Abstract
Purpose
We investigated the various impingement angles (including both bony and prosthetic impingement) and impingement types that can occur after THA, even when the same combined anteversion parameter is used. We also investigated the relationship between impingement angle and acetabular morphology or femoral anteversion.
Methods
We evaluated 83 patients with no hip arthritis. We divided them into six groups according to acetabular CE angle (≤15°, >15–≤25°, and >25°) and femoral anteversion (≤20° and >20°). Using three-dimensional templating software, we changed stem and cup anteversion to satisfy a combined anteversion (CA) of 50° in each hip (stem anteversion + cup anteversion = 50°) and investigated the resulting impingement angles.
Results
Even with the same CA, differences in impingement angle occurred: 18.3° ± 7.2° with flexion, 30.2° ± 9.7° with internal rotation at 90° flexion, 20.2° ± 12.5° with extension, and 26.2° ± 7.8° with external rotation. As stem anteversion increased, the impingement type changed from prosthetic impingement to bony impingement in flexion and internal rotation and from bony impingement to prosthetic impingement in extension and external rotation. The flexion angle and internal rotation angle at 90° flexion increased (p < 0.016) as CE angle decreased. There were no significant differences between high and low femoral anteversion.
Conclusions
Combined anteversion theory should be used with care because of large differences in impingement angles. A stem anteversion of 30° and cup anteversion of 20° appear to be ideal for obtaining a larger impingement angle under this condition.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Dislocation is one of the major complications that can occur following total hip arthroplasty (THA) [1]. To reduce the dislocation rate, a number of reports have suggested a safe zone of cup orientation [2,3,4]. Recently, variations on the “combined anteversion (CA) theory” have been established. The most well-known of these was proposed by Widmer et al. [5]. Others, including Masaoka et al. [6] and Nakashima et al. [7], recommend a CA of 40–60°. However, combined anteversion has not yet been studied in sufficient detail. For example, the Widmer et al. study [5] considered only prosthetic impingement, but in clinical practice there are many cases in which bony impingement can cause earlier problems [8, 9]. Bartz et al. [10] described three different dislocation mechanisms: prosthetic impingement, bony impingement, and spontaneous dislocation. Thus, in clinical practice, we should consider both prosthetic and bony impingement when describing the range of motion after THA. In addition, various stem and cup anteversion parameters can be combined to result in the same CA. When stem anteversion changes, the relationship between the femur and pelvis changes, and the impingement angle may thus also change. Femoral antetorsion and acetabular morphology also may influence the impingement angle.
In this study, we sought to answer the following questions. When the requirement for the same CA (stem anteversion + cup anteversion = 50°) is satisfied:
-
(1)
How does the impingement angle (including bony and prosthetic impingement) change?
-
(2)
Which impingement type occurs first?
-
(3)
Do differences in the acetabular morphology (based on the center-edge [CE] angle) affect the change in impingement angle?
-
(4)
Do differences in femoral antetorsion affect the change in impingement angle?
Materials and methods
Study design
This was a case-control study.
Methods and measurements
Patients
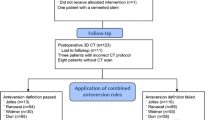
This study included patients who had undergone primary THA or who had been diagnosed with developmental dysplasia of the hip at our hospital between 2012 and 2015. Bilateral osteoarthritis cases, patients with insufficient data, and patients with inappropriate images were excluded based on pre-operative computed tomography (CT) (Fig. 1). We chose the other side with no arthritis change. For this study we reviewed data from 83 patients (83 hips) without osteoarthritis changes, including 16 men and 67 women. The mean age was 59.3 ± 13.1 years (16–86 years) (Table 1). We divided the patients into three groups according to the center-edge (CE) angle (CE ≤15°, 15° < CE ≤ 25°, and CE >25°) [11]. We also divided them into two groups according to femoral anteversion (≤20° and >20°) [12]. Thus, the 83 patients were divided into six groups. The number of patients in each group is shown in Table 2. Information for each group divided according to CE angle and femoral anteversion is shown in Tables 3 and 4, respectively.
Anatomical model and reference planes
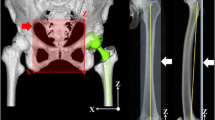
For each subject we constructed separate three-dimensional models of the pelvis and femur from CT images (LightSpeed VCT Series/Discovery CT750; GE Healthcare, Tokyo, Japan). All imaging data were transferred to a CT-based three-dimensional templating system (Zed Hip™ Lexi Co., Ltd., Tokyo, Japan). Zed Hip can investigate different impingement types, including bone-to-bone, bone-to-prosthetic, and prosthetic-to-prosthetic.
For all measurements and simulations, we defined the coordinate system of the pelvis relative to the anterior pelvic plane (APP). On the APP, the x-axis was defined by a line connecting the right and left anterior superior iliac spines. The z-axis was defined as a line passing through the pubic symphysis in the APP perpendicular to the x-axis. The y-axis was defined by a horizontal line passing through the middle point of the right and left anterior superior iliac spines perpendicular to the APP (Fig. 2a). The coordinate system for the femur was defined relative to the posterior condylar plane of the femur, which was formed by the proximal posterior surface, lateral condyle, and medial condyle. The point of origin of the plane was defined by projecting a point from the trochanteric fossa onto the posterior condylar plane. The z-axis was defined as a projected line onto the posterior condylar plane, passing through the knee centre and trochanteric fossa. The x-axis was defined by a projected line onto the posterior condylar plane and perpendicular to the z-axis. The y-axis was defined by a line perpendicular to the posterior condylar plane and bisecting the x-axis (Fig. 2b).
a and b Definitions for the axes in the anterior plane of the pelvis and the posterior condylar plane. (a) Axes in the anterior plane of the pelvis. The XZ plane is shown on the left, and the XY plane on the right. In the left panel, the x-axis is defined by a line connecting the right and left anterior superior iliac spines, and the z-axis by a line passing through the pubic symphysis in the anterior plane of the pelvis, perpendicular to the x-axis. In the right panel, the y-axis is defined by a horizontal line passing through the pubic symphysis perpendicular to the anterior plane of the pelvis. (b) Axes in the posterior condylar plane. The XZ plane is shown on the left, where the x-axis is defined as a line connecting the posterior surface of the lateral and medial condyles parallel to the posterior condylar plane, and the z-axis is defined by a line projected onto the posterior condylar plane that bisects the x-axis and passes along the midline of the knee and the trochanteric fossa. The YZ plane is shown on the right, with the y-axis defined by a line perpendicular to the posterior condylar plane and bisecting the z-axis. c and d Definitions for the range of motion used for the simulation analysis. (c) Flexion/extension, with 0° hip flexion on the left and 90° hip flexion on the right. (d) Internal rotation/external rotation, with the 0° internal hip rotation on the left and 30° internal hip rotation on the right
Definition of hip range of motion
The definition of hip range of motion is shown in Fig. 2c and d. The angle of hip flexion/extension along the sagittal plane of motion was defined as the angle between the APP and the z-axis on the posterior condylar plane (Fig. 2c). The angle of hip internal/external rotation was defined as the angle between the APP and the x-axis on the posterior condylar plane (Fig. 2d).
Impingement angle
Impingement angle was defined as the largest angle achieved before impingement occurred, which could be bone-to-bone, bone-to-prosthetic, or prosthetic-to-prosthetic.
Implant type and positioning
For our simulations, the Zimmer Biomet THA system was used (Zimmer Biomet, Warsaw, IN, USA). We chose a Continuum Shell, which was of a suitable size in each case, with a cup diameter that was approximately 6 mm larger than the femoral head diameter and a 32-mm flat liner. We selected the Wagner Cone Prosthesis (125°), which was of a suitable size in each case; the osteotomy level was fixed at a position 15 mm proximal from the apex of the lesser trochanter. A ceramic head with a 32-mm diameter was used in all cases. According to some registries, a 32-mm head is the most common [13, 14]. We placed the cup in contact with the outer wall of the tear drop, at the same height as the original femoral head. The radiographic inclination angle was fixed at 40° to the APP. Radiographic anteversion was varied from 0° to 50° to the APP. After placing the cup, we placed the stem, making leg length, position of the great trochanter, and position of the centre of the head the same as those in the original by changing the neck length and the depth of penetration of the stem. This position was defined as the reference point.
The anteversion orientation of the stem was defined by the angle between the posterior condylar plane and the reference plane of the stem. We changed stem and cup anteversion so as to satisfy the requirement for a CA of 50° (stem anteversion + cup anteversion = 50°). Stem anteversion was varied from 0° to 50°.
Measurements
We investigated the impingement angle, including bony and prosthetic impingement, in each case based on the flexion angle, internal rotation angle with 90° flexion, extension, and external rotation.
Statistical analysis
All data were expressed as means ± standard deviation (SD), and differences were analyzed using statistical software (SPSS version 23). Patients were divided into three groups according to CE angle. An analysis of variance was used to determine significant differences (p < 0.05) among the three groups. When there were significant differences, three pairwise t-tests were used to determine whether there was a significant difference (p < 0.016) between two groups. Patients were then divided into two groups according to femoral antetorsion. First, the F-test was used to investigate the state of dispersion. Second, the Student t-test was used to determine significant differences (p < 0.05).
Informed consent was obtained from all individual participants included in the study, and the study was approved by the Institutional Review Board of our university.
Results
#1
Results for changes in the impingement angle are shown in Fig. 3. The flexion angle increased significantly as stem anteversion increased from 0° to 30° (p < 0.001). However, when stem anteversion was ≥40°, the flexion angle decreased significantly (p < 0.001). The mean difference between the maximum and minimum angle was 18.3° ± 7.2° (8–40°) (Fig. 3a). The internal rotation angle at 90° flexion increased significantly as stem anteversion increased from 0° to 40° (p < 0.001), but when stem anteversion was >40°, the internal rotation angle did not change (p > 0.05). The mean difference between the maximum and minimum angles was 30.2° ± 9.7° (13–65°) (Fig. 3b). The extension angle increased significantly as stem anteversion increased from 0° to 30° (p < 0.001), and decreased significantly (p < 0.001) when stem anteversion was >40°. The mean difference between the maximum and minimum angle was 20.2° ± 12.5° (6–50°) (Fig. 3c). The external rotation angle increased significantly as stem anteversion increased from 0° to 30° (p < 0.001) then decreased significantly (p < 0.001) when stem anteversion was >30°. The mean difference between the maximum and minimum angle was 26.2° ± 7.8° (15–51°) (Fig. 3d).
#2
Table 5 shows changes based on impingement type (bone-to-prosthetic impingement was included in bony impingement). With respect to the flexion angle and internal rotation angle with 90° flexion, bony impingement occurred before prosthetic impingement when stem anteversion was ≤30°, and the ratio of prosthetic impingement increased when stem anteversion was >30°. In contrast, with respect to the extension and external rotation angles, prosthetic impingement occurred before bony impingement when stem anteversion was ≤20°, and the ratio of bony impingement increased when stem anteversion was >30°.
#3
Differences in impingement angles by acetabular morphology (CE angle) are shown in Fig. 4. When stem anteversion varied from 0° to 30°, the flexion angle increased significantly as the CE angle decreased (p < 0.016). When stem anteversion was 50°, there were no significant differences among the three groups (p > 0.016) (Fig. 4a). When stem anteversion varied from 0° to 30°, the internal rotation angle at 90° flexion increased significantly as the CE angle decreased (p < 0.016). When stem anteversion was ≥40°, there were no significant differences among the three groups (p > 0.016) (Fig. 4b). Neither the extension angle nor the external rotation angle differed significantly among the three groups at any stem anteversion angle (p < 0.016) (Fig. 4c and d).
#4
Differences in impingement angle by femoral antetorsion are shown in Fig. 5. The flexion, internal rotation at 90° flexion, and extension angles were not significantly different at any stem anteversion angle (Fig. 5a–c). Although the external rotation angles were significantly different when stem anteversion was 0°, 10°, and 20°, these differences were only 1–2° (Fig. 5d).
Discussion
Although the combined anteversion (CA) theory is used widely throughout the world, there have been no reports describing differences caused by various combinations of stem and cup anteversion. This was the first study to assess combined anteversion in detail. Moreover, this report also describes the relationship between impingement angle and the pelvic/femoral form.
The study had three limitations. First, we performed simulations using only one pattern of CA angle (i.e., 50°). We would likely have obtained additional differences if we had used different CA patterns. For example, Ranawat et al. [15] and Dorr et al. [16] recommended a smaller CA angle than that in our setting (CA of 50°). On the other hand, Jolles et al. [17] indicated that the dislocation risk was 6.9-fold higher if the total anteversion was not between 40° and 60°. Moreover, recently Nakashima et al. [7] and Fujishiro et al. [18] indicated that CA angles between 40° and 60°, as evaluated on CT, significantly reduced dislocations. Thus, as noted, it is possible that there would be differences using another CA angle. However, we are confident that a CA of 50° is suitable. Second, we did not consider soft tissue, which in clinical practice decreases the impingement angle. Third, we did not consider the state after impingement. In clinical practice, dislocation occurs after the head leaves the cup. In other words, we could not consider the jumping distance.
In this study, even with the same CA (cup anteversion + stem anteversion = 50°), there were differences in impingement angles. These differences were about 18° with flexion, 30° with internal rotation, 20° with extension, and 26° with external rotation. A change in stem anteversion led to changes in the femur’s neutral position. Regarding flexion and internal rotation angles, the impingement angle were expected to increase as stem anteversion increased. In contrast, extension and external rotation angles were expected to decrease as stem anteversion increased. However, because CA was kept at 50°, cup anteversion decreased as stem anteversion increased. With regard to flexion angle and internal rotation angle, bony impingement occurred before prosthetic impingement when stem anteversion was ≤30°, and the ratio of prosthetic impingement increased when stem anteversion was >30°. These changes were caused by increased ratios in which the cup hung over the acetabulum edge. The impingement angle decreased considerably after prosthetic impingement occurred. On the other hand, with respect to the extension angle and external rotation angle, prosthetic impingement occurred before bony impingement when stem anteversion was ≤20°, and the ratio of bony impingement increased when stem anteversion was >30°. The impingement angle decreased considerably after bony impingement occurred. When stem anteversion was 50°, the ratio of bony impingement was 50/83 during extension and 76/83 during external rotation. There was a high rate of bony impingement during external rotation.
This study described the angle to the point where the impingement occurred, including both bony and prosthetic impingement. In terms of the difference in the CE angle, the flexion angle and internal rotation angle at 90° flexion were significantly different when stem anteversion was ≤30°. As noted above, the main type of impingement angle when stem anteversion was ≤30° was bony impingement. Clearly, pelvic morphology is an important factor when determining the bony impingement point. The flexion angle and internal rotation angle at 90° flexion increased by about 5° as the CE angle decreased by about 10°. In contrast, with respect to the extension angle and external rotation angle, prosthetic impingement occurred before bony impingement when stem anteversion was <30°, and the ratio of bony impingement increased when stem anteversion was ≥30°. In terms of extension and external rotation angle, although the impingement angle tended to be larger as the CE angle decreased when stem anteversion was ≥40°, these differences were not significant (p > 0.016). Bony impingement decreased the impingement angle considerably, while non-bony impingement increased the impingement angle. We clarified that the impingement angle increases when the CE angle is small, in other words, when dysplasia of the acetabulum is severe. Shoji et al. [19] and Iftach et al. [20] showed that the bony impingement angle increases when the length from the centre of the femur to the antero-inferior iliac spine (AIIS) is shorter. The impingement angle after THA depends on the original pelvic morphology as well as the position of the prosthetics.
We expected that the impingement angle would change as the position between the pelvis and femur changed when femoral antetorsion was varied. Shoji et al. [21] showed that low femoral anteversion is a risk factor for bony impingement after bipolar hemiarthroplasty (BHA). However, we found no significant differences except for the external rotation angle, and even in external rotation there was a difference of only 1–2°. This result is because prosthetic impingement must be considered in THA, unlike in BHA. As a result, the original femoral anteversion does not affect the impingement angle after THA.
Conclusion
Care should be taken when determining the prosthetic orientation based on combined anteversion theory because impingement angle can have large differences even when the conditions for the same CA are satisfied. A stem anteversion of 30° and a cup anteversion of 20° appear to be the ideal conditions for obtaining a larger impingement angle while satisfying the requirement for a CA of 50°. Our study also showed that the impingement angle is dependent on morphology and tends to be larger as CE angle decreases. In contrast, the original femoral anteversion has little effect on the impingement angle.
References
Grinten M, Verhaar JAN (2003) Dislocation of total hip prostheses: risk factors and treatment. Ned Tijdschr Gen 147:286–290
Coventry MB (1985) Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am 67:832–841
Harris WH (1980) Advances in surgical technique for total hip replacement: without and with osteotomy of the greater trochanter. Clin Orthop Relat Res 146:188–204
Lewinnek GE, Lewis JL, Tarr R et al (1978) Dislocations after total hip replacement arthroplasties. J Bone Joint Surg Am 60:217–220
Widmer KH, Zurfluh B (2004) Compliant positioning of total hip components for optimal range of motion. J Orthop Res 22:815–821
Masaoka T, Yamamoto K, Shishido T et al (2006) Study of hip joint dislocation after total hip arthroplasty. Int Orthop 30:26–30
Nakashima Y, Hirata M, Akiyama M et al (2014) Combined anteversion technique reduced the dislocation in cementless total hip arthroplasty. Int Orthop 38:27–32
Kessler O, Patil S, Wirth S et al (2008) Bony impingement affects range of motion after total hip arthroplasty: A subject-specific approach. J Orthop Res 26:443–452
Suzuki K, Matsubara M, Morita S et al (2002) CT image evaluation of the internal rotation limit prior to bony impingement after total hip arthroplasty. J Orthop Sci 7:433–438
Bartz RL, Nobel PC, Kadakia NR et al (2000) The effect of femoral component head size on posterior dislocation of the artificial hip joint. J Bone Joint Surg Am 82:1300–1307
Inoue K, Wicart P, Kawasaki T et al (2000) Prevalence of hip osteoarthritis and acetabular dysplasia in french and japanese adults. Rheumatology 39:745–748
Sugano N, Noble PC, Kamaric E et al (1998) The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br 80:711–719
Australian Registry (2016) Australian Orthopaedic Association National Joint Replacement Registry annual report 2016. https://aoanjrr.sahmri.com/annual-reports-2016. Accessed 02 October 2017
The New Zealand Joint Registry (2016) New Zealand Orthopaedic Association 17 year report. https://nzoa.org.nz/nz-joint-registry. Accessed 02 October 2017
Ranawat CS, Maynard MJ (1991) Modern techniques of cemented total hip arthroplasty. Tech Orthop 6:17–25
Dorr LD, Malik A, Dastane M et al (2009) Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res 467:119–127
Jolles BM, Zangger P, Leyvraz PF (2002) Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplast 17:282–288
Fujishiro T, Hiranaka T, Hashimoto S et al (2016) The effect of acetabular and femoral component version on dislocation in primary total hip arthroplasty. Int Orthop 40:697–702
Shoji T, Yasunaga Y, Yamasaki T et al (2013) Bony impingement depends on the bone morphology of the hip after total hip arthroplasty. Int Orthop 37:1897–1903
Iftach H, Lazaros P, Asheesh B et al (2013) Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res 471:2497–2503
Shoji T, Yasunaga Y, Yamasaki T et al (2015) Low femoral antetorsion as a risk factor for bony impingement after bipolar hemiarthroplasty. J Orthop Surg Res. https://doi.org/10.1186/s13018-015-0248-y. Accessed 02 October 2017
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ohmori, T., Kabata, T., Kajino, Y. et al. Differences in range of motion with the same combined anteversion after total hip arthroplasty. International Orthopaedics (SICOT) 42, 1021–1028 (2018). https://doi.org/10.1007/s00264-017-3653-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3653-5