgeons displayed increases in heart rate from baseline and were thus actively engaged in the stress conditions (reactivity greater than zero) [28]. To differentiate challenge and threat states, an index was created by converting each surgeons’ cardiac output and total peripheral resistance residualized change scores into z-scores and summing them. Cardiac output was assigned a weight of +1 and total peripheral resistance a weight of −1, such that a larger value corresponded with greater challenge [28]. To compare the groups across the three stress conditions, two (group: robotic vs. laparoscopic) × 3 (condition: time pressure, multi-tasking, evaluative pressure) mixed design ANOVAs with follow-up least significant difference (LSD) post hoc t tests were conducted on the challenge and threat index data.
These ANOVAs were also conducted on the STAI, number of errors, and completion time data. In addition, the tone-counting error data were subject to an independent t test. Finally, to establish that any between-group differences were not due to differences in the age or the number of laparoscopic and robotic procedures performed by the surgeons previously, independent t tests were conducted on this data. Partial eta-squared (η 2p ) and Cohen’s d were used to calculate effect sizes.
Results
Demographics
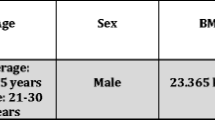
The results indicated no differences between the robotic and laparoscopic groups in terms of age (mean = 39.56 years, SD = 8.68 vs. mean = 40.25 years, SD = 9.50; t(30) = −0.21, p = 0.832, d = 0.08), number of laparoscopic procedures (mean = 485.25, SD = 1235.58 vs. mean = 282.81, SD = 385.08; t(30) = 0.63, p = 0.536, d = 0.23), or number of robotic procedures (mean = 5.63, SD = 17.50 vs. mean = 9.50, SD = 37.47; t(30) = −0.38, p = 0.710, d = 0.14). Thus, the randomization process was effective and any subsequent between-group differences can be attributed to the different surgical systems.
Stress
The ANOVA on the STAI data revealed no main effects for Group (F(1, 30) = 1.58, p = 0.218, η 2p = 0.05) or Condition (F(2, 60) = 2.70, p = 0.075, η 2p = 0.08) and no interaction effect (F(2, 60) = 1.15, p = 0.323, η 2p = 0.04). Thus, both groups experienced similar levels of stress across the three conditions. The stress data are presented in Table 1.
Cardiovascular response
The results revealed that on average, all surgeons displayed an increase in heart rate before the time pressure (mean = 1.91 bpm, SD = 4.13; t(31) = −2.61, p = 0.014, d = 0.94), multi-tasking (mean = 2.73 bpm, SD = 4.57; t(31) = −3.39, p = 0.002, d = 1.22), and evaluative pressure (mean = 3.54 bpm, SD = 4.20; t(31) = −4.76, p < 0.001, d = 1.71) conditions. Thus, the surgeons were actively engaged in all stress conditions, allowing further examination of challenge and threat states.
The ANOVA on the challenge and threat index data yielded a main effect for Group (F(1, 30) = 8.75, p = 0.006, η 2p = 0.23), but no main effect for Condition (F(2, 60) = 0, p = 1, η 2p = 0.00), and no interaction effect (F(2, 60) = 0.11, p = 0.894, η 2p = 0.00). Follow-up analyses revealed that the robotic group exhibited a higher index value (reflecting a ‘challenge’ cardiovascular response) than the laparoscopic group across the stress conditions (p = 0.006). The challenge and threat index data are presented in Table 1.
Surgical task and tone-counting performance
The ANOVA on the number of errors data revealed main effects for Group (F(1, 30) = 5.50, p = 0.026, η 2p = 0.16) and Condition (F(2, 60) = 3.36, p = 0.041, η 2p = 0.10), but no interaction effect (F(2, 60) = 0.35, p = 0.705, η 2p = 0.01). Follow-up analyses indicated that the robotic group made fewer errors across the conditions than the laparoscopic group (p = 0.026). Moreover, these analyses indicated that both groups made more errors in the evaluative pressure condition compared to the time pressure condition (p = 0.023). There were no differences between the other conditions (all ps > 0.129). The number of errors data is presented in Table 1.
The ANOVA on the completion time data revealed no main effect for Group (F(1, 30) = 1.30, p = 0.263, η 2p = 0.04) and no interaction effect (F(2, 60) = 1.61, p = 0.208, η 2p = 0.05). However, there was a main effect for Condition (F(2, 60) = 6.80, p = 0.002, η 2p = 0.19). Follow-up analyses indicated that both groups performed the task more quickly during the evaluative pressure condition than the time pressure (p = 0.001) and multi-tasking (p = 0.016) conditions. The completion time data are presented in Table 1.
In addition to performing the task more accurately in the multi-tasking condition, an independent t test indicated that the robotic group made fewer errors than the laparoscopic group during the secondary tone-counting task (mean = 0.19, SD = 0.75 vs. mean = 0.50, SD = 0.52). However, although this difference equated to a medium effect size, it was not statistically significant (t(30) = 1.37, p = 0.180, d = 0.50).
Discussion
Despite clinical studies generally highlighting the benefits of robotic versus laparoscopic surgery for the patient [2], little research has examined precisely how robotic technology benefits the surgeon. While the poor precision and ergonomics of laparoscopy may exacerbate stress, the improved vision and dexterity associated with robotic technology might help surgeons cope better with stress [3, 4]. Although robotic techniques have been associated with better training task performance and less workload than laparoscopic techniques [5, 6], limited research has examined if robotic techniques are more beneficial during stressful surgical tasks. Thus, the present study aimed to explore surgeons’ cardiovascular responses to, and performance during, a surgical task performed either on a robotic or laparoscopic platform under three stress conditions (time pressure, multi-tasking, and evaluative pressure).
The robotic and laparoscopic groups reported comparable levels of stress, in contrast to our hypothesis and previous research that has demonstrated that robotic technology is associated with less self-reported stress than laparoscopic technology [10–12]. For example, Klein and colleagues found that experienced surgeons who had performed an average of 533 laparoscopic and 225 robotic procedures reported less stress when performing a peg transfer task on a robotic rather than laparoscopic system [11]. However, it should be noted that the disparity in laparoscopic and robotic experience was far greater in the surgeons recruited in the present study (average of 384 laparoscopic and 8 robotic procedures), and this lack of familiarity with the robotic platform may have led the surgeons to report greater stress levels than those found in previous research. In addition, similar levels of stress were reported across the time pressure, multi-tasking, and evaluative pressure conditions. This is inconsistent with previous research that has suggested time pressure may be more stressful than evaluative pressure in laparoscopic surgery [8].
The surgeons’ cardiovascular responses did not vary across the stress conditions. However, while all surgeons displayed an increase in heart rate before each stress condition, indicating that they were actively engaged in the stressful conditions, the surgeons using the robotic system exhibited a more adaptive cardiovascular response. Specifically, in comparison to the laparoscopic group, the robotic group repeatedly displayed a cardiovascular response more reflective of a challenge state consisting of greater blood flow (i.e. higher cardiac output) and less vascular resistance (i.e. lower total peripheral resistance). Importantly, this ‘challenge’ cardiovascular response has been linked with better health outcomes when commonly experienced, compared to the ‘threat’ cardiovascular response (e.g. lower depression and hypertension risk) [18, 19]. Robotic technology may therefore also have benefits in terms of surgeons’ long-term mental and physical health, an important consideration given recent concerns regarding surgeons’ elevated suicide risk and reduced life expectancy [29, 30]. In addition, when compared to the ‘threat’ cardiovascular response, the ‘challenge’ cardiovascular response has been shown to predict superior motor performance in stressful environments [31].
As expected, the robotic group outperformed the laparoscopic group across the stress conditions, making fewer errors on the task. This may have been due to the proposed benefits of robotic technology (3-dimensional field of view, improved dexterity, etc.) and supports previous research that has identified that surgeons make fewer errors when performing training and stressful tasks on a robotic rather than laparoscopic system [5, 6, 11]. This finding is particularly interesting given the limited robotic experience of the participating surgeons. Indeed, previous research has shown that surgeons with vast laparoscopic experience and limited robotic experience often make more errors when utilizing robotic compared to laparoscopic systems [6]. Interestingly, despite no differences between the other conditions, all surgeons made more errors during the evaluative pressure condition than the time pressure condition. This suggests that evaluative pressure is a stressor that can influence both robotic and laparoscopic performance: a finding that contrasts previous research showing that multi-tasking has the largest influence on laparoscopic performance [8].
As well as making fewer errors on the surgical task during the multi-tasking condition, the robotic group also made fewer errors than the laparoscopic group during the secondary tone-counting task. Although this difference was not statistically significant, it did equate to a medium effect size. Consequently, it appears that the surgeons using the robotic system had more cognitive resources to apply to the secondary task than surgeons using the laparoscopic system. Spare resources might be a consequence of lower cognitive workload required to perform surgical tasks on the robotic platform than the laparoscopic platform [5, 6]. In the operating room, these extra cognitive resources could be used to more effectively deal with other demands, such as decision-making and communication, or to better cope with the many noises and distractions that are often encountered [32]. Such issues would be interesting to examine in future research.
Contrary to our hypothesis, the robotic and laparoscopic groups did not differ in terms of completion time across the stress conditions. This is inconsistent with previous research that has shown that surgeons complete various training tasks more quickly using a robotic rather than laparoscopic device [5, 6, 11]. However, it is worth noting that Lee and colleagues found that surgeons with considerably more laparoscopic than robotic experience performed tasks slower on a robotic compared to laparoscopic system [6]. Thus, our results are the first to show that surgeons can perform simple training tasks under stressful conditions in a similar time frame on both platforms despite having far greater laparoscopic experience. In addition, the surgeons performed the task faster in the evaluative pressure condition than the time pressure and multi-tasking conditions. This finding is likely caused by a learning effect as the order of the stress conditions was fixed and not counterbalanced (time pressure → multi-tasking → evaluative pressure), a potential limitation of the present study.
Another possible limitation of the present study was that a between-subjects design was employed rather than a within-subjects design (i.e. with surgeons’ performing the task on both systems under each stress condition). However, given that prior exposure to a stressful task has been shown to attenuate self-report and cardiovascular responses to stress [20], it was feared that a within-subjects design would reduce the effectiveness of the stress manipulations and the quality of the cardiovascular data, making it difficult to draw meaningful conclusions. It remains for future work to replicate the findings of the present study using different research designs (e.g. longitudinal). Finally, another potential limitation is the relatively simple task used. However, it is likely that the benefits found in the present study will be even greater during more complex tasks (e.g. intracorporeal suturing) and in the operating room. Indeed, this would be an interesting avenue for future research.
To conclude, the findings highlight the benefits of using robotic technology during stressful surgical tasks. Specifically, the results show that stressful tasks can be performed more accurately with a robotic platform than a laparoscopic platform. Furthermore, surgeons’ cardiovascular responses are more favourable when stressful tasks are completed using a robotic rather than laparoscopic system. Importantly, the ‘challenge’ cardiovascular response displayed by the surgeons when using the robotic system has been associated with more positive long-term health outcomes when frequently experienced (e.g. lower cardiovascular disease risk). Interestingly, these results emerged despite the surgeons in the present study having considerably less experience with robotic technology than laparoscopic technology.
References
Breitenstein S, Nocito A, Puhan M, Held U, Weber M, Clavien PA (2008) Robotic-assisted versus laparoscopic cholecystectomy: outcome and cost analyses of a case-matched control study. Ann Surg 247:987–993. doi:10.1097/SLA.0b013e318172501f
Payne TN, Dauterive FR (2008) A comparison of total laparoscopic hysterectomy to robotically assisted hysterectomy: surgical outcomes in a community practice. J Minim Invasive Gynecol 15:286–291. doi:10.1016/j.jmig.2008.01.008
Reinhardt-Rutland AH, Annett JM, Gifford M (1999) Depth perception and indirect viewing: reflections on minimally invasive surgery. Int J Cogn Ergon 3:77–90. doi:10.1207/s15327566ijce0302_1
Gallagher AG, McClure N, McGuigan J, Ritchie K, Sheehy NP (1998) An ergonomic analysis of the fulcrum effect in the acquisition of endoscopic skills. Endoscopy 30:617–620. doi:10.1055/s-2007-1001366
Hubens G, Coveliers H, Balliu L, Ruppert M, Vaneerdeweg W (2003) A performance study comparing manual and robotically assisted laparoscopic surgery using the da Vinci system. Surg Endosc 17:1595–1599. doi:10.1007/s00464-002-9248-1
Lee GI, Lee MR, Clanton T, Sutton E, Park AE, Marohn MR (2014) Comparative assessment of physical and cognitive ergonomics associated with robotic and traditional laparoscopic surgeries. Surg Endosc 28:456–465. doi:10.1007/s00464-013-3213-z
Arora S, Sevdalis N, Nestel D, Woloshynowych M, Darzi A, Kneebone R (2010) The impact of stress on surgical performance: a systematic review of the literature. Surgery 147:318–330. doi:10.1016/j.surg.2009.10.007
Poolton JM, Wilson MR, Malhotra N, Ngo K, Masters RSW (2011) A comparison of evaluation, time pressure and multi-tasking as stressors of psychomotor surgical performance. Surgery 149:776–782. doi:10.1016/j.surg.2010.12.005
Moorthy K, Munz Y, Dosis A, Bann S, Darzi A (2003) The effect of stress-inducing conditions on the performance of a laparoscopic task. Surg Endosc 17:1481–1484. doi:10.1007/s00464-002-9224-9
Klein MI, Warm JS, Riley MA, Matthews G, Doarn C, Donovan JF, Gaitonde K (2012) Mental workload and stress perceived by novice operators in the laparoscopic and robotic minimally invasive surgical interfaces. J Endourol 26:1089–1094. doi:10.1089/end.2011.0641
Klein MI, Mouraviev V, Craig C, Salamone L, Plerhoples TA, Wren SM, Gaitonde K (2014) Mental stress experienced by first-year residents and expert surgeons with robotic and laparoscopic surgery interfaces. J Robot Surg 8:149–155. doi:10.1007/s11701-013-0446-8
Van der Schatte Olivier RH, Van’t Hullenaar CDP, Ruurda JP, Broeders IAMJ (2009) Ergonomics, user comfort and performance in standard and robot-assisted laparoscopic surgery. Surg Endosc 23:1365–1371. doi:10.1007/s00464-008-0184-6
Blascovich J (2008) Challenge and threat. In: Elliot AJ (ed) Handbook of approach and avoidance motivation. Psychology Press, New York, pp 431–445
McGrath JS, Moore LJ, Wilson MR, Freeman P, Vine SJ (2011) Challenge and threat states in surgery: implications for surgical performance and training. Br J Urol Int 108:795–796. doi:10.1111/j.1464-410X.2011.10558.x
Seery MD (2011) Challenge or threat? Cardiovascular indexes of resilience and vulnerability to potential stress in humans. Neurosci Biobehav Rev 35:1603–1610. doi:10.1016/j.neubiorev.2011.03.003
Moore LJ, Vine SJ, Wilson MR, Freeman P (2014) Examining the antecedents of challenge and threat states: the influence of perceived required effort and support availability. Int J Psychophysiol 93:267–273. doi:10.1016/j.ijpsycho.2014.05.009
Vine SJ, Freeman P, Moore LJ, Chandra-Ramana R, Wilson MR (2013) Evaluating stress as a challenge is associated with superior attentional control and motor skill performance: testing the predictions of the biopsychosocial model of challenge and threat. J Exp Psychol Appl 19:185–194. doi:10.1037/a0034106
Blascovich J (2008) Challenge, threat, and health. In: Shah JY, Gardner WL (eds) Handbook of motivation science. Guildford, New York, pp 481–493
O’Donovan A, Tomiyama AJ, Lin J, Puterman E, Adler NE, Kemeny M, Wolkowitz OM, Blackburn EH, Epel ES (2012) Stress appraisals and cellular aging: a key role for anticipatory threat in the relationship between psychological stress and telomere length. Brain Behav Immun 26:573–579. doi:10.1016/j.bbi.2012.01.007
Kelsey RM, Blascovich J, Leitten CL, Schneider TR, Tomaka J, Wiens S (2000) Cardiovascular reactivity and adaptation to recurrent psychological stress: the moderating effects of evaluation observation. Psychophysiology 37:748–756. doi:10.1017/S004857720098209X
Vine SJ, Masters RSW, McGrath JS, Bright E, Wilson MR (2012) Cheating experience: guiding novices to adopt the gaze strategies of experts expedites technical laparoscopic skill learning. Surgery 152:32–40. doi:10.1016/j.surg.2012.02.002
Wilson MR, Vine SJ, Bright E, Masters RSW, Defriend D, McGrath JS (2011) Gaze training enhances laparoscopic technical skill acquisition and multi-tasking performance: a randomized controlled study. Surg Endosc 25:3731–3739. doi:10.1007/s00464-011-1802-2
Marteau TM, Bekker H (1992) The development of a six-item short-form of the state scale of the Spielberger State Trait Anxiety Inventory (STAI). Br J Clin Psychol 31:301–306
Charloux A, Lonsdorfer-Wolf E, Richard R, Lampert E, Oswald-Mammosser M, Mettauer B et al (2000) A new impedance cardiograph device for the non-invasive evaluation of cardiac output at rest and during exercise: comparison with the “direct” Fick method. Eur J Appl Physiol 82:313–320. doi:10.1007/s004210000226
Sherwood A, Allen M, Fahrenberg J, Kelsey R, Lovallo W, Van Doornen L (1990) Methodological guidelines for impedance cardiography. Psychophysiology 27:1–23. doi:10.1111/j.1469-8986.1990.tb02171.x
Cywinski J (1980) The essentials in pressure monitoring. Martinus Nijhoff Publishers, Boston
Vine SJ, Chaytor RJ, McGrath JS, Masters RSW, Wilson MR (2013) Gaze training improves the retention and transfer of laparoscopic technical skills in novices. Surg Endosc 27:3205–3213. doi:10.1007/s00464-013-2893-8
Moore LJ, Vine SJ, Wilson MR, Freeman P (2012) The effect of challenge and threat states on performance: an examination of potential mechanisms. Psychophysiology 49:1417–1425. doi:10.1111/j.1469-8986.2012.01449.x
Gold KJ, Sen A, Schwenck TL (2013) Details on suicide among US physicians: data from the National Violent Death Reporting System. Gen Hosp Psychiatr 35:45–49. doi:10.1016/j.genhosppsych.2012.08.005
Aasland OG, Hem E, Haldorsen T, Ekeberg O (2011) Morality among Norwegian doctors 1960–2000. BMC Public Health 11:173–180
Turner MJ, Jones MV, Sheffield D, Slater MJ, Barker JB, Bell JJ (2013) Who thrives under pressure? Predicting the performance of elite academy cricketers using the cardiovascular indicators of challenge and threat states. J Sport Exerc Psychol 35:387–397
Healey AN, Sevdalis N, Vincent CA (2006) Measuring intraoperative interference from distraction and interruption observed in the operating theatre. Ergonomics 49:589–604
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research was funded by Intuitive Surgical Ltd. through their, ‘Surgical Clinical Robotics Research Grant’ Program. However, Intuitive Surgical Ltd. had no involvement in the design and execution of the research, or in the analysis or interpretation of the data presented. Therefore, Dr Lee Moore, Ms Elizabeth Waine, Dr Mark Wilson, Mr John McGrath, Prof Rich Masters, and Dr Samuel Vine have no conflicts of interest or financial ties to disclose.
Informed consent statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients before being included in the study.
Rights and permissions
About this article
Cite this article
Moore, L.J., Wilson, M.R., Waine, E. et al. Robotically assisted laparoscopy benefits surgical performance under stress. J Robotic Surg 9, 277–284 (2015). https://doi.org/10.1007/s11701-015-0527-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-015-0527-y