Abstract
Purpose
To analyze the safety and efficacy of image-guided genicular nerve cooled radiofrequency ablation (C-RFA) for the treatment of pain in non-surgical candidates with moderate to severe knee osteoarthritis (OA) and to compare three- vs four-needle technique.
Method
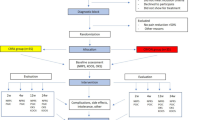
This retrospective study included 50 consecutive patients with pain from moderate to severe knee OA refractory to anti-inflammatory analgesia that failed multiple intra-articular lidocaine-steroid injections and who were non-surgical total knee arthroplasty candidates because of comorbidities. Patients initially underwent anesthetic blocks of the superior medial/lateral femoral and inferior medial tibial genicular nerve branches and in some cases the suprapatellar genicular nerve branch. Radiofrequency ablations of the same nerve branches were performed 1–2 weeks after the nerve blocks. Follow-up outcome was collected at approximately 2 weeks, 1, 3, and 6 months after the C-RFA procedure utilizing VAS and clinically validated questionnaires.
Results
A total of 77 knees were treated. The mean total KOOS score improved significantly from baseline at 24.7 ± 14.1 to 59.4 ± 26.5 at 6 months after treatment (p < 0.0001), with significant improvement in mean pain score from 25.5 ± 15.2 to 64.5 ± 25.2 (p < 0.0001) and mean stiffness score from 35.1 ± 21.9 to 65.8 ± 24.9 (p < 0.0001). At 6 months, 65% of all patients demonstrated decreased opiate medication usage, 79% of patients in the four-needle, and 45% of patients in the three-needle arms (p = 0.03). No complications were reported.
Conclusions
The four-needle treatment approach offers an advantage in the overall efficacy in treating stiffness and pain in patients with moderate-to-severe OA refractory to conservative treatments leading to decreased opiate usage without complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis is the most common form of arthritis affecting approximately 30 million people in the USA. Around 10 million of those people have advanced symptomatic OA, resulting in a significant impact on the quality of life and functional independence related to the disabling pain [1]. In 2013, medical care costs and earning losses among adults with arthritis amounted to over $300 billion, with OA being the second most costly health condition treated in US hospitals and accounting for over $16.5 billion dollars [2,3,4].
Knee OA accounts for more than 80% of the overall arthritis-related disease burden [5]. Currently, the treatment algorithm for knee osteoarthritis includes weight loss, physical therapy, and pharmacological therapy such as non-steroidal anti-inflammatory drugs, followed by non-surgical interventions like intra-articular corticosteroid injections and viscosupplementation [5, 6]. These therapies are often not effective in providing patients with chronic severe OA long-term pain relief and have recently been called into question in terms of accelerating cartilage damage in the joint [2]. Ultimately, long-lasting treatments may require arthroplasty, which may preclude many patients who are not candidates due to medical comorbidities or those who are undesiring of surgery. Patients are frequently prescribed opioids for treatment for chronic knee pain. With the continual rise of health care costs and the opioid crisis, the impact of chronic pain and its treatment options is difficult to understate [6].
Cooled radiofrequency ablation (C-RFA) of the genicular nerves has been introduced as an alternative, FDA approved, minimally invasive, non-surgical treatment option for patients who suffer from chronic knee osteoarthritis pain refractory to conservative management and who are unwilling or unable to undergo surgery [7,8,9,10,11,12]. The technique involves using radiofrequency ablation to disrupt the sensory pathways of the genicular nerves. C-RFA differs from standard radiofrequency ablation in that it utilizes a water-based coolant system that allows for a larger spherical-shaped ablation zone, thereby increasing the area for neurolysis and prolonging the duration of pain relief. While some outcome studies have shown the effectiveness of ablation of primarily three genicular nerves—superolateral (SL), superomedial (SM), and inferomedial (IM)—recent cadaveric and anatomic studies have demonstrated that the sensory pathways of the knee are quite complex, with multiple additional sensory nerves innervating the joint capsule [13, 14]. One of such nerves is the medial retinacular branch (MR), which originates from nerve branches supplying the vastus intermedius and contributes to the subpatellar plexus (Figs. 1 and 2) [13, 14]. This nerve branch can be targeted for radiofrequency ablation in patients with anterior knee pain with the potential to improve patient outcomes. To our knowledge, no studies have reported the clinical outcome of radiofrequency ablation of four nerves—SL, SM, IM, and MR—compared with the more commonly performed three-nerve technique. Thus, we compared the effectiveness of three- vs four-needle approach in improving pain, stiffness, and functional daily living after 6 months of follow-up in patients with moderate-to-severe primary knee osteoarthritis refractory to anti-inflammatory analgesia and multiple intra-articular lidocaine-corticosteroid injections.
Comparison of the three-needle (left) vs four-needle (right) technique for genicular nerve ablation. The three-needle technique demonstrates the introducer needles targeting the superomedial (SM), superolateral (SL), and inferomedial (IM) genicular nerves. In the four-needle technique, an additional needle is located approximately 3 cm proximal to the patella to target the medial retinacular nerve (MR)
Materials and methods
This was a longitudinal-retrospective study conducted at a tertiary academic medical center between July 2018 and April 2019. Institutional review board approval was obtained prior to commencing the study. All patients were referred to interventional musculoskeletal radiology after thorough evaluation by the orthopedic surgical service. Standing knee radiographs were acquired of the affected knee or knees and assessed for the degree of arthritis. Inclusion criteria included patients > 45 years of age able to provide written and verbal consent, presence of moderate to severe knee osteoarthrosis based upon Kellgren and Lawrence classification and knee radiographs, refractory to anti-inflammatory analgesia and previously failed intra-articular lidocaine-steroid injections, 50% or greater pain relief of typical knee pain following diagnostic genicular nerve blocks with 1 mL of 2% lidocaine at each location, and no history of knee arthroplasty. Patients were selected randomly for the three- or four-needle nerve blocks and RFA. The radiofrequency ablation procedures were done approximately 3–4 weeks after the initial anesthetic nerve blocks.
Diagnostic genicular nerve block procedure
The patient was placed supine on a fluoroscopy table with the symptomatic knee(s) at 30° of flexion. After a skin wheal was created with 1–2 mL of 2% lidocaine for superficial local anesthesia, 22-gauge 3.5-in. Whitacre spinal needles were introduced at three locations to block the superolateral, superomedial, and inferomedial genicular nerves. The superolateral and superomedial genicular nerves course through the respective concave transitions of the femoral metadiaphysis and femoral condyles. The inferomedial genicular nerve site is found at the concave transition between the tibial plateau and adjacent metadiaphyseal shaft. If the patient underwent the four genicular nerve procedure block technique, an additional needle was placed at the midline anterior distal femoral diaphysis 3 cm cephalad to the superior aspect of the patella (Figs. 1 and 2). At each genicular nerve site, 1.0 mL of 2% lidocaine was injected in order to anesthetize each genicular nerve. Patients were assessed within 15 min of the nerve blocks by physical examination and ambulation. A positive response was considered as at least 50% of pain reduction.
Genicular nerve radiofrequency ablation procedure
Similar initial steps utilized for the diagnostic genicular nerve procedures were followed for the ablation sections. Patients were continuously monitored and given conscious sedation (1–2 mg IV and/or fentanyl (25–100 mcg IV)) and supplemental oxygen. One to 2 mL of 2% of lidocaine was used to provide soft tissue and skin anesthesia at each of the nerve sites (three vs four). A 50–150-mm 17-gauge introducer needles were placed to ablate the SL, SM, and IM genicular nerves. If the patient underwent the four genicular nerve blocks, then an additional introducer needle was placed to ablate the MR genicular nerve. After placement of the introducer needle, the 18 gauge internally cooled 4-mm active tip RFA electrode (Coolief, Halyard Health, Alpharetta, GA USA) was placed into the introducer needle. Positioning again was confirmed with AP and lateral (covering at least 60% of the bone shaft width) fluoroscopic views. Motor nerve activity was excluded with testing 2 Hz at 1 mA. One milliliter of 2% lidocaine was injected through the introducer needles to anesthetize the area prior to ablation. Each target was lesioned for 180 s at a set temperature of 60 °C.
Data collection
An initial search in the electronic medical record system was performed to review demographic data of each patient pertaining to age, gender, body mass index (BMI), recent and ongoing analgesic medication use, laterality of symptom presentation, and whether the patient underwent three (SL, SM, IM) or four (SL, SM, IM, MR) genicular nerve block/ablations. With verbal consent, the participants were administered a standardized survey by telephone to assess the efficacy of treatment using the Knee Injury and Osteoarthritis Outcome Score (KOOS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and visual analog scale (VAS), which are clinically validated surveys to assess knee functional states [15, 16]. Procedure-related complications such as bleeding and infection were also assessed. Follow-up surveys were acquired at approximately 2 weeks, 1 month, 3 months, and 6 months post-treatment. In addition, information about opioid medication usage before the RFA treatments and at 6 months were assessed by looking into the electronic medical records and asking patients about their medication usage.
Study outcomes
Primary outcomes measured included pain and functional scores assessed using the KOOS, WOMAC, and VAS scores. KOOS is an extension of WOMAC and is a 48-item questionnaire to evaluate overall pain and function of the subject’s knee with 5 separately scored subscales including pain, function in daily living, function in sports and recreation, and quality of life [15]. WOMAC is a 24-item questionnaire that is used to assess hip and knee osteoarthritis and is divided into 3 subscales: pain, stiffness, and function [16]. Item responses on the WOMAC were added to yield subscale scores (pain 0–20, stiffness 0–8, physical function 0–68) with higher scores representing worst health. WOMAC osteoarthritis index scores were then transformed to a 0–100 scale, with zero representing worst knee conditions and 100 representing best knee conditions as common in orthopedic scales such as the KOOS scoring system. Presenting the data in a similar fashion across the KOOS and WOMAC questionnaires utilizing a similar 0–100 scale would make it easier to understand and compare the results. In order to calculate percentage scores in accordance with the KOOS, the following formula provided below can be used to convert the original WOMAC scores following previously proposed guidance (http://www.koos.nu/):
-
Possible maximum raw scores: pain, 20; stiffness, 8; function, 68.
VAS score is a single item pain scale. Each knee that underwent the ablation procedure was treated separately; thus, each knee, even if the procedure was performed on the same patient, has a unique score. In addition, to simplify the analysis of opioid medication usage and change over time, each of these medications was assigned a full unit value and any changes before and after the intervention was quantify. For example, if a patient was taking two opioid medications before the procedure and 1 at 6 months, that patient would receive a − 1 score and so on.
Statistical analysis
Patient characteristics in each treatment arm were compared using Wilcoxon rank sum test for continuous variables and chi-squared test (or Fisher exact test) for categorical variables. The Wilcoxon signed rank test was used for average score comparisons between time points of baseline and 6 months regardless of the number of needles used. Wilcoxon rank sum test was conducted for score comparisons between 3- and 4-needle treatments at each time period (2 weeks, 1 month, 3 months, and 6 months) post-treatment. Subgroup analyses including score comparisons based upon laterality, BMI > 30, age > 65 years old, and degree of osteoarthritis (grade 4) were also obtained. We further investigated the effect of treatment on each score over time using generalized linear mixed models with subject-specific random intercepts without and with controlling for age, BMI, pain location, relief after nerve blocks, and medication change. The base model included fixed effects of treatment (3 vs 4 needles), time, and treatment-by-time interaction. p values were all two sided and considered as statistically significant when p < 0.05. All analyses were performed based on available cases and conducted in the SAS version 9.4 software.
Results
Patient demographics
Overall, a total of fifty patients met the inclusion criteria with 77 total C-RFA procedures on discrete knees. Of the fifty patients, 30 patients underwent the four-needle technique (47 total knees) and 20 patients underwent the three-needle technique (30 total knees). Baseline demographic, clinical, and procedural characteristics between the two treatment arms are shown in Table 1. Mean follow-up time after intervention was 6.1 months. There was a statistically significant difference in age (p = 0.028), with the four-needle group average age of 63.9 ± 13.6 years vs 72.5 ± 14.4 in the three-needle group. Ethnicity was also statistically significant with a higher African American demographic in the 4-needle treatment group. There was no statistically significant difference in sex or BMI between the treatment arms (Table 1). Most patients were females, African Americans, and 67 years of age with a mean BMI of approximately 38. Based on Kellgren and Lawrence classification system, most patients had grade 4 arthritis (grade 4 N = 38; grade 3 N = 12). Patients suffer of knee pain for an average of 2.5 years prior to the procedure. There was no statistically significant difference in duration of knee pain or number of anesthetic-corticosteroid injection with most patients receiving at least one injection within the last year prior to C-RFA (Table 1). There were no reported serious adverse events related to the ablation procedure.
Primary outcomes
KOOS, WOMAC, and VAS
Regardless of the number of needles utilized, there was a statistically significant improvement in overall KOOS, WOMAC, and VAS scores at 2 weeks and 1, 3, and 6 months after genicular nerve ablation (Table 2). The mean total KOOS score (out of 100) progressed positively from baseline at 24.7 to 59.5 at 6 months post-treatment (p < 0.0001). Sub-analysis of the pain component of the KOOS questionnaire demonstrated significant improvement in the mean overall symptoms score from 25.5 to 64.5 (p < 0.0001). There was also significant decrease in mean stiffness score and improved functional daily living. The mean total WOMAC score improved significantly from baseline at 25.2 to 60.5 at 6 months post-treatment. Perceived pain VAS scores changed from 8.4 at baseline to 3.3 at 6 months post-treatment. These improvements remained significant when controlling for laterality with no substantial dissimilarity between the overall scores between right and left knees (p < 0.001).
Three- vs four-needle C-RFA technique (Fig. 3)
The mean total and individual KOOS scores at 2 weeks and 1 month in patients treated with 4 needles were consistently higher, however not statistically significant compared with the three-needle treatment arm. Similar findings were seen in the WOMAC scores (Fig. 3). At 6 months, subgroup KOOS and WOMAC scores of symptoms and stiffness demonstrated statistically significant better scores favoring the four-needle technique. The VAS score was statistically different for the two treatment arms at each time point, favoring the four-needle technique.
Sub-analysis
Sub-analyses were also done to compare four-needle vs three-needle approach in obese patients with BMI > 30, age > 65 years, and osteoarthritis severity, grade 4. Regardless of the number of needles utilized, there was an overall statistically significant improvement in all KOOS, WOMAC, and VAS scores at each time point. In obese patients, there was a statistically significant difference in VAS scores in favor of the patients treated with 4 needles over time. At baseline, the patients treated with 3 needles reported a mean baseline scores of 8.3 ± 1.1 in comparison with the 4-needle arm’s score of 8.5 ± 0.9; p = 0.51. At 2 weeks, patients treated with 3 needles reported a VAS score of 5.2 ± 1.9 vs 3.9 ± 1.4 in 4-needle patients (p = 0.002). Scores at 1, 3, and 6 months were similar. As a reference, 3-needle patients reported a score of 4.8 ± 2.2 vs 2.4 ± 1.9 among 4-needle patients (p < 0.001).
There was also significant improvement in symptom and stiffness at 6 months in patients who underwent four-needle treatment based on the KOOS and WOMAC scores (KOOS, 52.3 ± 27.8 in 3-needle patients vs 73.3 ± 23.5 in 4-needle patients; p = 0.004; WOMAC, 4.2 ± 2.2 in 3-needle patients vs 5.9 ± 1.9 in 4-needle patients; p = 0.004). In patients younger than 65 years of age, there was a significant improvement in VAS scores at 2 weeks, 1 months, 3 months, and 6 months (mean values for 4-needle patients 8.3 ± 1.0 at baseline; 3.8 ± 1.4 at 2 weeks; 3.0 ± 1.5 at 1 month; 2.8 ± 1.4 at 3 months; and 2.3 ± 1.6 at 6 months). The KOOS and WOMAC scores did not show statistically significant difference (p > 0.05) comparing patients treated with 3 vs 4 needles in each subscoring; however, over time, there was an overall improvement similar to information shown on Tables 3, 4, 5, 6, and 7. In patients older than 65 years of age, there was also significant improvement in VAS scores as well as stiffness at 2 weeks (KOOS, 3-needle arm 60.7 ± 21.8 vs 4-needle arm 74.4 ± 26.4; p = 0.018), 1 month (KOOS, 3-needle arm 62.7 ± 21.6 vs 4-needle arm 74.7 ± 26.6; p = 0.027), and 6 months (KOOS, 3-needle arm 51.2 ± 24.8 vs 4-needle arm 72.0 ± 24.5; p = 0.008) with a greater degree of improvement seen in patients treated with a 4-needle approach.
In patients with grade 4 osteoarthritis, again, there was statistical difference of VAS scores at 2 weeks, 1 month, 3 months, and 6 months in a fashion similar to already discussed, as well as stiffness at 6 months (KOOS, 3-needle arm 52.4 ± 25.3 vs 4-needle arm 66.5 ± 26.6; p = 0.024). The remaining scores did not show significant differences (p > 0.05).
Opiate use (Table 8)
Chart review of the opiate medication usage was also performed to determine if four-needle treatment resulted in lower opiate medication usage compared with three-needle technique at 6 months compared with baseline (Table 8).
Decrease in medication usage was quantified as a positive result if the patient was able to eliminate at least one opiate from their medication regiment. In our patient population, 43 out of 50 patients were taking opioid medication at the time of referral to our clinical service (Table 8). Overall, approximately 65% of patients demonstrated decreased opiate medication usage at 6 months with 79% of patients in the four-needle and 45% of patients in the three-needle technique able to reduce opiate medication usage (p = 0.03). Overall, 22 patients went from using 1 medication to none; 12 patients went from 2 to 0; 4 patients went from 2 to 1; 3 patients went from 3 to 0, and 2 from 5 to 3.
Complications
No complications such as hematoma, allergic reactions, or infections were reported during this study.
Generalized linear mixed model
A generalized linear mixed model regression was used to investigate the influence of time, the number of needles used, and the interaction between time and the number of needles used (time * needles in Tables 5, 6, and 7) on the treatment effect (KOOS, WOMAC, VAS scores).
These values were then adjusted for risk factors after controlling variables such as age, BMI, pain location, relief after nerve blocks (weeks), and medication change in order to better assess the effects of the number of needles used. For instance, in the KOOS overall score, there was a statistically significant difference in the scores with time, regardless of the number of needles used (p = 0.029). When adjusting for treatment group factors such as age, BMI, pain location, relief after nerve blocks, and medication change (Table 1), this effect with time was reduced although the trend was still apparent (p = 0.06). The KOOS overall score and subscores of function daily living (p = 0.035), quality of life (p = 0.008), and sports (p = 0.002) demonstrated statistically significant improvement over time. When adjusting for treatment group factors, quality of life and sports function remained statistically significant (p = 0.027 and p = 0.005, respectively). KOOS symptoms and stiffness as well as the WOMAC stiffness subscores demonstrated statistically significant improvement in the time * needle interaction when adjusting for treatment group factors (p = 0.028 and p = 0.03, respectively). This suggests that the stiffness subscore improved at a faster rate in the four-needle treatment group compared with the three-needle group, even after adjusting for other confounding factors. The VAS scores demonstrated statistically significant improvement in scores over time, regardless of the number of needles used (p = 0.0005). The VAS scores also demonstrated more rapid improvement in scores in the four-needle group (p = 0.016), after adjusting for treatment group factors.
Discussion
There is growing evidence that radiofrequency ablation of the genicular nerves is an effective treatment for patients who suffer from pain related to chronic moderate to severe osteoarthritis. Compared with conventional RFA, cooled radiofrequency ablation (C-RFA) utilizes a water-cooling mechanism to provide an ablation zone that is approximately five times larger, improving the ability to target a greater neuronal tissue. This can provide a treatment advantage given the complexity and variability of the neural anatomy of the knee [10,11,12, 14]. Our study compared the effectiveness of four-needle treatment vs three-needle treatment. Various anatomic dissections have shown the complexity of the sensory neural anatomy of the knee, with branches arising from the femoral, sciatic, obturator, and saphenous nerves. The study by Franco et al. demonstrated that an additional nerve branch—known as the medial retinacular branch—is consistently found in the prefemoral-suprapatellar space and can be targeted for ablation [13]. In ablating this nerve, we had hypothesized that targeting four nerve branches would provide improved outcomes compared with the three main nerve targets which have been studied previously allowing for symptomatic relief from the patellofemoral compartment arthritis. In our patient population, most of the subjects (84%) described anterior knee pain with documented arthritic changes on the radiographs.
In agreement with previous studies, approximately 80% of patients demonstrated improvement in symptoms at 6 months after C-RFA, with significant improvement in mean overall KOOS, WOMAC, and VAS scores (7, 8, 10,11,12, 17). Irrespective of the number of needles utilized, there was statistically significant improvement in the subscores related to stiffness, pain, functional daily living, and quality of life. At the time points of 2 weeks, 1 month, and 3 months after the procedure, the KOOS and WOMAC scores were consistently higher in the four-needle treatment arm; however, this difference was not statistically significant. As patients reached the 6-month time point, there was a statistically significant difference in the WOMAC and KOOS stiffness subgroup scores favoring the four-needle treatment arm. The four-needle treatment arm also tended to have more rapid improvement in the stiffness subgroup scores even when adjusting for the other risk factors. A possible explanation for the absent difference in early KOOS and WOMAC outcomes may be that both treatment groups have had adequate neurotomy. It is not until the 6-month time point that patients may begin to have nerve recovery and diminished effect of the nerve ablation, thus manifesting the potential advantage of ablating a fourth target to provide longer duration of relief. The medial retinacular nerve in particular may help patients who suffer from anterior knee pain as it provides contributions to the subpatellar plexus and patellofemoral compartment. In addition, no patients reported any adverse effects or complications directly related to genicular nerve ablation. There does not appear to be an added risk to targeting an additional nerve for genicular nerve ablation. The results of this study suggest that targeting an additional nerve for ablation can provide longer-term relief, thus extending the “bridge” that C-RFA genicular nerve ablation can be for patients with osteoarthritis who have failed conservative measures and are unwilling or unable to undergo surgery. Further investigations with randomized controlled trials and larger patient samples are needed.
The VAS scores consistently favored the four-needle treatment group, even after accounting for the other risk factors despite the KOOS and WOMAC pain subscores did not show statistical significance. A possible explanation for the difference in results may be the individual components of the survey. The KOOS and WOMAC pain subscore consists of multiple questions regarding pain related to range of motion, ambulation, and position, whereas the VAS score is a more general, global perceived score. Patients may have difficulty discerning their pain level with different movements and positions or in some cases, may not have even attempted certain movements, however, are better able to characterize their pain on a numeric scale [1,2,3,4,5,6,7,8,9, 18].
The data presented here also demonstrated that more patients were able to reduce their opiate medication usage in the four-needle treatment group as compared with the three-needle group (79 compared with 45%, p value 0.03). Most patients were treated with opioid to ameliorate their pain prior to the intervention. The most common pain medication regimens used by our patients prior to C-RFA included hydrocodone bitartrate-acetaminophen 10 mg/325 mg every 6 h, tramadol 100 mg every 6 h, trazodone 100 mg BID, and oxycodone 5 to 15 mg orally every 4 to 6 h. A major contribution of this work is that approximately 65% of all patients experienced decreased opiate medication usage at 6 months. Approximately, 400,000 people died from an opioid-related overdose from 1999 to 2017 emphasizing the relevance of interventions that can lead to decrease in the utilization of adjunctive pain analgesics [19].
There are several limitations to our study. The study included a retrospective component with chart review followed by prospective follow-up at a single academic institution. Additionally, the unblinded nature of the study also introduces the potential for bias. There was also a significant difference in the baseline ages between the four-needle (63.9) and three-needle (72.5) treatment groups. However, this difference did not significantly change our results in our linear regression model, when controlling for age as a risk factor; thus, this difference in age is not likely to introduce a confounding risk factor. We recognized that the high incidence of opioid consumption among the patients in our cohort may be unique to our large clinical referral setting reflecting a subset of the overall knee arthritis symptomatic patient population that do not qualify for surgical intervention with a chronic disease history. The high prevalence of opioid use reported in this study may not reflect national trends, and a selection bias may have been unintentionally introduced. Furthermore, the process of self-reporting about the usage of opiates is challenging as pain medication may be acquired from multiple providers and that all prescriptions may not be documented in the medical record. Lastly, the change in the consumption of opiate medication was recorded whereas the total opiate consumption was not measured.
Cooled radiofrequency ablation of genicular nerves is a safe, alternative, non-surgical treatment option for patients with chronic knee osteoarthritis pain. In patients with moderate to severe OA refractory to conservative treatments, cooled radiofrequency ablation of genicular nerves is a safe and effective technique in improving pain, stiffness, and functional daily living. Although there are three main nerve targets for ablation, the complex neural anatomy of the knee provides additional targets for treatment. The four-needle technique produced better individual KOOS, WOMAC, and VAS scores than the three-needle technique at multiple post-treatment time points; some of which were statistically significant. Additionally, patients treated with the 4-needle technique had a greater reduction in the number of opiate medications.
References
Barbour KE, Helmick CG, Boring M, et al. Vital signs: prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation - United States, 2013-2015. MMWR Morb Mortal Wkly Rep. 2017;66:246–53.
Barbour KE, Stevens JA, Helmick CG, et al. Falls and fall injuries among adults with arthritis--United States, 2012. MMWR Morb Mortal Wkly Rep. 2014;63:379–83.
Hootman JM, Helmick CG, Barbour KE, et al. Updated projected prevalence of self-reported doctor-diagnosed arthritis and arthritis-attributable activity limitation among US adults, 2015-2040. Arthritis Rheumatol. 2016;68:1582–7.
Theis KA, Roblin DW, Helmick CG, et al. Prevalence and causes of work disability among working-age U.S. adults, 2011-2013, NHIS. Disabil Health J. 2018;11:108–15.
Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cartil. 2019;27:1578–89.
Bruyere O, Honvo G, Veronese N, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Semin Arthritis Rheum. 2019;49:337–50.
Iannaccone F, Dixon S, Kaufman A. A review of long-term pain relief after genicular nerve radiofrequency ablation in chronic knee osteoarthritis. Pain Physician. 2017;20:E437–e44.
Choi WJ, Hwang SJ, Song JG, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. 2011;152:481–7.
Davis T, Loudermilk E, DePalma M, et al. Prospective, multicenter, randomized, crossover clinical trial comparing the safety and effectiveness of cooled radiofrequency ablation with corticosteroid injection in the management of knee pain from osteoarthritis. Reg Anesth Pain Med. 2018;43:84–91.
Hunter C, Davis T, Loudermilk E, et al. Cooled radiofrequency ablation treatment of the Genicular nerves in the treatment of osteoarthritic knee pain: 18 and 24-month results. Pain Pract. 2020;20(3):238–46.
Jamison DE, Cohen SP. Radiofrequency techniques to treat chronic knee pain: a comprehensive review of anatomy, effectiveness, treatment parameters, and patient selection. J Pain Res. 2018;11:1879–88.
McCormick ZL, Korn M, Reddy R, et al. Cooled radiofrequency ablation of the genicular nerves for chronic pain due to knee osteoarthritis: six-month outcomes. Pain Med. 2017;18:1631–41.
Franco CD, Buvanendran A, Petersohn JD, et al. Innervation of the anterior capsule of the human knee: implications for radiofrequency ablation. Reg Anesth Pain Med. 2015;40:363–8.
Tran J, Peng PWH, Lam K, et al. Anatomical study of the innervation of anterior knee joint capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43:407–14.
Roos EM, Roos HP, Lohmander LS, et al. Knee injury and osteoarthritis outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96.
Wolfe F, Kong SX. Rasch analysis of the Western Ontario MacMaster questionnaire (WOMAC) in 2205 patients with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Ann Rheum Dis. 1999;58:563–8.
Kim SY, Le PU, Kosharskyy B, et al. Is Genicular nerve radiofrequency ablation safe? A literature review and anatomical study. Pain Physician. 2016;19:E697–705.
McAlindon TE, LaValley MP, Harvey WF, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical trial. Jama. 2017;317:1967–75.
Scholl L, Seth P, Kariisa M, et al. Drug and opioid-involved overdose deaths - United States, 2013-2017. MMWR Morb Mortal Wkly Rep. 2018;67:1419–27.
Acknowledgments
We would like to recognize the contributions of Monica Umpierrez, M.D., Guillermo Umpierrez, M.D., Samuel Earl Broida, M.D., Janice Newsome, M.D., David Prologo, M.D., and Zackary Bercu, M.D. from the department of radiology and imaging sciences at Emory University School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was selected as scientific paper of the year during the 2019 42nd SSR meeting in Scottdale, AZ, and was subsequently selected for presentation in the International Skeletal Society 2019 Meeting in Vancouver, Canada.
Rights and permissions
About this article
Cite this article
Wong, P.KW., Kokabi, N., Guo, Y. et al. Safety and efficacy comparison of three- vs four-needle technique in the management of moderate to severe osteoarthritis of the knee using cooled radiofrequency ablation. Skeletal Radiol 50, 739–750 (2021). https://doi.org/10.1007/s00256-020-03619-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03619-1