Abstract
Purpose
Opening wedge high tibial osteotomy (HTO) as a treatment in unicompartimental osteoarthritis of the knee can significantly relieve pain and prevent or at least delay an early joint replacement. The fixation of the osteotomy has undergone development and refinements during the last years. The angle-stable plate fixator is currently one of the most commonly used plates in HTOs. The angular stable fixation between screws and the plate offers a high primary stability to retain the correction with early weight-bearing protocols. This surgical technique is performed as a standard of care and generally well tolerated by the patients. Nevertheless, some studies observed that many patients complained about discomfort related to the implant.
Methods
Therefore, the stability of two different intramedullary nails, a short implant used in humeral fractures and a long device used in tibial fractures for stabilization in valgus HTOs, was investigated as an alternative fixation technique. The plate fixator was defined as reference standard. Nine synthetic tibia models were standardly osteotomized and stabilized by one of the fixation devices. Axial compression was realized using a special testing machine and two protocols were performed: a multi-step fatigue test and a load-to-failure test.
Results
Overall motion, medial, and lateral displacements were documented. Fractures always occurred at the lateral cortex. Axial cyclic loading up to 800 N was tolerated by all implants without failure. The tibia nail provided highest fatigue strength under the load-to-failure conditions.
Conclusions
The results suggest that intramedullary nailing might be used as an alternative concept in HTO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis of the knee occurs in 10–18% of all adults aged over 60 [1]. The resulting morbidity reduces quality of life, and without treatment, osteoarthritis often leads to significant physical disability [2, 3]. Conservative treatments to relieve pain and inactivity include therapy with NSAIDs, physical activity, braces, and injections of steroids or hyaluronic acids. When conservative approaches become insufficient, the patients often request surgery. Surgical treatment options include arthroscopic debridement and lavage, high tibial osteotomy (HTO), and unicompartimental or total knee arthroplasty [4]. Especially total knee replacement has progressed to a well-established treatment option, enabling patients to return to normal activities with a pain-free knee after recovery from surgery [5]. Despite actual progresses in knee surgery, younger age is still associated with increased revision rates after primary knee replacements [6]. For this patient population, prevention strategies such as early joint-conserving surgical interventions are of high importance. Therefore, considering appropriate indication, precise planning, and accurate surgical skills, HTO has progressed to a well-accepted procedure in younger patients with unicompartimental osteoarthritis and pathologic mechanical axis [7].
Currently, many different implants from different manufacturers are available for HTO. The current state-of-the-art fixation system is an angle-stable plate fixator. This angular stable locking plate enables a reliable fixation, with a safe bone union and a long-term maintenance of the correction [8, 9]. The surgical fixation allows early weight-bearing protocols after surgery and major procedure-specific risks such as infections, dislocation, mal-union, and thrombosis are low [10,11,12]. Modifications with a longer shaft portion and the possibility to apply compression to the lateral hinge have further increased the stability and reduced complications due to implant failure. Nevertheless, a high proportion of patients reported discomfort in relation to the implant. Niemeyer and colleagues reported that 40.6% of patients that underwent opening wedge HTOs and were stabilized with a plate fixator complained about pain related to the implant in a three year follow-up survey [13].
The main objective of this study was to analyze whether intramedullary nails that have been designed to reduce local tissue irritation and pain caused by extramedullary devices could be used in HTO. Using intramedullary nails might prevent secondary surgical treatment to remove a potentially pain-causing extramedullary fixation device. Therefore, two different intramedullary nails—a short nail designed to stabilize fractures of the proximal humerus and a longer nail designed to stabilize fractures of the proximal tibia—were used to test HTO mechanical stability in a synthetic tibia model.
Materials and methods
Experimental setup
The mechanical testing system was set up according to the work published by Agneskirchner and colleagues in 2006 [8]. The Tomofix® Medial High Tibial Plate (DePuy Synthes, Zuchwil, Switzerland) served as the reference standard. Nine (n = 9) left composite tibia synthetic bones (Model 3401-1, Sawbones Europe AB, Malmö, Sweden) with a 10° varus to simulate the axis deviation were used. Synthetic bones are considered to have similar structural and mechanical properties like natural bones [14, 15]. Synthetic bones were mounted into a specially designed fixture (Fig. 1a) which allowed to guide an axial loading with a 62% lateral offset from the centre of the joint according to the procedure described by Fujisawa and colleagues [16]. A typical biplanar osteotomy with a horizontal cut of the posterior 2/3 of the tibia, leaving 10 mm of lateral bone intact and a second complete cut in the frontal plane (110°) behind the tibial tuberosity, was performed [17]. A special sawing device was used to guarantee that all osteotomies were performed similarly (Fig. 1b). After pre-operative planning using the MediCad® software package (Hectec GmbH, Altdorf bei Landshut, Germany), a standardized opening wedge osteotomy of 10 mm was created in all synthetic bones. Three bone-implant-combinations were tested and experiments were run in triplicates. The same surgeon, certified by the German Knee Society, performed each osteosynthesis. After osteosynthesis, the bone models were embedded in a grouting compound with their proximal and distal ends without compromising the osteotomy gap (Ren-Cast® FC 53, Huntsman Advanced Materials GmbH, Basel, Switzerland). Ren-Cast® FC 53 with its high stiffness was used in order to prevent errors by a possible cushioning effect. Then, models were mounted in the versatile material testing system MTS 810® (MTS Systems GmbH, Berlin, Germany) (Fig. 1a). The system is able to generate a maximal force of 50 kN. The load was applied to the tibial plateau through a ball joint, which allowed complete freedom of rotational motion (Fig. 1c). A cylinder attached to a universal joint at the distal end of the tibia allowed frontal- and sagittal-plane rotation but restricted axial rotation. Two lasers (M5L/10®, MEL Mikroelektronik GmbH, Eching, Germany), attached at the medial and lateral sides of the osteotomy gap, measured the motion between the proximal and distal bone segment (Fig. 1a). Data were recorded by a data acquisition system HBM QuantumX® (Hottinger Baldwin Messtechnik GmbH, Darmstadt, Germany). The data from the MTS 810® were analyzed by the digital controller MTS Star IIs® (MTS Systems GmbH, Berlin, Germany).
a Experimental setup with the mounted bone model (asterisk) and the two lasers (right-pointing arrow) for measurement of displacement between the proximal and distal bone segment. Lasers are located on the medial and the lateral side of the osteotomy gap. b Special sawing unit with a solid clamping device (asterisk) for the synthetic bone models. Sawing was guided by a kerf (right-pointing arrow). c Mounting device for guaranteed adjustment of the load axis
Implants
Two different intramedullary nails were compared: Targon TX® (B. Braun Aesculap AG, Tuttlingen, Germany), which is used to stabilize proximal fractures of the tibia and Targon PH® (B. Braun Aesculap AG, Tuttlingen, Germany), which is used to stabilize fractures of the proximal humerus. In spite of different implant designs, the same bone canal entrance points could be used. Tomofix® Medial High Tibial Plate (DePuy Synthes, Zuchwil, Switzerland) was used as the reference device.
Targon TX®
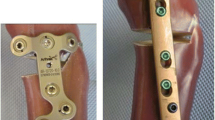
Targon TX® is a titanium intramedullary nail with an anatomically curved shaft, 200 mm long (short version), and with a diameter of 8 mm with multidirectional angle-stable epiphyseal fixation capabilities. For the opening wedge HTO procedure, three proximal screws were inserted monocortically (with the most distal screw inserted just above the osteotomy) and three screws were inserted bicortically through an aiming device distal of the osteotomy (Fig. 2a).
Targon PH®
Targon PH® is a titanium intramedullary nail with a straight shaft, 150-mm long, and with a diameter of 8 mm with four proximal interlocking screws inserted proximal to the osteotomy. Compared to the Targon TX, the two distal transfixation holes are located closer to the distal edge of the osteotomy. Four proximal screws were inserted monocortically and two distal screws were inserted bicortically (Fig. 2b).
Tomofix® medial high tibial plate
Tomofix® medial high tibial plate is a 115-mm-long (standard version) and rigid T-shaped titanium internal fixator with uniaxial locking system. The edges of the plate are rounded to reduce irritation of surrounding tissues. Four proximal screws as well as the most distal screw were inserted monocortically. The three screws directly below to the osteotomy were inserted bicortically (Fig. 2c).
Testing protocols
Two protocols were performed: a multi-step load-controlled fatigue test (I) and a load-to-failure test (II). The continuous load test was used to simulate a post-operative patient, partially weight-bearing (e.g., using crutches). Therefore, axial load was applied for 20,000 cycles at 2 Hz (axial cyclic load), beginning at a loading level of 250 N. Then, cyclic loading was increased to 800 N, simulating a patient of a normal weight of 80 kg. The load was then further increased stepwise to 960, 1120, 1280, 1440, and 1600 N. After the multi-step fatigue test, the load-to-failure test was performed. All of the three synthetic bones, each one of them with a different implant for osteosynthesis (see above), were loaded until fracturing. Stability provided by the implants was defined as the displacement between the bone fragments at different locations (the lateral cortex of the osteotomy, the medial gap of the osteotomy, and the overall motion between the proximal and the distal bone fragment).
Statistics
Statistical analysis was performed with statistical software package SPSS® Version 24 (IBM, Armonk, North Castle, NY, USA). Groups were compared using one-way analysis of variance (ANOVA) followed by Dunn’s post hoc test with Bonferroni correction for multiple testing. Group size was determined by a power calculation using G-Power® (Heinrich-Heine-University of Düsseldorf, Düsseldorf, Germany). Kaplan-Maier curves were generated from survival data of the implants and groups were compared using the Tarone-Ware test, the log-rank test, and the modified Wilcoxon test. A P value of less than 0.05 was considered significant.
Availability of the data and materials
Data are available via the corresponding author.
Results
In summary, 54 measurements were performed. Power calculation with an estimated effect size of 0.6, an alpha level of 0.05, and the power of 0.8 the software recommended to have a total sample size of at least 30 cases.
Mean values of interfragmentary displacement as a parameter for stability of the three different bone-implant-combinations were compared at three locations: the lateral cortex (hinge) of the osteotomy, the medial gap of the osteotomy, and the overall motion between the proximal and the distal bone fragment (Table 1). Overall displacement of the proximal and distal bone fragments was similar between each tested fixation device (Fig. 3a). On the medial osteotomy gap, the Tomofix® implant which stabilizes directly the medial cortex of the tibia showed less displacement and therefore a higher stability than the Targon PH® nail when the bone models were loaded according to test protocol I but did not differ compared to the Targon TX® (Fig. 3b). In contrast, when stability of the lateral hinge was measured, the Targon PH® and the Targon TX® demonstrated a significantly higher stability than the Tomofix® implant (Fig. 3c). Taken together, these results demonstrate that the tibia nail Targon PH® provided the highest stability of all three implants. Only for stability of the medial gap, the Tomofix® implant showed similar results.
Stability measurements of high tibial osteotomy (HTO) performed with Tomofix® (red), Targon PH® (orange), and Targon TX (blue). a Overall displacement of the proximal and distal bone fragments in mm related to continuous load in Newton (N), b displacement of the proximal and distal bone fragments in millimeter on the medial osteotomy gap related to fatigue load range in Newton, and c displacement of the proximal and distal bone fragments in mm on the lateral osteotomy gap related to fatigue load range in Newton
To detect the load that is necessary to fracture the bone models, the load-to-failure test was performed (test protocol II). In all nine models, failure always occurred at the lateral hinge. The failure limit of the Targon TX® long nail was consistently higher compared to the failure limit of the Targon PH® short nail and both nails improved upon the Tomofix® plate fixator (Fig. 4 and Table 2). Taken together, these results demonstrate that the Targon TX® long nail provided a greater prevention against implant failure compared to the Targon PH® and the Tomofix® locking plate.
Discussion
In this study, two intramedullary nails (Targon PH® and Targon TX®) were investigated for stability in opening wedge HTO and compared to the current gold standard, an angle-stable plate fixator (Tomofix®). The current analysis demonstrated that (1) axial cyclic load imitating full weight-bearing up to 800 N was tolerated by all implants without failure, (2) the Targon TX® nail provided the highest fatigue strength when tested for maximum load until failure, and (3) all the tested bone implant constructs failed in fatigue at the lateral cortex.
The experimental setup and protocol were based on the study published by Agneskirchner and colleagues, which compared the static and dynamic fatigue fixation stability provided by four different medial opening wedge HTO plates [8]. The loading of an osteotomized tibia model in a standing patient (800 N) was simulated and well tolerated by all tested implants. However, the authors could not test the vertical tibiofemoral contact force that occurs in slow walking of a patient weighing 80 kg and is represented by a load close to 2400 N [18]. In the current study, we could demonstrate that both intramedullary nails withstood a static load of 2400 N. In contrast, the Tomofix® plate fractured at a load of 1120 N. Comparing medial and lateral movements within the osteotomy, the plate showed a similar (compared to Targon TX®) or higher (compared to Targon PH®) stability for the medial movement, whereas both nails demonstrated higher stability at the lateral cortex. Because failure in all of the bone models occurred at the lateral cortex, this area appears to be the weakest point in an axial cyclic loading on a corrected knee joint line. Therefore, the use of intramedullary nails might be superior in clinical stability compared to the Tomofix® plate.
Comparing plates designed for HTOs with different length, Agneskirchner and colleagues found that also the length of the implant contributed significantly to the stability of the osteosynthesis [8]. In concordance, the longer Targon TX® showed a higher stability during axial cyclic loading and higher resistance to failure than the shorter Targon PH®.
Intramedullary nail devices are a standard of care for the treatment of long bone fractures with a high success rate and safety profile [19]. Previous studies comparing intramedullary and extramedullary fixating devices in tibia fractures have demonstrated that dependent on the individual clinical setting, each system has specific advantages and disadvantages [20, 21]. Intramedullary nailing shows a faster wound healing with reduced local tissue irritation and a lower rate of superficial infections [22, 23]. Fixation with a plate appears to be superior to prevent anterior knee pain and mal-union of the bone segments [24]. In a clinical study, Meena and colleagues compared intramedullary nail systems with proximal plating in extra-articular proximal tibial fractures, a condition very similar to HTO. However, a significant difference in the mal-union rate was not detected [25]. Furthermore, Viberg and colleagues investigated the biomechanical stability of nail fixation systems versus plate fixation systems in complex tibial plateau fractures. They demonstrated that nail fixation and a dual plating technique provided a similar rigid intraarticular stability [26]. Data from the present study suggest that insufficient stability with concordant mal-union of the osteotomy gap appears not to be a relevant problem after implantation of a Targon® TX nail. However, these data are based on an experimental bone model and contributing forces and stabilizers such as muscles and ligaments that significantly affect knee biomechanics were not simulated.
For translational approaches of the current data, it needs to be considered that the angle-stable plate fixator already showed a sufficiently high stiffness and strength in previous clinical studies [9, 27, 28]. So Pape and colleagues compared a spacer plate vs. a plate fixator for HTO. They found a significant micromotion only in the spacer plate group in radiostereometric analysis (RSA) and suggested a shorter delay of weight-bearing following plate fixator fixation compared to a spacer plate [28]. Another prospective, randomized evaluation on early weight-bearing versus partial weight-bearing after opening wedge HTO with an angular locking plate reported an earlier improvement of clinical outcome parameters such as Lequesne, Lysholm, HSS, and IKDC scores for early full weight-bearing [11]. So far, there is no standardized postoperative guideline for HTOs yet. However, in clinical practice, most surgeons recommend a period of protected weight-bearing for the first two to six weeks after surgery [17]. One reason for this recommendation might be that biomechanical studies demonstrated that forces generated by early weight-bearing patients seem to exceed the fatigue strength of an angular locking plate. However, as stated earlier, results from biomechanical testing might not fully reflect the biomechanical conditions that are present in the clinical setting [26]. Furthermore, data of this study is limited by the small number of samples of the tested bone implant models. However, the main objective of this study was not to find an implant with higher stability compared to the current gold standard, but rather to test intramedullary nails as an alternative approach. The use of intramedullary nails might have advantages in reducing post-interventional soft tissue irritation such as the medial collateral ligament and pes anserinus tendons associated with the implantation of an external fixation system in HTO, which is considered by the developers (Tomofix®) too [29]. A reasonable cause of this irritation could have been seen in the tight anatomical relations (ligaments and tendons) at the medial aspect of tibial head (Fig. 5). Nevertheless, this suggestion has not been analyzed in the literature yet. Further research, e.g., with human cadavers including the knee joint in a kinematic analysis, could validate our findings and hypothesis.
Patient suffering from pain according to the Tomofix® Plate underwent a computed tomography with scanner settings: 135 kV, 150 mAS, 2 mm slice thickness, scanner model Toshiba Aquilion RXL®. a Axial plane shows the relation between the plate fixator (asterisk), the tibial bone (t), and tendons of the pes anserinus (pes). b Coronal plane shows the relation between the plate fixator (asterisk), the tibial bone (t), and the medical collateral ligament (mcl)
Irritated tissue is more likely to become infected and causes a delay in wound healing. Infection rates of 4–5% have been reported in opening wedge HTO [30, 31]. A more convenient implant could possibly further reduce the risk of infection. With diligent surgical technique, usually wound healing is not compromised. However, tissue irritation around the implanted plate might still cause significant postoperative pain and a high percentage of patients (40.6%) need revision surgery to remove the plate after consolidation [13]. Therefore, intramedullary nails could prevent the pain related to soft tissue irritation by a prominent subcutaneous plate. Nevertheless, this suggestion was not confirmed in the international literature yet. Unfortunately, postoperative knee pain is a common complication of the use of intramedullary nails in tibial fractures [32,33,34]. Therefore, although intramedullary nails appear to be an interesting option in stabilizing HTO, the risk of postoperative knee pain from intramedullary nails has to be carefully balanced against the benefit of avoiding soft tissue irritation caused by a plate fixation system in the clinical setting.
Completing limitations to the present new fixation option for HTO need of removal of a nail (e.g., total knee arthroplasty) should be considered too. But with a ten year survivorship of HTO frequency of conversion to a total knee arthroplasty is still low after HTO [35, 36]. While plate removal is an easy procedure mostly, nail extraction could be tricky. Nevertheless, there has not been stated a high notable risk according to these implant removals [37,38,39].
Conclusion
In conclusion, the tested intramedullary nails showed a sufficient strength on static and fatigue loading, equivalent to, or in the case of an applied overload, even surpassing the stability of the angle-stable plate fixator. The tibial nail Targon TX® turned out to be a promising fixation device to stabilize an HTO similar to an extra-articular proximal tibial fracture. Further research on clinical application, surgical technique, and biomechanical design of intramedullary nails is necessary to test this promising new surgical approach for opening wedge HTO. In particular, the anatomical relation between different fixation devices and soft tissue like ligaments or tendons should be a subject of further research such as human cadaver studies.
Abbreviations
- HSS:
-
Hospital for special surgery
- HTO:
-
High tibial osteotomy
- IKDC:
-
International Knee Documentation Committee
- NSAID:
-
Nonsteroidal anti-inflammatory drugs
References
WHO Department of Chronic Diseases and Health Promotion (2017). http://www.who.int/chp/topics/rheumatic/en. Accessed September 30, 2017
Covinsky KE, Lindquist K, Dunlop DD, Gill TM, Yelin E (2008) Effect of arthritis in middle age on older-age functioning. J Am Geriatr Soc 56(1):23–28
McDonough CM, Jette AM (2010) The contribution of osteoarthritis to functional limitations and disability. Clin Geriatr Med 26(3):387–399
Sutton PM, Holloway ES (2013) The young osteoarthritic knee: dilemmas in management. BMC Med. https://doi.org/10.1186/1741-7015-11-14
Steinhaus ME, Christ AB, Cross MB (2017) Total knee arthroplasty for knee osteoarthritis: support for a foregone conclusion? HSS J 13(2):207–210
Julin J, Jämsen E, Puolakka T, Konttinen YT, Moilanen T (2010) Younger age increases the risk of early prosthesis failure following primary total knee replacement for osteoarthritis. A follow-up study of 32,019 total knee replacements in the Finnish Arthroplasty Register. Acta Orthop 81(4):413–419
Floerkemeier D, Staubli AE, Schroeter D, Goldhahn S, Lobenhoffer P (2013) Outcome after high tibial open-wedge osteotomy: a retrospective evaluation of 533 patients. Knee Surg Sports Traumatol Arthrosc 21(19):170–180
Agneskirchner JD, Freiling D, Hurschler C, Lobenhoffer P (2006) Primary stability of four different implants for opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 14(3):291–300
Petersen W, Wall A, Paulin T, Park HU, Heymann L (2014) Stability of two angular stable locking plates for open wedge high tibial osteotomy (HTO): Tomofix versus LOQTEQ HTO Plate. Arch Orthop Trauma Surg 2014;134(10):1437–1442
Brinkman JM, Luites JWH, Wymenga AB, van Heerwaarden RJ (2010) Early full weight bearing is safe in open-wedge high tibial osteotomy. Acta Orthop 81(2):193–198
Schröter S, Ateschrang A, Löwe W, Nakayama H, Stöckle U, Ihle C (2017) Early full weight-bearing versus 6-week partial weight-bearing after open wedge high tibial osteotomy leads to earlier improvement of the clinical results: a prospective, randomised evaluation. Knee Surg Sports Traumatol Arthrosc 25(1):325–332
Seo SS, Kim OG, Seo JH, Kim DH, Kim YG, Lee IS (2016) Complications and short-term outcomes of medial opening wedge high tibial osteotomy using a locking plate for medial osteoarthritis of the knee. Knee Surg Relat Res 28(4):289–296
Niemeyer P, Schmal H, Hauschild O, von Heyden J, Südkamp NP, Köstler W (2010) Open-wedge osteotomy using an internal plate fixator in patients with medial-compartment gonarthritis and varus malalignment: 3-year results with regard to preoperative arthroscopic and radiographic findings. Arthroscopy 26(12):1607–1616
Cristofolini L, Viceconti M (2000) Mechanical validation of whole bone composite tibia models. J Biomech 33(3):279–288
Heiner AD, Brown TD (2001) Structural properties of a new design of composite replicate femurs and tibias. J Biomech 34(6):773–781
Fujisawa Y, Masuhara K, Shiomi S (1979) The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am 10(3):585–608
Galla M, Lobenhoffer P, Staubli AE (2008) High-tibial open-wedge valgization osteotomy with plate fixator. In: Lobenhoffer P, van Heerwarden RJ, Jakob RP, Galla M, Agneskirchner JD (ed) Osteotomies around the knee. AO Foundation Publishing, Davos, pp 87–104
Taylor WR, Heller MO, Bergmann G, Duda GN (2004) Tibio-femoral loading during human gait and stair climbing. J Orthop Res 22(3):625–632
Zelle BA, Boni G (2015) Safe surgical technique: intramedullary nail fixation of tibial shaft fractures. Patient Saf Surg. https://doi.org/10.1186/s13037-015-0086-1
Kurylo JC, Tornetta P (2013) Extra-articular proximal tibial fractures: nail or plate? Instr Course Lect 62:61–77
Mao Z, Wang G, Zhang L, Zhang L, Chen S, Du H, Zhao Y, Tang P (2015) Intramedullary nailing versus plating for distal tibia fractures without articular involvement: a meta-analysis. J Orthop Surg Res. https://doi.org/10.1186/s13018-015-0217-5
Im GI, Tae SK (2005) Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate an screws fixation. J Trauma 59(5):1219–1223
Xue XH, Yan SG, Cai XZ, Shi MM, Lin T (2014) Intramedullary nailing versus plating for extra-articular distal tibial metaphyseal fracture: a systematic review and meta-analysis. Injury 45(4):667–676
Polat A, Kose O, Canbora K, Yanık S, Guler F (2015) Intramedullary nailing versus minimally invasive plate osteosynthesis for distal extra-articular tibial fractures: a prospective randomized clinical trial. J Orthop Sci 20(4):695–701
Meena RC, Meena UK, Gupta GL, Gahlot N, Gaba S (2015) Intramedullary nailing versus proximal plating in the management of closed extra-articular proximal tibial fracture: a randomized controlled trial. J Orthop Traumatol 16(3):203–208
Viberg B, Rasmussen KMV, Overgaard S, Roogmark C (2017) Poor relation between biomechanical and clinical studies for the proximal femoral locking compression plate. Acta Ortthop 88(4):427–433
Watanabe K, Kamiya T, Suzuki D, Otsubo H, Teramoto A, Suzuki T, Yamashita T (2014) Biomechanical stability of open-wedge high tibial osteotomy: comparison of two locking plates. J Orthop 4:257–262
Pape D, Kohn D, van Giffen N, Hoffmann A, Seil R, Lorbach O (2013) Differences in fixation stability between spacer plate and plate fixator following high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):82–89. https://doi.org/10.1007/s00167-011-1693-8
Galla M, Lobenhoffer P, Staubli AE (2008) High-tibial open-wedge valgization osteotomy with plate fixator. In: Lobenhoffer P, van Heerwarden RJ, Jakob RP, Galla M, Agneskirchner JD (eds) Osteotomies around the knee. AO Foundation Publishing, Davos, p 98
De Mello Junior WA, Arruda LR, Coluccini AM, da Silva Nunes RP, Pedro Mdo A, de Souza MR, Zabeu JL (2015) Complications following medial opening wedge osteotomy of the knee: retrospective study. Rev Bras Ortop 46(1):64–68
Spahn G (2004) Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg 124(10):649–653
Katsoulis E, Court-Brown C, Giannoudis PV (2006) Incidence and aetiology of anterior knee pain after intramedullary nailing of the femur and tibia. J Bone Joint Surg Br 88(5):567–580
Labronici PJ, Pires RES, Franco JS, Fernandes HJA, dos Reis FB (2011) Recommendations for avoiding knee pain after intramedullary nailing of tibial shaft fractures. Patient Saf Surg. https://doi.org/10.1186/1754-9493-5-31
Avilucea FR, Sathiyakumar V, Greenberg SE, Ghiam M, Thakore RV, Francois E, Benvenuti MA, Siuta M, Smith AK, Ehrenfeld JM, Evans JM, Obremskey WT, Sethi MK (2016) Open distal tibial shaft fractures: a retrospective comparison of medial plate versus nail fixation. Eur J Trauma Emerg Surg 42(1):101–106. https://doi.org/10.1007/s00068-015-0519-7
Ruangsomboon P, Chareancholvanich K, Harnroongroj T, Pornrattanamaneewong C (2017) Survivorship of medial opening wedge high tibial osteotomy in the elderly: two to ten years of follow up. Int Orthop 41(10):2045–2052. https://doi.org/10.1007/s00264-017-3517-z
Kim JH, Kim HJ, Lee DH (2017) Survival of opening versus closing wedge high tibial osteotomy: a meta-analysis. Sci Rep 7(1):7296. https://doi.org/10.1038/s41598-017-07856-8
Reith G, Schmitz-Greven V, Hensel KO, Schneider MM, Tinschmann T, Bouillon B, Probst C (2015) Metal implant removal: benefits and drawbacks—a patient survey. BMC Surg 15:96. https://doi.org/10.1186/s12893-015-0081-6
Sidky A, Buckley RE (2008) Hardware removal after tibial fracture has healed. Can J Surg 51(4):263–268
Minkowitz RB, Bhadsavle S, Walsh M, Egol KA (2007) Removal of painful orthopaedic implants after fracture union. J Bone Joint Surg Am 89(9):1906–1912
Acknowledgements
Dr. Graw is participant in the BIH-Charité Clinician Scientist Program funded by the Charité – Universitätsmedizin Berlin and the Berlin Institute of Health.
We thank Mrs. Monica Kosiol (Monash University of Melbourne) for language editing and proofreading of the manuscript.
Funding
This study received funding from the Gesellschaft für Prävention und Rehabilitation im Sport e.V.
Author information
Authors and Affiliations
Contributions
DK, AP, ML, and RB conceived and designed the experiments. MH, GD, WR, AP, AO, HJC, and CPF performed the experiments. RB, JAG, and DK analyzed the data. CS performed the statistical analysis. RB, JAG, AP, ML, and DK wrote the paper. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Rights and permissions
About this article
Cite this article
Burchard, R., Katerla, D., Hammer, M. et al. Intramedullary nailing in opening wedge high tibial osteotomy—in vitro test for validation of a method of fixation. International Orthopaedics (SICOT) 42, 1835–1843 (2018). https://doi.org/10.1007/s00264-018-3790-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3790-5