Abstract
Background
Few studies in the literature have reported recovery data for different types of recurrent laryngeal nerve injuries (RLNIs). This study is the first attempt to classify RLNIs and rank them by severity.
Methods
This prospective clinical study analyzed 281 RLNIs in which a true loss of signal was identified by intraoperative neuromonitoring (IONM), and vocal cord palsy (VCP) was confirmed by a postoperative laryngoscope. For each injury type, the prevalence of VCP, the time of VCP recovery, and physical changes on nerves were analyzed. Additionally, different RLNI types were experimentally induced in a porcine model to compare morphological change.
Results
The overall VCP rate in at-risk patients/nerves was 8.9/4.6 %, respectively. The distribution of RLNI types, in order of frequency, was traction (71 %), thermal (17 %), compression (4.2 %), clamping (3.4 %), ligature entrapment (1.6 %), suction (1.4 %), and nerve transection (1.4 %). Complete recovery from VCP was documented in 91 % of RLNIs. Recovery time was significantly faster in the traction group compared to the other groups (p < 0.001). The rates of temporary and permanent VCP were 98.6 and 1.4 % for traction lesion, 72 and 28 % for thermal injury, 100 and 0 % for compression injury, 50 and 50 % for clamping injury, 100 and 0 % for ligature entrapment, 100 and 0 % for suction injury, and 0 and 100 % for nerve transection, respectively. Physical changes were noted in 14 % of RLNIs in which 56 % of VCP was permanent. However, among the remaining 86 % IONM-detectable RLNIs without physical changes, only 1.2 % of VCP was permanent. A porcine model of traction lesion showed only distorted outer nerve structure, whereas the thermal lesion showed severe damage in the inner endoneurium.
Conclusions
Different RNLIs induce different morphological alterations and have different recovery outcomes. Permanent VCP is rare in lesions that are visually undetectable but detectable by IONM. By enabling early detection of RLNI and prediction of outcome, IONM can help clinicians plan intra- and postoperative treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The recurrent laryngeal nerve (RLN) is a branch of the vagus nerve that supplies most of the intrinsic muscles of the larynx. Recurrent laryngeal nerve injury (RLNI) is a major cause of morbidity after thyroid and parathyroid surgery [1]. Unilateral RLNI and vocal cord palsy (VCP) can cause paralytic dysphonia and dysphagia whereas bilateral RLNIs and VCP can be life threatening because of the potential effects on the airway. Although the causes of RLNI are manifold, most result from incorrectly performed surgical techniques such as transection, ligature, compression, stretching/traction, and thermal stress [2–4]. In cases of unexplained (idiopathic) RLNI, the hypothesized mechanism is usually ischemia [5]. Intraoperative neuromonitoring (IONM) may be the only way to elucidate the mechanism of RLNI because, in most cases, the injured nerve is visibly intact and has an anatomically normal appearance [2–7]. According to IONM results reported in the literature, traction lesion is the most common type of RLNI (67–93 %) and most of the injury sites were visually undetectable [2–4].
Nerve injuries can be broadly grouped into three degrees. Neuropraxia is the least severe degree. It results in complete block of nerve transmission, despite intact nerve fibers. It usually recovers spontaneously over a few hours to few months. The second degree is axonotmesis, in which the nerve sheath remains intact but the axons are divided. The recovery usually takes several months to years. The third degree is neurotmesis, which is the most severe nerve injury because the axons and the sheath are partially or completely severed. Based on the electrophysiology results during IONM, RLNIs can be divided into two different subtypes [2, 4]. Type1 RLNI results from direct stress on the nerve and is characterized by a nerve injury at a specific site (i.e., localized or segmental RLNI). In type1 injury, distal stimulation of the nerve induces normal evoked activity. However, proximal to the injured segment, no stimulation greater than 100 µV could be elicited. In a type 2 injury, the exposed RLN shows no specific disruption site (i.e., global or diffuse RLNI) and reveals no visible change in appearance [2, 4, 5].
Few studies have compared recovery time in different types of RLNIs [2, 3, 8]. The causes and possible mechanisms of RLNIs during thyroidectomy must be understood and elucidated to improve the surgical pitfalls and further reduce the injury rate [2, 4]. A clear understanding of the expected outcomes of RLNI is also important not only for prognosis, but also for making correct intraoperative decisions about the extent and timing of contralateral thyroidectomy and the need for nerve repair. Finally, this information is needed to improve the postoperative course of treatment, including patient counseling and therapy for reducing voice dysfunction and aspiration.
In this study, we conducted a prospective analysis of the clinical RLNIs identified by IONM and stratified the RLNIs by injury mechanism and by recovery time. The main limitation of a clinical RLNI investigation is the limited availability of specimens for histopathology analysis. Since previous studies have already used IONM in animal models of RLNI [9–12], this study performed a histopathologic analysis of RLNIs experimentally induced in a porcine model and calculated correlations with the clinical data. The objective was to develop a simple system for classifying RLNIs by severity.
Materials and methods
This clinical study analyzed 3143 patients who had received monitored thyroidectomy during 2008–2014 (1st Division of General Surgery, University of Insubria, Italy). Exclusion criteria were preoperative VCP (n = 29), no record of pre- or postoperative laryngeal examination (n = 16), an RLNI mechanism that could not be explained or identified by IONM (n = 13), loss of signal (LOS) in intraoperative electromyography (EMG) with complete or partial recovery before wound closure (n = 47), thyroidectomy received in the learning curve period for conventional IONM (n = 50) [13] or continuous IONM (C-IONM, n = 50), and monitoring accessory failure (n = 7). The analysis included 6093 at-risk nerves (3013 right nerves and 3080 left nerves) in 2950 thyroidectomies and 193 lobectomies.
Further analysis refers to 281 RLNIs in which true LOS was identified intraoperatively by conventional IONM (n = 214) or by C-IONM (n = 67) and in which VCP was positively identified by postoperative laryngeal examination. LOS was defined as an absence of the primary, normal, biphasic waveform at supramaximal stimulation with amplitude that was decreased to <100 µV, and it was managed following the troubleshooting algorithm described in the International Neural Monitoring Study Group (INMSG) Guidelines [5, 14].
Surgical technique
IONM
The IONM was performed according to the standard equipment setup, induction and maintenance anesthesia procedures, tube positioning verification tests, and EMG definitions described by the INMSG Guidelines [5]. In accordance with the standard IONM procedures, the endotracheal EMG tube-based surface electrodes were positioned with the neck at full extension, and vagal stimulation and registration of EMG signals were performed before and after RLN dissection [4, 5].
C-IONM
The C-IONM technique was performed as described in the literature [15]. After connecting the vagal nerve C-IONM electrode to the monitoring system, the baseline latencies and amplitudes of evoked responses were calibrated automatically for use as control data. The stimulation frequency for C-IONM was set to 1 per second. Initial baseline responses were expected to exceed 500 μV. The upper limit threshold for the latency (+10 %) and the lower limit threshold for amplitude (−50 %) were depicted as separate alarm lines.
Identifying and elucidating RLNI mechanisms
In each step of the IONM procedures, the surgeon used a handheld stimulating probe for repeated tests of the RLN to observe any modification of amplitude or latency EMG signal and to elucidate where and how the RLN may have been injured. In case of true LOS and nerve injury, the surgeon maps and pinpoints the location of disrupted nerve conduction with identification of the supposed mechanism of the RLNI. For example, if the occurrence of LOS is sudden after the application of energy-based devices (EBD) or during bipolar or monopolar electrocautery near the RLN, the RLNI was classified as thermal injury. If the patient had a gradually decrease in the EMG signal after a medial thyroid retraction maneuver, the RLNI was classified as traction injury. In patients with ligature or clip entrapment, the ligature or clip was immediately removed. In cases of transection (discontinuity) of the injured nerve, tentative re-approximation was performed with sutures or glue under magnification loupes.
Follow-up
Pre- and postoperative follow-up of all RLNIs was performed by an independent laryngologist. Vocal cord mobility was checked by direct laryngoscopy 24–48 h before surgery and within 2 days after surgery [16]. Any reduction in vocal cord mobility was recorded as postoperative VCP. In all patients with documented postoperative VCP, examinations were performed every week for 1 month and every 3–4 weeks thereafter until full recovery of vocal cord function was confirmed by the laryngologist. If the patient showed no evidence of recovery within 12 months of surgery, the VCP was defined as permanent.
Stratification of RLNIs by injury mechanism
The following issues were analyzed and compared for each RLNI type:
-
(1)
Prevalence of presumed RLNI mechanism As described above, in case of true LOS and RLNI, the surgeon follows the standardized procedures to elucidate the supposed injury mechanism. [1, 3, 5]. The RLNIs investigated in this study were classified into seven categories according to injury mechanism: (1) intentional or non-intentional complete transection of the nerve, (2) ligature entrapment with subsequent release, (3) traction lesion caused by medial retraction and lateral dissection of the thyroid, (4–6) clamping, suction, or compression injury caused by a surgical instrument, and (7) thermal injury caused by a monopolar or bipolar or EBD.
-
(2)
Comparison of recovery time and permanent VCP rates Recovery time is defined as the time interval (days) from postoperative VCP to vocal function recovery during follow-up. Permanent RLN palsy is defined as VCP lasting longer than 12 months.
-
(3)
Physical changes in injured nerve As noted above, after confirming true LOS by following the troubleshooting algorithm, the surgeon identifies and maps the location of the disrupted nerve conduction and examines for physical change on the injured nerve. Positive physical change (visible RLNI) is defined as any discontinuity (transection lesion), compression notch, hyperemia, or charcoal black lesion at the site of disrupted nerve conduction. All clinical data for injured nerves were collected prospectively in a dedicated electronic Microsoft Office Access Data Base (Microsoft Corp, Redmond, Wash). Statistical analysis was performed with SPSS, release 15.0 for Windows (SPSS Inc, Chicago-Ill, USA). A P-value less than 0.05 was considered statistically significant. Efforts were made to avoid sources of bias such as the loss of individuals to follow-up during the study. The Chi square test was used for the statistical analysis.
Animal models for comparing RLNI severity
A well-established prospective porcine RLN research model combined with C-IONM [9–11] was used to induce different types of RLNI and compare the morphological change. Six Duroc–Landrace male pigs (weight 20–25 kg) were used for animal models according to protocols 100,097 and 102,100 of the Institutional Animal Care and Use Committee of Kaohsiung Medical University. In accordance with the typical clinical scenario, C-IONM was used to detect and confirm true LOS after RLNI. The C-IONM equipment and settings used in the animal studies were identical to those used in the clinical phase of this study. The animals were subjected to RLN traction, clamping, and thermal injury experiments (each group used 2 animals and 4 RLNs). Injured RLN segments were collected for histopathology to compare the morphological alterations caused by the experiments above.
Results
Prevalence of RLNI mechanisms
All 281 RLNIs were unilateral, and the overall VCP rate was 4.6 % in at-risk nerves and 8.9 % in at-risk patients. The order of prevalence of the RLNIs was traction injury (71 %; n = 202), thermal injury (17 %; n = 45), compression injury (4.2 %; n = 12), clamping injury (3.4 %; n = 10), ligature entrapment (1.6 %; n = 5), suction injury (1.4 %; n = 4), and nerve transection (1.4 %; n = 4). (Table 1) There injury types did not significantly differ in epidemiological characteristics, body mass index, thyroid pathology, extent of operations, proportion of bilateral procedures, side, mean weight of thyroid, mean size of dominant nodules, RLN identification rate, RLN extralaryngeal bifurcation, incidence of non-RLN, cumulative dose of intraoperative and postoperative corticosteroids, and the use of IONM or C-IONM (data not shown).
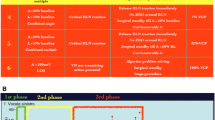
Comparison of palsy recovery for each RLNI type
Figure 1 shows the VCP recovery time stratified by RLNI type. Recovery time for temporary RLNIs ranged from 7 days for traction injury to 10 months for thermal injury (mean 35.2 days). Recovery time exceeded 6 months in four patients with VCP (three with thermal injuries and one with clamping injury). In Table 1, the mean recovery time for temporary VCP is stratified by injury type. Recovery of VCP was significantly faster in the traction group compared to other groups (p < 0.001). None of the transection nerves were recovered.
Stratified recovery times for transient injuries in seven different RLNI types. Time interval from VCP to VCP recovery during follow-up. Recovery of injured nerves was significantly (p < 0.001) faster in traction injuries compared to other injury types. No nerves with transection injury were recovered (data not shown)
Complete recovery of vocal cord function was documented in 91 % (n = 256) of the nerve injuries. Thus, 9 % (25/281) of the RLNIs were permanent. Because of the insufficient number of permanent RLN palsies, none of the analyzed variables revealed a statistically significant difference. Table 1 stratifies the overall ratios of temporary and permanent VCP for each RLNI type. Fifty-two (18.5 %) patients with VCP had no symptoms at the first postoperative laryngeal examination. All patients with VCP periodically received laryngeal examinations, and all symptomatic patients received speech therapy for at least 12 months. In patients who did not show satisfactory improvement after 12 months of speech therapy, surgical options were considered. Medialization thyroplasty for permanent lesion was performed in 9 of the 25 patients who were continuingly suffered from dysphonia and aspiration.
Physical changes in injured nerve
Physical changes were noted in 14 % (39 of 281) of the injured nerves, including 4/4 (100 %) nerve transections, 9/10 (90 %) clamping injuries, 4/5 (80 %) ligature entrapments, 2/4 (50 %) suction injuries, 10/202 (5 %) traction lesions, 10/45 (22 %) thermal injuries, and 0/12 (0 %) compression injuries. The rate of permanent VCP in visibly injured nerves was 56 % (22/39). Among the remaining 86 % (242/281) IONM-detectable RLNIs without physical changes, the rate of permanent VCP was only 1.2 % (3/242) (Table 1).
Morphological analysis of animal models of RLNI
Table 2 summarizes the design and protocol of the animal study and the obtained data. Figure 2 shows the experimental RLNI model and cross-sectional light microscopy images of traction injury (A–C), mechanical injury (D–F), and thermal injury (G–I). In the traction injury group, all RLNs showed a progressive LOS after the injury was induced (mean time to LOS, 102 ± 9.8 s (range, 93–118 s). Figure 2b, c shows the results of the histopathology examination. Most morphological changes occurred in outer structures such as the epineurium and perineurium. In contrast, structures in the endoneurium remained relatively intact. All RLNs with mechanical injury showed an immediate (less than 1 s) LOS after clamping (Fig. 2d). Regarding general morphology, Fig. 2e,f shows that distortion of the epineurium and perineurium was greater in the mechanical injury group compared to the traction injury group. However, structures in the endoneurium remained relatively intact in this group. All RLNs with thermal injury (Fig. 2g) showed a rapid LOS after application of bipolar electrocautery at 60 W from a distance of 1 mm (mean duration: 1.4 ± 0.3 s; range: 1.1–1.8 s). Figure 2h, i shows that compared to the traction and mechanical injury groups, the thermal injury group had less distortion of the outer structure but more severe damage to the inner endoneurium, including the myelin sheath and the axon.
Experimental porcine model of RLNIs and light microscopic images of toluidine blue-stained cross-sections of RLN fibers after traction injury (a–c), clamping injury (d–f), and thermal injury (g–i). All injured nerves showed complete loss of EMG signal during continuous RLN electrophysiologic neuromonitoring. The precise locations of RLNIs (arrows) were confirmed with a handheld stimulation probe (stars)
Discussion
This study prospectively evaluated 6093 nerves at risk during monitored thyroidectomy and compared the recovery characteristics in 281 RLNIs. Morphological changes caused by different RLNI types were compared in a porcine model. The results revealed that each RLNI type had a different clinical recovery outcome (Fig. 1) and was associated with different morphological changes (Fig. 2). We noted that traction injury is the most common (71 %) and has a shorter recovery time, low definitive RLN palsy (1.4 %), low rate of physical changes (5 %) (Table 1), and associated with less histological disturbance than mechanical trauma or thermal injury (Fig. 2). Additionally, cord immobility was permanent in 56 % of cases of visible RLNI. In cases of IONM-detectable RLNIs without physical changes, however, cord immobility was permanent in only 1.2 % (Table 1).
According to the present analysis of clinical recovery outcome (Fig. 1), the morphological findings of the animal studies (Fig. 2), and the definitions and mechanisms of different RLNI types reported in the literature [2, 3, 8], we defined, classified, and ranked each RLNI type by severity (Table 3). Traction injuries (Class-A) were defined as injuries of mild severity because of their short recovery time, low rate of definitive RLN palsy and physical changes, and mild histological disturbance. Mechanical trauma (Class-B, such as compression, clamping, or suction injures) and constricting injury (Class-C) were defined as injuries of mild or moderate severity. In traction and mechanical injuries, the recovery outcome may depend on the dose and duration of the injury stress applied on the injured nerve.
Thermal injuries (Class-D) were defined as injuries of moderate or severe severity because they were associated with a slow recovery time (Fig. 1) and severe histological disturbance in the endoneurium (Fig. 2). Of course, the severity of the injury and the recovery outcome may be affected by temperature [11] and by the extent of thermal spread from various EBDs [9]. Transection injuries (Class-E), which were injuries that caused loss of nerve continuity, were classified as injuries of high severity. However, the proposed classification system requires further validation in a multicenter prospective analysis of the recovery outcome of different RLNI types.
This study found that the most common cause of RLNI was traction injury (71 %) followed by thermal injury (17 %), mechanical trauma (9 %, including compression, clamping, and suction injury), ligature entrapment (1.6 %), and nerve transection (1.4 %). The high prevalence of traction injury may be associated with the need for mobilization and medial retraction of the thyroid lobe during RLN dissection. For example, the RLN can be overstretched during RLN dissection. The RLN can also be compressed between the trachea and a dense fibrous band or crossing artery (especially within the region of the Berry’s ligament) [2]. All thermal injuries in this study were induced by EBDs used near the RLN. The wide availability of EBDs is expected to increase the incidence of thermal injury in the future [17]. Therefore, the use of EBDs during thyroidectomy should be standardized to avoid RLNI [9].
This study confirmed the hypothesis that different RLNI types have very different potentials for recovery (Fig. 1; Table 1). Therefore, the RLNI type should be considered when deciding whether to perform a staged operation. For example, in malignant cases that clearly require a radical thyroidectomy and postoperative radioiodine or radiotherapy, staged surgery is not recommended for transection (Class-E) or for visible thermal lesions (Class-D) because of the low possibility of functional recovery in a short period of time, even after a successful repair. Wang et al. [18] reported that intraoperative administration of corticosteroids can shorten the surgical recovery time in patients with temporary RLN palsy. In this study, however, the use of corticosteroids did not show a significantly recovery outcome difference among the different RLNI types.
The 50 thermal injuries analyzed in this study had a long mean recovery time. Surprisingly, however, the overall rate of VCP recovery was relatively high (72 %). According to the present animal study, thermal injured nerve is associated with greater histological disturbance (Fig. 2) and therefore the VCP should be less reversible in clinical sequence. Further analyses revealed that most permanent injuries occurred during conventional IONM, whereas most temporary thermal injuries occurred during C-IONM. Although this study did not reveal a statistically significant difference between IONM and C-IONM, the difference in permanent injuries is consistent with the finding of our recent animal studies that C-IONM may be helpful for detecting thermal injury in its earliest phases and may reduce the severity of thermal RLNI [11]. According to the literature, C-IONM is a technological improvement over conventional IONM. Notably, hundreds of cases of C-IONM performed without side effects have been reported in the literature [19].
This study revealed physical changes in only 14 % of the injured nerves. Permanent VCP was detected in a high percentage (56 %) of visible RLNIs but in a very low percentage (1.2 %) of RLNIs without physical changes. This finding also highlights the effectiveness of IONM as a tool for intraoperative detection of EMG loss, which can alert surgeons to the need for early corrective surgical treatment to reduce the risk of a visible or permanent RLNI.
A limitation of this study is that the cause of RLNI might be multi-factorial and due to a combination of multiple events [20, 21]. Another limitation is the highly variable severity of RLNI. The extent and magnitude of injury are expected to vary widely, even within individual categories of injury. However, this study used standard IONM procedures for registering and comparing EMG signals in each step, and the analysis was limited to cases in which the loss of function and the cause of the lesion were certain. Therefore, we believe that the dominant mechanisms of the RLNIs analyzed in this study were accurately identified. One difficulty of this study was that data needed for analyzing and defining RLNI mechanisms are not widely reported [2, 3]. Another challenge is the inconsistent definitions used in the literature. For example, the definition of “compression” applied by Snyder’s study is similar to the definition of “stretching” applied by Chiang [2, 3]. Snyder defines “ligature” injury as a RLN being caught in a small branch vessel ligature, whereas Chiang defines “constricting” injury as an RLN being caught in a constricting band of connective tissue, which can be confused with a “compression” injury. The present work is the first attempt to develop a simple system for defining and classifying RLNIs and for ranking their severity (Table 3). The novel classification scheme proposed in this study can help clinicians predict the functional outcomes of nerve problems after thyroid surgery.
Conclusions
Different RLNIs cause different morphological changes and have different recovery outcomes. This study revealed that permanent VCP is rare in lesions that are visually undetectable but detectable by IONM. Therefore, clinicians can use IONM as a tool for early detection and classification of RLNIs; this information can then be used to predict recovery outcomes and to formulate intra- and postoperative treatment plans for RLNI.
References
Randolph GW (2013) Surgery of the thyroid and parathyroid glands. Saunders, Philadelphia
Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC, Wu CW (2008) The mechanism of recurrent laryngeal nerve injury during thyroid surgery–the application of intraoperative neuromonitoring. Surgery 143(6):743–749
Snyder SK, Lairmore TC, Hendricks JC, Roberts JW (2008) Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg 206(1):123–130
Chiang FY, Lee KW, Chen HC, Chen HY, Lu IC, Kuo WR, Hsieh MC, Wu CW (2010) Standardization of intraoperative neuromonitoring of recurrent laryngeal nerve in thyroid operation. World J Surg 34(2):223–229
Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, Carnaille B, Cherenko S, Chiang FY, Dionigi G, Finck C, Hartl D, Kamani D, Lorenz K, Miccolli P, Mihai R, Miyauchi A, Orloff L, Perrier N, Poveda MD, Romanchishen A, Serpell J, Sitges-Serra A, Sloan T, Van Slycke S, Snyder S, Takami H, Volpi E, Woodson G (2011) Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 121(Suppl 1):S1–S16
Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A (2008) Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 32(7):1358–1366
Dionigi G, Barczynski M, Chiang FY, Dralle H, Duran-Poveda M, Iacobone M, Lombardi CP, Materazzi G, Mihai R, Randolph GW, Sitges-Serra A (2010) Why monitor the recurrent laryngeal nerve in thyroid surgery? J Endocrinol Invest 33(11):819–822. doi:10.1007/bf03350349
Dionigi G, Alesina PF, Barczynski M, Boni L, Chiang FY, Kim HY, Materazzi G, Randolph GW, Terris DJ, Wu CW (2012) Recurrent laryngeal nerve injury in video-assisted thyroidectomy: lessons learned from neuromonitoring. Surg Endosc 26(9):2601–2608
Wu CW, Chai YJ, Dionigi G, Chiang FY, Liu X, Sun H, Randolph GW, Tufano RP, Kim HY (2015) Recurrent laryngeal nerve safety parameters of the harmonic focus during thyroid surgery: porcine model using continuous monitoring. Laryngoscope 125(12):2838–2845. doi:10.1002/lary.25412
Wu CW, Dionigi G, Sun H, Liu X, Kim HY, Hsiao PJ, Tsai KB, Chen HC, Chen HY, Chang PY, Lu IC, Chiang FY (2014) Intraoperative neuromonitoring for the early detection and prevention of RLN traction injury in thyroid surgery: a porcine model. Surgery 155(2):329–339
Lin YC, Dionigi G, Randolph GW, Lu IC, Chang PY, Tsai SY, Kim HY, Lee HY, Tufano RP, Sun H, Liu X, Chiang FY, Wu CW (2015) Electrophysiologic monitoring correlates of recurrent laryngeal nerve heat thermal injury in a porcine model. Laryngoscope 125(8):E283–E290. doi:10.1002/lary.25362
Puram SV, Chow H, Wu CW, Heaton JT, Kamani D, Gorti G, Chiang FY, Dionigi G, Barczynski M, Schneider R, Dralle H, Lorenz K, Randolph GW (2015) Vocal cord paralysis predicted by neural monitoring electrophysiologic changes with recurrent laryngeal nerve compressive neuropraxic injury in a canine model. Head Neck. doi:10.1002/hed.24225
Dionigi G, Bacuzzi A, Boni L, Rovera F, Dionigi R (2008) What is the learning curve for intraoperative neuromonitoring in thyroid surgery? Int J Surg 6(Suppl 1):S7–12
Dralle H, Sekulla C, Lorenz K, Thanh PN, Schneider R, Machens A (2012) Loss of the nerve monitoring signal during bilateral thyroid surgery. Br J Surg 99(8):1089–1095
Dionigi G, Chiang FY, Hui S, Wu CW, Xiaoli L, Ferrari CC, Mangano A, Lianos GD, Leotta A, Lavazza M, Frattini F, Annoni M, Rausei S, Boni L, Kim HY (2015) Continuous intraoperative neuromonitoring (C-IONM) technique with the automatic periodic stimulating (APS) accessory for conventional and endoscopic thyroid surgery. Surg Technol Int 26:101–114
Dionigi G, Boni L, Rovera F, Rausei S, Castelnuovo P, Dionigi R (2010) Postoperative laryngoscopy in thyroid surgery: proper timing to detect recurrent laryngeal nerve injury. Langenbeck’s Arch Surg 395(4):327–331. doi:10.1007/s00423-009-0581-x
Dionigi G (2009) Energy based devices and recurrent laryngeal nerve injury: the need for safer instruments. Langenbeck’s Arch Surg 394(3):579–580 author reply 581-576
Wang LF, Lee KW, Kuo WR, Wu CW, Lu SP, Chiang FY (2006) The efficacy of intraoperative corticosteroids in recurrent laryngeal nerve palsy after thyroid surgery. World J Surg 30(3):299–303
Bacuzzi A, Dralle H, Randolph GW, Chiang FY, Kim HY, Barczynski M, Dionigi G (2015) Safety of continuous intraoperative neuromonitoring (C-IONM) in thyroid surgery. World J Surg. doi:10.1007/s00268-015-3288-x
Phelan E, Schneider R, Lorenz K, Dralle H, Kamani D, Potenza A, Sritharan N, Shin J, Randolph WG (2014) Continuous vagal IONM prevents recurrent laryngeal nerve paralysis by revealing initial EMG changes of impending neuropraxic injury: a prospective, multicenter study. Laryngoscope 124(6):1498–1505. doi:10.1002/lary.24550
Schneider R, Bures C, Lorenz K, Dralle H, Freissmuth M, Hermann M (2013) Evolution of nerve injury with unexpected EMG signal recovery in thyroid surgery using continuous intraoperative neuromonitoring. World J Surg 37(2):364–368
Acknowledgments
The animal experiments in this study were supported by grants from the Kaohsiung Medical University Hospital (KMUH 103-3T07, 103-3R36) and the Ministry of Science and Technology, Taiwan. (MOST 103-2314-B-037-037- MY2).The authors are grateful to Dr. Pao-Chu Hun (Veterinarian, Laboratory Animal Center, KMU), Dr. Pi-Ying Chang, Dr. I-Cheng Lu (Anesthesiologists, KMUH), and Dr. Kuo-Bow Tsai (Pathologist, KMU) for their valuable technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Dionigi, G., Wu, CW., Kim, H.Y. et al. Severity of Recurrent Laryngeal Nerve Injuries in Thyroid Surgery. World J Surg 40, 1373–1381 (2016). https://doi.org/10.1007/s00268-016-3415-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3415-3