Abstract
Purpose
To evaluate the regenerative potential of surnatants (SNs) from bone marrow concentrate (SN-BMC) and expanded mesenchymal stromal cells (SN-MSCs) loaded onto a collagen scaffold (SC) in comparison with cell-based treatments (BMC and MSCs) in an osteochondral (OC) defect model in rabbits.
Methods
OC defects (3 × 5 mm) were created in the rabbit femoral condyles and treated with SC alone or combined with SN-BMC, SN-MSCs, BMC, and MSCs. In control groups, the defects were left untreated. At three and six months, the quality of regenerated tissue was evaluated with macroscopic, histologic, microtomographic, and immunohistochemical assessments. The production of several immunoenzymatic markers was measured in the synovial fluid.
Results
All proposed treatments improved OC regeneration in comparison with untreated and SC-treated defects. Both BMC and MSCs showed a similar healing potential than their respective SNs, with the best performance exerted by BMC as demonstrated with macroscopic and histological scores and type I and II collagen results.
Conclusions
SNs loaded onto SC exerted a positive effect on OC defect regeneration, underlying the biological significance of the trophic factors, thus potentially opening new opportunities for the use of cell-free-based therapies. BMC was confirmed to be the most beneficial treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteochondral (OC) lesions involve injuries of both bone and cartilage compartments, leading to an alteration in tissue architecture with the release of inflammatory and catabolic mediators [1]. Current therapies regenerate a tissue with reduced biological, biomechanical, biochemical, and viscoelastic characteristics, leading to poor long-term outcomes [2]. Among the biological treatments, the transplantation of expanded mesenchymal stromal cells (MSCs) alone or in combination with bioactive scaffolds has attracted researchers [3,4,5]. Also, the one-step approach, with the transplantation of bone marrow concentrate (BMC), has been developed not only to overcome the limits associated with the use of the culture expanded MSCs, but mainly because of good results reported in preclinical and clinical studies [6,7,8,9].
MSCs show a secretory pattern and their key paracrine control molecules (exosomes, microvesicles) are involved in tissue healing processes, making the cell-free approaches a new and still less exploited therapeutic tool [1, 10, 11]. Thus, MSC surnatant (SN-MSCs) could be employed for a cell-free therapeutic approach, overcoming the drawbacks of the use of cells and a direct release of autologous factors immediately into the lesion site. In vivo, SN-MSCs have already been employed prevalently in rat calvarial and periodontal defects or in osteopenic animals [11]. However, less is known about cartilage regeneration, and to date, only one study showed a neocartilage formation in athymic mice, after the subcutaneous implantation of MSCs expanded in chondrocyte SN [11]
Therefore, the present research aims to evaluate the feasibility of the use of SNs derived from BMC and MSCs as a new approach for the treatment of OC defects created in rabbit knees. To ensure a better stay into the defects site, SN-BMC, SN-MSCs, BMC, and MSCs were loaded onto a collagen scaffold (SC). Based on the importance of paracrine role by progenitor cells, we hypothesized that the use of SN-BMC and SN-MSCs could contribute to the regeneration of the OC tissues, thus posing the basis for the development of a cell-free therapeutic approach
Materials and methods
The experimental protocol and surgical procedures were approved by a local Ethical Committee and authorized by the Italian Ministry of Health (Title of the project: One-step surgery with stem cells for the treatment of osteochondral lesions—No. 0017661, approved on May 29, 2013). Thirty-six male New Zealand rabbits (HARLAN Laboratories SRL, Udine-Italy) (3.0 ± 0.2 kg) were used and maintained in accordance with 2007/526/CE protocols. The animals were housed individually with enriched materials in a controlled environment and exposed to a 12 hour light/dark cycle. Rabbit welfare was monitored daily and animals had free access to food and water and were maintained for at least ten days prior to the beginning of the surgical procedures to allow for acclimatization.
Experimental design
Bilateral OC defects were created in medial femoral condyles. BIOPAD (Novagenit, Trento-Italy), a heterologous equine type I collagen, was used as SC for cells and their SNs and properly shaped before implantation.
Animals were randomized into three groups of 12 animals each:
-
Group 1 (CTR): SC (left condyle), no treatment (right condyle);
-
Group 2: SC + BMC (left condyle), SC + SN-BMC (right condyle);
-
Group 3: SC + MSCs (left condyle), SC + SN-MSCs (right condyle).
Groups 1 and 2 were treated in the same surgical session. In group 3, OC defects were created two weeks after BM harvesting and MSC isolation and expansion.
A lateral knee arthrotomy was performed to expose the femoral condyles and an OC defect (3 × 5 mm) was created in the loading area of both medial condyles. The general anesthesia, post-operative management, and euthanasia protocols were indicated in Online Resource 1.
At the time of euthanasia, synovial fluid (SF) was collected for immunoenzymatic assays and femoral condyles were explanted for macroscopy, microtomography (Micro-CT), histology, and immunohistochemistry (IHC).
BMC and MSCs
Before surgery, 5.0 ± 0.5 ml of bone marrow aspirate (BMA) from the posterior iliac crest of each animal was placed into a syringe coated with saline-heparin solution. In group 2, BMA was centrifuged for 10′ at 1000 rpm to obtain both BMC and SN-BMC, prepared in the same surgical session and combined with SC to be implanted into group 2. In group 3, BMA was processed to isolate and culture MSCs up to passage 2, as already reported [6]. In order to obtain SNs, MSCs at passage 2 were seeded at a density of 10,000 cells/cm2. At 70–80% confluence, MSCs were cultured in serum-free medium and kept for 48 hours at 37 °C and 5% CO2. After this incubation, each SN was collected, placed onto SC, and implanted (1 ml of BMC and 2 × 106 MSCs).
The remaining amount of BMC was analyzed through haemocromocytometry, May Grunwald Giemsa staining, and the colony-forming unit fibroblast (CFU-F) assay and colonies (> 50 cells) were counted [12]. An aliquot of SN-BMC and SN-MSCs was collected for immunoenzymatic assessments. Moreover, remnants of engineered constructs of BMC and MSCs were embedded in optimal cutting temperature (OCT) sectioning medium. Samples were cryosectioned at 12 μm and stained with haematoxylin and eosin (Sigma-Aldrich, St. Louis, MO, USA).
Post-explant evaluations
Femoral condyles were evaluated according to the International Cartilage Repair Society (ICRS) macroscopic assessment scale [13].
Micro-CT evaluations were performed as in Online Resource 2.
Femoral condyles were fixed in 10% neutral buffered formalin, decalcified in a 4% hydrochloric acid and 5% formic acid solution, and then processed for paraffin embedding. Coronal sections (5 ± 1 μm) were obtained and sections from the central portion of each defect were stained with Safranin O/Fast Green (Sigma-Aldrich). Histological images were acquired and analyzed with the digital scanner Aperio ScanScope (Aperio ScanScope CS, Aperio Technologies, Leica Biosystems, USA) and the slides were scored by two blinded histologists adopting the semi-quantitative O’Driscoll modified grading score [14].
IHC (type I and type II collagen) and immunoenzymatic assays of SF were performed as indicated in Online Resource 3.
Statistical analysis
Statistical analysis was performed using R v.3.4.3 software [15]. Data are reported as mean ± SD at a significant level of p < 0.05. After having verified normal distribution (Shapiro-Wilk test) and homogeneity of variance (Levene test), data of bone marrow processing were analyzed with Student’s t test, while the other data with two-way ANOVA, considering “treatment”—six levels (CTR, SC, SC + BMC, SC + SN-BMC, SC + MSCs, and SC + SN-MSCs) and “experimental time”—two levels (3 and 6 months) factors as fixed effects. For each dependent variable, the best model was obtained, verifying both the main effects of factors and their interactions. Thus, the analysis continued using the Tukey HSD test to compare the effects or the interactions of factors between the groups adjusting p value with the Holm-Sidak correction.
Results
BMA and BMC
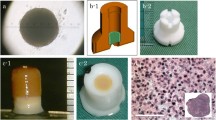
BMC showed higher total nucleated cells (TNC) (p < 0.05) and platelets (PLTs) (p < 0.005) than BMA (Fig. 1a). The resulting concentration factors of TNC and PLTs in BMC were 3.12 and 2, respectively. May-Grunwald-Giemsa staining showed that most of TNC were neutrophils, whereas lymphocytes and monocytes were present at less extent (Fig. 1b). After 14 days, the number of CFU-F was higher in BMC than in BMA (p < 0.005) (Fig. 1c).
In vitro analysis of bone marrow aspirate (BMA) and bone marrow concentrate (BMC). a Bar charts of haemocromocytometric analysis showing values of erythrocytes (RBC), total nucleated cells (TNC), and platelets (PLT) from BMA and BMC (mean ± SD, n = 6); Student’s t test: *p < 0.05; **p < 0.005 versus BMC. b Representative micrographs of May-Grunwald-Giemsa staining of BMA and BMC (scale bar = 100 μm). c Bar charts of CFU-F assay carried out on BMA and BMC (mean ± SD, n = 6); Student’s t test: **p < 0.005 versus BMC. d Representative micrographs of haematoxylin and eosin staining from SC + BMC and SC + MSCs (scale bar = 100 μm)
Histological analysis on SC + BMC and SC + MSCs showed cell colonization of the scaffold and the presence of a heterogeneous population containing erythrocytes and different cellular populations in the group of SC + BMC (Fig. 1d).
SN-BMC showed higher TGF-β1, IGF-I, IL6 (p < 0.0005), and VEGF (p < 0.005) than SN-MSCs. BMC secreted lower MMP-13 (p < 0.0005) than MSCs, even though both cell-based treatments displayed low levels of this protein (Fig. 2a–e).
Post-explant results
Results of the ICRS macroscopic score and of Micro-CT are observed in Table 1.
The greatest repair activity was obtained in the defects treated with SC-BMC at both experimental times. No bone cysts were observed and the SC was no longer visible at three months.
At three months, untreated, SC-implanted defect, SC + MSCs and SC + SN-MSC defects repaired with fibrous tissue with no hyaline-like cartilage, SC + BMC defects with a cartilagineous tissue with organized cells, and SC + SN-BMC with fibrous tissue and chondrocyte clustering at the native edges. Subchondral bone (SB) formation was detected in both SC + BMC and SC + SN-BMC defects.
At six months, SB restoration was observed with a different degree of thickness in all conditions. The untreated condyles showed the absence of staining and several fissures and the SC-treated lesions repaired with deep fissures and chondrocyte clusters along cartilage surface. SC + BMC defects repaired with hyaline cartilage with orthochromatic red staining and normal cell organization in a columnar fashion, SC + SN-BMC ones with a greater cartilage organization, even if the center of the defect was still occupied by a pale stained tissue with minor cellular organization, and SC + MSC and SC + SN-MSC defects with a fibrocartilaginous tissue with no cartilaginous extracellular matrix except at the edges of the defects (Fig. 3).
At three months, a significantly higher score value was observed for SC + BMC than for SC, SC + MSCs (p < 0.005), SC + SN-BMC, and SC + SN-MSCs (p < 0.05). SC + SN-BMC and SC + MSCs performed better than SC + SN-MSCs (p < 0.05) (Fig. 4a).
Bar charts of O’Driscoll total score (a), percentage of positivity for type I collagen (b) and type II collagen (c) in cartilage tissue for each treatment at 3 and 6 months (mean ± SD, n = 6). Two-way ANOVA (factors: “treatment,” “experimental time”) highlighted significant factor interactions for O’Driscoll total score (F = 4.20, p < 0.05) and type I collagen (F = 7.51, p < 0.0005), and a significant effect of “treatment” factor for type II collagen (F = 8.78, p < 0.0005). Tukey HSD test: °p < 0.05; °°p < 0.005; and °°°p < 0.0005 versus CTR (or CTR at 3 months); □p < 0.05, □□p < 0.005, and □□□p < 0.0005 versus SC (or SC at 3 months); ●p < 0.05 and ●●●p < 0.0005 versus CTR at 6 months; †p < 0.05, ††p < 0.005, and †††p < 0.0005 versus SC + BMC at 3 months; ‡‡p < 0.005 and ‡‡‡p < 0.0005 versus SC + BMC at 6 months; §p < 0.05 versus SC + SN-BMC at 3 months; ^p < 0.05 versus SC + MSCs at 3 months; $p < 0.05 versus SC + MSCs at 6 months; and *p < 0.05, **p < 0.005, and ***p < 0.0005 at 6 versus 3 months
At six months, SC + BMC and SC + MSCs performed significantly better than control (p < 0.05), while SC + SN-MSCs score was lower than SC + MSCs (p < 0.05) (Fig. 4a).
Regarding type I collagen, at three months, untreated femoral condyles showed higher positivity than all other conditions with different degree of significance (p < 0.005 and p < 0.0005). SC + BMC (p < 0.0005) and SC + SN-MSCs (p < 0.005) had significant lower value than SC-treated defects. SC + BMC positivity was significantly lower than SC + SN-BMC (p < 0.0005) and SC-MSCs (p < 0.005) (Fig. 4b).
At six months, all treatments and SC-treated defects showed significantly lower positivity than untreated condyles (p < 0.0005 and p < 0.05). A higher significant positivity was found for SC + MSCs (p < 0.0005) and SC + SN-BMC (p < 0.005) than for SC + BMC (Fig. 4b).
Regarding type II collagen, independently from experimental time, SC + BMC showed higher value than untreated defects (p < 0.005) and SC (p < 0.0005), while SC + SN-BMC and SC + MSCs (p < 0.05) showed a significantly higher values than SC (Fig. 4c).
SC + BMC treatment displayed significantly higher IGF-1 than untreated (p < 0.05) and SC-treated defects (p < 0.005), independently from experimental time (Fig. 5a). SC + BMC, SC + SN-BMC, and SC + MSCs led to significantly lower MMP-1 than untreated (p < 0.005 and p < 0.0005), while SC + BMC (p < 0.0005) and SC + SN-BMC (p < 0.05) than SC-treated defects, independently from experimental time (Fig. 5b). No significant differences were highlighted for MMP-13 (Fig. 5c).
Bar charts of protein concentrations of IGF-1 (a), MMP-1 (b), and MMP-13 (c) on synovial fluids for each treatment at 3 and 6 months (mean ± SD, n = 6). Two-way ANOVA (factors: “treatment,” “experimental time”) highlighted a significant effect of “treatment” factor for IGF-1 (F = 6.44, p < 0.0005) and MMP-1 (F = 9.91, p < 0.0005); Tukey HSD test: °p < 0.05, °°p < 0.005, and °°°p < 0.0005 versus CTR; □p < 0.05, □□p < 0.005, and □□□p < 0.0005 versus SC
Discussion
Effective treatments for OC defects are still a challenge for orthopedic surgeons, because large cartilage defects, if not properly treated, lead to OA. Cellular treatments are now available for OC defect in clinics, but they still give unsatisfactory results in terms of cartilage tissue regeneration, especially depending on the age of the patient [3, 16,17,18,19].
Currently, great attention is paid to the evaluation of advanced cell-free-based therapies, since a clear knowledge of soluble factors and mechanisms underpinning their healing potential is lacking in various models of disease like OC defects [20].
Therefore, the present study aimed to evaluate for the first time the healing potential of SNs from expanded MSCs and BMC, and compare their effect with the respective cell treatments for the care of OC defects in a rabbit model.
The overall results of this study showed that all proposed treatments gave a net improvement in the OC regeneration in comparison with untreated and SC-treated defects. In addition, BMC possesses the highest regenerative ability. The use of BMC ameliorated significantly the histological appearance of the defects, downregulated type I collagen, and upregulated type II collagen at both experimental times. Results from cell-based treatments confirmed literature data: a literature review highlighted that BMC seemed to be the best choice for OC defect treatment than MSCs [3]. BMC contains various cell populations, not only MSCs but also hematopoietic cells, endothelial cells, PLTs, and several GFs that are able to induce chondrogenic or osteogenic differentiation of the resident MSCs and to improve the healing process [21,22,23].
Both BMC and MSCs showed a similar healing potential than their respective SNs. In detail, BMC and MSCs performed better in comparison with their respective SNs as also observed for type I collagen for BMC. The lower histological outcome observed for SC + SN-BMC and SC + SN-MSCs compared to cells could be dependent on various factors. It is well known that tissue regeneration is a complex process, where the delivery of specific combinations of multiple factors in a proper dosage and time of exposure is mandatory to obtain the desired effect [24, 25]. Therefore, we can speculate that the use of SN containing factors can provide a good stimulus to launch first repair processes but results were not so efficient at the long-term follow-up.
Presumably, the larger and deeper the defect is, the more the SN fails to regenerate the tissue in comparison to the cell use. Indeed, another factor to consider is that the secreted factors have a short half-life and are not able to counteract the OC defect progression at three and six months; thus, more than one injection into the lesion site may be necessary to sort out a therapeutic effect. In addition, the in vivo injection of SNs into the inflammatory microenvironment of the lesion site could have reduced the amount and the activity of SN proteins for a short period of time. Also, the timing of SN injection has to be taken into account, as the half-life of proteins is context-sensitive. One of the limitations of the present study is due to the exposure of the paracrine factors to a stressed microenvironment during surgery, thus affecting the cellular and molecular mechanisms of tissue repair. Therefore, other treatment modalities are required for future studies.
SN-BMC showed higher protein expression for TGF-β1, IGF1, and VEGF, essential for cartilage and bone healing, and lower MMP13 than SN-MSCs. These results could explain the superior healing potential of the treatment with SC + BMC since TGF-β1 and IGF-1 are important key factors involved in cartilage and bone repair [26]. It is likely that the downregulation of MMP-13 found in BMC-SN is dependent on IGF-1 and TGF-β1, known to prevent ECM degradation through the inhibition of collagenases [27]. Similar findings were found in our previous in vivo study, in which BMC seeded onto a hyaluronic scaffold resulted more beneficial than MSCs in delaying changing an OA sheep model [8].
Further assessments on the efficacy of treatments were carried out on SF, where a reduction of MMP-1 production was detected in all treatments. The highest IGF-1 expression was found following the SC-BMC treatment. Further studies are mandatory to investigate also the effect of EVs, recovered from the culture medium through centrifugation, in comparison to culture medium in toto. EVs are released into the cell medium and are responsible of the intercellular communication, being a reservoir of lipids, proteins, mRNA, and miRNA [28]. It is also hypothesized that the use of EVs instead of SNs could improve the regenerative ability of the culture medium in a cell-free approach.
This study examined and compared for the first time the biological features of SN from BMC and MSCs and the in vivo effect of a cell-free approach in OC defects. The feasibility of the use of cell-free approaches was demonstrated, thus increasing the knowledge towards a future cell-free OC lesion treatment.
References
Hofer HR, Tuan RS (2016) Secreted trophic factors of mesenchymal stem cells support neurovascular and musculoskeletal therapies. Stem Cell Res Ther 7(131). https://doi.org/10.1186/s13287-016-0394-0
Cavallo C, Desando G, Ferrari A, Zini N, Mariani E, Grigolo B (2016) Hyaluronan scaffold supports osteogenic differentiation of bone marrow concentrate cells. J Biol Regul Homeost Agents 30:409–420
Veronesi F, Giavaresi G, Tschon M, Borsari V, Nicoli Aldini N, Fini M (2013) Clinical use of bone marrow, bone marrow concentrate, and expanded bone marrow mesenchymal stem cells in cartilage disease. Stem Cells Dev 22:181–192. https://doi.org/10.1089/scd.2012.0373
Sartori M, Pagani S, Ferrari A, Costa V, Carina V, Figallo E, Maltarello MC, Martini L, Fini M, Giavaresi G (2017) A new bi-layered scaffold for osteochondral tissue regeneration: in vitro and in vivo preclinical investigations. Mater Sci Eng C Mater Biol Appl 70:101–111. https://doi.org/10.1016/j.msec.2016.08.027
Veronesi F, Torricelli P, Borsari V, Tschon M, Rimondini L, Fini M (2011) Mesenchymal stem cells in the aging and osteoporotic population. Crit Rev Eukaryot Gene Expr 21:363–377
Desando G, Giavaresi G, Cavallo C, Bartolotti I, Sartoni F, Nicoli Aldini N, Martini L, Parrilli A, Mariani E, Fini M, Grigolo B (2016) Autologous bone marrow concentrate in a sheep model of osteoarthritis: new perspectives for cartilage and meniscus repair. Tissue Eng Part C Methods 22:608–619. https://doi.org/10.1089/ten.TEC.2016.0033
Veronesi F, Cadossi M, Giavaresi G, Martini L, Setti S, Buda R, Giannini S, Fini M (2015) Pulsed electromagnetic fields combined with a collagenous scaffold and bone marrow concentrate enhance osteochondral regeneration: an in vivo study. BMC Musculoskelet Disord 16(233). https://doi.org/10.1186/s12891-015-0683-2
Desando G, Bartolotti I, Vannini F, Cavallo C, Castagnini F, Buda R, Giannini S, Mosca M, Mariani E, Grigolo B (2017) Repair potential of matrix-induced bone marrow aspirate concentrate and matrix-induced autologous chondrocyte implantation for talar osteochondral repair: patterns of some catabolic, inflammatory, and pain mediators. Cartilage 8:50–60
Giannini S, Buda R, Vannini F, Cavallo M, Grigolo B (2009) One-step bone marrow-derived cell transplantation in talar osteochondral lesions. Clin Orthop Relat Res 467:3307–3320. https://doi.org/10.1007/s11999-009-0885-8
Caplan AI, Dennis JE (2006) Mesenchymal stem cells as trophic mediators. J Cell Biochem 98:1076–1084
Veronesi F, Borsari V, Sartori M, Orciani M, Mattioli-Belmonte M, Fini M (2018) The use of cell conditioned medium for musculoskeletal tissue regeneration. J Cell Physiol 233:4423–4442. https://doi.org/10.1002/jcp.26291
Cavallo C, Desando G, Cattini L, Cavallo M, Buda R, Giannini S, Facchini A, Grigolo B (2013) Bone marrow concentrated cell transplantation: rationale for its use in the treatment of human osteochondral lesions. J Biol Regul Homeost Agents 27:165–175
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A(Suppl 2):58–69
O’Driscoll SW, Keeley FW, Salter RB (1986) The chondrogenic potential of free autogenous periosteal grafts for biological resurfacing of major full-thickness defects in joint surfaces under the influence of continuous passive motion. An experimental investigation in the bone. J Bone Joint Surg Am 68:1017–1035
R Development Core Team (2008) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-07-0, URL http://www.R-project.org
Im GI (2017) Clinical use of stem cells in orthopaedics. Eur Cell Mater 33:183–196. https://doi.org/10.22203/eCM.v033a14
Welch T, Mandelbaum B, Tom M (2016) Autologous chondrocyte implantation: past, present, and future. Sports Med Arthrosc Rev 24:85–91. https://doi.org/10.1097/JSA.0000000000000115
Hochrein A, Zinser W, Spahn G, Angele P, Löer I, Albrecht D, Niemeyer P (2018) What parameters affect knee function in patients with untreated cartilage defects: baseline data from the German Cartilage Registry. Int Orthop. https://doi.org/10.1007/s00264-018-4125-2
Volz M, Schaumburger J, Frick H, Grifka J, Anders S (2017) A randomized controlled trial demonstrating sustained benefit of autologous matrix-induced Chondrogenesis over microfracture at five years. Int Orthop 41(4):797–804. https://doi.org/10.1007/s00264-016-3391-0
Lavoie JR, Rosu-Myles (2013) Uncovering the secretes of mesenchymal stem cells. Biochimie 95:2212–2221. https://doi.org/10.1016/j.biochi.2013.06.017
Sampson S, Botto-van Bemden A, Aufiero D (2013) Autologous bone marrow concentrate: review and application of a novel intra-articular orthobiologic for cartilage disease. Phys Sportsmed 41(3):7–18. https://doi.org/10.3810/psm.2013.09.2022
Cicione C, Muinos-Lopez E, Hermida-Gomez T, Fuentes-Boquete I, Diaz-Prado S, Blanco FJ (2016) Alternative protocols to induce chondrogenic differentiation: transforming growth factor-beta superfamily. Cell Tissue Bank 16:195
Hernigou J, Vertongen P, Chahidi E, Kyriakidis T, Dehoux JP, Crutzen M, Boutry S, Larbanoix L, Houben S, Gaspard N, Koulalis D, Rasschaert J (2018) Effects of press-fit biphasic (collagen and HA/βTCP) scaffold with cell-based therapy on cartilage and subchondral bone repair knee defect in rabbits. Int Orthop 42:1755–1767. https://doi.org/10.1007/s00264-018-3999-3
Santo VE, Gomes ME, Mano JF, Reis RL (2013) Controlled release strategies for bone, cartilage, and osteochondral engineering--part II: challenges on the evolution from single to multiple bioactive factor delivery. Tissue Eng Part B Rev 19:327–352. https://doi.org/10.1089/ten.TEB.2012.0138
Wang Q, Zhang H, Gan H, Wang H, Li Q, Wang Z (2018) Application of combined porous tantalum scaffolds loaded with bone morphogenetic protein 7 to repair of osteochondral defect in rabbits. Int Orthop 42(7):1437–1448. https://doi.org/10.1007/s00264-018-3800-7
Zhang Z, Li L, Yang W, Cao Y, Shi Y, Li X, Zhang Q (2017) The effects of different doses of IGF-1 on cartilage and subchondral bone during the repair of full-thickness articular cartilage defects in rabbits. Osteoarthr Cartil 25:309–320. https://doi.org/10.1016/j.joca.2016.09.010
Lin H, Hay E, Latourte A, Funck-Brentano T, Bouaziz W, Ea HK, Khatib AM, Richette P, Cohen-Solal M (2018) Proprotein convertase furin inhibits matrix metalloproteinase 13 in a TGFβ-dependent manner and limits osteoarthritis in mice. Sci Rep 8(10488). https://doi.org/10.1038/s41598-018-28713-2
Chen B, Li Q, Zhao B, Wang Y (2017) Stem cell-derived extracellular vescicles as a novel potential therapeutic tool for tissue repair. Stem Cells Transl Med 6:1753–1758. https://doi.org/10.1002/sctm.16-0477
Funding
This work was partially supported by the Ministry of Health-Ricerca Corrente to the IRCCS Rizzoli Orthopaedic Institute and by a grant from Regione Emilia Romagna: Programma di Ricerca Regione-Università 2010–2012—Strategic Program “Regenerative Medicine of Cartilage and Bone” (PRUa1RI-2012-007).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The experimental protocol and surgical procedures were approved by a local Ethical Committee and authorized by the Italian Ministry of Health (Title of the project: One-step surgery with stem cells for the treatment of osteochondral lesions—No. 0017661, approved on May 29, 2013).
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Francesca Veronesi and Giovanna Desando equally contributed to this work.
Rights and permissions
About this article
Cite this article
Veronesi, F., Desando, G., Fini, M. et al. Bone marrow concentrate and expanded mesenchymal stromal cell surnatants as cell-free approaches for the treatment of osteochondral defects in a preclinical animal model. International Orthopaedics (SICOT) 43, 25–34 (2019). https://doi.org/10.1007/s00264-018-4202-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4202-6