Abstract
Purpose
Bone marrow oedema (BME) in the knee is a feature of several pathological conditions, and it has been described with high frequency in patients with acute anterior cruciate ligament (ACL) injury. The aim of this study is to evaluate the significance of BME, assessed in MRIs performed for ACL injury, with regards to clinical outcome and return to sport.
Methods
A total of 134 patients (98 men, 36 women) with ACL tear and MRI knee scan within six months from trauma were analysed. The presence of BME was evaluated on MRI images considering: extension and hyperintensity, the WORMS score oedema classification, and measuring the BME area. The clinical results were documented by IKDC-subjective score and the sport activity level by Tegner score at a minimum of five years follow up.
Results
BME was present in 74 knees (55.2 %), with a mean area of 523 ± 370 mm². The presence of BME showed a gradual decrease over time (p = 0.008), being detectable in MRIs performed more than three months after trauma in just 25.0 % of cases. Although 54 % of the patients without BME after three months returned to their previous sport level, no patients with oedema reached a full sport recovery (p = 0.01). In the group that underwent ACL reconstruction, the BME area was significantly correlated with a return to the previous sport level at the mid/long-term follow-up (p = 0.038).
Conclusions
BME is a common finding, which decreases over time after injury. However, when BME is still detectable it correlates with clinical prognosis, and even in sport-active patients undergoing ACL reconstruction, a higher BME area is a negative predictive factor for a successful outcome at the mid/long-term follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In recent decades bone marrow oedema (BME), bone bruise, and bone contusion have been gaining increasing interest. These terms seem to be used as synonyms [1], referring to an entity recognized as post-traumatic bone marrow change which is caused by the combination of haemorrhage, oedema, and micro-trabecular fracture without the destruction of adjacent cortex [2]. BME in the knee is a feature of several pathological conditions, and it has been described very often in patients with acute anterior cruciate ligament (ACL) injury.
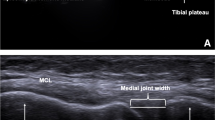
BME is occult in radiographic studies and requires magnetic resonance imaging (MRI) to be identified: on T1-weighted images it appears as an area of decreased signal intensity in the bone marrow, unlike on T2-weighted images or STIR (short T1 inversion recovery), where it is visualized as increased signal intensity. Sensitivity and specificity of MRI for detecting knee BME have already been documented at 83–96 % and 86–96 %, respectively [2]. MRI evaluation reveals the prevalence of BME in ACL injuries; BME has been shown to occur in more than 80 % of patients with complete rupture [3]. Several studies have also investigated the aetiopathology and have found that these abnormal MRI signals are caused by the original impact of the femoral cartilage to the tibial plateau during the traumatic event [4]. The classic example is the lateral compartment contusion of the posterior aspect of the lateral tibial plateau and of the mid-lateral femoral condyle just above the anterior horn of the lateral meniscus, which are associated with ACL injury [5, 6]. An association between ACL and meniscal lesions with BME has also been shown [2], as well as correlation of acute BME MRI patterns with the mechanism of ACL injury [7].
However, whereas the prevalence and aetiopathology of BME in ACL injured knees have been widely reported, less clear is its clinical relevance in terms of clinical prognosis. The purpose of this study was to evaluate the significance of BME, assessed during MRIs performed for ACL injury, in terms of clinical outcome and return to sport. The hypothesis was that a higher level of post-traumatic BME might correlate with a poorer prognosis at mid/long-term follow-up.
Methods
All knee MRIs performed at our institute between June 2004 and June 2008 were analysed in this retrospective study to have a minimum of five years’ clinical follow-up with respect to the imaging analysis. The patients were clinically evaluated at a mean of 79.9 ± 10.5 months from MRI.
MRI examinations were carried out using a 1.5-T superconducting magnet (General Electric Co, Fairfield, Connecticut) with a dedicated quadrature detection knee coil (Quadknee) (diameter, 18 cm). The following sequences were used: (1) sagittal fast spin echo and proton density weighted with fat saturation (repetition time [TR], 3200 ms; echo time [TE], 22 ms; echo train, 8; field of view [FOV], 160 mm; matrix, 512 3 256; slice thickness, 3.5 mm; gap, 0.5 mm; number of excitations [NEX], 2; number of slices, 22) and (2) sagittal dual fast spin echo (TR, 2850 ms; TE, 100 and 44 ms [T2 weighted and proton density weighted, respectively]; echo train, 8; FOV, 160 mm; matrix, 512 3 256; slice thickness, 3.5 mm; gap, 0.5 mm; NEX, 2).
Among 1,151 patients who underwent knee MRI, we selected 134 patients (98 men, 36 women) with the following characteristics: radiological diagnosis of ACL tear, age at the time of MRI between 16 and 50 years, and MRI scan of the knee within six months from injury. Patients having complex lesions of the knee (cartilage lesions, fractures, complete tears of other ligaments), and infective, tumor and rheumatic pathology were excluded from analysis. Detailed characteristics of the patients are provided in Table 1. Sixty-seven of the selected 134 patients (50 %) underwent ACL reconstruction. ACL reconstructions were performed either at our institute or other hospitals, using various grafts and techniques.
The presence of BME was evaluated by two independent authors (blinded to the clinical outcome) on MRI images using a three-level grading considering extension and hyperintensity (1: no edema; 2: small edema or slightly hyperintense; 3: large edema or highly hyperintense), and the WORMS score edema classification: altered signal intensity in the epiphyseal marrow was graded from 0 to 3 on the extent of regional involvement (0 = none; 1 = <25 % of the region; 2 = 25 % to 50 % of the region; 3 = >50 % of the region). The area of the BME was also recorded, using the single slice with the biggest BME area in lateral projection. The clinical results were obtained through a phone interview and evaluated using the International Knee Documentation Committee (IKDC) subjective score. The sport activity level was rated using the Tegner score, taking into account the Tegner score pre-injury and at the time of mid/long-term follow-up. In particular, the group of patients who underwent ACL reconstruction was evaluated by Tegner score both at one-year follow-up, retrospectively, and then at mean six years after surgery to better document their return to sport participation. The Hospital Ethics Committee and Internal Review Board approved this study, and informed consent of all patients for analysis and publication of MRI and clinical data was obtained.
Statistical methods
All continuous data were expressed in terms of the mean and the standard deviation of the mean, and the categorical data were expressed as frequency and percentages. The Kolmogorov–Smirnov test was performed to test normality of continuous variables. The ANOVA test was performed to assess the between-group differences of continuous, normally distributed and homoscedastic data; the Mann–Whitney test was used otherwise. The ANOVA test followed by the Scheffè post hoc pairwise comparison was used also to assess the differences among groups of continuous, normally distributed and homoscedastic data; the Kruskal–Wallis test followed by the Mann–Whitney test with the Bonferroni correction for multiple comparison was used otherwise. The Spearman rank correlation was used to assess correlation between continuous data. The Kendall tau correlation was used to assess correlation between ordinal data. The Fisher chi square test was performed to investigate the relationships between dichotomous variables. The Pearson chi square test evaluated by exact methods for small samples was performed to investigate the relationships between grouping variables. For all tests p < 0.05 was considered significant.
All statistical analysis was performed using SPSS v.19.0 (IBM Corp., Armonk, NY, USA).
Results
The MRI analysis on 134 patients showed that BME was present in 74 knees (55.2 %).
The primary BME location was: 35 in the lateral tibial plateau (LTP), 31 of which were in the posterior part of the LTP; 23 in the lateral femoral condyle (LFC), 14 of which were in the central third of the LFC; 11 in the medial tibial plateau (MTP); and five in the medial femoral condyle (MFC). The mean BME area was 523 ± 370 mm².
MRI was performed at a mean of 1.8 ± 1.5 months after trauma. The analysis of the presence of BME depending on the time of MRI after ACL injury showed a decrease in BME over time (p = 0.008, Fig. 1). Comparing the BME rate in the MRI performed before or after three months after trauma, we found that in the “earlier group” BME was present in 64.7 %, while in the “later group” 25.0 % of the MRI presented BME.
No correlation was found between edema and clinical outcome in the whole group of MRIs.
In the hypothesis that the presence of BME after more than three months might be due to a major trauma, we performed a sub-analysis on the 32 patients of this group to assess the correlation of major trauma and clinical outcome; we observed that no patient with oedema after three months reached a full sport recovery at the mid/long-term follow-up, whereas in the group without BME 54 % of patients were able to reach at least 90 % of their pre-injury sport activity level evaluated by Tegner score (p = 0.01; Fig. 2).
Further analysis was performed to evaluate separately patients who underwent and those who did not undergo ACL reconstruction. These groups differed in terms of patient characteristics, namely, patients who underwent ACL reconstruction were more active with a higher pre-injury Tegner score (p = 0.002), and they were also younger (p = 0.003), and more men belonged to this group (p = 0.05).
No correlation between edema and clinical outcome was found in the 67 patients who did not undergo ACL reconstruction.
Conversely, a significant correlation was found in the analysis of the group that underwent ACL reconstruction, a very sport-active group where 97 % of the patients presented a pre-injury Tegner score ≥ 6. The recovery of sport activity was shown to be different based on the presence of BME: patients with edema had a tendency towards an inferior recovery at one year (p = 0.07) and the BME area was significantly correlated with the return to the previous sport level at the mid/long-term follow-up (mean 72.6 ± 12.9 months after surgery; p = 0.038) (Fig. 3).
No other correlations were found between BME and the other variables analysed.
Discussion
The main finding of this study was that the presence of BME in MRIs performed after ACL injury correlated with the prognosis at mid/long-term follow-up.
The analysis of 134 MRIs performed within six months after trauma allowed us to underline several aspects concerning frequency, evolution, and significance of BME. In regard to frequency, in our series BME was detected in 55.2 % of the patients evaluated for an acute ACL injury. In agreement with several authors we observed a greater frequency of BME in the postero-lateral aspect of the tibia and the anterior half of the LFC, which can be explained by the pivot shift mechanism, commonly implicated in ACL injury [4, 8–13].
The BME rate in our survey falls within the range of that reported in the literature, namely, 33–90 % [2, 3, 14, 15]. This wide variability, as well as our relatively lower rate of BME, can be explained by the well-known resolution time of BME. As described by Bretlau et al. [16] on serial MRIs in 64 patients with an acute knee trauma, BME reduced over time until resolution, with only 12 % rate still detectable at 12 months. Miller et al. [17] also showed that most BMEs resolve within two to four months after injury. We also observed that the frequency of BME depends on the time that has elapsed after the trauma. In fact, within three months after trauma the BME rate was 65 %, whereas over three months it was reduced to 25 %.
Even if the evolution of BME is mainly a spontaneous resolution within three to 12 months after trauma, it is still unclear how the original trauma can affect the joint homeostasis, and consequently the prognosis. Some authors showed that the presence of BME can be considered as a sign of major trauma, with concomitant damage to other tissues. Illingworth et al. [18] focused on the correlation between BME and meniscal lesions, and documented the association of a large femoral bone bruise on MRI after acute ACL tears with an increased rate of meniscal tears. Similarly, Bisson et al. [14] showed that moderate-to-severe LTP bruising was associated with medial meniscal tears.
Other authors focused instead on the influence of the trauma causing BME on the cartilage. Theologis et al. [19] found a correlation between BME and articular cartilage injury, thus showing that in ACL reconstructed patients the cartilage overlying the BME presented signs of damage with altered extracellular matrix. Cartilage evaluated at 12 months’ follow-up had elevated T1ρ values compared to those of the surrounding tissue, thus suggesting that despite the resolution of BME, cartilage lesions persist. These results were confirmed also at longer follow-up by Faber et al. [20], who showed that cartilage thinned in the site of the initial BME by analyzing MRI performed six years after ACL lesion. Potter et al. [21] also showed that the size of BME at baseline was significantly associated with increased cartilage loss at follow-up, both for medial and lateral compartment injury. Moreover, after three years there was a mean rise in Outerbridge scores for all compartments. The degenerative changes in compartments unaffected by the initial bone bruise support the notion that chondral injury sustained at the time of the injury affects the overall cartilage homeostasis, resulting in a global degradation in joint integrity. Finally, Nishimori et al. [15] reached similar conclusions when evaluating BME and associated lesions in 39 patients with ACL rupture, i.e. bone bruise in ACL injury was correlated with cartilage lesions that can act as a catalyst to cause osteoarthritis even after a successful reconstruction.
In light of that, it appears logical to suppose that such an important trauma, which has such deleterious consequences on the joint tissues, might also affect the prognosis. However, results on this matter are controversial. Hanypsiak et al. [22] evaluated 44 patients who underwent ACL reconstruction, and did not find any correlation between the presence of bone bruise at the time of injury and the clinical outcome at 12 years follow-up. Also Costa-Paz et al. [23] failed to find any correlation between BME and IKDC scores. Conversely, other authors showed a correlation between BME and symptoms. Johnson et al. [24] found that patients with a bone bruise had protracted clinical recovery. The analysis at short-term follow-up of 20 patients with BME lesions and 20 patients without them showed more effusions and pain at matched time intervals and a slower return to motion and non-antalgic gait in those with evidence of bone bruising. Szopek et al. [25] confirmed the significant relationship between pain and bone bruise by studying 17 patients at short-term follow up.
Although the joint tissue damage has been clearly proven, the available studies include too few evaluated patients and too short a follow-up to show clearly the correlation between BME and the clinical prognosis. Thus, in this study we tried to investigate the correlation of post-traumatic BME and mid/long-term prognosis after ACL injuries. No correlations were found between BME and symptoms or activity level in the overall group. However, since the evolution of most BMEs is spontaneous resolution, the evaluation of all MRIs from zero to six months might include many cases with minor injuries and thus without the alteration of the overall joint homeostasis. Although most BMEs tend to resolve, the ones persisting over time are likely to represent those associated with a major trauma. Thus, we focused on the analysis of the MRI obtained three months or more after trauma, and found that the persistence of BME in these MRIs correlated with a poorer prognosis. The analysis of the 32 patients who performed MRI more than three months after trauma showed that no patients with BME reached full sport recovery at the final follow-up. Conversely, 54 % of the patients without BME returned to 90 % of their previous level of sport, independently of the ACL reconstruction.
Another aspect to consider is that the joint tissue damage can variably affect patients with a different activity level. In fact, reconstructed and not reconstructed groups represented two different populations. These patients are very different with regards to age, sex, pre-injury activity level, and thus in terms of physical demands and expectations. The trauma entity might also differ between these two groups, as well as the impact of the tissue damage on the joint’s functional demands, and therefore this might have an overall final influence on the clinical results [26, 27]. In fact, further analysis revealed that, although no correlation could be found in the non-reconstructed ACL group, the group of sport-active patients, who underwent ACL reconstruction to recover their activity level, had a different return to sport rate according to the presence of BME. The group of ACL reconstructed patients consisted of a very athletic group, where 97 % of patients presented a pre-injury Tegner score ≥ 6. In this cohort, patients presenting oedema had a tendency towards a lower return to sport activity at one year compared with patients without BME. This protracted clinical recovery can be traced back to the documented early symptoms associated to BME, which are more effusion and pain, and a slower return to motion and non-antalgic gait [24]. Moreover, in this group of sport-active patients a higher BME area was correlated with a lower probability to return to the previous activity level at the mid/long-term follow-up. This might be due to the accelerated cartilage degeneration that has been shown to be associated with large BME. In fact, at a similar follow-up of five to seven years from trauma, BME has been shown to correlate with cartilage loss, with the whole knee joint integrity being probably already compromised [21].
This study has some limitations—first, the heterogeneity in the time that elapsed between trauma and MRI. Thus, some patients who suffered from BME after the trauma might not have been recognized, because MRI might have been performed after oedema resolution. Moreover, the oedema evaluated at different follow-ups can have different meanings, and evaluating BMEs found at various times together may complicate the results analysis. To limit this potential bias, we introduced the criteria of six months as the maximum time interval between trauma and MRI. Furthermore, we analysed earlier and later MRIs separately, which allowed us to show the importance of the BME when persisting over time. Patients were heterogeneous also with regards to the ACL surgery, but this might actually be a strength of this study, which allows the analysis of results to be extended to patients affected by ACL injury regardless of the surgical reconstruction and the particular technique chosen [28–34]. Another weakness of this study is its retrospective design. However, this is the largest series of patients evaluated at mid/long term follow-up, and it allowed us to show the importance of post-traumatic BME in terms of prognosis, as well as its different clinical impact according to the time after injury when BME is detected and to the type of patients affected by an ACL injury.
During ACL injury the entire joint undergoes a high-energy impact, which may compromise other tissues, thus affecting the long-term prognosis. Future research should aim at developing strategies to restore the overall joint homeostasis rather than just the ACL, thus allowing a better prognosis and a higher rate of return to full activity. BME has been an underestimated finding in ACL injured knees. Surgeons managing patients with ACL tears should be aware of the importance of BME in terms of prognosis and possibility to return to full sport activity.
Conclusion
This study highlighted the correlation between post-traumatic BME in patients affected by ACL injury and the clinical outcome over time. BME is a common finding, which decreases over time after injury, being detectable only in a minority of cases after more than three months. However, when BME is still detectable, it correlates with the clinical prognosis, and even in sport-active patients undergoing ACL reconstruction to regain previous sport level, a higher BME area is a negative predictive factor for a successful outcome at the mid/long-term follow-up.
References
Terzidis IP, Christodoulou AG, Ploumis AL, Metsovitis SR, Koimtzis M, Givissis P (2004) The appearance of kissing contusion in the acutely injured knee in the athletes. Br J Sports Med 38(5):592–596. doi:10.1136/bjsm.2003.006718
Jelic D, Masulovic D (2011) Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit Pregl 68(9):762–766
Dunn WR, Spindler KP, Amendola A, Andrish JT, Kaeding CC, Marx RG, McCarty EC, Parker RD, Harrell FE Jr, An AQ, Wright RW, Brophy RH, Matava MJ, Flanigan DC, Huston LJ, Jones MH, Wolcott ML, Vidal AF, Wolf BR (2010) Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. Am J Sports Med 38(9):1778–1787. doi:10.1177/0363546510370279
Fowler PJ (1994) Bone injuries associated with anterior cruciate ligament disruption. Arthroscopy 10(4):453–460
Mandalia V, Fogg AJ, Chari R, Murray J, Beale A, Henson JH (2005) Bone bruising of the knee. Clin Radiol 60(6):627–636. doi:10.1016/j.crad.2005.01.014
Khan MS, Seon JK, Song EK (2011) Risk factors for anterior cruciate ligament injury: assessment of tibial plateau anatomic variables on conventional MRI using a new combined method. Int Orthop 35(8):1251–1256. doi:10.1007/s00264-011-1217-7
Viskontas DG, Giuffre BM, Duggal N, Graham D, Parker D, Coolican M (2008) Bone bruises associated with ACL rupture: correlation with injury mechanism. Am J Sports Med 36(5):927–933. doi:10.1177/0363546508314791
Chin YC, Wijaya R, Chong LR, Chang HC, Lee YH (2014) Bone bruise patterns in knee injuries: where are they found? Eur J Orthop Surg Traumatol 24(8):1481–1487. doi:10.1007/s00590-013-1319-6
Davies NH, Niall D, King LJ, Lavelle J, Healy JC (2004) Magnetic resonance imaging of bone bruising in the acutely injured knee–short-term outcome. Clin Radiol 59(5):439–445. doi:10.1016/j.crad.2003.11.012
Rosen MA, Jackson DW, Berger PE (1991) Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy 7(1):45–51
Sanders TG, Medynski MA, Feller JF, Lawhorn KW (2000) Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics 20:S135–S151. doi:10.1148/radiographics.20.suppl_1.g00oc19s135
Speer KP, Spritzer CE, Bassett FH 3rd, Feagin JA Jr, Garrett WE Jr (1992) Osseous injury associated with acute tears of the anterior cruciate ligament. Am J Sports Med 20(4):382–389
Yoon KH, Yoo JH, Kim KI (2011) Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am 93(16):1510–1518. doi:10.2106/JBJS.J.01320
Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM (2013) A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med 41(8):1801–1807. doi:10.1177/0363546513490649
Nishimori M, Deie M, Adachi N, Kanaya A, Nakamae A, Motoyama M, Ochi M (2008) Articular cartilage injury of the posterior lateral tibial plateau associated with acute anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 16(3):270–274. doi:10.1007/s00167-007-0458-x
Bretlau T, Tuxoe J, Larsen L, Jorgensen U, Thomsen HS, Lausten GS (2002) Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc 10(2):96–101. doi:10.1007/s00167-001-0272-9
Miller MD, Osborne JR, Gordon WT, Hinkin DT, Brinker MR (1998) The natural history of bone bruises. A prospective study of magnetic resonance imaging-detected trabecular microfractures in patients with isolated medial collateral ligament injuries. Am J Sports Med 26(1):15–19
Illingworth KD, Hensler D, Casagranda B, Borrero C, van Eck CF, Fu FH (2013) Relationship between bone bruise volume and the presence of meniscal tears in acute anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 22(9):2181–2186. doi:10.1007/s00167-013-2657-y
Theologis AA, Kuo D, Cheng J, Bolbos RI, Carballido-Gamio J, Ma CB, Li X (2011) Evaluation of bone bruises and associated cartilage in anterior cruciate ligament-injured and -reconstructed knees using quantitative t(1rho) magnetic resonance imaging: 1-year cohort study. Arthroscopy 27(1):65–76. doi:10.1016/j.arthro.2010.06.026
Faber KJ, Dill JR, Amendola A, Thain L, Spouge A, Fowler PJ (1999) Occult osteochondral lesions after anterior cruciate ligament rupture. Six-year magnetic resonance imaging follow-up study. Am J Sports Med 27(4):489–494
Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S (2012) Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med 40(2):276–285. doi:10.1177/0363546511423380
Hanypsiak BT, Spindler KP, Rothrock CR, Calabrese GJ, Richmond B, Herrenbruck TM, Parker RD (2008) Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med 36(4):671–677. doi:10.1177/0363546508315468
Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L (2001) Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy 17(5):445–449. doi:10.1053/jars.2001.23581
Johnson DL, Bealle DP, Brand JC Jr, Nyland J, Caborn DN (2000) The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med 28(2):152–155
Szkopek K, Warming T, Neergaard K, Jorgensen HL, Christensen HE, Krogsgaard M (2012) Pain and knee function in relation to degree of bone bruise after acute anterior cruciate ligament rupture. Scand J Med Sci Sports 22(5):635–642. doi:10.1111/j.1600-0838.2011.01297.x
Conteduca F, Caperna L, Ferretti A, Iorio R, Civitenga C, Ponzo A (2013) Knee stability after anterior cruciate ligament reconstruction in patients older than forty years: comparison between different age groups. Int Orthop 37(11):2265–2269. doi:10.1007/s00264-013-2050-y
Struewer J, Ziring E, Oberkircher L, Schuttler KF, Efe T (2013) Isolated anterior cruciate ligament reconstruction in patients aged fifty years: comparison of hamstring graft versus bone-patellar tendon-bone graft. Int Orthop 37(5):809–817. doi:10.1007/s00264-013-1807-7
Struewer J, Frangen TM, Ishaque B, Bliemel C, Efe T, Ruchholtz S, Ziring E (2012) Knee function and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using bone-patellar tendon-bone graft: long-term follow-up. Int Orthop 36(1):171–177. doi:10.1007/s00264-011-1345-0
Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A (2011) Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop 35(7):1093–1097. doi:10.1007/s00264-011-1206-x
Chechik O, Amar E, Khashan M, Lador R, Eyal G, Gold A (2013) An international survey on anterior cruciate ligament reconstruction practices. Int Orthop 37(2):201–206. doi:10.1007/s00264-012-1611-9
Feller J, Webster KE (2013) Return to sport following anterior cruciate ligament reconstruction. Int Orthop 37(2):285–290. doi:10.1007/s00264-012-1690-7
Struewer J, Ziring E, Frangen TM, Efe T, Meissner S, Buecking B, Bliemel C, Ishaque B (2013) Clinical outcome and prevalence of osteoarthritis after isolated anterior cruciate ligament reconstruction using hamstring graft: follow-up after two and ten years. Int Orthop 37(2):271–277. doi:10.1007/s00264-012-1653-z
Hu J, Qu J, Xu D, Zhou J, Lu H (2013) Allograft versus autograft for anterior cruciate ligament reconstruction: an up-to-date meta-analysis of prospective studies. Int Orthop 37(2):311–320. doi:10.1007/s00264-012-1720-5
Streich NA, Reichenbacher S, Barie A, Buchner M, Schmitt H (2013) Long-term outcome of anterior cruciate ligament reconstruction with an autologous four-strand semitendinosus tendon autograft. Int Orthop 37(2):279–284. doi:10.1007/s00264-012-1757-5
Acknowledgments
F. Perdisa, M. Ciancio: II Clinic - Biomechanics Laboratory, Rizzoli Orthopaedic Institute, Bologna, Italy. E. Pignotti, K. Smith: Task Force, Rizzoli Orthopaedic Institute, Bologna, Italy.
Competing interests
All the authors of the present paper declare no competing interests with regard to the results and contents of the present study.
Declaration on ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Filardo, G., Kon, E., Tentoni, F. et al. Anterior cruciate ligament injury: post-traumatic bone marrow oedema correlates with long-term prognosis. International Orthopaedics (SICOT) 40, 183–190 (2016). https://doi.org/10.1007/s00264-015-2672-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2672-3