Abstract
Background
Recurrent laryngeal nerve palsy (RLNP) is one of the most common complications after thyroidectomy. We aim to evaluate the role of intraoperative corticosteroids in preventing or treating postoperative RLNP.
Materials and Methods
We conducted a prospective study of 295 patients who underwent either total lobectomy or total thyroidectomy with or without using intraoperative corticosteroids. All cases were operated on by the same surgeon. Measurement of the RLNP rate was based on the number of nerves at risk. Data were analyzed for differences in postoperative temporary or permanent RLNP rate and recovery days.
Result
The rate of temporary/permanent RLNP was 5.7% (11 out of 194)/0.52% (1 out of 194) and 6.9% (12 out of 173)/0.58% (1 out of 173) according to groups with and without corticosteroids. This difference did not reach statistical significance. Among those 23 patients who recovered from RLNP, the mean time to recovery was significantly shorter for patients receiving intraoperative steroids (28.6 vs. 40.5 days, P = 0.045).
Conclusion
A single dose of intraoperative corticosteroids did not produce any benefit in terms of reducing the postoperative temporary/permanent RLNP rate, but it did shorten the recovery time for patients suffering from temporary RLNP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
One of the most common serious and unpleasant complications of thyroid surgery is iatrogenic recurrent laryngeal nerve palsy (RLNP). The resulting hoarseness is not only a terrible complication for patients who rely on their voice professionally, but it also leads to dyspnea and life-threatening glottal obstruction when bilateral recurrent laryngeal nerves (RLNs) have been jeopardized. Therefore, strategies that prevent RLNP are of great interest. One way is to ensure the integrity of the nerves with routine identification of RLN, which is proposed by most surgeons today. However, RLNP may result from direct mechanical damage without disruption. This disparity between anatomic neural integrity and actual RLN function probably results from trauma to the intact nerve. Nerve manipulation during thyroid surgery may cause neural edema and consequent dysfunction, resulting in anything from neurapraxia to axonotmesis.
There are both experimental and clinical data supporting the notion that the administration of steroids may prevent or reduce neural edema.1–3 Patients with idiopathic facial palsy have shown improved facial nerve function after an empiric course of corticosteroids.4,5 To date, only Lore et al.6 in their book have mentioned the benefit of intraoperative steroids in thyroid surgery. In order to elucidate the role of intraoperative corticosteroids in ameliorating postoperative nerve paresis by reducing the neural edema accompanying the inevitable nerve manipulation during nerve identification, as well as to promote recovery of nerve function when paresis occurs, we conducted a prospective, case-controlled study of patients undergoing either total thyroidectomy or total lobectomy, with routine identification of RLN, with or without a single, intraoperative dose of corticosteroids to verify the therapeutic value of this strategy and its associated complications.
MATERIALS AND METHODS
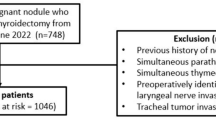
Patients
We designed a prospective, case-controlled clinical trial to evaluate the efficacy of systemic corticosteroids with regard to RLNP following total thyroidectomy or lobectomy running from January 1997 to August 2004. All patients enrolled were operated on by the same surgeon (Dr. Chiang). Routine identification of RLN was performed during all operative procedures. The surgical procedure for identification of RLN was similar to that described in 1986 by Harness et al.7 RLN was not identified early in the operative procedure. When dissection proceeded to the area of Berry’s ligament, RLN was identified where it coursed through the ligament or close to it. Where a large thyroid mass or substernal goiter was encountered RLN was identified and traced from the recurrent nerve triangle, as advocated by Lore.8
In the first half of this period (experimental group), all patients received a single intravenous dose of 100 mg hydrocortisone (Solucortef, Pharmacia-Upjohn). The steroids were given just before we began to identify RLN. In the second half of this period (control group), no steroids were administered. All patients received preoperative and postoperative flexible laryngoscopic examinations of the vocal cords. When vocal cord palsy was identified, follow-up was weekly initially and then every 3–4 weeks thereafter until recovery was achieved, with the dysfunction considered permanent if it still persisted after 6 months. Patients were excluded from the study if they had preoperative RLNP or nerves encased by cancer, in which intentional sacrifice was necessary.
Data Analysis
In this study, the rate of RLNP was calculated based on the number of nerves at risk. In order to investigate the effect of intraoperative steroid on RLNP in patients with different underlying diseases, we further divided our patients into four groups:
-
1.
Primary benign thyroid disease
-
2.
Thyroid cancer
-
3.
Graves’ disease
-
4.
Reoperation
Patients undergoing a first operation for a nodular goiter, adenoma or thyroiditis were included in the primary benign thyroid disease category. Individuals diagnosed with thyroid carcinoma from histopathology, or those who underwent completion thyroidectomy for cancer were grouped with the thyroid cancer cases. Patients who had thyrotoxicosis, a diffuse goiter or ophthalmopathy clinically were included in the Graves’ disease category, with 6 of these associated with thyroid cancer. Patients who had previously undergone thyroid surgery were included in the reoperation group. Of these, 1 was recurrent Graves’ disease, 3 thyroid cancer, and 5 were recurrent goiter. To test the effects of intraoperative steroids on RLN outcome and complications, inter-group differences were assessed using the appropriate Chi-squared or Fisher exact tests for categorical data. Mann–Whitney U tests were used to verify the differences in recovery days between patients with or without the use of intraoperative steroids. P values of 0.05 or less were considered significant.
RESULTS
The details of this study are shown in Table 1. There were 143 (194 nerves at risk) and 152 (173 nerves at risk) patients in the experimental and control groups respectively. The integrity of all RLNs (367 nerves at risk) was ensured at the end of surgery. The overall risk of temporary/permanent RLNP was 6.3% (23 out of 367)/0.54% (2 out of 367). The risk of temporary/permanent RLNP in patients with or without the use of intraoperative steroids was 5.7% (11 out of 194)/0.52% (1 out of 194) and 6.9% (12 out of 173)/0.58% (1 out of 173) respectively. It seemed that the rate of postoperative RLNP increased without the use of intraoperative steroids, although the difference did not reach statistical significance (temporary/permanent RLNP, P = 0.49/0.53). Among the 23 patients who had temporary RLNP, the recovery times ranged from 10 to 36 days and 14 to 61 days for patients with or without intraoperative steroids respectively. The mean recovery time for temporary RLNP was 28.6/40.5 days for patients with/without intraoperative steroids and the difference was statistically significant (P = 0.045). Table 2 showed the effect of intraoperative steroids on RLNP in patients with different underlying diseases. No statistical significance was found among the groups when they used or did not use intraoperative steroids. None of these patients reported complications associated with the use of intraoperative steroids.
DISCUSSION
Identification of RLN has been advocated as a standard procedure in thyroid surgery.9–11 Although RLN can be safely dissected and preserved by a skillful surgeon, postoperative nerve paralysis, usually temporary, will still occur in as many as 3%–4% of patients who have benign thyroid disease undergoing thyroid surgery.9,10,12 The incidence may be triple or more for patients having a thyroid operation for Graves’ disease13–15 or thyroid cancer.16,17 Empirically, some surgeons use steroids during thyroid operations in an attempt to reduce postoperative neural edema resulting from inevitable nerve manipulation during identification of RLN, as well as to promote recovery of nerve function when nerve paralysis occurs. However, there have only been few published data concerning the efficacy of intraoperative steroids in the management or prevention of nerve dysfunction resulting from operation.
Buchman et al.18 used a single dose of intraoperative corticosteroids in patients receiving surgery for acoustic neuroma, showing no apparent benefit from intraoperative steroid use in terms of preventing or treating postoperative facial nerve palsy. Lee et al.19 used perioperative corticosteroids in an attempt to ameliorate facial nerve palsy after parotidectomy, showing no benefit in the controlled trial. On the contrary, Lore et al.6 said that the rate of temporary RLNP can be reduced from 9 to 2.6% with the use of preoperative or/and intraoperative steroids. In addition, the use of steroids reduces the longest duration of temporary vocal cord paralysis from 9 to 2 months. Given the above observations, we conducted a prospective study to evaluate the role of intraoperative corticosteroids in the prevention or management of RLNP resulting from thyroid surgery.
We routinely identify RLN in every case when performing thyroidectomy. There will be RLN dysfunction after thyroid surgery relating to axonal discontinuity, functional impairment of the intact nerve, or a combination of these factors resulting from nerve manipulation. In this study, the integrity of all RLNs was ensured after operation. However, there were still 2 patients (1 control subject and 1 subject from the experimental group) who had permanent RLNP in our study. This study showed that a single dose of intraoperative steroids was not effective in preventing RLNP during thyroid operation. Although the rate of RLNP did not decrease to a statistically significantly amount, the number of days to recovery for patients using intraoperative steroids was significantly lower (28.6 vs. 40.5 days, P = 0.045). The reason may have been that steroids decrease the chance of traumatic edema or vasospasm, which might have led to neurapraxia.
Hydrocortisone sodium succinate was chosen as the experimental drug in this study because it is a potent glucocorticoid agonist with rapid metabolism. No complications occurred as a result of the use of steroids, including brief behavior changes, such as euphoria or psychosis, electrolyte imbalance, increased susceptibility to infection, and hypersensitivity response.
The controversy surrounding this study may contribute to the lack of randomization. In the first half of the study period, all participants in the experimental group received a single intravenous dose of 100 mg of hydrocortisone (Solucortef) during operation. The steroids were given just before we began to identify RLN. In the second half of the study period, no steroids were administered to the control group. Some may conclude that surgical experience may obscure the use of steroids. However, we considered that this factor could be neglected if all the procedures were performed by the same experienced thyroid surgeon, who had performed thyroid surgery for more than 20 years.
CONCLUSION
Although we were unable to demonstrate any benefit in terms of reducing the rate of RLNP, we demonstrated that the duration of temporary RLNP can be reduced with the use of a single dose of intraoperative steroids in a prospective study. We think that this is important, not only to the patients, but also to the physicians caring for them. In the absence of increased morbidity from the single dose of steroids, it may be efficacious to consider using the steroids, particularly in patients where difficult dissection around the nerves is anticipated, such as those with locally advanced cancers, Graves’ disease, and patients undergoing reoperation.12 We expect that increasing our sample size or extending the steroid dosing scheme will result in a treatment advantage for patients who receive steroids while undergoing thyroidectomy.
References
Jones KJ, Drengler SM, Oblinger MM. Gonadal steroid regulation of growth-associated protein GAP-43 mRNA expression in axotomized hamster facial motor neurons. Neurochem Res 1997;22(11):1367–1374
Bansberg SF, McCaffrey TV. The effect of systemic triamcinolone acetonide on nerve repair. Otolaryngol Head Neck Surg 1987;96(2):158–164
Lipton R, McCaffrey TV, Ellis J. The beneficial effect of triamcinolone acetonide on nerve repair with autogenous grafts. Otolaryngol Head Neck Surg 1986;94(3):310–315
Stankiewicz JA. A review of the published data on steroids and idiopathic facial paralysis. Otolaryngol Head Neck Surg 1987;97(5):481–486
Austin JR, Peskind SP, Austin SG, et al. Idiopathic facial nerve paralysis: a randomized double blind controlled study of placebo versus prednisone. Laryngoscope 1993;103(12):1326–1333
Lore JM Jr, Farrell M, Castillo NB. Endocrine surgery. In: Lore JM Jr, Medina JE (eds) An Atlas of Head and Neck Surgery, 4th edn. Elsevier, Philadelphia 2005:963–965
Harness JK, Fung L, Thompson NW, et al. Total thyroidectomy: complications and technique. World J Surg 1986;10(5):781–786
Lore JM Jr. Practical anatomical considerations in thyroid tumor surgery. Arch Otolaryngol 1983;109(9):568–574
Jatzko GR, Lisborg PH, Muller MG, et al. Recurrent nerve palsy after thyroid operations—principal nerve identification and a literature review. Surgery 1994;115(2):139–144
Lo CY, Kwok KF, Yuen PW. A prospective evaluation of recurrent laryngeal nerve paralysis during thyroidectomy. Arch Surg 2000;135(2):204–207
Liu Q, Djuricin G, Prinz RA. Total thyroidectomy for benign thyroid disease. Surgery 1998;123(1):2–7
Chiang FY, Wang LF, Huang YF, et al. Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery 2005;137(3):342–347
Wagner HE, Seiler C. Recurrent laryngeal nerve palsy after thyroid gland surgery. Br J Surg 1994;81(2):226–228
Razack MS, Lore JM Jr, Lippes HA, et al. Total thyroidectomy for Graves’ disease. Head Neck 1997;19(5):378–383
Agarwal A, Mishra SK. Role of surgery in the management of Graves’ disease. J Indian Med Assoc 2001;99(5):252, 254–256
Steurer M, Passler C, Denk DM, et al. Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of preoperative and postoperative laryngoscopic examination in more than 1000 nerves at risk. Laryngoscope 2002;112(1):124–133
Flynn MB, Lyons KJ, Tarter JW, et al. Local complications after surgical resection for thyroid carcinoma. Am J Surg 1994;168(5):404–407
Buchman CA, Fucci MJ, Slattery WH, et al. Intraoperative corticosteroids in acoustic tumor surgery. Am J Otol 1999;20(3):386–389
Lee KJ, Fee WE Jr, Terris DJ. The efficacy of corticosteroids in postparotidectomy facial nerve paresis. Laryngoscope 2002;112(11):1958–1963
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, LF., Lee, KW., Kuo, WR. et al. The Efficacy of Intraoperative Corticosteroids in Recurrent Laryngeal Nerve Palsy after Thyroid Surgery. World J. Surg. 30, 299–303 (2006). https://doi.org/10.1007/s00268-005-0399-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0399-9