Abstract
Purpose
Management of segmental rim defects and bone mineral density (BMD) loss in the elderly prior to total hip replacement is unclear within classification systems for acetabular bone loss. In this study, our objectives were (1) to understand how a reduction in BMD in the elderly affects the oversizing of a press-fit cup for primary fixation and (2) to evaluate whether the location of the segmental defect affected cup fixation.
Methods
A finite element (FE) model was used to simulate and evaluate cup insertion and fixation in the context of segmental rim defects. We focused on the distribution of patients over age 70 and used BMD (estimated from CT) as a proxy for aging’s implications on THR and used probabilistic FE analysis to understand how BMD loss affects oversizing of a press-fit cup.
Results
A cup oversized by 1.10 ± 0.28 mm provides sufficient fixation and lower stresses at the cup-bone interface for elderly patients. Defects in the anterior column and posterior column both required the same mean insertion force for cup seating of 84% (taken as an average of 2 anterior column and 2 posterior column defects) compared to the control configuration, which was 5% greater than the insertion force for a superior rim defect and 12% greater than the insertion force for an inferior rim defect.
Conclusions
A defect along the superior or inferior rim had a minimal effect on cup fixation, while a defect in the columns created cup instability and increased stress at the defect location.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip replacement (THR) is one of the most commonly performed orthopaedic procedures to improve the mobility and relieve pain at the hip in patients suffering from osteoarthritis of the hip [1]. Approximately 10% of patients with THRs have complications ten to 15 years after the procedure and often require revision arthroplasty [2]. When the prosthesis fails, it is often accompanied by significant acetabular bone deficiency that was not augmented prior to primary THR or developed after arthroplasty [3]. Thus, it is necessary for the orthopaedic surgeon to evaluate and understand how acetabular deficiency may compromise cup fixation to reduce the risk of revision.
Current classification systems, Paprosky and the American Academy of Orthopaedic Surgeons (AAOS), are used by most orthopaedic surgeons to assess the bone stock of the acetabulum for primary or revision THR. In case of extensive bone loss following acetabular revision such as acetabular defects classified as Paprosky type 3A, several effective approaches have been cited in the literature. These approaches vary significantly based on the study and include elliptical trabecular metal cups and trans-acetabular screws [4], modular ring system MRS-Titan combined with acetabular defect reconstruction [5], and cementless trabecular titanium acetabular modular implants [6].
In the presence of a segmental acetabular defect, classified as Paprosky type I defects, whether the ‘gold standard’ press-fit cup can provide sufficient fixation is unclear [7]. It is well understood that under-reaming, cup design (such as circumferential rims) [8], and screw fixation can be valuable in providing both mechanical stability and biological fixation in both primary and revision arthroplasty. However, determining an ideal surgical approach for a specific patient is not a precise science. Unsurprisingly, management of hip fractures in osteoporotic patients can prove to be a difficult task. D’Imporzano et al. have reported that since osteoporotic patients have more acetabular fragility fractures, dedicated implants should be implemented [9]. It is truly important to understand the ideal treatment of elderly patients with fractures or initiation of fractures.
Factors that influence the cup fixation are numerous and have proven to be indicative of successful outcomes with THR [10–12]. Factors such as age-related bone loss of the pelvis [13] and size and location of acetabular defect [12] have been identified as important components in determining cup fixation and stability; however, management of these factors is not entirely clear.
In the past decade, finite element (FE) analysis has been applied with great success in orthopaedics to analyze problems such as implant design, bone remodeling, fracture healing, and the interactions at the bone–implant interface. This paper highlights further how probabilistic FE analysis can potentially help surgeons develop guidelines for under-reaming in THA specific to certain age groups with acetabulum rim defects.
In this study, our objective was to first understand how a reduction in pelvic bone mineral density (BMD) in the elderly affects the ideal oversizing of the endoprosthesis for primary fixation. We then evaluated whether the location of the segmental defect affected cup fixation. Our aim is to shed light on how segmental rim defects and pelvic BMD loss should be managed in the elderly to provide a better cup fixation.
Material and methods
Probabilistic finite element analysis
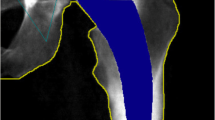
A FE model of the pelvis, previously validated in our laboratory [11, 14–16], was used to determine the optimum under-reaming for elderly patients. To develop our FE model, we used a metal alloy cup (Ti-6Al-4V) with a diameter of 58 mm that matched previous in vitro cadaveric studies [14, 15].
After the 3D bone surface was extracted, the model was then imported into the 3-Matic software package (Materialise, Leuven, Belgium), and a FE mesh of the pelvis was generated. We evaluated the Young’s modulus for every element of mesh using a power relationship developed by Keller et al. [17] for both trabecular and cortical bone. We imposed a Poisson ratio of 0.3 and Young’s modulus value of 17 GPa for the largest Hounsfield unit (HU) from the CT scan, which was in range with values obtained by Taddei et al. for the femur [18]. The development of the FE model along with the final inhomogeneous 3D reconstruction of the pelvis is shown in Fig. 1.
Based on previously established methodology [19], we divided the acetabular body into three clinically relevant zones (shown in Fig. 2) where loosening of the endo-prosthesis can occur. All CT data was obtained from a unique study performed by Wodzislawski et al. [19] which is most relevant to this study. The frequency distributions for each zone are shown in Fig. 2. We focused on the distribution in patients over age 70 since these patients are the largest demographic for THR and used BMD as a proxy for aging’s implications on THR. We assessed the normality of the CT data measured by Wodzislawkski et al. by performing a Shapiro–Wilk’s test. The critical value for the Shapiro-Wilk’s test at a 0.05 significance level for nine samples is 0.829. Since our test statistic W was 0.955, 0.932, and 0.963 for zones I, II, and III, respectively, we found that the data was normally distributed. Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA) was used for all statistical analysis.
Pelvis is divided into three clinically relevant zones in the frontal and diagonal planes where failure of the endoprosthesis may arise. Average bone density in each zone is measured via CT within the frontal plane for patients over age 70 prior to THR to generate a normal distribution of each zone for probabilistic finite element analysis. Monte Carlo Simulation solved for the optimum under-reaming of 100 configurations by randomly sampling from each zone’s bone density distribution
The model was imported into ANSYS 13.0 (Ansys Inc., Canonsburg, PA, USA), and a simulation was performed using probabilistic FE analysis. The Monte Carlo simulation solved the model by randomly sampling from the range of bone densities given by the distributions in each of the three zones [19]. We solved for the optimum reaming diameter for 100 configurations to obtain a stable cup bone interface, defined by the percentage of surface contact, amount of micromotion, and von Mises stress distribution. A frequency distribution of the optimum under-reaming diameters was generated and assessed for normality using the Shapiro-Wilk test. We applied a 1600 N load that simulates one leg stance during fast walking to compute the von Mises stress distribution and contact surface area. The model of the acetabular cup was inserted with a 15 degree anteversion and 45 degree inclination. We computed the contact surface area and insertion force required to ensure seating, which was measured as the percent of rebound of the cup upon insertion. The technical details of the biomechanical validation and processing of the osseous FE model have previously been published [14, 15].
Finite element analysis of segmental acetabular defects
The defects along the acetabular rim were generated to fit the AAOS classification of minor type I segmental defects. A summary of how the FE model was generated in comparison to previously validated in vitro experiments is shown in Fig. 3. Using a U-shaped profile we created six defects by rotating the volume 60 degrees around the plane of the acetabular rim. The parametric volume, which was 20 mm in depth and width, was subtracted from the intact reconstructed pelvis. The defects were rounded at the edges to avoid false stress concentrations. The mean and standard deviation of the Young’s modulus for the bone removed to create each defect was calculated and compared using a 2-tailed Student t test. The acetabular cup position was identical to that described for the probabilistic finite element analysis. We then applied a 1600 N load that simulates one leg stance during fast walking to compute the von Mises stress distribution and contact surface area.
(1) FE model was previously validated by performing in vitro studies where a segmental defect was created along the superior rim of the acetabulum. CT scan of the pelvis was performed and imported into MIMICS, and the defect was created using a Boolean subtraction between the 3D model and the CAD volume. (2) Cementless press-fit acetabular cup was inserted into the acetabulum. (3) FE analysis was used to evaluate contact surface, cup insertion force, and stress distribution with different loading profiles. Five other segmental defects were created along the acetabular rim and evaluated for the same properties to understand the implications of the location of a segmental rim defect
Results
Optimal under-reaming for elderly patients
The optimum under-reaming diameter for a press-fit cup was computed by the probabilistic FE analysis for 100 random configurations of patients over age 70, and the frequency distribution is shown in Fig. 4. The average optimum under-reaming value was 1.10 mm with a standard deviation of 0.278 mm, and under-reaming values ranged from 0.63 mm to 2.13 mm. The Shapiro-Wilk test (W = 0.923) confirmed that the optimum under-reaming values for the various pelvic bone density configurations fell within a normal distribution. To evaluate the amount of stress on the acetabulum with a press-fit cup resulting from under-reaming variation, the von Mises stress yield was measured for under-reaming of 0.63 mm and 2.13 mm (Fig. 4). As the under-reaming increased from 0.63 mm to 2.13 mm, the stress on the inferior rim of the acetabulum increased by 136.63%.
Von Mises stress distribution (MPa) under a load of 1600 N, which simulates one leg stance during fast walking: a a normal acetabulum with an intact rim and cementless press-fit acetabular cup, b acetabulum with bone mineral density (BMD) loss for under-reaming of 2.13 mm, c acetabulum with BMD loss for under-reaming of 0.63 mm; d Frequency distribution of the results obtained with the probabilistic FE analysis with an overlapping normal distribution curve calculated from the mean and variance of the optimal under-reaming diameter for 100 pelvic configurations of elderly patients
Segmental rim defects and cup fixation
To study the effect of six different segmental rim defects without repair on press-fit cup fixation, the contact surface area, insertion force for cup seating, and peak stresses were measured (Table 1). All measurements were scaled to our control configuration of a press-fit cup in an intact pelvis prior to constructing the segmental defects. Thus, the contact surface area between the cup-bone interface was measured as the percentage reduction from our control configuration. The insertion force for cup seating was also measured as a percentage of insertion force required for the control configuration.
For our control configuration, a maximum peak stress was noted on the posterior-inferior region of the cortical acetabular rim, and stresses were lower in the subchondral bone (Fig. 4). For all six defects, the maximum peak stress was located at the same location as the control configuration (Fig. 5). A defect located along the anterior column (defects 5 and 6) generated increased stress near the location of the defect compared to other segmental rim defects.
The stiffness of the acetabular rim was evaluated by determining the Young’s modulus of the bone removed to create each defect. Compared to the rest of the acetabular rim, the superior rim (defect 1) had the largest Young’s modulus of 5.78 GPa, while the inferior rim had the smallest Young’s modulus of 4.27 GPa. The order of the stiffness for the defects from greatest to least was: superior rim, posterior column, anterior column, and inferior rim (Table 1). The difference between the average Young’s modulus of the anterior and posterior columns was statistically significant (P < 0.05, paired t-test).
A defect in the superior rim (defect 1) resulted in a 31.6% reduction in contact surface area at the cup-bone interface (Table 1). Similar to the superior rim, a defect in the inferior rim (defect 4) also resulted in a markedly decreased contact surface area of 31.4% and required the least insertion force for cup seating compared to the other segmental rim defects. Defects in the posterior column (defects 2 and 3) resulted in a contact surface area reduction of 20.7%, which was less than any other segmental rim defect. Defects in the anterior column and posterior column both required the same insertion force for cup seating of 84% (approximated as an average of both anterior defects and both posterior defects, respectively) compared to the control configuration, which was 5% greater than the insertion force for a superior rim defect and 12% greater than the insertion force for an inferior rim defect. Defects in the anterior column (defects 5 and 6) significantly compromised the contact surface area of the cup-bone interface, resulting in a 30.1% contact surface area reduction compared to the control configuration.
Discussion
The management of acetabular defects can be challenging since determining the amount of acetabular bone loss that will compromise the mechanical stability of the cup is not always clear [20]. Currently, surgeons quantify the bone loss by using centre edge angle measurements obtained from false-profile radiographs and AP radiographs, but there is significant variation in inter-observer reliability with this method [21]. In this paper, we performed probabilistic FE analysis to determine the optimum under-reaming in elderly patients. We then used a subject-specific FE model to understand how the location of segmental rim defects affects cementless press-fit cup fixation.
Based on our Monte Carlo simulation of optimum under-reaming for elderly patients, we found that a more stable fixation can be achieved if we under-ream by 1 mm rather than 2 mm in patients older than 70. Our study suggests that probabilistic FE analysis may be used to develop guidelines for under-reaming specific to certain age groups since the prevalence of hip replacements has increased among most age groups.
Based on our analysis of various minor segmental rim defects, we found that defects located along the anterior or posterior columns produced the highest stress concentration around the defect. Defects in the anterior column produced a greater stress concentration centered near the defect compared to defects in the posterior column, suggesting that the anterior column may be more important than the posterior column for cup fixation. Harnroongroj et al. previously suggested that the anterior column is vital for pelvic stability in a biomechanical study of human cadaveric pelvises [22]. A defect in the superior or inferior rim had similar peak stresses to the control configuration with no increase in stress near the defect location. Thus, defects in the superior or inferior rim may not require additional mechanical augmentation.
Defects in the anterior and posterior columns both required an increased insertion force for cup seating compared to defects in the superior or inferior rim. The inhomogeneous distribution of stiffness around the acetabular rim explains the differences in insertion force for cup seating. The large stiffness of the superior rim is required since this is where the main load transfers occur [23]. Hence, a segmental defect along the superior rim will require a significantly reduced insertion force for cup seating. The lower stiffness of the acetabular columns may explain the greater prevalence of fractures at the columns in the clinical setting [24]. An orthopaedic surgeon may consider augmentation of a defect along the anterior column prior to cup implantation since the anterior column has a lower stiffness than the rest of the rim.
A larger contact surface area between the implant surface and the acetabulum facilitates stable biological fixation [25]. For defects in the posterior column, a greater contact surface area of the press-fit cup was maintained in comparison to defects in the anterior column. The largest reduction in contact surface area was for defects along the superior or inferior rim located primarily at the iliac and ischial facets, respectively. These locations have been identified in the literature as the critical regions to obtain the tightest press-fit; thus, mechanical augmentation of superior and inferior rim defects may improve biological fixation and reduce the risk of micromotion [23]. However, unlike defects along the columns, defects in the superior or inferior rim do not affect the von Mises stresses at the acetabulum.
Differences between the parameters measured in this study for various segmental rim defects suggest that management must vary based on the defect location. If a segmental defect is along the superior or inferior rim, the use of a press-fit cup does not substantially reduce the initial cup fixation, as measured by the von Mises stress distribution and insertion force required for cup seating. Previous studies have shown that under-reaming by greater than 2 mm can improve cup fixation, but increases the risk of fracture since the stresses generated along the rim can approach the yield strength of osteoporotic bone [14, 17]. The balance between the increased fixation and greater risk of fracture achieved with increased under-reaming is still not very well understood.
In our analysis on various rim defects, we used a single normal hemi-pelvis to perform the experiment. If the pelvis were affected by a severe pathology such as osteoporosis, it would dramatically change the mechanical characteristics of the bone. Future development of this model may include the influence of both BMD loss with aging and segmental rim defects. This would require further investigation.
References
Kurtz S, Ong K, Lau E et al (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89:780–785. doi:10.2106/jbjs.f.00222
Labek G, Thaler M, Janda W et al (2011) Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg (Br) 93:293–297. doi:10.1302/0301-620x.93b3.25467
Choplin RH, Henley CN, Edds EM et al (2008) Total hip arthroplasty in patients with bone deficiency of the acetabulum. Radiographics 28:771–786. doi:10.1148/rg.283075085
Pierannunzii L, Mambretti A, D’Imporzano M (2011) Trabecular metal cup without augments for acetabular revision in case of extensive bone loss and low bone-prosthesis contact. Int J Immunopathol Pharmacol 24:133–137
Schmolders J, Friedrich MJ, Michel RD et al (2014) Acetabular defect reconstruction in revision hip arthroplasty with a modular revision system and biological defect augmentation. Int Orthop 39:623–630. doi:10.1007/s00264-014-2533-5
Steno B, Kokavec M, Necas L (2014) Acetabular revision arthroplasty using trabecular titanium implants. Int Orthop 39:389–395. doi:10.1007/s00264-014-2509-5
Cuckler JM (2002) Management strategies for acetabular defects in revision total hip arthroplasty. J Arthroplast 17:153–156
Huber WO, Noble PC (2014) Effect of design on the initial stability of press-fit cups in the presence of acetabular rim defects: experimental evaluation of the effect of adding circumferential fins. Int Orthop 38:725–731. doi:10.1007/s00264-013-2187-8
D’Imporzano M, Liuni FM, Tarantino U (2011) Acetabular fragility fractures in elderly patients. Aging Clin Exp Res 23:71–73
Gonzalez MH, Amirouche F (2014) Cementless acetabular revision with rim acetabular defects: experimental and FEA investigation. University of Illinois at Chicago
Zivkovic I, Gonzalez M, Amirouche F (2010) The effect of under-reaming on the cup/bone interface of a press fit hip replacement. J Biomech Eng 132:41008. doi:10.1115/1.2913228
Sporer SM, Paprosky WG, O’Rourke M (2005) Managing bone loss in acetabular revision. J Bone Joint Surg Am 87:1620–1630
Arden NK, Nevitt MC, Lane NE et al (1999) Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Study of Osteoporotic Fractures Research Group. Arthritis Rheum 42:1378–1385
Amirouche F, Solitro GF, Broviak S et al (2014) Factors influencing initial cup stability in total hip arthroplasty. Clin Biomech 29:1177–1185. doi:10.1016/j.clinbiomech.2014.09.006
Gonzalez MH, Amirouche F, Solitro GF (2015) Cup stability of decreased radius metal on metal acetabular cups: a finite element analysis. In: Orthop. Res. Soc. Annu. Meet. La Vegas, p 957
Amirouche F, Solitro GF (2011) Challenges in modeling total knee arthroplasty and total hip replacement. Procedia IUTAM 2:18–25. doi:10.1016/j.piutam.2011.04.003
Keller TS (1994) Predicting the compressive mechanical behavior of bone. J Biomech 27:1159–1168
Taddei F, Cristofolini L, Martelli S et al (2006) Subject-specific finite element models of long bones: An in vitro evaluation of the overall accuracy. J Biomech 39:2457–2467. doi:10.1016/j.jbiomech.2005.07.018
Wodzislawski W, Krupa S, Nowicki J et al (2009) The reaction of the pelvis to the implantation of the acetabular component of the hip endoprosthesis—initial tests with the use of computerized tomography. Acta Bioeng Biomech 11:45–54
Gozzard C, Blom A, Taylor A et al (2003) A comparison of the reliability and validity of bone stock loss classification systems used for revision hip surgery. J Arthroplast 18:638–642
Kappe T, Kocak T, Neuerburg C et al (2011) Reliability of radiographic signs for acetabular retroversion. Int Orthop 35:817–821. doi:10.1007/s00264-010-1035-3
Harnroongroj T (1998) The role of the anterior column of the acetabulum on pelvic stability: a biomechanical study. Injury 29:293–296
Widmer KH, Zurfluh B, Morscher EW (2002) Load transfer and fixation mode of press-fit acetabular sockets. J Arthroplast 17:926–935
Nwankwo C, Dong NN, Heffernan CD, Ries MD (2014) Do jumbo cups cause hip center elevation in revision THA? A computer simulation. Clin Orthop Relat Res 472:572–576. doi:10.1007/s11999-013-3169-2
Jasty M (1998) Jumbo cups and morselized graft. Orthop Clin N Am 29:249–254. doi:10.1016/S0030-5898(05)70323-0
Acknowledgements
The work was partially supported by the Aurelio M. Caccomo Family Foundation
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Amirouche, F., Solitro, G.F., Walia, A. et al. Segmental acetabular rim defects, bone loss, oversizing, and press fit cup in total hip arthroplasty evaluated with a probabilistic finite element analysis. International Orthopaedics (SICOT) 41, 1527–1533 (2017). https://doi.org/10.1007/s00264-016-3369-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3369-y