Abstract
Purpose
The aim of this study is evaluation of the efficacy of the use of platelet rich plasma (PRP) in management of femoral neck fractures.
Materials and methods
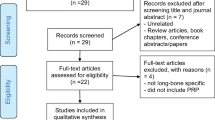
This is a prospective study that was conducted between February 2010 and March 2013. A total of 60 patients were included in this study, categorized randomly into two groups. Group A included fracture neck femur treated by closed reduction and internal fixation with three cannulated screws and group B by addition of PRP to internal fixation. We planned to compare time of healing, need for revision and incidence of complications between the two groups.
Results
Union occurred in 53 patients (88.33 %) in both groups, 25 cases (83.3 %) in group A and 28 cases (93.3 %) in group B, including three cases (5 %) with avascular necrosis (AVN): two in group A (6.7 %) and one case in group B (3.3 %).Revision surgery was done for six cases (20 %) in group A and for two cases (6.7 %) in group B. In both groups, all united cases had good to excellent clinical outcome as regards Harris hip score (HHS) at the end of the follow up.
Conclusion
Despite advances in surgical techniques and medical care, the risk of nonunion and avascular necrosis (AVN) after treatment of femoral neck fractures have not been changed appreciably in the last 50 years. Results of this study generally showed that both the median clinical and radiographic healing time were lower in group B compared to group A.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Platelet-rich plasma (PRP) was first described by Whitman et al. in 1997 [1], as an autologous preparation that concentrates platelets in a small volume of plasma [1]. It contains multiple growth factors, including transforming growth factor, insulin-like growth factor, fibroblast growth factor, and platelet derived growth factor and because of these it has been shown to have positive effects on stimulation of bones, blood vessels, and the formation of chondrocytes [2]. Femoral neck fractures are one of the greatest challenges facing nearly all orthopaedic surgeons with medical and economic burden. The risk of non union and implant failure remain the main concern and it may be up to 35 % of displaced fractures requiring revision surgery [3]. We hypothesize that PRP may reduce the incidence of failure of internal fixation in patients with femoral neck fracture, so this study was conducted to clarify the effect of using PRP in the management of these patients and to determine if it has any advantageous effect in bone healing.
Materials and methods
This was a prospective study that had been conducted between February 2010 and March 2013 by the same surgeon in the author’s institution, after approval of the local ethical committee and obtaining informed consent from all patients. It included 60 patients categorized randomly into two groups. Group A included 30 patients with fracture neck femur that were treated by closed reduction and internal fixation with three cannulated screws and group B that included 30 patients with fracture neck femur that were treated by the same method with addition of PRP. We planned to compare time of healing, need for revision and incidence of complications between two groups.
Inclusion criteria:
-
Age between 20 and 45 years
-
Early presentation of the fracture (within first 24 h)
-
Ability to achieve an acceptable closed reduction intra-operatively
Exclusion criteria:
-
Late presentation (more than 24 hours) after the fracture
-
Failure to achieve an acceptable reduction intra-operatively by closed methods
-
Pathological fractures
-
Auto-immune disease e.g., rheumatoid arthritis and systemic lupus erythematoses
-
Endocrinal disorders
-
Need for bone graft
This study included 39 males (65 %) and 21 females (35 %) with a mean age 30 ± 7.8: 32 ± 6.4 for group A and 28 ± 8.4 for group B. Participants were subjected to radiographs on admission which revealed 13 cases of basal neck fractures, 21 subcapital and 26 transcervical. Thirty-two cases were Garden III (18 patients group A and 14 patients group B) and 28 cases were Garden IV (12 patients for group A and 16 for group B).
Surgical technique
Under regional or general anaesthesia, the patient was placed supine on a traction table and closed reduction was performed. Garden’s alignment index was used to assess fracture reduction, with 155–180° in both antero-posterior and lateral view as the criterion for adequate reduction [4]. After confirmation of successful reduction by image intensifier, an internal fixation was done by three cannulated screws through a standard lateral approach (this was done for group A). On the other hand, in group B, after successful reduction was done, three guide wires were introduced as usual, followed by measuring of the screw’s length and reaming. Then the screw was introduced over the guide wire till it reached the fracture site, after that the guide wire was withdrawn and PRP was injected through the screw’s hole into the fracture site. During injection the lower limb was internally rotated to avoid back flow of PRP by gravity. The guide wire was reintroduced again through the screw hole which was advanced till the end without compression. The same procedure was repeated for every screw, and then tightening of the screws was done to compress the fracture site Fig. 1.
a Surgical technique on a male patient, 28 years old, with transcervical fracture neck femur (Garden III). b Post-reduction. c Introduction of the screw till the fracture site. d, e Withdrawal of the guide wire and injection of PRP. f The same was done for other screws. g Post-operative radiograph. h Follow up X-rays after ten weeks with complete union
Platelet preparation
The procedure consisted of 150-ml venous blood sample which was centrifuged twice. In the first spin, whole blood was centrifuged at 1480 rpm for ten minutes. This resulted in formation of three layers (a bottom layer composed of RBC; an upper layer composed of plasma, platelets and some WBCs; and an intermediate layer, composed mostly of WBCs), and the upper layer was collected with a pipette and transferred to an empty siliconized glass tube. In the second spin, the collected sample underwent another centrifugation at 3400 rpm for 15 minutes to concentrate platelets and produced 15 ml of PRP that was divided on the three screws [5].
Post-operative care
All patients started functional training of the hip from the second day post-operatively and were ambulated with non-weight bearing crutches until there was radiological evidence of union followed by partial weight bearing for an additional one month. Full weight bearing was allowed after that guided by the radiological follow up. All participants were followed up for a total of 12–48 months with an average of 28 months, initially at the onset of treatment and at six weeks, three months, six months, one year and then every six months. The clinical evaluation focused on the presence and the severity of pain. Degrees of pain were recorded according to visual analogue score (VAS) [6]. In addition, Harris hip score (HHS) [7] was used for functional assessment of the hip joint at the end of follow up after complete union and rehabilitation. Complications of the treatment were registered at each follow-up visit. Post-operative hip radiographs were analysed for acceptability of fracture reduction using the Garden’s alignment index [4]. Radiographs were taken at each visit to assess the progress of union, signs of failure of fixation and evidence of neck or head resorption. Radiographic outcomes were assessed by an independent consultant radiologist. In suspected cases, an MRI study was done to exclude or confirm any evidence of avascular necrosis. Radiographic non union was defined as “failure of the fracture to show signs of bony union on the antero-posterior or lateral radiograph nine months after surgery” [8]. Successful completion of treatment was defined as the accomplishment of both clinical and radiological union with no evidence of avascular necrosis.
Statistical analysis
Patients’ data were tabulated and processing was done using SPSS. Quantitative variables were expressed by means and standard deviation. Qualitative data were analysed using Pearson chi-square test and Fisher’s exact test. A P value > 0.05 means insignificant, P value < 0.05 means significant results and P value < 0.01 was highly significant.
Results
Our two randomly assigned populations were similar in most aspects, including age, gender, and Garden classification. The power of this study with a confidence level set at 5 % was 77.4 %. Various observations and results are presented in Table 1. Union occurred in 53 patients (88.33 %) in both groups, while the non united cases numbered 7 (11.67 %).
In our series, we were confronted with three cases (5 %) of AVN, two of which were in group A (6.7 %) and only one case in group B (3.3 %). These results were statistically insignificant (p = 0.0821).
We found no significant association between age of patient, gender or displacements of the fractures and the incidence of AVN (p = 0.462; Table 2).
Revision surgery was done for eight cases (13.33 %), of which six cases (20 %) were in group A, one of them due to arthritis following AVN in the form of total hip arthroplasty, and the other five cases of non union were revised by subtrochanteric osteotomy in two cases and total hip arthroplasty in the other three patients. For group B, revision surgery was done for two patients (6.7 %) of non union and managed by total hip arthroplasty. The relation of revision surgery between two groups was found to be statistically insignificant (p = 0.063).
In both groups, all united cases had good to excellent clinical outcome as regards HHS at the end of the follow up. However, cases of AVN in both groups had fair results.
Upon analysing the effect of location of fractures, whether basal neck, transcervical or subcapital, we found no statistical significance between locations of fractures and incidence of avascular necrosis or time of union (p = 0.096).
The relation between Garden’s classification and various results are presented in Table 3.
Discussion
Despite advances in surgical techniques and medical care, the risk of nonunion and AVN after treatment of femoral neck fractures have not been changed appreciably in the last 50 years [9]. In the era of regenerative medicine with the advances in the field of molecular biology, much attention has been recently placed on the healing environment of the fractures by better understanding of the exact pathophysiology of bone repair failure. Improvement of the local fracture environment by application of growth factors has been considered a treatment option that can be used alone or in conjunction with other traditional methods of fracture management from which positive results have been reported [10]. While PRPs osteogenic properties are not novel, we believe that this report is the first to document a translation of this property in clinical use in femoral neck fractures by direct application at the fracture site using simple, effective and novel techniques. Few data exist from other similar studies exploring platelet-rich therapy in bone healing with which to compare our findings. The rates of nonunion and AVN which have been reported after internal fixation varied widely. In various studies nonunion has ranged from 4 to 59 % and AVN from 10 to 86 %. The reasons for such a large variation could be the difference in the selection of patients with respect to age, the quality of bone, the pattern of fracture, the method of reduction, the mode of fixation and the timing of surgery [11]. Haidukewych et al. [11] reported its incidence as 23 % and Leighton [12] as 11–19 % in a meta-analysis study.
In our study, the overall incidence of non union (11.67 %) may have some similarity with these results but a noticeable difference was found while comparing both groups in favour of group B with a significant decrease in non union rate (6.7 %) compared to group A (16.67 %).
The united cases in group A had a mean time of union of 4.23 ± 1.2 months (range 3.2–6.2 months), and 3.55 ± .9 months (range 2.3–4.8 months) in group B, and this is much better than reported by Shih and Wang [13] with a union time of six months. Rodríguez-Merchán [14] reported a 92 % union rate after fixation with cannulated screws, and Ort et al. [15] reported a 90.4 % union rate after fixation of femoral neck fractures with DHS. This is comparable to our union rate in group B (93.3 %) but higher than group A (83.3 %). On the other hand, many orthopaedic surgeons are still sceptical about the effect of PRP in bone healing as in the study done by Gosens et al. [2] on open wedge osteotomy of tibia which concluded that there was no positive effect of PRP on bone healing when comparing its use with bone graft versus graft alone [2]. However, this study had some limitations as it did not correlate the gap of the osteotomy with the time of healing, and also the method of local injection of PRP after closure of the wound may be prone to leakage of some PRP. In contrast to our method of injection directly into the fracture site that may be more effective. These conflicting results may be also due to haematological variations, the method of preparation and concentration of platelet used. Also, age is another important factor that may have a direct influence on the haematological character of PRP. In an animal study done by Urgas et al. [16] about the efficacy of PRP on integration of osteochondral defects with mosaicoplasty, he found that PRP produced a better healing response with superior histological scores than the control group [16].
The incidence of AVN in our study was (6.7 %) in group A and (3.3 %) in group B with and overall incidence of 5 %. These results were much better than the majority of previously published data (ranging from 10 to 30 %) [17, 18]. Swiontkowski et al. [19] reported AVN rates of 20 % in femoral neck fractures treated by cannulated screws, Barnes et al. [20] reported an AVN rate of 22 % [20] and Ort et al. [15] reported an AVN rate of 24 % in femoral neck fractures treated by dynamic hip screw [15]. On the other hand, Zuckerman et al. [21] reported that this complication will occur at an 11 % lower rate in patients who were operated in the first 48 hours, regardless of the fixation technique used [21]. This can explain our better results as all of our cases were done in the first 24 hours with nearly anatomical reduction, and stable fixation in addition to good bone quality in all patients of our study.
Marwaha et al. [22] found patients experienced less pain after total knee replacement when they were injected by PRP than the control group with a better range of motion in the first 12 weeks postoperatively in contrast to the results of our series [22]. We found no statistical difference between two groups as regards pain improvement (VAS) as well as HHS. This was similar to the results reported by Peerbooms et al. and Berghoff et al. [23, 24]. These differences may be attributed to the reduction of the inflammatory reactions by the use of a leucocytic filter by Marwaha et al. to produce a leucocyte-free PRP.
The overall successful radiological healing rate in group A was 83.3 % compared to 93.3 % in group B which was statistically highly significant (p < 0.0001). Nevertheless, the overall rate of fixation failure of all intracapsular fractures of the femur is reported to be 20–35 % [20]; our study showed a decrease in this rate which was recorded in group B (6.7 %). This was significantly lower compared to the one observed in group A (20 %).
Our study was only conducted at a single centre, by the same surgeon with the same technique in reduction and fixation strategies. This probably reflects the better efficacy and confidence of the results by elimination of the surgeon’s effect. In addition, a review of the admission and screening data revealed no substantial differences between both groups as regards the age, sex, and fracture displacement. Although our study included a limited number of patient with a relatively short follow up period, the results were more precise as we excluded most of the secondary effects that can delay union by our inclusion and exclusion criteria.
Conclusion
Despite the ongoing developments of new strategies and the improvement of the existing ones for the treatment of fracture neck femur, their management remains difficult. In the daily clinical environment, many orthopaedic surgeons are still sceptical about the current levels of evidence supporting the use of biological response modifiers. Based on our results, we conclude in favour of the use of PRP in the treatment of femoral neck fracture as an adjuvant to the classic internal fixation in terms of clinical and radiological efficacy. However, the use and clinical validation of PRP is still in its early stages and it is mandatory to do further research to explore the best and most effective method of preparation and the ideal concentration to obtain maximum healing power and avoid undesirable inflammatory reaction.
References
Whitman DH, Berry RL, Green DM (1997) Platelet gel: an autologous alternative to fibrin glue with applications in oral and maxillofacial surgery. J Oral Maxillofac Surg 55(11):1294–1299
Peerbooms JC, Colaris JW, Gosens T et al (2012) No positive bone healing after using platelet rich plasma in a skeletal defect. An observational prospective cohort study. Int Orthop 36(10):2113–2119
Lu-Yao GL, Keller RB, Littenberg B et al (1994) Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am 76:15–25
Garden RS (1961) Low-angle fixation in fractures of the femoral neck. JBJS 43:647–663
Filardo G, Kon E, Ruiz MTP et al (2012) Platelet-rich plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approach. Knee Surg Sports Traumatol Arthrosc 20:2082–2091
Warden V, Hurley AC, Volicer L (2003) Development and psychometric evaluation of the pain assessment in advanced dementia (PAINAD) scale. J Am Med Dir Assoc 4:9–15
Yoo MC, Chung DW, Hahn CS (1992) Free vascularized fibula grafting for the treatment of osteonecrosis of the femoral head. Clin Orthop Relat Res 277:128–138
Parker MJ, Raghavan R, Gurusamy K (2007) Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Relat Res 458:175–179
Stravrakis TA, Lyras DN, Psillakis IG (2009) Fractures of the femoral neck treated with hemi arthroplasty. Folia Med 51:134–145
Wong RW, Rabie AB (2003) Statin collagen grafts used to repair defects in the parietal bone of rabbits. Br J Oral Maxillofac Surg 41:244–248
Haidukewych GJ, Rothwell WS, Jacofsky DJ (2004) Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. JBJS (Am) 86:1711–1716
Leighton R (2008) Classification and treatment and treatment of femoral neck nonunions in young patients. J Bone Joint Surg Br 90:124–128
Shih CH, Wang KC (1991) Femoral neck fractures. 121 cases treated by Knowles pinning. Clin Orthop Relat Res 271:195–200
Rodríguez-Merchán EC (2002) In situ fixation of nondisplaced intracapsular fractures of the proximal femur. Clin Orthop Relat Res 399:42–51
Ort PJ, LaMont J (1984) Treatment of femoral neck fractures with a sliding compression screw and two Knowles pins. Clin Orthop Relat Res 190:158–162
Altan E, Aydin K, Ugras S et al (2014) The effect of platelet-rich plasma on osteochondral defects treated with mosaicplastynt. Orthopedics 38(6):1321–1328
Gerber C, Strehle J, Ganz R (1993) The treatment of the fractures of the femoral neck. Clin Orthop 292:77–86
Cserhati P, Kazar G, Manninger J et al (1996) Non-operative or operative treatment for undisplaced femoral neck fractures: a comparative study of 122 non-operative and 125 operatively treated cases. Injury 27:583–588
Swiontkowski MF (1994) Current concept review: intracapsuler fractures of the hip. JBJS 76A:129–138
Barnes R, Brown JT, Garden RS, Nicoll EA (1976) Subcapital fractures of the femur. A prospective review. J Bone Joint Surg Br 58:2–24
Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH (1995) Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am 77:1551–1556
Aggarwal AK, Shashikanth VS, Marwaha N (2014) Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop 38(2):387–395
Peerbooms JC, Wolf GS, Colaris JW, Bruijn DJ, Verhaar JA (2009) No positive effect of autologous platelet gel after total knee arthroplasty. Acta Orthop 80:557–562
Berghoff W, Pietrzak W, Rhodes R (2006) Platelet-rich plasma application during closure following total knee arthroplasty. Orthopedics 29(7):590–598
Acknowledgments
The author would like to extend his appreciation to all technicians and physicians in the clinical pathology department at his institute for their magnificent help.
Role of the funding source
The author did not receive any fund for this research.
Competing interest
The author has no competing interests to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Samy, A.M. The role of platelet rich plasma in management of fracture neck femur: new insights. International Orthopaedics (SICOT) 40, 1019–1024 (2016). https://doi.org/10.1007/s00264-015-2844-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2844-1