Abstract
Ectopic pregnancy (EP), in which a fertilized ovum implants outside the uterine cavity, is the leading cause of pregnancy-related death in the first trimester. EP is usually suspected by a positive pregnancy test and an empty uterus on transvaginal sonography (TVS). Although TVS is the initial modality of choice, it may occasionally fail to demonstrate the implantation site. When TVS findings are indeterminate, magnetic resonance imaging (MRI) may provide better delineation of the focus of EP owing to its excellent tissue contrast. The key MRI features of EP include gestational sac (GS)-like structures that typically appear as a cystic sac-like structure, frequently associated with surrounding acute hematoma of distinct low intensity on T2-weighted images. In tubal pregnancy, an enhanced tubal wall on postcontrast images may be another diagnostic finding. Ruptured EP is inevitably associated with acute hematoma outside these structures. In intrauterine EP, recognition of the relationship between GS-like structure and the myometrium can aid in differentiating from normal pregnancy. Diagnostic pitfalls include heterotopic pregnancy, decidual changes in endometrial cyst and theca lutein cysts mimicking GS-like structures. Knowledge of a spectrum of clinical and MRI features of EP is essential for establishing an accurate diagnosis and determining appropriate management.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ectopic pregnancy (EP), in which a fertilized ovum implants outside the uterine cavity, is the most common emergency in early pregnancy. Although the mortality rate of EP has decreased, the incidence has greatly increased in the last few decades [1]. This increased incidence may be attributed to the growing number of the risk factors such as pelvic inflammatory disease, endometriosis, previous tubal surgery, infertility treatment and late primiparity. EP commonly occurs in the fallopian tube, but rarely in unusual sites including the interstitium, cervix, cesarean scar, anomalous rudimentary horn of the uterus and abdominal cavity [2]. Since none of these anatomic sites can accommodate placental attachment, EP is a potentially life-threatening condition associated with rupture and subsequent massive bleeding. Thus, the prompt and accurate diagnosis of EP in an unruptured stage is mandatory for determining appropriate treatment.
EP is basically treated by laparoscopy. Although medical treatment with methotrexate is gaining favor among gynecologists, the selection criteria for the latter treatment differ among the investigators. Some advocate methotrexate as an option when the gestational mass measures less than 3.5 cm in greatest diameter, when there is no significant evidence of hemoperitoneum, and when a living extrauterine embryo has not been visualized [3]. Methotrexate therapy is contraindicated in case of heterotopic pregnancy (EP with normal intrauterine pregnancy), unless the patient does not wish to maintain the intrauterine pregnancy. The usefulness of emergency or preventive arterial embolization for controlling hemorrhage has also been reported in cervical, interstitial and abdominal pregnancy [4, 5].
Transvaginal sonography (TVS) is highly accurate in the diagnosis of EP with a reported sensitivity of 69–99% and specificity of 84–99.9%, and is generally used as the initial modality for its convenience and cost-effectiveness [6–10]. Nonetheless, TVS occasionally may fail to delineate the focus of EP because of its limited tissue contrast, resolution and field of view. When TVS findings are indeterminate, magnetic resonance imaging (MRI) can serve as a problem-solving tool owing to its excellent tissue contrast. The advantage of MRI for the diagnosis of EP has been reported to be its capability to identify fresh blood and to precisely localize the site of implantation [11, 12]. The recognition of MRI findings in EP is essential for accurate interpretation of this condition. In this article, we illustrate clinical and MRI features of EP in correlation with TVS and laparoscopic findings, and present key findings and pitfalls of MRI for the diagnosis of EP.
Pathologic features
A vast majority (97%) of EP occurs in the fallopian tube: 55% in the ampulla, 25% in the isthmus and 17% in the fimbria. Other unusual locations of EP are extrauterine sites including the ovary and peritoneal cavity, or intrauterine sites including the interstitium, cervix, cesarean scar and anomalous rudimentary uterine horn [2]. In tubal pregnancy, the gestational sac consists of embryonal and tubal tissue. Following the implantation of the ovum in the tubal epithelium, chorionic villi and trophoblasts grow intraluminally or penetrate into the tubal wall to form the placenta. Trophoblastic cells can extensively invade into the muscles and vessels. The maternal vessels often rupture into the gestational sac, subsequently resulting in tubal hematoma (hematosalpinx).
Clinical features
In unruptured tubal pregnancy, patients typically present with amenorrhea for 6–8 weeks after the last menstrual period with no or minimal symptoms, or they occasionally complain of lower abdominal pain and vaginal bleeding. EP is sometimes complicated by rupture, which may be a life-threatening surgical emergency due to massive hemorrhage and is the leading cause of maternal mortality in the first trimester of pregnancy. Women with a history of previous EP may be more likely to develop ruptured tubal pregnancy [13]. Tubal rupture typically occurs at 6–8 weeks after the last menstrual period, and the common clinical presentations include acute severe abdominal pain, guarding and rebound tenderness at physical examination, hemodynamic instability and dropping hematocrit [14]. Early diagnosis of rupture is crucial because ruptured tubal pregnancy requires immediate surgical intervention with salpingectomy, whereas unruptured EP can be treated conservatively or with salpingostomy with conceptus removal. Despite the recent advances of imaging modalities, diagnosis of rupture and determination of the need for surgery still depends on the clinical status of the patient, since no reliable imaging findings indicative of tubal rupture have been established [15]. As compared with tubal pregnancy, rare forms of EP such as abdominal or interstitial pregnancy tend to be diagnosed later and have a higher risk of disastrous hemorrhage or uterine rupture [16]. Although rare, recognition of these rare types of EP is also important for determining appropriate management and surgical planning.
Diagnostic approach
EP can be initially suspected by the absence of an intrauterine gestational sac (GS) on TVS and a serum hCG level higher than 1,500 mIU/ml [17]. TVS is highly accurate for the diagnosis of EP with a reported sensitivity of 69–99% and specificity of 84–99.9% [6–10]. However, TVS may occasionally fail to detect extrauterine GS in the presence of tubal hematoma or hemoperitoneum, and furthermore, extrauterine GS can mimic corpus luteum cysts or theca lutein cysts. Although an adnexal echogenic mass indicates tubal hematoma, which is an indirect sign of EP, it can simulate hydrosalpinx, tubo-ovarian abscess or intraperitoneal hematoma due to abdominal pregnancy. In interstitial pregnancy, the intrauterine GS may be misinterpreted as normal pregnancy.
The role of MRI is mainly to confirm or better define suspected EP, especially when TVS fail to demonstrate focus of EP or to distinguish it from incomplete abortion. The demonstration of GS is of particular importance when laparoscopic surgery is considered. The advantage of MRI is that it can identify fresh blood owing to its excellent tissue contrast [11], and it can also accurately localize the site of abnormal implantation, even if EP exists in unusual sites. Postcontrast images may provide better delineation of GS even in the presence of tubal hematoma or hemoperitoneum. Another expected role of MRI is to differentiate among acute emergency situations, such as ovarian torsions, ovarian hemorrhage and pelvic inflammatory disease [18]. Even in the presence of normal intrauterine pregnancy, MR has an excellent potential to diagnose acute appendicitis [19]. However, the utility of MRI may be limited in hemodynamically unstable patients, especially due to ruptured EP.
We perform pelvic MRI with a 1.5-T MR unit (Symphony; Siemens AG, Erlangen, Germany) using a six-channel phased-array coil. Prior to MR examination, intramuscular injection of hypotonic drugs such as butylscopolamine or glucagon is given to reduce motion artifacts due to intestinal peristalsis. After obtaining localizing images of the female pelvis, we perform the following pulse sequences: (1) sagittal T1-weighed spin-echo imaging (TR/TE, 565-600/10-15 ms; section thickness, 5 mm; intersection gap, 1.5 mm; field of view, 26 cm; matrix, 512×384; number of slices, 19; number of acquisitions, 1) and (2) transverse and sagittal T2-weighted fast spin-echo imaging (TR/TE, 3,700-5,000/80–120 ms; echo-train length, 15; section thickness, 5 mm; intersection gap, 1.5 mm; field of view, 26–32 cm; matrix, 512×384; number of slices, 19; number of acquisitions, 2). Coronal section can be added or be an alternative to the sagittal section. Contrast-enhanced images may be selectively obtained with the acquisition of written informed consent when non-enhanced MR images are considered to be inconclusive or equivocal. Contrast-enhanced MRI is performed with T1-weighed spin-echo or gradient-echo sequence in both the transverse and sagittal plane after intravenous administration of gadolinium. The combined use of the fat-suppression technique is recommended since it can improve the visualization of an abnormal implantation site owing to exclusion of pelvic fat signals. Contrast-enhanced MRI has been reported to be useful for the diagnosis of tubal pregnancy by demonstrating enhancement in the placental tissues and the affected tubal wall [11], even if non-enhanced MR images are indeterminate due to the presence of a large hematoma or hemoperitoneum.
Radiologists should be alert to the fact that MRI should be performed when normal intrauterine pregnancy can be definitely excluded on TVS. In the presence of normal pregnancy, MR examination is not recommended in the first trimester, although no adverse effect to human has been reported [20, 21]. Moreover, the use of gadolinium is contra-indicated in pregnancy because of its teratogenic effect shown in animal studies [20].
MRI features of EP
Tubal pregnancy
Typical radiologic features in tubal pregnancy
Tubal pregnancy is the most common form of EP, accounting for approximately 98% of all EP. Most of tubal pregnancy occurs in the ampulla (75–80%), followed by the isthmus (10–15%) and fimbria (5%) [22]. At laparoscopy, the affected fallopian tube typically shows a sausage-shaped distention due to containing hematoma (Fig. 1). The most specific radiologic finding of EP is identification of extrauterine GS, which is typically demonstrated as a thick echogenic ring-like structure on TVS [23] and as a sac-like cystic structure surrounded by a thick wall on MRI (Fig. 1). The wall of the GS-like structure typically exhibits high intensity on T2-weighed images containing areas of distinct low intensity [24]. The GS-like structure is usually associated with fresh hemorrhage, which is demonstrated as an area of intermediate or high signal intensity on T1-weighed images and distinct low intensity on T2-weighed images (Figs. 1, 2, 3) [11]. It is important not to confuse a corpus luteum cyst with a GS-like structure. A corpus luteum cyst exists in the ovary and typically has a thick wall showing a slightly increased intensity on T1-weighted images and relatively low intensity on T2-weighted images [18], but rarely contains acute hematoma with distinct low intensity on T2-weighted images.
Left tubal pregnancy in a 38-year-old woman at 6 weeks’ gestation. (a) Transvaginal sonogram shows a thick echogenic ring-like structure (arrow) in the left fallopian tube adjacent to the left ovary (ov). (b) Sagittal T2-weighted magnetic resonance (MR) image shows a cystic GS-like structure in the left fallopian tube, surrounded by a thick wall of predominantly high intensity (arrow). (c) Sagittal T1-weighted image shows homogeneously hypointense thick wall (arrow). (d) Sagittal postcontrast T1-weighted image with fat suppression clearly demonstrates the enhancement in both the wall of the GS-like structure (arrow) and the dilated tubal wall (arrowhead). (e) Laparoscopy revealed a sausage-shaped distention of the ampullary portion of the left fallopian tube with a dusky red serosal surface (arrows). Salpingotomy with conceptus removal was performed to maintain her fertility
Right tubal pregnancy in a 33-year-old woman at 11 weeks’ gestation. (a) Transvaginal sonogram shows a heterogeneous echogenic mass in the right adnexa (arrows), but failed to demonstrate the focus of implantation. (b) Sagittal T2-weighted magnetic resonance (MR) image shows a right adnexal mass of heterogeneous signal intensity, indicating tubal hematoma (arrow). Small areas of prominent low intensity within the mass indicate fresh hemorrhage. (c) Sagittal T1-weighted image demonstrates the mass shows mixed low and high intensity (arrow). (d) Sagittal postcontrast T1-weighted image shows heterogeneous enhancement in the mass, suggesting the presence of placental tissues (arrow)
Left tubal pregnancy in a 32-year-old woman at 9 weeks’ gestation. (a) Sagittal T2-weighted magnetic resonance (MR) image shows a cystic GS-like structure (arrow) surrounded by area of distinct low intensity (arrowhead), representing fresh hematoma. (b) Sagittal T1-weighted image shows slightly increased intensity in the wall of the GS (arrow) and surrounding hematoma. (c) Sagittal postcontrast T1-weighted image with fat suppression clearly demonstrates the GS with ring-like enhancement (arrow) associated with prominent tubal wall enhancement (arrowheads), which can allow definitive diagnosis of tubal pregnancy
When noncontrast images are indeterminate, postcontrast images may allow more accurate detection of a GS-like structure by demonstrating a thick enhanced wall that can be detected even in the presence of hematoma (Figs. 3, 4) [11]. Occasionally, the placental tissues may be demonstrated as papillary solid components within the dilated tube (Fig. 4) or as a large heterogeneously enhancing mass associated with acute hemorrhage (Fig. 2). The recognition of wall enhancement of dilated tubal structure is another key MRI finding indicating suspicion of tubal pregnancy, which may reflect increased vascularity of the tubal wall following implantation [11]. The presence of enhanced tubal wall surrounding the GS-like structure is another useful sign in differentiating it from a corpus luteum cyst.
Left tubal pregnancy in a 21-year-old woman at 8 weeks’ gestation. (a) Sagittal T2-weighted magnetic resonance (MR) image shows pelvic fluid of high intensity (asterisk) and hematoma of intermediate signal intensity (double asterisks) surrounding the cystic lesion. GS-like structure is not evident on this image. (b) Sagittal T1-weighted image shows that both pelvic fluid and hematoma exhibit slightly high intensity compared to that of urine, indicating hemorrhagic fluid. (c) Sagittal postcontrast T1-weighted image with fat suppression demonstrates enhanced wall of a dilated tube (arrowheads) associated with papillary enhancing mural nodule indicating placental tissues (arrow). The cystic structure posterior to the site of EP is a follicle of the left ovary
A substantial amount of hematoma or hemorrhagic ascites may be associated even in unruptured tubal pregnancy, which typically shows higher signal intensity than that of the urine in the bladder on T1-weighed images, and they may often hinder the recognition of implantation site (Fig. 4). In such instances, postcontrast images may be more helpful for the diagnosis of EP by demonstrating tubal wall enhancement and enhancing placental tissues (Fig. 4).
Ruptured tubal pregnancy
Rupture of tubal wall is the most clinically important complication of tubal pregnancy and commonly occurs at near the end of the 2nd month of gestation due to destruction of the tubal wall by the invading trophoblast. This condition is often a life-threatening surgical emergency due to massive bleeding and is the leading cause of maternal mortality in the first trimester of pregnancy. The diagnosis of tubal rupture is essentially made on clinical presentations including acute severe abdominal pain, guarding and rebound tenderness at physical examination, hemodynamic instability and dropping hematocrit. A moderate to large amount of echogenic pelvic fluid can be commonly observed on TVS. However, since a substantial amount of pelvic fluid is also seen in 70% of EP and in 30% of normal pregnancy [23], the presence of pelvic fluid is not suggestive of tubal rupture [15]. Although any specific MRI findings for the diagnosis of tubal rupture have not been described, the disruption of tubal wall enhancement and the presence of acute hematoma showing distinct low intensity on T2-weighed images located outside the implantation sites may indicate tubal rupture in symptomatic patients. In the absence of this finding, the suspicion of ruptured EP may depend on clinical settings.
Non-tubal intraperitoneal pregnancy
Abdominal pregnancy
Abdominal pregnancy is an extremely rare form of EP, accounting for approximately 0.1% of all EP, and can be primary or secondary to a tubal pregnancy that aborts out of the fimbria and reimplants in the peritoneal cavity [25, 26]. Since the pregnancy can potentially continue to term, this condition is associated with considerably high morbidity and mortality due to delayed diagnosis and usually requires surgical intervention. At MRI, GS-like structure associated with hematoma may be depicted in the Douglas pouch. In such cases, enhancement of the peritoneum around the GS-like structure may also be a clue to suspect this condition (Fig. 5). MR angiography may allow detecting the origin of the vascular supply of the placenta that can aid surgical planning [27]. Other rare sites of EP in the abdomen included the omentum [28, 29], liver [30] and spleen [31].
Abdominal pregnancy in a 29-year-old woman with pelvic pain at 8 weeks’ gestation. (a) Transvaginal sonogram shows a hypoechoic mass (arrowheads) in the left adnexa suggesting hematoma, which mimics left tubal pregnancy. A GS-like structure is not identified. (b) Axial T2-weighted magnetic resonance (MR) image shows a GS-like structure (arrow) posterior to hematoma in the Douglas pouch. (c) Laparoscopy reveals a hemorrhagic mass (arrows) firmly attached to the left uterosacral ligament
Ovarian pregnancy
Ovarian pregnancy is the implantation of a fertilized ovum confined to the ovary, accounting for 0.5–3% of all EP [32–34]. Unlike tubal pregnancy, this condition is associated with neither pelvic inflammatory disease nor infertility. The presenting symptoms are similar to those of EP in other sites. In this condition, the distinction between GS-like structure and ovarian functional cysts may become problematic. Unlike GS-like structure, corpus luteum cysts do not contain acute hematomas with distinct low intensity on T2-weighted images as described above [18]. Ovarian follicles and theca lutein cysts usually have thin walls [18].
Intrauterine EP
Interstitial pregnancy
Interstitial pregnancy is defined as implantation at the proximal part of the fallopian tube, which is embodied within the muscular wall of the uterus. Since patients with interstitial pregnancy tend to present later in gestation compared with those with tubal pregnancy, this condition may be associated with increased risk of uterine rupture. However, the early diagnosis of interstitial pregnancy is often challenging since it can be occasionally misdiagnosed as normal intrauterine pregnancy or angular pregnancy on TVS [35]. Occasionally, a fetus may be recognized in the enlarged GS. At MRI, interstitial pregnancy can be highly suspected by recognition of a GS-like structure located lateral to the cornua surrounded by the myometrium (Fig. 6) [16, 35–37]. The presence of the intact junctional zone between the uterine cavity and the GS-like structure may also support the diagnosis [35], and this finding implies that the GS is not within the uterine cavity.
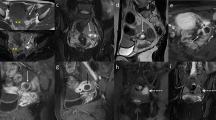
Interstitial pregnancy in a 37-year-old woman treated with IVF at 9 weeks’ gestation. (a) Transvaginal sonogram demonstrates a GS-like structure (arrows) with a fetus inside the sac. Fetal heart beat (FHB) could not be detected. (b) Axial T2-weighted magnetic resonance (MR) image shows a cystic GS-like structure (arrows) at the right uterine cornu, surrounded by a thick wall of heterogeneous signal intensity. (c) Axial postcontrast T1-weighted image shows heterogeneous enhancement in the wall of the GS-like structure (arrows). The GS-like structure is contiguous to the myometrium (arrowheads), suggesting that the lesion originates from the myometrium
Cervical pregnancy
Cervical pregnancy is the implantation in the cervical mucosa below the level of the internal os. This condition may clinically mimic ongoing spontaneous abortion, gestational trophoblastic disease, or low-lying placenta. Even with TVS or MRI, cervical pregnancy may not be accurately differentiated from ongoing abortion. Although polypoid adenomyoma with hemorrhage protruding into the cervical canal may mimic cervical pregnancy, negative pregnancy test can readily exclude this condition [38]. Reported MRI finding of cervical pregnancy is a heterogeneous hemorrhagic mass with enhancing papillary components of retained fetoplacental tissues (Fig. 7) [16, 39, 40]. The absence of expanded uterine cavity and dilated internal os, which is caused by retained products of conception and associated bleeding, may be more suggestive of cervical pregnancy than ongoing abortion.
Cervical pregnancy in a 37-year-old woman treated with IVF with vaginal bleeding and abdominal pain at 7 weeks’ gestation. Sagittal T2-weighted magnetic resonance (MR) image shows a cystic GS-like structure of predominantly high intensity in the cervical canal (arrow), containing foci of distinct low intensity. A uterine leiomyoma (M) in the anterior myometrium is also demonstrated
Cesarean scar pregnancy
Cesarean scar pregnancy is the implantation at the site of incision from a previous cesarean delivery. Although successful births have been reported [41], the risk of uterine rupture always exists, even in the first trimester. Early diagnosis is crucial for determining appropriate management to preserve uterine integrity and infertility. MRI may be useful in delineating the GS-like structure within the lower segment of the anterior wall of the uterus corresponding to the location of a previous cesarean section. The markedly thinned myometrium between the GS-like structure and the urinary bladder on T2-weighed images can be a key finding to diagnose this condition (Fig. 8) [16, 42].
Cesarean scar pregnancy in a 38-year-old woman at 7 weeks’ gestation. Sagittal T2-weighted magnetic resonance (MR) image shows a GS-like structure within the lower segment of the anterior uterine wall, corresponding to the cesarean scar (arrow). Markedly thinned myometrium between GS-like structure and the urinary bladder can be a clue to diagnose this condition
Pregnancy in an anomalous rudimentary horn of unicornuate uterus
The identification of correctly classifying uterine malformation is of importance, since a certain type of uterine anomaly may be complicated with abnormal pregnancy. The unicornuate uterus, which accounts for approximately 20% of müllerian duct anomalies, is caused by failure of development of the unilateral mullerian duct. The rudimentary uterine horn is present in 65% of cases, and it is classified into noncavitary horn without associated endometrium (33%), cavitary horn communicating with the endometrium of the contralateral horn (10%), and cavitary but non-communicating horn (22%) [43]. Although rare, pregnancy even in a non-communicating rudimentary horn is possible when the migration of spermatozoa occurs through the peritoneal cavity or through an unseen communication between the rudimentary horn and the main uterus [44]. At MRI, the contralateral main uterus is laterally deviated and shows a characteristic elongated shape, which is called “banana-shaped uterus” [45]. EP in a rudimentary horn is recognized as a GS-like structure surrounded by a thick wall, whose inner layer may show decreased intensity producing layering appearance, and the outer layer shows identical signal intensity to that of the outer myometrium of the main uterus on all sequences (Fig. 9).
Rudimentary horn pregnancy in a 32-year-old woman at 7 weeks’ gestation. (a) Axial T2-weighted magnetic resonance (MR) image shows a cystic GS-like structure surrounded by a thick wall in the right adnexal region (arrow). The contralateral unicornuate uterus shows laterally deviated shape. (b) Axial postcontrast T1-weighted image with fat suppression shows marked enhancement of the thick wall similar to that of the outer myometrium of the unicornuate uterus
Diagnostic pitfalls
Heterotopic pregnancy
Heterotopic pregnancy is a clinical condition defined by simultaneous coexistence of EP and normal intrauterine pregnancy. Although this condition can spontaneously occur in one of 2600 pregnancies (0.04%), the incidence is as high as 3% in women treated with assisted conceptions [46]. Thus, a careful evaluation is necessary even when the intrauterine sac has been visualized on TVS in women with assisted conceptions. MRI has an excellent modality for detecting both intra- and extrauterine pregnancy, although the indication of MRI should be carefully determined if the maintenance of intrauterine pregnancy is desired.
Decidual changes in endometrial cysts
Decidual changes of endometrial tissue in endometrial cysts can be seen in patients with EP. At MRI, the decidualized endometrial tissues can manifest as mural nodules along the wall of the hemorrhagic cyst, which may simulate secondary neoplasms arising from endometrial cysts such as clear cell carcinomas and endometrioid adenocarcinomas [18, 47]. Although the possibility of malignancy cannot be always excluded, the combination of the signal intensity of mural nodules similar to that of the decidualized endometrium on all sequences and the patient’s pregnant condition may favor the diagnosis of decidual changes in endometrial cysts (Fig. 10).
Decidual change of endometrial cyst of the left ovary in a 29-year-old woman. (a) Sagittal T2-weighted magnetic resonance (MR) image shows a hypointense mass containing hyperintense areas (arrows), which may simulate hematoma of tubal pregnancy. (b) Sagittal T1-weighted image shows a mass is predominantly high intensity. This signal pattern is typical for endometrial cyst. Solid components of low intensity (arrows) are identified corresponding to hyperintense areas on T2-weighted image. (c) Sagittal postcontrast T1-weighted image shows enhancement in the solid components (arrows). Hyperintense signal of the solid components on T2-weighted image similar to that of the decidualized endometrium (not shown) indicates decidual change of the ectopic endometrial tissues in the endometrial cyst
Theca lutein cysts associated with pregnancy
In patients with EP, theca lutein cysts can develop in response to increased hCG level. At MRI, theca lutein cysts appear as multiple, variably sized cystic lesions in bilateral symmetric enlarged ovaries [24]. Although theca lutein cysts may often simulate GS-like structures, the wall of these cysts is usually thin and does not contain acute hemorrhage unlike GS-like structures. Postcontrast images may be helpful since GS-like structure is usually associated with linear enhancement of the surrounding tubal wall. Recognition of these MRI findings may be helpful for avoiding misinterpretation of these physiologic changes as focus of EP.
Conclusion
MRI is an excellent problem-solving modality to confirm or better define suspected EP, especially when TVS fail to demonstrate focus of EP or to distinguish from incomplete abortion. In emergency conditions, MRI may also play an important role in differentiating EP from other acute diseases, and thus facilitate determining appropriate management of the patients. The key MRI features for the diagnosis of EP include GS-like structure that typically appears as a cystic sac-like structure, frequently associated with acute hematomas of distinct low intensity on T2-weighted images. In tubal pregnancy, recognition of an enhanced tubal wall on postcontrast images can be another diagnostic finding. In cases of uncommon forms of EP outside the tube, identification of GS-like structure and lack in enhancement of the tubal wall can be suggestive findings of these conditions. In intrauterine EP, recognition of a relationship between GS-like structure and the myometrium may be helpful in differentiating it from normal pregnancy. Precise knowledge of a spectrum of clinical and MRI features of EP is essential for establishing accurate diagnosis and determining appropriate management.
References
Condous G (2004) The management of early pregnancy complications. Best Pract Res Clin Obstet Gynaecol 18:37–57
Della-Giustina D, Denny M (2003) Ectopic pregnancy. Emerg Med Clin North Am 21:565–584
Patel MD (2006) “Rule out ectopic”: Asking the right questions, getting the right answers. Ultrasound Q 22:87–100
Ophir E, Singer-Jordan J, Oettinger M, Odeh M, Tendler R, Feldman Y, Fait V, Bornstein J (2004) Uterine artery embolization for management of interstitial twin ectopic pregnancy: case report. Hum Reprod 19:1774–1777
Badawy SZ, Etman A, Singh M, Murphy K, Mayelli T, Philadelphia M (2001) Uterine artery embolization: the role in obstetrics and gynecology. Clin Imaging 25:288–295
Sadek AL, Schiotz HA (1995) Transvaginal sonography in the management of ectopic pregnancy. Acta Obstet Gynecol Scand 74:293–296
Braffman BH, Coleman BG, Ramchandani P, Arger PH, Nodine CF, Dinsmore BJ, Louie A, Betsch SE (1994) Emergency department screening for ectopic pregnancy: a prospective US study. Radiology 190:797–802
Brown DL, Doubilet PM (1994) Transvaginal sonography for diagnosing ectopic pregnancy: positivity criteria and performance characteristics. J Ultrasound Med 13:259–266
Condous G, Okaro E, Khalid A, Lu C, Van Huffel S, Timmerman D, Bourne T (2005) The accuracy of transvaginal ultrasonography for the diagnosis of ectopic pregnancy prior to surgery. Hum Reprod 20:1404–1409
Shalev E, Yarom I, Bustan M, Weiner E, Ben-Shlomo I (1998) Transvaginal sonography as the ultimate diagnostic tool for the management of ectopic pregnancy: experience with 840 cases. Fertil Steril 69:62–65
Kataoka ML, Togashi K, Kobayashi H, Inoue T, Fujii S, Konishi J (1999) Evaluation of ectopic pregnancy by magnetic resonance imaging. Hum Reprod 14:2644–2650
Nishino M, Hayakawa K, Kawamata K, Iwasaku K, Takasu K (2002) MRI of early unruptured ectopic pregnancy: detection of gestational sac. J Comput Assist Tomogr 26:134–137
Latchaw G, Takacs P, Gaitan L, Geren S, Burzawa J (2005) Risk factors associated with the rupture of tubal ectopic pregnancy. Gynecol Obstet Invest 60:177–180
Saxon D, Falcone T, Mascha EJ, Marino T, Yao M, Tulandi T (1997) A study of ruptured tubal ectopic pregnancy. Obstet Gynecol 90:46–49
Frates MC, Brown DL, Doubilet PM, Hornstein MD (1994) Tubal rupture in patients with ectopic pregnancy: diagnosis with transvaginal US. Radiology 191:769–772
Ha HK, Jung JK, Kang SJ, Koong SE, Kim SJ, Kim JY, Shinn KS (1993) MR imaging in the diagnosis of rare forms of ectopic pregnancy. AJR Am J Roentgenol 160:1229–1232
Tenore JL (2000) Ectopic pregnancy. Am Fam Physician 61:1080–1088
Tamai K, Koyama T, Saga T, Kido A, Kataoka M, Umeoka S, Fujii S, Togashi K (2006) MR features of physiologic and benign conditions of the ovary. Eur Radiol 16:2700–2711
Pedrosa I, Levine D, Eyvazzadeh AD, Siewert B, Ngo L, Rofsky NM (2006) MR imaging evaluation of acute appendicitis in pregnancy. Radiology 238:891–899
Levine D (2006) Obstetric MRI. J Magn Reson Imaging 24:1–15
Coakley FV, Glenn OA, Qayyum A, Barkovich AJ, Goldstein R, Filly RA (2004) Fetal MRI: a developing technique for the developing patient. AJR Am J Roentgenol 182:243–252
Breen JL (1970) A 21 year survey of 654 ectopic pregnancies. Am J Obstet Gynecol 106:1004–1019
Atri M, Leduc C, Gillett P, Bret PM, Reinhold C, Kintzen G, Aldis AE, Thibodeau M (1996) Role of endovaginal sonography in the diagnosis and management of ectopic pregnancy. Radiographics 16:755–774; discussion 775
Jung SE, Byun JY, Lee JM, Rha SE, Kim H, Choi BG, Hahn ST (2001) MR imaging of maternal diseases in pregnancy. AJR Am J Roentgenol 177:1293–1300
Cohen JM, Weinreb JC, Lowe TW, Brown C (1985) MR imaging of a viable full-term abdominal pregnancy. AJR Am J Roentgenol 145:407–408
Wagner A, Burchardt AJ (1995) MR imaging in advanced abdominal pregnancy. A case report of fetal death. Acta Radiol 36:193–195
Malian V, Lee JH (2001) MR imaging and MR angiography of an abdominal pregnancy with placental infarction. AJR Am J Roentgenol 177:1305–1306
Ozdemir I, Demirci F, Yucel O, Alper M (2003) Primary omental pregnancy presenting with hemorrhagic shock. A case report. Gynecol Obstet Invest 55:116–118
Wong WC, Wong BP, Kun KY, Ng TK, Kwok SY, Lee CK (2004) Primary omental ectopic pregnancy. J Obstet Gynaecol Res 30:226–229
Borlum KG, Blom R (1988) Primary hepatic pregnancy. Int J Gynaecol Obstet 27:427–429
Cormio G, Santamato S, Vimercati A, Selvaggi L (2003) Primary splenic pregnancy. A case report. J Reprod Med 48:479–481
Grimes HG, Nosal RA, Gallagher JC (1983) Ovarian pregnancy: a series of 24 cases. Obstet Gynecol 61:174–180
Itoh H, Ishihara A, Koita H, Hatakeyama K, Seguchi T, Akiyama Y, Kataoka H (2003) Ovarian pregnancy: report of four cases and review of the literature. Pathol Int 53:806–809
Raziel A, Schachter M, Mordechai E, Friedler S, Panski M, Ron-El R (2004) Ovarian pregnancy-a 12-year experience of 19 cases in one institution. Eur J Obstet Gynecol Reprod Biol 114:92–96
Filhastre M, Dechaud H, Lesnik A, Taourel P (2005) Interstitial pregnancy: role of MRI. Eur Radiol 15:93–95
Hamada S, Naka O, Moride N, Higuchi K, Takahashi H (1997) Ultrasonography and magnetic resonance imaging findings in a patient with an unruptured interstitial pregnancy. Eur J Obstet Gynecol Reprod Biol 73:197–201
Yamashita Y, Harada M, Torashima M, Takahashi M, Tashiro H, Matsui M, Miyazaki K, Okamura H (1995) Unruptured interstitial pregnancy: a pitfall of MR imaging. Comput Med Imaging Graph 19:241–246
Tamai K, Togashi K, Ito T, Morisawa N, Fujiwara T, Koyama T (2005) MR imaging findings of adenomyosis: correlation with histopathologic features and diagnostic pitfalls. Radiographics 25:21–40
Jung SE, Byun JY, Lee JM, Choi BG, Hahn ST (2001) Characteristic MR findings of cervical pregnancy. J Magn Reson Imaging 13:918–922
Rafal RB, Kosovsky PA, Markisz JA (1990) MR appearance of cervical pregnancy. J Comput Assist Tomogr 14:482–484
Herman A, Weinraub Z, Avrech O, Maymon R, Ron-El R, Bukovsky Y (1995) Follow up and outcome of isthmic pregnancy located in a previous caesarean section scar. Br J Obstet Gynaecol 102:839–841
Noguchi S, Adachi M, Konishi H, Habara T, Nakatsuka M, Kudo T (2005) Intramural pregnancy in a previous cesarean section scar: a case report on conservative surgery. Acta Obstet Gynecol Scand 84:493–495
Saleem SN (2003) MR imaging diagnosis of uterovaginal anomalies: current state of the art. Radiographics 23:e13
Smolders D, Deckers F, Pouillon M, Vanderheyden T, Vanderheyden J, De Schepper A (2002) Ectopic pregnancy within a rudimentary horn in a case of unicornuate uterus. Eur Radiol 12:121–124
Ozeren S, Caliskan E, Corakci A, Ozkan S, Demirci A (2004) Magnetic resonance imaging and angiography for the prerupture diagnosis of rudimentary uterine horn pregnancy. Acta Radiol 45:878–881
Bright DA, Gaupp FB (1990) Heterotopic pregnancy: a reevaluation. J Am Board Fam Pract 3:125–128
Tanaka YO, Shigemitsu S, Nagata M, Shindo M, Okamoto Y, Yoshikawa H, Itai Y (2002) A decidualized endometrial cyst in a pregnant woman: a case observed with a steady-state free precession imaging sequence. Magn Reson Imaging 20:301–304
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tamai, K., Koyama, T. & Togashi, K. MR features of ectopic pregnancy. Eur Radiol 17, 3236–3246 (2007). https://doi.org/10.1007/s00330-007-0751-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-007-0751-6