Abstract
Objective
To review the MRI appearances of tubal and non-tubal implantation sites in ectopic pregnancy.
Conclusion
Transvaginal ultrasound is the primary imaging modality in ectopic pregnancy and MRI is used as a problem-solving tool in selected indications as detailed in the article. MRI features of tubal, interstitial, cervical, cesarean scar, cornual, ovarian, abdominal, and heterotopic pregnancies are provided to familiarize the radiologists with their appearances thereby assisting them in making early and accurate diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Ectopic pregnancy (EP) is defined as a condition in which the fertilized ovum or blastocyst implants and grows anywhere outside the endometrial cavity and accounts for 2% of all pregnancies [1, 2]. EP, without timely diagnosis and intervention, may be associated with rupture, hemorrhage, hypovolemic shock, and death. Maternal mortality is significantly increased with tubal rupture (with tubal rupture also having an impact on future fertility) which accounts for 4% of pregnancy-related deaths [3]. Apart from being the leading cause of maternal mortality in the first trimester, the incidence of EP is showing an increasing trend. Late primiparity, infertility, intrauterine contraceptive device, assisted reproductive techniques (ART), tubal surgeries, pelvic inflammatory disease, and endometriosis are primary causes for the increased incidence of EP [4].
Classically, an EP is diagnosed based on clinical features, transvaginal ultrasonography (TVUS) findings, and beta human chorionic gonadotropin (hCG) levels; however, patient factors (such as: obesity, presence of bowel gas and pain) combined with operator experience may sometimes limit the usefulness of TVUS. On these occasions, further imaging may be required to ascertain the diagnosis, site, and complications related to EP [5, 6].
While MRI is frequently used especially with inconclusive sonography in various acute gynecological emergencies like torsion, hemorrhage within ovarian cyst, pelvic abscesses, as well as in non-gynaecologic emergencies presenting in pregnancy such as acute appendicitis, it is not conventionally used in the diagnosis of EP. However in several cases, is a useful problem-solving tool and may assist management planning in complicated or rare forms of EP [7, 8].
In this article, we discuss the role of MRI in the diagnosis of common, uncommon, and rare types of EP and the utility of MRI for management decisions of EP.
Diagnosis of ectopic pregnancy
Clinical features
EP has variable clinical presentations. Typically, women of child-bearing age present with a short history of amenorrhea (approximately 6–8 weeks), lower abdominal pain, and vaginal bleeding after a missed period. Rupture of an EP (commonly at 6–8 weeks) can lead to severe abdominal pain, rebound tenderness, and dropping hematocrit. These symptoms are neither sensitive, nor specific, and can occur with other pregnancy-related or unrelated complications. Further limiting the usefulness of clinical findings is the fact that up to 50% of patients with EP are asymptomatic; hence it is good practice to document the site of pregnancy in all women with a positive UPT [5].
Beta hCG
A serum beta hCG level higher than 1500 mIU/ml is suggestive of EP in the appropriate clinical setting after excluding intrauterine pregnancy (IUP). A single positive test of serum beta hCG level is of less clinical utility than serial tests. A doubling time of 50% in a 48 h interval is noted in normal IUP, while it is less than 50% in failing IUP or EP. However, serial beta hCG level estimation may not be feasible in an emergency setting. Moreover, a doubling time nearing that of IUP may be seen in up to 21% of EP [9, 10]
TVUS
TVUS is the initial and preferred modality of choice in the diagnosis of EP. It offers superior contrast resolution as compared to transabdominal ultrasonography, provides real time imaging, detects vascularity and demonstrates fetal cardiac activity through M mode Doppler. TVUS has a reported sensitivity of 69%–99% and specificity of 84%–99.9%. Lack of intrauterine gestational sac, thick echogenic cystic structure in the adnexa with “ring of fire” appearance on Doppler, associated tubal hematoma, or echogenic fluid in the pouch of Douglas are all imaging findings that may be seen on TVUS. A yolk sac or embryo with cardiac activity within the sac is highly specific but not commonly encountered [11, 12].
Role of MRI in ectopic pregnancy
MRI should be considered only in hemodynamically stable patients where the information from TVUS is inadequate or any specific added information is needed for patient management. MRI offers a larger field of view with excellent tissue contrast and characterization and can be useful when TVUS is limited by patient or operator factors [13]. It provides more specific tissue differentiation than TVUS and can accurately delineate fresh hemorrhagic contents and hemoperitoneum from ascites [14].
MRI protocol
MRI in pregnancy should always be focussed to answer the clinical question while using the minimum number of low energy pulse sequences required. If an IUP has not been excluded, then one should attempt to keep the specific absorption rate (SAR) as low as possible to further minimize the already extremely low risk to the fetus. A detailed MRI protocol for evaluation of EP is generally similar to a protocol designed to evaluate acute abdominal pain or bleeding in a pregnant woman. Various sequences and their benefits are discussed in Table 1 [8, 15,16,17] but generally consist of single-shot fast spin echo and balanced steady-state free precession sequences with or without fat suppression.
Indications
The specific indications of MRI in the diagnosis and treatment of EP are listed below.
-
(1)
MRI is indicated in the diagnosis of EP when TVUS has a limited role from factors such as severe tenderness, body habitus, bowel gas, co-existence of ovarian mass, and limited operator experience.
-
(2)
In a non-interstitial tubal pregnancy, a large tubal hematoma and hemoperitoneum may obscure visualization of the gestational sac, and MRI is useful to ascertain the diagnosis, site, and complications related to EP [18].
-
(3)
MRI has a role even in certain cases where TVUS has already diagnosed a tubal pregnancy. It is especially useful in correct topographic localization in patients with previous tubal surgeries or inflammation, those undergoing ART, when conservative management or laparoscopic surgery is being planned in patients who desire fertility preservation [19].
-
(4)
MRI is particularly useful in early diagnosis of interstitial pregnancy and to differentiate it from intrauterine and cornual pregnancy. Curettage often fails to demonstrate any trophoblastic tissue in cases of interstitial or intramural EP misdiagnosed as IUP and in those cases, MRI helps to demonstrate the interstitial or intramural location of EP [20].
-
(5)
MRI is indicated in certain cases to distinguish a cervical pregnancy from incomplete abortion, when TVUS is not diagnostic. In cases of misdiagnosis of the cervical ectopic as a miscarriage or incomplete abortion, dilatation and curettage may lead to severe potentially life-threatening hemorrhage [21].
-
(6)
Early diagnosis of Cesarean scar pregnancy may be achieved with MRI. Prompt diagnosis is essential in planning further management and reducing maternal morbidity. Complications such as bladder wall invasion are best detected on MRI [22, 23].
-
(7)
In cases of cornual pregnancies MRI helps in diagnosis, differentiation from other types of EP, and in prognostication [24, 25].
-
(8)
MRI has a limited role in an ovarian EP, but is sometimes useful to distinguish an ovarian EP from other cystic ovarian lesions such as corpus luteum, and decidualized endometriomas [15, 26].
-
(9)
In case of a pregnancy of unknown location (no sac identified on TVUS), MRI in indicated for localization of the pregnancy, including cases of abdominal pregnancy not localized on ultrasound [19, 22].
-
(10)
Acute abdomen in pregnancy is a clinical challenge, and MRI may be performed in select cases where TVUS and ultrasound are inconclusive, not only for detecting EP, but for the diagnosis of other non-gynaecologic emergencies in pregnancy-like acute appendicitis and acute cholecystitis. MRI also has a role in gynaecologic emergencies like hemorrhage into an ovarian cyst, torsion of adnexal cysts and masses, and conditions unique to pregnancy-like red degeneration of fibroid. In these cases, ultrasound has a limited role, and CT carries the risk of ionizing radiation to the fetus (biologic dose is as high at 35 msv), which is damaging in the initial periods of organogenesis, notably the same time in which EP usually presents [8, 27, 28].
Contraindications
If there is suspicion of rupture of EP with hypotension, falling hematocrit, and urgent need for surgical management, MRI delays patient care and generally should not be performed. Other relative contraindications to MRI in general include: claustrophobia, non-compatible cardiac pacemakers, cochlear implants, and other metallic devices [15, 29].
Although MRI carries no risk of ionizing radiation to the fetus, biologic effects such as tissue heating have been described. In a pregnant woman, especially those with possible IUP or heterotopic pregnancy, MRI can be performed after explaining the unknown risks to the patient. In a large population-based study performed in Ontario Canada, MRI was not shown to be related with any adverse maternal or fetal outcomes in any trimester of pregnancy. Limited MRI sequences with the lowest SAR should be performed and only when there are clear benefits of the investigation outweighing possible risks [30, 31].
Gadolinium-enhanced MRI is rarely indicated in the diagnosis of EP and should be considered only to delineate the gestational sac when there is difficulty in the identification of the sac within a tubal hematoma or hemoperitoneum, to assess vascularity in cases of alternate diagnosis such as ovarian torsion with mass, and to look for active bleeding. Intravenous gadolinium-based contrast agents are classified as pregnancy category C drugs by the United States Food and Drug Administration suggesting that the results of animal studies have shown an adverse effect on the fetus, but adequate studies are not available in humans. Hence, traditionally it has been suggested that intravenous gadolinium should be avoided if an IUP is possible and cannot be excluded [32, 33]. More recently, the study by Ray JG et al. showed associations between still birth, neonatal deaths, various skin conditions, and gadolinium exposure in utero which further emphasizes that gadolinium should not be used if there is a chance of a viable IUP and considered only when absolutely necessary [30].
MR imaging appearances in ectopic pregnancy
EP occurs most commonly in the fallopian tubes and less commonly in the cervix, previous Cesarean scar, rudimentary horn of a unicornuate uterus, the ovary, peritoneal cavity, and even abdominal organs and the thoracic diaphragm [34]. Most of the features seen on MRI have similar correlates and are derived from ultrasound. Hence it is essential to be familiar with the typical sonographic appearances of EP for optimal and prompt reporting of MRI. Sonographic appearances of different types of EP have been extensively published in the literature and hence here we are restricting ourselves to the MRI appearances of EP.
Non-interstitial tubal pregnancy
This is the most common site, accounting for approximately 97% of EP (50%–80% in the ampulla, 10%–25% in the isthmus, and 5%–17% in the fimbrial end) [13, 35]. Complex adnexal mass separate from the ovary with absent IUP is the most common imaging appearance of tubal EP. On TVUS, a thick echogenic cystic structure is seen in the adnexal region separate from the ovary, with associated echogenic adnexal mass, representing a hematosalpinx [36, 37]. Similarly MRI shows an oval or round extrauterine gestational sac lateral to the uterus, with a cystic appearance and a trilaminar wall on T2 images has been reported in 81% cases: outer hypointensity representing tubal wall, inner hypointensity corresponding to the extra-embryonic celom/amnion, and middle characteristic T2 hyperintensity corresponding to chorionic villus tissue with distinct linear- or dot-like areas of T2 low signal within, corresponding to blood vessels [29]. The sac may contain non-specific liquid, enhancing papillary, dot- or tree-like solid components, fresh blood, or fluid-fluid level. Fresh or acute tubal hematoma occurs as a result of rupture of tubal intramural arterioles caused by trophoblastic invasion, and appears as T1 hyperintense, with a distinct low signal on T2-weighted images [18, 27] (Fig. 1).
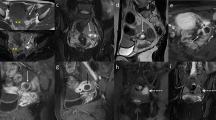
Tubal ectopic pregnancy. Twenty-nine-year-old woman with 11 weeks amenorrhea, vaginal spotting, and lower abdominal pain for 2 days. A–C Axial fat-saturated T2-weighted MRI of pelvis (A), axial T1-weighted pre-contrast (B), and axial T1-weighted post-contrast MRI of pelvis (C) shows large midline subacute pelvic hematoma with T1 hyperintensity and T2 shading (asterisk) with left hydrosalpinx (short arrow). Small irregular cystic structure on the left side (long arrows) with blood products and irregular peripheral enhancement (long arrows in C) in close relation to the hematoma suggesting ruptured left tubal ectopic pregnancy
Hemoperitoneum, seen even in unruptured EP (as a result of spillage from the blood-filled tube through the fimbrial end), appears as mildly hyperintense on T1 images, compared with urine in the bladder, and hypointense on T2 images depending on the age of the blood products (Fig. 2). Although hemoperitoneum in the pouch of Douglas in a pregnant woman has a 93% positive predictive value for EP, other causes of hemoperitoneum such as ruptured ovarian cysts, corpus luteum, placenta accreta, and spontaneous abortion must be borne in mind [15, 37].
Tubal ectopic pregnancy. Thirty-two-year-old woman with 7 weeks amenorrhea and acute lower abdominal pain. Beta hCG was positive with no obvious intrauterine pregnancy. A Axial T2-weighted MRI of pelvis shows pelvic fluid with fluid levels of varying signal intensity (arrow). B Axial T1-weighted out-of-phase image shows dependent T1 hyperintensity in the fluid (arrow). Overall features suggest acute on subacute hematoma. No intrauterine or ectopic pregnancy could be identified on MRI. Laparoscopy confirmed hemoperitoneum and right salpingectomy was done due to suspicion of ectopic pregnancy and histopathology confirmed tubal pregnancy
The corpus luteum of pregnancy may sometimes be confused with the gestational sac. It is situated in the ovary and typically has high T1 signal intensity in its wall, whereas it is often hypointense in an unruptured gestational sac. It can be associated with acute hemorrhage and resolves spontaneously by the end of the second trimester [26].
Post-contrast fat-suppressed images, after an IUP has been excluded, can help better delineate the gestational sac when there is difficulty in the identification of the sac within a tubal hematoma or hemoperitoneum; these are usually well-enhancing thick cystic structures and clearly visualized even in the background of hematoma. Tubal enhancement (related to increased vascularity post implantation) and enhancing papillary projections of placental tissue may be identified within the tube, reported in 81% of the cases [29, 38]. MRI has a high diagnostic accuracy for EP. According to a study by Takahashi A et al., the presence of a direct sign or at least two indirect signs raised the diagnostic accuracy of MRI to 100%. Direct sign includes the detection of ectopic gestational sac, while indirect signs included tubal dilatation with hemosalpinx, adnexal hematoma, and hemorrhagic ascites [39].
Interstitial pregnancy
Interstitial pregnancy is one in which implantation of the blastocyst occurs in the intramural segment of the fallopian tube, just as it takes off from the cornua or lateral angle of the uterus. It comprises 2% of all ectopic pregnancies [40]. This segment of the tube is completely surrounded by myometrium and allows greater distensibility of the sac, with the result that rupture is late with more severe hemorrhage, given the proximity to the intramyometrial arcuate vasculature, and uterine perforation in some cases. Maternal mortality is up to 15 times higher than non-interstitial tubal EP [14, 41].
On TVUS, signs such as the “interstitial line sign,” “myometrial mantle sign,” and “bulging sign” require significant operator expertise, and diagnosis may be missed or delayed on TVUS [14, 42, 43]. MRI is of definite clinical utility in doubtful cases. Studies have shown that the presence of an intact junctional zone between the gestational sac and the uterine cavity is suggestive of interstitial pregnancy and are surrounded by < 5 mm myometrium all around [20, 44] (Fig. 3). In contrast in angular pregnancy, implantation occurs at the lateral angle of the uterine cavity, medial to the uterotubal junction and is not associated with myometrium or junctional zone medial to the sac, and typically demonstrates a wide angle of contact with uterine cavity [14, 45]. MRI, owing to its ability to tissue characterization, helps differentiate an interstitial pregnancy from gestational trophoblastic disease. The latter is usually associated with disruption of the junctional zone [18, 27].
Interstitial pregnancy. Thirty-two-year-old woman with 8 weeks amenorrhea with no definite intrauterine pregnancy. A and B Coronal (A) and Axial (B) T2-weighted MRI of pelvis shows small irregular cystic gestational sac-like structure (arrows) lateral to the right cornua with preserved junctional zone (asterisk) suggestive of interstitial pregnancy. C Axial fat-saturated T1-weighted MRI of pelvis shows T1 hyperintense contents in the endometrial cavity (arrows) suggestive of blood products
Cervical pregnancy
A cervical pregnancy is one in which implantation occurs in the endocervical canal of the cervix uteri, below the level of the internal os, and accounts for less than 1% of ectopic pregnancies [40]. Typically, the uterus assumes an “hour-glass” or “figure of eight” appearance, with the narrow waist of the hourglass represented by the internal os, with a ballooned cervix [5].
Ultrasound shows a rounded sac below the level of the internal os, with surrounding echogenic margins of the “decidualized” cervical stroma. MRI may demonstrate a heterogeneous hemorrhagic mass with enhancing papillary components of the placenta distending the cervical canal. A T2 hypointense rim is seen around the mass [21, 44] (Fig. 4).
Cervical pregnancy. Thirty-seven-year-old woman who underwent fertility treatment presented with 12 weeks amenorrhea and vaginal spotting. A Axial T2-weighted MRI of pelvis shows cystic gestational sac-like structure (arrow) in the cervical canal with hourglass appearance of the uterus. B Coronal T2-weighted MRI of pelvis demonstrated the fetus inside the cervical gestational sac (arrow) and the developing placenta on the left side invading the cervical stroma (asterisk). C Sagittal T2-weighted MRI of pelvis shows the cervical gestational sac (long arrow) with partially open internal os (black asterisk). Note made of cesarean scar superior to implantation (short arrow) and myometrial contraction (white asterisk)
Cervical pregnancy has to be differentiated from incomplete abortion. In cases of misdiagnosis of the cervical ectopic as incomplete abortion, dilatation and curettage may lead to severe potentially life-threatening hemorrhage, owing to the increased vascularity of the pregnant cervix, and lack of muscular tamponade effect of cervical fibrous stroma. Although TVUS may provide clues such as presence of hematometra, open internal os, lack of fetal cardiac activity, and no increase in stromal vascularity in incomplete abortion, MRI is useful in earlier diagnosis and prompt management. It may demonstrate a well-defined gestational sac surrounded by T2 hypointense stromal ring, and absence of T1 hyperintense fluid in the endometrial cavity [4, 14, 18, 44].
Cesarean scar pregnancy
Cesarean scar pregnancy in defined as implantation of the blastocyst in a previous lower segment Cesarean scar, where the myometrium is thinned with associated fibrosis. This comprises approximately 6% of pregnancies in women with a prior Cesarean section [46]. It carries a substantial risk of maternal morbidity and mortality related to uterine dehiscence, rupture, hemorrhage due to placenta previa and morbidly adherent placenta, pregnancy failure and future fertility. This is because the invasion of trophoblastic tissue occurs in an area of scarred myometrium where there is paucity of the decidual layer of endometrium, similar to early placenta accreta [47].
TVUS may demonstrate a gestational sac which is located eccentrically and anteriorly in the inferior body of uterus (above the internal os) with thinning of the anterior wall of uterus [2]. When in doubt, MRI helps delineate the exact site of the gestational sac within the lower segment of uterus in the region of previous Cesarean scar, with significant thinning of the overlying T2 hypointense anterior myometrium (Fig. 5). Sometimes there may be no myometrium visualized between the sac and the urinary bladder [13, 48].
Cesarean scar pregnancy. Thirty-year-old woman with 12 weeks amenorrhea and intermittent lower abdominal pain for 1 week. A–C Sagittal T2-weighted (A), sagittal fat-saturated T2-weighted (B) and sagittal fat-saturated T1-weighted (C) MRI of pelvis scans show thick-walled gestational sac (arrows) within anterior lower uterine segment scar, with adjacent myometrial thinning (dotted arrow in B). Endometrial cavity shows T1 hyperintense and T2 heterogenous contents (black asterisks) suggestive of blood products. Note made of myometrial contraction (white asterisk in A)
Differentials include a low lying pregnancy and a cervical pregnancy; the former does not assume an eccentric anterior location, while the latter distends the cervical canal [22]. Prompt diagnosis is essential in planning further management and reducing maternal morbidity. Similar to a cervical EP, dilatation and curettage of an undiagnosed Cesarean scar pregnancy can lead to scar rupture, severe hemorrhage, bladder injury, and incomplete evacuation due to deep penetration of the chorionic villus tissue into the fibrous scar [49].
Cornual pregnancy
Cornual pregnancy can occur in a rudimentary horn (communicating or non-communicating) of a unicornuate uterus, single horn of a bicornuate or septate uterus. It has an increased risk of uterine rupture, preterm labor, and abortion. This is because the myometrium in a rudimentary horn is often thin and has varying degrees of capability to placental attachment, and there may be a morbidly adherent placenta. Timely diagnosis helps prevent these complications [50, 51].
At TVUS, this can sometimes be confused with an interstitial pregnancy, especially in the setting of previously undiagnosed uterine anomaly, and MRI is increasingly preferred for accurate characterization. MRI findings have been classically described as a gestational sac within the cornua, surrounded by an outer ring whose signal intensity matches that of the main uterus, unlike an interstitial pregnancy which is within the myometrium (Figs. 6 and 7). The main uterus is displaced laterally and stretched by the enlarging horn and is called a “banana-shaped uterus.” The sac is described as lying more than 1 cm from the lateral wall of the endometrial cavity (to differentiate it from an interstitial pregnancy) [52, 53]. A ‘pseudopattern’ of an asymmetric bicornuate uterus, lack of a visual continuity between the cervical canal and the lumen of the pregnant horn, and presence of myometrial tissue surrounding the gestational sac, are certain features described in literature, which can guide in the diagnosis [25].
Cornual pregnancy. Twenty-two-year-old woman with 10 weeks amenorrhea and eccentric intrauterine pregnancy on transvaginal ultrasound (not shown here). A and B Axial T2-weighted (A) and coronal T2-weighted (B) MRI of pelvis show thick-walled gestational sac (arrows) with fetal parts in the left horn of an incomplete septate uterus. Right horn endometrial cavity shows T1 hyperintense (not shown here) and T2 heterogenous contents (asterisks) suggestive of blood products
Cornual pregnancy. Twenty-eight-year-old woman with 7 weeks amenorrhea and transvaginal ultrasound showed eccentric intrauterine pregnancy versus interstitial pregnancy (not shown here). A–C Coronal T2-weighted (A), axial T2-weighted (B), and axial fat-saturated T1-weighted (C) MRI of pelvis scans show small cystic gestational sac-like structure (arrows) lateral to left cornua with intact junctional zone but surrounded completely by myometrium suggesting non-communicating rudimentary horn pregnancy rather than an interstitial pregnancy. Gestational sac shows T1 hyperintensity (arrow in C) suggestive of blood. Empty endometrial cavity (asterisk) in the dominant horn
MRI is useful in the confident diagnosis of underlying mullerian duct anomalies providing more specific details like the uterine contour, presence or absence of communication between the rudimentary horn and the unicornuate uterus, and continuity of the rudimentary horn lumen with the cervix. MRI also helps in prognostication in terms of pregnancy outcome and surgical morbidity in a cornual pregnancy, and guide treatment planning, by detecting the thickness of myometrium in the rudimentary horn, and diagnosing placenta accreta which correlates with worse outcomes [15, 24].
Ovarian pregnancy
Ovarian EP is quite rare and account for about 0.5%–3% of all EP [34, 54]. On imaging, gestational sac-like structure with thick echogenic wall is identified, lying entirely within the ovary or arising from it, and not associated with hematosalpinx [55].
MRI has a limited role, and is sometimes useful to distinguish an ovarian EP from tubal EP and other cystic ovarian lesions such as corpus luteum. It is helpful in localizing the cystic structure to ovary thereby excluding tubal EP [15, 56]. Next step would be to differentiate ovarian EP and corpus luteal cyst which is commonly seen in early pregnancy. Both are located in the ovary and can contain hemorrhage. GS shows typical trilaminar pattern on T2 with slightly irregular wall showing heterogenous enhancement. In contrast corpus luteal cyst shows thin smooth T2 hypointense and mildly T1 hyperintense wall and shows homogenous enhancement [8, 26, 27]. In practice, it is hard to differentiate these two entities unless definite fetal pole or yolk sac could be demonstrated.
Theca lutein cysts are typically bilateral, multiple, occur in the setting of ovarian hyperstimulation, and have thin walls and no hemorrhage within. Other thin-walled ovarian functional cysts, chocolate cysts, and hemorrhagic cysts may also be accurately diagnosed on MRI [27].
Abdominal pregnancy
Abdominal pregnancy comprises 0.1%–1% of all EP, and includes sites such as the peritoneal cavity including the pouch of Douglas, the uterine serosa, the broad ligament, uterosacral ligaments, pelvic sidewall, large pelvic vessels, omentum, bowel, abdominal organs like liver and spleen, the retroperitoneum, and diaphragm [18, 57, 58]. They have an expected mortality rate of 5%–20% (up to 7.7 times higher than other ectopic pregnancies), because the placenta of an abdominal EP has the potential to invade surrounding organs, derive blood supply, and present quite late with significant morbidity and mortality [59, 60].
Theories of abdominal implantation are (1) primary implantation, and (2) secondary to a primarily tubal sac that aborts through the fimbrial end and reimplants in the peritoneal cavity. In cases where TVUS has failed to detect the site (pregnancy of unknown location), MRI may demonstrate an ectopic gestational sac in the peritoneal cavity, with hemoperitoneum and focal peritoneal enhancement [61, 62]. A fetus may be seen within the sac because these may present quite late, sometimes even at term. In fact, when presenting late, it is easier to confuse an abdominal EP with normal intrauterine pregnancy, rudimentary horn pregnancy, or uterine rupture. However, certain features such as a deformed non-round shape of the sac, absence of myometrial tissue around the gestational sac or amnion, abnormal location and shape of the placenta (like a flattened contour), oligohydramnios, and abnormal fetal lie may help to raise a suspicion of abdominal pregnancy [63] (Fig. 8).
Abdominal pregnancy. Twenty-six-year-old woman with 17 weeks amenorrhea. A–C Sagittal T2-weighted (A), axial T2-weighted (B), and axial fat-saturated T1-weighted (C) MRI of pelvis scans shows intraabdominal (cul de sac) pregnancy along the posterior aspect of uterus (arrow in A). Placenta is on the right pelvic side wall (asterisk in B). There was a hematosalpinx on the right (short arrow in C) and small volume hemoperitoneum (long arrow in C) on the left
MRI is usually diagnostic because it confirms the abdominal location of the pregnancy by demonstrating lack of T2 hypointense myometrium around the products of conception. It also detects site of placental attachment, which helps plan further management [64]. MR angiography may enable further planning by identifying the dominant vascular supply of the sac. Sometimes, the diagnosis of abdominal ectopic pregnancy may be missed, and a lithopedion may form and be detected incidentally at a later date [65].
Heterotopic pregnancy
Heterotopic pregnancy, in which there is simultaneous presence of pregnancies at two separate sites, usually a combination of IUP and EP, although thought to be rare and almost non-existent, has increased in incidence owing to ART. The reported incidence is one in 4000 pregnancies increasing to about one in 100 pregnancies in women undergoing ART [18, 56]. It is important to diagnose heterotopic pregnancy to minimize morbidity and mortality to both mother and the intrauterine fetus resulting from rupture of a missed concomitant EP.
Visualization of an intrauterine pregnancy may not completely exclude an EP, and the adnexa, ovaries, cervix, and pouch of Douglas must be thoroughly scanned, especially in clinically suspect patients. Sometimes, it may present as an abdominal emergency, after abortion or termination of an IUP, due to rupture of an undiagnosed EP. Imaging features are those of an IUP with associated decidual reaction, along with a coexisting extrauterine sac, usually tubal or ovarian (Fig. 9). There may be ancillary features of ovarian hyperstimulation, such as bilaterally enlarged ovaries or theca lutein cysts [14, 66].
Heterotopic pregnancy. Thirty-two-year-old woman with 8 weeks amenorrhea. A and B Coronal T2-weighted MRI of pelvis shows intrauterine gestational sac (asterisk) and irregular thick-walled right adnexal cystic structure separate from the right ovary (long arrow) suggestive of unruptured right tubal pregnancy. Also note the right ovarian small smooth-walled cystic lesion suggestive of corpus luteal cyst (short arrows)
MRI in these cases is controversial, especially in cases where continuation of intrauterine pregnancy is desired, because there are not enough studies proving the safety of MRI in the first trimester, when organogenesis is at its peak. Nonetheless, it may prove useful in certain clinical scenarios, weighing the potential benefits against possible risks to the fetus [22, 38].
Conclusion
EP once a rare entity, is demonstrating a rising incidence in recent years and remains the leading cause of maternal mortality in the first trimester. MRI is not conventionally used in the diagnosis of EP, but can be a problem-solving tool, and help plan further management in complicated or rare forms of EP where TVUS is non-diagnostic or inconclusive. MRI has a high diagnostic accuracy for EP, owing to its multiplanar capabilities, larger FOV, and unique ability to identify tissue characteristics and blood products. It is especially useful in correct topographic localization in patients with previous tubal surgeries or inflammation, those undergoing ART, and when conservative management or laparoscopic surgery is being planned. It is essential for the radiologist to be oriented to the MR imaging appearance of EP as this diagnosis should be considered in any woman of reproductive age presenting with acute abdomen, hemoperitoneum, or adnexal mass. In conclusion, precise knowledge of the clinical presentations and imaging characteristics of the common as well as rare form of EP, and using MRI as a diagnostic tool in the relevant cases, will go a long way in improving patient outcome.
References
Ectopic pregnancy–United States, 1990–1992 (1995). MMWR Morb Mortal Wkly Rep 44 (3):46–48
Jurkovic D, Wilkinson H (2011) Diagnosis and management of ectopic pregnancy. BMJ 342:d3397
Creanga AA, Shapiro-Mendoza CK, Bish CL, et al. (2011) Trends in ectopic pregnancy mortality in the United States: 1980–2007. Obstet Gynecol 117(4):837–843. https://doi.org/10.1097/AOG.0b013e3182113c10
Condous G (2004) The management of early pregnancy complications. Best Pract Res Clin Obstet Gynaecol 18(1):37–57. https://doi.org/10.1016/j.bpobgyn.2003.09.011
Lin EP, Bhatt S, Dogra VS (2008) Diagnostic clues to ectopic pregnancy. Radiographics 28(6):1661–1671. https://doi.org/10.1148/rg.286085506
Tenore JL (2000) Ectopic pregnancy. Am Fam Physician 61(4):1080–1088
Oto A, Ernst RD, Ghulmiyyah LM, et al. (2009) MR imaging in the triage of pregnant patients with acute abdominal and pelvic pain. Abdom Imaging 34(2):243–250. https://doi.org/10.1007/s00261-008-9381-y
Knoepp US, Mazza MB, Chong ST, Wasnik AP (2017) MR imaging of pelvic emergencies in women. Magn Reson Imaging Clin N Am 25(3):503–519. https://doi.org/10.1016/j.mric.2017.03.009
Lipscomb GH, Stovall TG, Ling FW (2000) Nonsurgical treatment of ectopic pregnancy. N Engl J Med 343(18):1325–1329. https://doi.org/10.1056/nejm200011023431807
Seeber BE, Barnhart KT (2006) Suspected ectopic pregnancy. Obstet Gynecol 107(2 Pt 1):399–413. https://doi.org/10.1097/01.AOG.0000198632.15229.be
Braffman BH, Coleman BG, Ramchandani P, et al. (1994) Emergency department screening for ectopic pregnancy: a prospective US study. Radiology 190(3):797–802. https://doi.org/10.1148/radiology.190.3.7509494
Condous G, Okaro E, Khalid A, et al. (2005) The accuracy of transvaginal ultrasonography for the diagnosis of ectopic pregnancy prior to surgery. Hum Reprod 20(5):1404–1409. https://doi.org/10.1093/humrep/deh770
Tamai K, Koyama T, Togashi K (2007) MR features of ectopic pregnancy. Eur Radiol 17(12):3236–3246. https://doi.org/10.1007/s00330-007-0751-6
Chukus A, Tirada N, Restrepo R, Reddy NI (2015) Uncommon implantation sites of ectopic pregnancy: thinking beyond the complex adnexal mass. Radiographics 35(3):946–959. https://doi.org/10.1148/rg.2015140202
Parker RA, Yano M, Tai AW, et al. (2012) MR imaging findings of ectopic pregnancy: a pictorial review. Radiographics 32(5):1445–1460 (discussion 1460-1442). https://doi.org/10.1148/rg.325115153
Yoshigi J, Yashiro N, Kinoshita T, O’Uchi T, Kitagaki H (2006) Diagnosis of ectopic pregnancy with MRI: efficacy of T2*-weighted imaging. Magn Reson Med Sci 5(1):25–32
Schieda N, Isupov I, Chung A, Coffey N, Avruch L (2017) Practical applications of balanced steady-state free-precession (bSSFP) imaging in the abdomen and pelvis. J Magn Reson Imaging 45(1):11–20. https://doi.org/10.1002/jmri.25336
Kao LY, Scheinfeld MH, Chernyak V, et al. (2014) Beyond ultrasound: CT and MRI of ectopic pregnancy. AJR Am J Roentgenol 202(4):904–911. https://doi.org/10.2214/ajr.13.10644
Masselli G, Derme M, Piccioni MG, et al. (2018) To evaluate the feasibility of magnetic resonance imaging in predicting unusual site ectopic pregnancy: a retrospective cohort study. Eur Radiol . https://doi.org/10.1007/s00330-017-5237-6
Filhastre M, Dechaud H, Lesnik A, Taourel P (2005) Interstitial pregnancy: role of MRI. Eur Radiol 15(1):93–95. https://doi.org/10.1007/s00330-004-2306-4
Jung SE, Byun JY, Lee JM, Choi BG, Hahn ST (2001) Characteristic MR findings of cervical pregnancy. J Magn Reson Imaging 13(6):918–922
Koroglu M, Kayhan A, Soylu FN, et al. (2013) MR imaging of ectopic pregnancy with an emphasis on unusual implantation sites. Jpn J Radiol 31(2):75–80. https://doi.org/10.1007/s11604-012-0151-y
Peng KW, Lei Z, Xiao TH, et al. (2014) First trimester caesarean scar ectopic pregnancy evaluation using MRI. Clin Radiol 69(2):123–129. https://doi.org/10.1016/j.crad.2013.07.021
Srisajjakul S, Prapaisilp P, Bangchokdee S (2017) Magnetic resonance imaging in tubal and non-tubal ectopic pregnancy. Eur J Radiol 93:76–89. https://doi.org/10.1016/j.ejrad.2017.05.023
Tsafrir A, Rojansky N, Sela HY, Gomori JM, Nadjari M (2005) Rudimentary horn pregnancy: first-trimester prerupture sonographic diagnosis and confirmation by magnetic resonance imaging. J Ultrasound Med 24(2):219–223
Tamai K, Koyama T, Saga T, et al. (2006) MR features of physiologic and benign conditions of the ovary. Eur Radiol 16(12):2700–2711. https://doi.org/10.1007/s00330-006-0302-6
Jung SE, Byun JY, Lee JM, et al. (2001) MR imaging of maternal diseases in pregnancy. AJR Am J Roentgenol 177(6):1293–1300. https://doi.org/10.2214/ajr.177.6.1771293
Kereshi B, Lee KS, Siewert B, Mortele KJ (2017) Clinical utility of magnetic resonance imaging in the evaluation of pregnant females with suspected acute appendicitis. Abdom Radiol (NY). https://doi.org/10.1007/s00261-017-1300-7
Si MJ, Gui S, Fan Q, et al. (2016) Role of MRI in the early diagnosis of tubal ectopic pregnancy. Eur Radiol 26(7):1971–1980. https://doi.org/10.1007/s00330-015-3987-6
Ray JG, Vermeulen MJ, Bharatha A, Montanera WJ, Park AL (2016) Association between MRI exposure during pregnancy and fetal and childhood outcomes. JAMA 316(9):952–961. https://doi.org/10.1001/jama.2016.12126
Yip YP, Capriotti C, Talagala SL, Yip JW (1994) Effects of MR exposure at 1.5 T on early embryonic development of the chick. J Magn Reson Imaging 4(5):742–748
Prola-Netto J, Woods M, Roberts VHJ, et al. (2018) Gadolinium chelate safety in pregnancy: barely detectable gadolinium levels in the juvenile nonhuman primate after in utero exposure. Radiology 286(1):122–128. https://doi.org/10.1148/radiol.2017162534
Patenaude Y, Pugash D, Lim K, et al. (2014) The use of magnetic resonance imaging in the obstetric patient. J Obstet Gynaecol Can 36(4):349–363
Bouyer J, Coste J, Fernandez H, Pouly JL, Job-Spira N (2002) Sites of ectopic pregnancy: a 10 year population-based study of 1800 cases. Hum Reprod 17(12):3224–3230
Breen JL (1970) A 21 year survey of 654 ectopic pregnancies. Am J Obstet Gynecol 106(7):1004–1019
Pellerito JS, Taylor KJ, Quedens-Case C, et al. (1992) Ectopic pregnancy: evaluation with endovaginal color flow imaging. Radiology 183(2):407–411. https://doi.org/10.1148/radiology.183.2.1561341
Russell SA, Filly RA, Damato N (1993) Sonographic diagnosis of ectopic pregnancy with endovaginal probes: what really has changed? J Ultrasound Med 12(3):145–151
Kataoka ML, Togashi K, Kobayashi H, et al. (1999) Evaluation of ectopic pregnancy by magnetic resonance imaging. Hum Reprod 14(10):2644–2650
Takahashi A, Takahama J, Marugami N, et al. (2013) Ectopic pregnancy: MRI findings and clinical utility. Abdom Imaging 38(4):844–850. https://doi.org/10.1007/s00261-012-9969-0
Shan N, Dong D, Deng W, Fu Y (2014) Unusual ectopic pregnancies: a retrospective analysis of 65 cases. J Obstet Gynaecol Res 40(1):147–154. https://doi.org/10.1111/jog.12146
Lau S, Tulandi T (1999) Conservative medical and surgical management of interstitial ectopic pregnancy. Fertil Steril 72(2):207–215
Ackerman TE, Levi CS, Dashefsky SM, Holt SC, Lindsay DJ (1993) Interstitial line: sonographic finding in interstitial (cornual) ectopic pregnancy. Radiology 189(1):83–87. https://doi.org/10.1148/radiology.189.1.8372223
Jafri SZ, Loginsky SJ, Bouffard JA, Selis JE (1987) Sonographic detection of interstitial pregnancy. J Clin Ultrasound 15(4):253–257
Dibble EH, Lourenco AP (2016) Imaging Unusual Pregnancy Implantations: Rare Ectopic Pregnancies and More. AJR Am J Roentgenol 207(6):1380–1392. https://doi.org/10.2214/ajr.15.15290
Baldawa PS, Chaudhari HK (2008) Angular ectopic pregnancy presenting as rupture of lateral wall of the uterus. J Hum Reprod Sci 1(1):33–34
Seow KM, Huang LW, Lin YH, et al. (2004) Cesarean scar pregnancy: issues in management. Ultrasound Obstet Gynecol 23(3):247–253. https://doi.org/10.1002/uog.974
Timor-Tritsch IE, Monteagudo A, Cali G, et al. (2014) Cesarean scar pregnancy and early placenta accreta share common histology. Ultrasound Obstet Gynecol 43(4):383–395. https://doi.org/10.1002/uog.13282
Wu R, Klein MA, Mahboob S, Gupta M, Katz DS (2013) Magnetic resonance imaging as an adjunct to ultrasound in evaluating cesarean scar ectopic pregnancy. J Clin Imaging Sci 3:16. https://doi.org/10.4103/2156-7514.109758
Nonaka M, Toyoki H, Imai A (2006) Cesarean section scar pregnancy may be the cause of serious hemorrhage after first-trimester abortion by dilatation and curettage. Int J Gynaecol Obstet 95(1):50–51. https://doi.org/10.1016/j.ijgo.2006.06.019
Saleem SN (2003) MR imaging diagnosis of uterovaginal anomalies: current state of the art. Radiographics 23(5):e13. https://doi.org/10.1148/rg.e13
Smolders D, Deckers F, Pouillon M, et al. (2002) Ectopic pregnancy within a rudimentary horn in a case of unicornuate uterus. Eur Radiol 12(1):121–124. https://doi.org/10.1007/s003300100939
Jayasinghe Y, Rane A, Stalewski H, Grover S (2005) The presentation and early diagnosis of the rudimentary uterine horn. Obstet Gynecol 105(6):1456–1467. https://doi.org/10.1097/01.aog.0000161321.94364.56
Malinowski A, Bates SK (2006) Semantics and pitfalls in the diagnosis of cornual/interstitial pregnancy. Fertil Steril 86(6):1764. https://doi.org/10.1016/j.fertnstert.2006.03.073
Raziel A, Schachter M, Mordechai E, et al. (2004) Ovarian pregnancy-a 12-year experience of 19 cases in one institution. Eur J Obstet Gynecol Reprod Biol 114(1):92–96. https://doi.org/10.1016/j.ejogrb.2003.09.038
Marcus SF, Brinsden PR (1993) Primary ovarian pregnancy after in vitro fertilization and embryo transfer: report of seven cases. Fertil Steril 60(1):167–169
Oliver R, Malik M, Coker A, Morris J (2007) Management of extra-tubal and rare ectopic pregnancies: case series and review of current literature. Arch Gynecol Obstet 276(2):125–131. https://doi.org/10.1007/s00404-006-0311-3
Ozdemir I, Demirci F, Yucel O, Alper M (2003) Primary omental pregnancy presenting with hemorrhagic shock. A case report. Gynecol Obstet Invest 55(2):116–118. https://doi.org/10.1159/000070188
Poole A, Haas D, Magann EF (2012) Early abdominal ectopic pregnancies: a systematic review of the literature. Gynecol Obstet Invest 74(4):249–260. https://doi.org/10.1159/000342997
Atrash HK, Friede A, Hogue CJ (1987) Abdominal pregnancy in the United States: frequency and maternal mortality. Obstet Gynecol 69(3 Pt 1):333–337
Perkins KM, Boulet SL, Kissin DM, Jamieson DJ (2015) Risk of ectopic pregnancy associated with assisted reproductive technology in the United States, 2001–2011. Obstet Gynecol 125(1):70–78. https://doi.org/10.1097/aog.0000000000000584
Cohen JM, Weinreb JC, Lowe TW, Brown C (1985) MR imaging of a viable full-term abdominal pregnancy. AJR Am J Roentgenol 145(2):407–408. https://doi.org/10.2214/ajr.145.2.407
Wagner A, Burchardt AJ (1995) MR imaging in advanced abdominal pregnancy. A case report of fetal death. Acta Radiol 36(2):193–195
Liu J, Khan A, Johnson S, Grigorian C, Li T (2014) The usefulness of gestational sac and placental sonographic morphology in differentiating between second-trimester tubal and abdominal pregnancy: case report and a review of literature. J Clin Ultrasound 42(3):162–168. https://doi.org/10.1002/jcu.22076
Lockhat F, Corr P, Ramphal S, Moodley J (2006) The value of magnetic resonance imaging in the diagnosis and management of extra-uterine abdominal pregnancy. Clin Radiol 61(3):264–269. https://doi.org/10.1016/j.crad.2005.10.013
Malian V, Lee JH (2001) MR imaging and MR angiography of an abdominal pregnancy with placental infarction. AJR Am J Roentgenol 177(6):1305–1306. https://doi.org/10.2214/ajr.177.6.1771305
Soriano D, Shrim A, Seidman DS, et al. (2002) Diagnosis and treatment of heterotopic pregnancy compared with ectopic pregnancy. J Am Assoc Gynecol Laparosc 9(3):352–358
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ramanathan, S., Raghu, V., Ladumor, S.B. et al. Magnetic resonance imaging of common, uncommon, and rare implantation sites in ectopic pregnancy. Abdom Radiol 43, 3425–3435 (2018). https://doi.org/10.1007/s00261-018-1604-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1604-2