Abstract
Purpose
The aim of this study was to investigate the effects of platelet-rich plasma (PRP) on fracture union rate and fracture union time in pseudoarthrosis surgery and to evaluate the clinical and functional results of the patients.
Methods
The patients who were undergone pseudoarthrosis surgery between 2011 and 2014 were evaluated retrospectively. Twenty-four patients were included in the study. Patients were divided into two groups with used PRP and not used PRP during surgery. There were 14 patients in the PRP group and 10 patients in the control group. The two groups were compared in terms of demographic characteristics, fracture union time, and functional scores of the Lower Extremity Functional Scale and Upper Extremity Functional Index.
Results
Fractures were healed in both groups, and no complications were encountered. A statistically significant difference was found between the two groups in terms of fracture union time. The mean time of union was 5.3 months in the PRP group and 11.3 months in the control group (p: 0.000). There was no statistically significant difference between the two groups in terms of functional scores (p: 0.250).
Conclusion
As a result of our study, we concluded that PRP is an effective and safe method in pseudoarthrosis surgery that reduces fracture union time. Controlled studies with more patient numbers are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A healthy bone is capable of self-repair and rearrangement, but complications can cause delayed healing or pseudoarthrosis [1]. For the purposes of this study, we have defined nonunion as the lack of union formation of the fracture line for at least 9 months and no signs of fracture healing for 3 consecutive months [2, 3]. The incidence of pseudoarthrosis ranges between 1 and 6% in long-bone fractures [4, 5]. Pseudoarthrosis may be hypertrophic or atrophic depending on the vascularity of the fracture line. In addition, pseudoarthrosis can be septic or aseptic [6]. In hypertrophic pseudoarthrosis, there is a solid vascular support in the fracture line, whereas in atrophic pseudoarthrosis the fracture line is avascular [6].
Pseudoarthrosis treatment is one of the most challenging areas of orthopedics7. Treatment may vary from non-invasive techniques where pulsatile ultrasound and electromagnetic waves are applied to the field of pseudoarthrosis, from major and aggressive surgeries depending on the type of pseudoarthrosis and the degree of complication [7,8,9]. Pseudoarthrosis has a complex treatment and usually requires aggressive surgery [7] . Nevertheless, the failure rate has been reported to be %5–40 [10].
Platelets have an very important role in fracture healing and are involved in the formation of a complex inflammatory response in the fracture site [11]. Platelets have important functions in the formation of angiogenesis, mesenchymal cells, and growth factors that provide fracture union [12,13,14]. Platelets also increase osteoblast proliferation [15]. Platelet-rich plasma (PRP) is obtained from autologous blood and is defined as ``a certain plasma volume with a platelet concentration several times above physiological levels'' [16]. PRP is very important to be source of growth factors such as platelet-derived growth factor (PDGF), transforming growth factor beta (TGF-β), insulin-like growth factor-1 (IGF-1), fibroblast growth factor (FGF-b), vascular endothelial growth factor (VEGF), and epidermal growth factor(EGF) that play a role in healing and bone regeneration [17,18,19].
The aim of this study was to investigate the effects of PRP on pseudoarthrosis in terms of fracture union, fracture union time, and clinical and functional outcomes.
Patients and methods
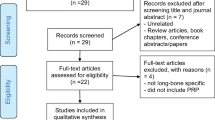
Patients who underwent pseudoarthrosis surgery between 2011 and 2014 by the Department of Orthopedics and Traumatology of Balıkesir University Faculty of Medicine were retrospectively analyzed. The presence of post-traumatic aseptic pseudoarthrosis for at least 9 months and no radiological signs of fracture union during the last 3 months, and complete patient data and contact information were determined as the inclusion criteria. Skeletal immaturity, septic pseudoarthrosis, pseudoarthrosis due to pathological fracture, presence of systemic infection, presence of autoimmune and neoplastic disease, loss of data and communication were evaluated as exclusion criteria.
As a result of inclusion and exclusion criteria, 24 patients were included in the study. Patients were divided into two groups with and without used PRP during surgery. There were 14 patients in the PRP group and 10 patients in the control group. Both groups were compared in terms of demographic characteristics, fracture union time, and functional scores.
Pseudoarthrosis surgeries were performed by two surgeons: one who used PRP and another who did not. All surgeries were performed in accordance with open reduction and internal fixation rules. In all cases, the pseudoarthrosis area was reached by the incision in accordance with the characteristics of the pseudoarthrosis region and neurovascular structures were protected. Pseudoarthrosis tissues and sclerotic bones were removed from the area until alive bone tissue was seen at the fracture ends. In all cases, the resulting defect was filled using autograft, allograft or autograft and allograft, and it was aimed to stimulate healing in the fracture ends. The choice of fixation material in the cases was chosen and applied according to the surgeon's decision.
Patients in both groups were followed up until fracture union occurred. Follow-up was performed monthly in first postoperative 3 months and 3-month intervals after first 3 months. X-ray radiographs were performed in follow-up periods. The presence of callus in 3 cortex in the region where pseudoarthrosis surgery was performed was accepted as fracture union [20]. Lower Extremity Functional Scale (LEFS) and Upper Extremity Functional Index (UEFI) tests were used to evaluate the functional capacities of the patients at the final follow-up. None of the patients had any complications during and after surgery. PRP application did not cause surgical morbidity, increase operation time and complications in any patient. Complete fracture union was achieved in all patients.
Ethics committee approval was obtained from Balıkesir University Clinical Research Ethics Committee. The study was carried out taking into account the principles of the Declaration of Helsinki.
PRP preparation and application
Platelet-rich plasma was produced according to a method previously described [21, 22]. 75 ml of whole blood taken from the patient was taken into a tube containing 0.163 ml of acid-citrate-dextrose per 1 ml of anticoagulant and centrifuged at 2500 rpm for 15 min. Plasma and erythrocytes were separated end of the first centrifugation; the plasma was centrifuged for a second time at 2500 rpm for 10 min. Thus, platelet-poor plasma (TFP) and PRP were separated from each other. As a result of the procedures, 10 ml PRP was available for the surgery.
The achieved PRP was applied in autograft, allograft, or combination with both autograft and allograft as the cancellous type used to close the defect during surgery in the pseudoarthrosis field.
Statistical Method
The data obtained from the study were analyzed using SPSS (Statistical Package for Social Sciences) Windows 22.0 program. Number, percentage, mean, and standard deviation were used as descriptive statistical methods in the evaluation of the data. The relationship between the grouped variables was tested by Chi-square analysis. The t-test was used to compare the quantitative continuous data between two independent groups.
Results
Of the 24 patients included in the study, 11 (45.8%) were male and 13 (54.2%) were female. Of the 14 patients in the PRP group, 7 (50.0%) were male and 7 (50.0%) were female, while 4 (40.0%) of the 10 patients in the control group were male and 6 (60%) were female. There was no statistically significant difference between the two groups in terms of gender (p:0.632) (Table 1). The mean age of the patients in the PRP group was 50.5 (range: 25–77), and the mean age of the patients in the control group was 48.9 (range: 25–75) (p: 0.894) (Table 2).
In the PRP group, the pseudoarthrosis regions were femur (n: 6, 42.9%), humerus (n: 3, 21.4%), tibia (n: 2, 14.3%), ulna (n: 2, 14.3%), and clavicle (n: 1, 7.1%) while pseudoarthrosis regions were femur (n: 5, 50.0%), humerus (n: 4, 40.0%), and tibia (n: 1, 10.0%) in the control group. There was no statistically significant difference between the two groups in terms of pseudoarthrosis regions (p: 0.538) (Table 1). In the PRP group, 9 (64.3%) of the pseudoarthroses were atrophic pseudoarthrosis and 5 (35.7%) were hypertrophic pseudoarthrosis. In the control group, 7 (70.0%) patients had atrophic pseudoarthrosis and 3 (30.0%) patients had hypertrophic pseudoarthrosis. There was no statistically significant difference between the two groups in terms of pseudoarthrosis types (p: 0.598) (Table 1).
The trauma mechanism was due to the vehicle traffic accident in 8 (57.2%) patients in the PRP group and 5 (50.0%) patients in the control group; 1 patient (7.1%) in the PRP group and 1 (10.0%) patient in the control group had fracture due to non-vehicle traffic accident. Fall was the cause of trauma in 5(35.7%) patients in the PRP group and 4 (40.0%) patients in the control group. While 1 (7.1%) patient in the PRP group had an open fracture, 13 (92.9%) patients had a closed fracture, 1 (10.0%) patient in the control group had an open fracture, and 9 (90.0%) patients had a closed fracture. There was no difference between the two groups in terms of fracture type (p: 0.619) and injury type (p: 0.776) (Table 1).
In the PRP group, 7 (50.0%) patients were treated with plate, 5 (35.7%) patients with intramedullary nail, 1 (7.1%) patient with plate + intramedullary nail, 1 (7.1%) patient with external fixator. In the control group, 5 (50.0%) patients were treated with plate and 5(50.0%) patients with intramedullary nail. In the PRP group, autograft was applied to 6 (42.9%) patients, allograft to 5 (35.7%) patients, autograft + allograft to 3(21.4%) patients. In the control group, autograft was applied to 4 (40.0%) patients, allograft to 4(40.0%) patients, autograft + allograft to 2(20.0%) patients. There was no significant difference between the use of fixation material (p: 0.417) and bone graft use (p: 0.205) between the two groups (Table 1).
There was no statistically significant difference between two groups in terms of previous treatment method, chronic disease, and smoking (p > 0.05) (Table 1).
The mean time of pseudoarthrosis was 34.3 months in the PRP group and 11.3 months in the control group (p: 0.057) (Table 2). Fracture union time was 5.3 (range: 3–9) months in the PRP group and 11.3 (range: 6–12) months in the control group. There was a statistically significant difference between the two groups in terms of fracture union time (p: 0.000) (Table 2). There was no statistically significant difference between the two groups in terms of functional scores (p: 0.250) (Table 2). Pseudoarthrosis time, fracture union time, and functional scores of the groups are shown in Fig. 1.
Discussion
Twenty-four patients who underwent pseudoarthrosis surgery were divided into two groups as the PRP group (n: 14) and the control group (n: 10). The two groups were compared in terms of demographic characteristics, fracture union time, and clinical and functional results. As a result, the time of fracture union was significantly shorter in patients with PRP applied to the pseudoarthrosis area during surgery compared to the control group. The fracture union time was 5.3 months in the PRP group and 11.3 months in the control group (p: 0.000). In this result, we believe PRP has an effect on the release and transport of the growth factors (PDGF, TGF-β, IGF-1, FGF-b, VEGF, EGF) to the fracture site involved in the healing and bone regeneration [17,18,19]. No statistically significant difference was found between the two groups in terms of functional results (LEFS / UEFI) at the last follow-up after fracture union. Depending on this result, it may be concluded that PRP reduces fracture union time but has no significant effect on functional results.
Delayed union or pseudoarthrosis is seen in 1–6% of long-bone fractures, but in 5–10% of all fractures [4, 5, 23]. This can be caused by several factors. Major and widespread trauma, unstable fracture fixation, large gap in fracture line, excessive damage of soft tissue during surgery, early mobilization, infection, presence of comorbid diseases, advanced age are the major causes of delayed union or pseudoarthrosis [24,25,26]. There are various methods used in the literature to increase the union in the treatment of pseudoarthrosis [6, 9, 11, 27].
As the study of Sanchez et al., they performed the surgery of 15 patients with atrophic pseudoarthrosis with PRP and reported that they achieved fracture union in all patients [6]. Galasso et al. applied PRP to the fracture site in 22 patients with atrophic pseudoarthrosis and achieved fracture union within a mean of 21.5 weeks in all patients [11]. In contrast to these studies, in our study, there was a control group besides PRP group. In the literature, we found one study investigating the efficacy of PRP in pseudoarthrosis by comparing it with the control group [27]. Ghaffarpasand et al. compared the patients with pseudoarthrosis who underwent PRP during the surgery with the control group. They stated that there was a high fracture union rate, short fracture union time, and lower postoperative pain in the PRP group compared to the control group, but the infection rate was higher in the PRP group [27]. Similar to this study, in our study the time of fracture union was significantly shorter in the PRP group than in the control group, unlike there were no postoperative complications in any patient. The fact that the number of patients was higher than our study may have revealed this result. Furthermore, unlike the study of Ghaffarpasand et al., We compared both groups in terms of functional outcomes. We did not find any significant difference between the two groups in terms of functional results.
Most studies investigating the efficacy of PRP in the treatment of pseudoarthrosis include pre-clinical animal studies [28,29,30,31,32]. There is no consensus on the effectiveness of PRP in the treatment of pseudoarthrosis. The use of PRP has been reported to be effective in the treatment of pseudoarthrosis in the majority of pre-clinical animal studies [28,29,30]. There are also some pre-clinical animal studies suggesting that PRP has no extra positive effect on the treatment of pseudoarthrosis [31, 32].
The limitations of our study are retrospective nature and number of patients. The different time of pseudoarthrosis between groups can be considered as another limitation of the study. This may be caused by the presence of two different surgeons who applied and did not apply PRP in pseudoarthrosis surgery. In addition to PRP, groups could be formed in different methods; for example, bone morphogenic protein-7 and platelet-rich fibrin were compared. In addition, the scope of the study could be expanded and evaluation of callus formation with computed tomography could be added to the comparison criteria. The cost-effectiveness of the PRP application could also be evaluated within the study.
Conclusion
PRP application in pseudoarthrosis surgery is an effective and safe method that accelerates fracture healing with the growth factors it provides. In addition, surgical skill, timing of surgery, patient selection, and fixation methods may all have a role on the outcome of pseudoarthrosis surgery. There is a need for studies in which the number of patients is higher and different groups are compared.
References
Malhotra A, Pellethier MH, Yu Y et al (2013) Can platelet-rich plasma (PRP) improve bone healing? A comparison between the theory and experimental outcomes. Arch Orthop Trauma Surg 133(2):153–165. https://doi.org/10.1007/s00402-012-1641-1
Nwagbara IC (2010) Osseous union in cases of non-union in long bones treated by osteosynthesis. Niger J Clin Pract 13(4):436–440
Rubel IF, Kloen P, Campbell D et al (2002) Open reduction and internal fixation of humeral non-unions: a biomechanical and clinical study. J Bone Joint Surg Am 84(8):1315–1322. https://doi.org/10.2106/00004623-200208000-00004
Nakase T, Kawai H, Yoshikawa H (2009) In situ grafting of excised fracture callus followed by Ilizarov external fixation for treatment of nonunion after open fracture of tibia. J Trauma 66(2):550–552. https://doi.org/10.1097/01.ta.0000229979.06520.72
Wolinsky PR, McCarty E, Shyr Y et al (1999) Reamed intramedullary nailing of the femur: 551 cases. J Trauma 46(3):392–399. https://doi.org/10.1097/00005373-199903000-00007
Sanchez M, Anitua E, Cugat R et al (2009) Nonunions Treated With Autologous Preparation Rich in Growth Factors. J Orthop Trauma 23(1):52–59. https://doi.org/10.1097/BOT.0b013e31818faded
Bances IF, Basterrechea MP, Lopez SP et al (2013) Repair of long-bone pseudoarthrosis with autologous bone marrow mononuclear cells combined with allogenic bone graft. Cytotherapy 15(5):571–577. https://doi.org/10.1016/j.jcyt.2013.01.004
Griffin XL, Costa ML, Parsons N et al (2011) Electromagnetic field stimulation for treating delayed union or non-union of long bone fractures in adults. Cochrane Database Syst Rev 13(4):CD008471. https://doi.org/10.1002/14651858.CD008471.pub2
Calori GM, Mazza E, Colombo M et al (2011) Treatment of long bone non-unions with polytherapy: indications and clinical results. Injury 42(6):587–590. https://doi.org/10.1016/j.injury.2011.03.046
La Velle D (2004) Delay in union and pseudoarthrosis fracture. In: Canale S (ed) CAMPBELL cirugia ortopedica. Elsevier, Madrid, Spain España SA, pp 3125–3126
Galasso O, Mariconda M, Romano G et al (2008) Expandable intramedullary nailing and platelet rich plasma to treat long bone non-unions. J Orthopaed Traumatol 9(3):129–134. https://doi.org/10.1007/s10195-008-0021-7
Simpson AHRW, Mills L, Noble B (2006) The role of growth factors and related agents in accelerating fracture healing. J Bone Joint Surg Br 88(6):701–705. https://doi.org/10.1302/0301-620X.88B6.17524
Tsiridis E, Upadhyay N, Giannoudis P (2007) Molecular aspects of fracture healing: which are the important molecules? Injury 38:11–25. https://doi.org/10.1016/j.injury.2007.02.006
Veillette CJ, McKee MD (2007) Growth factors—BMPs, DBMs, and buffy coat products: are there any proven differences amongst them? Injury 38:38–48. https://doi.org/10.1016/j.injury.2007.02.009
Slater M, Patava J, Kingham K et al (1995) Involvement of platelets in stimulating osteogenic activity. J Orthop Res 13(5):655–663. https://doi.org/10.1002/jor.1100130504
Roukis TS, Zgonis T, Tiernan B (2006) Autologous platelet-rich plasma for wound and osseous healing: a review of the literature and commercially available products. Adv Ther 23(2):218–237. https://doi.org/10.1007/bf02850128
Dohan EDM, Rasmusson L, Albrektsson T (2009) Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol 27(3):158–167. https://doi.org/10.1016/j.tibtech.2008.11.009
Intini G (2009) The use of platelet-rich plasma in bone reconstruction therapy. Biomaterials 30(28):4956–4966. https://doi.org/10.1016/j.biomaterials.2009.05.055
Lenza M, Ferraz SB, Viola DCM et al (2013) Platelet-rich plasma for long bone healing. Einstein (Sao Paulo) 11(1):122–127. https://doi.org/10.1590/S1679-45082013000100023
Bhandari M, Guyatt GH, Swiontkowski MF et al (2002) A lack of consensus in the assessment of fracture healing among Orthopaedic surgeons. J Orthop Trauma 16(8):562–566. https://doi.org/10.1097/00005131-200209000-00004
Marx RE, Carlson ER, Eichstaedt RM et al (1998) Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85(6):638–646. https://doi.org/10.1016/s1079-2104(98)90029-4
Mariconda M, Cozzolino F, Cozzolino A et al (2008) Platelet gel supplementation in long bone nonunions treated by external fixation. J Orthop Trauma 22(5):342–345. https://doi.org/10.1097/BOT.0b013e318172cea5
Kloen P, Doty SB, Gordon E et al (2002) Expression and activation of the BMP signaling components in human fracture nonunions. J Bone Joint Surg Am 84(11):1909–1918. https://doi.org/10.2106/00004623-200211000-00001
Rodriguez-Merchan EC, Forriol F (2004) Nonunion: general principles and experimental data. Clin Orthop 419:4–12
Resnick D, Goevgen T, Niwayama G (1988) Diagnosis of bone joint disorders. WB Saunders, Philadelphia
Soucacos PN, Dailiana Z, Beris AE et al (2006) Vascularised bone grafts for the management of non-union. Injury 37(1):41–50. https://doi.org/10.1016/j.injury.2006.02.040
Ghaffarpasand F, Shahrezaei M, Dehghankhalili M (2016) Effects of platelet rich plasma on healing rate of long bone nonunion fractures: a randomized double-blind placebo controlled clinical trial. Bull Emerg Trauma 4(3):134–140
Malhotra R, Kumar V, Garg B et al (2015) Role of autologous platelet-rich plasma in treatment of long-bone nonunions: a prospective study. Musculoskelet Surg 99(3):243–248. https://doi.org/10.1007/s12306-015-0378-8
Simman R, Hoffmann A, Bohinc RJ et al (2008) Role of platelet-rich plasma in acceleration of bone fracture healing. Ann Plast Surg 61(3):337–344. https://doi.org/10.1097/SAP.0b013e318157a185
Guzel Y, Karalezli N, Bilge O et al (2015) The biomechanical and histological effects of platelet-rich plasma on fracture healing. Knee Surg Sports Traumatol Arthrosc 23(5):1378–1383. https://doi.org/10.1007/s00167-013-2734-2
Sarkar MR, Augat P, Shefelbine SJ et al (2006) Bone formation in a long bone defect model using a platelet-rich plasma-loaded collagen scaffold. Biomaterials 27(9):1817–1823. https://doi.org/10.1016/j.biomaterials.2005.10.039
Hernandez-Fernandez A, Vélez R, Soldado F et al (2013) Effect of administration of platelet-rich plasma in early phases of distraction osteogenesis: an experimental study in an ovine femur model. Injury 44(7):901–907. https://doi.org/10.1016/j.injury.2012.10.018
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Başdelioğlu, K., Meriç, G., Sargın, S. et al. The effect of platelet-rich plasma on fracture healing in long-bone pseudoarthrosis. Eur J Orthop Surg Traumatol 30, 1481–1486 (2020). https://doi.org/10.1007/s00590-020-02730-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02730-2