Abstract
Objective
The purpose of our study was to determine the role of brown adipose tissue (BAT) in cancer progression.
Materials and methods
Our study was approved by our institutional review board and Health Insurance Portability and Accountability Act–compliant. Our study group comprised 132 cancer patients (116 f, 16 m; mean age 50 ± 16 years) who underwent F18-FDG PET/CT per standard clinical protocol, for staging or surveillance of cancer. We included patients who were BAT-positive on PET/CT and had clinical follow-up data available for at least 12 months or until tumor recurrence or tumor-related death, whichever occurred first. BAT volume by PET/CT was quantified by PET-CT Viewer shareware. Clinical information including tumor type, tumor recurrence, survival, and outside temperature at time of scan were recorded. Cox proportional hazard models were used to determine longitudinal associations between BAT volume and tumor recurrence/mortality.
Results
There were 55 tumor recurrences/tumor-related deaths over a median follow-up period of 71 (33; 110 interquartile range) months. Higher BAT volume was associated with an increased likelihood of tumor recurrence/tumor-associated mortality after adjustment for covariates (p = 0.03).
Conclusion
BAT volume, assessed using routine PET/CT, is a predictor of tumor recurrence/mortality in patients with cancer, independent of other factors that can influence BAT activity, such as sex, age, BMI, or tumor type.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Emerging evidence suggests that tumor progression does not only depend on tumor cells but also the surrounding stromal tissue and tumor microenvironment. Tumor cells can induce microenvironments at local and distant sites that protect cells from apoptosis and stimulate neovascularity, thereby promoting tumor cell survival [1,2,3]. Adipocytes have been found to play an important role in modulating tumor microenvironment through secretion of inflammatory cytokines, which promote tumor invasiveness and metastases [4], and secretion of fatty acids, which provide energy for cancer cells [5, 6].
While most studies examining the role of adipocytes in cancer have focused on white adipose tissue (WAT) [7, 8], recent studies suggest that brown adipose tissue (BAT) can promote tumor growth and might play a role in the development of cancer cachexia [9,10,11,12]. BAT is metabolically active and consumes energy through non-shivering thermogenesis [13]. BAT is characterized by the expression of uncoupling protein 1 (UCP1), is activated by cold exposure, and is more prevalent in women and young and lean subjects [14]. Importantly, BAT demonstrates increased vascularity and a higher mitochondrial content compared to WAT [13]. BAT can also be induced in WAT, a process termed “browning,” and these adipocytes are called “brite” or “beige” [15, 16]. During the transition from WAT into brite/beige fat, activation of angiogenesis results in increased vascularity [17]. This is relevant in the context of tumor growth and cancer progression. Implantation of different tumor types into BAT in mice has resulted in accelerated tumor growth compared to cells implanted into WAT [18]. These findings suggest that vascularized BAT might promote tumor growth and cancer progression.
BAT can be quantified non-invasively by 18 F-fluorodeoxyglucose positron emission tomography/computerized tomography (PET/CT) [19, 20] and PET/CT is routinely used in patients with cancer to assess treatment response. Whereas many studies have examined the role of WAT, especially abdominal adipose tissue, as predictor of cancer progression [21,22,23,24], only few studies have focused on BAT in this context [9,10,11].
The purpose of our study was to determine the role of BAT in cancer progression. We hypothesized that higher BAT volume was associated with an increased likelihood of tumor recurrence or tumor-associated mortality.
Materials and methods
Our study was approved by our institutional review board (IRB) and Health Insurance Portability and Accountability Act (HIPAA)–compliant with exemption status for individual informed consent.
Patients
We performed a retrospective search of consecutive PET/CT examinations in patients older than 18 years with a history of cancer who were BAT-positive and had clinical follow-up data available for at least 12 months or until tumor recurrence or tumor-related death, whichever occurred earlier. Medical records were reviewed and clinical information including tumor type, tumor recurrence, and survival were recorded. Tumor recurrence was defined by new tumor on cross-sectional imaging (MRI, CT, PET/CT) or biopsy. In patients who had subsequent PET/CTs, the number of PET/CTs and the presence or absence of BAT on follow-up studies was recorded. Outdoor temperatures at the time of scan were recorded. BAT volume and baseline clinical characteristics have been reported previously in a subset of patients [9, 25]; however, no outcome data have ever been reported.
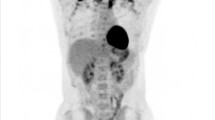
18F-FDG PET/CT
Whole-body PET/CT (Siemens Biograph 16 or 64, Siemens, Erlangen, Germany or GE Discovery, GE Healthcare, Milwaukee, WI, USA) was performed per standard clinical protocol as previously described [9]. Patients fasted 6 h before the exam and blood glucose levels were measured upon arrival and 18 F-FDG was injected only if blood glucose was ≤ 200 mg/dl. Attenuation correction CT obtained in mid-expiration phase without intravenous contrast (slice thickness, 5 mm; table feed per rotation, 18 mm; time per table rotation, 0.5 s; tube voltage, 120 kVp; tube current, 11 mAs; field of view, 48 cm) and PET images were acquired. 3D PET images were obtained from the skull base to the mid-thigh, with 6–8 bed positions lasting 3–7 min each. Images were reconstructed to a slice thickness of 2.4 mm. The CT scanners used in this study were tested on an annual basis according to American Association of Physicists in Medicine (AAPM) and American College of Radiology (ACR) guidelines (AAPM report #74 and #96 and ACR CT QC manual) and standard clinical quality assurance measures were performed to assess for reproducibility of scans over time.
Image analysis
Semiquantitative and qualitative evaluation of BAT was performed on fused FDG PET and CT images. BAT activity was assessed by measuring FDG uptake along the neck, supraclavicular, mediastinal, and paravertebral regions corresponding to adipose tissue attenuation on CT and standardized uptake values (SUV) were calculated. The SUVs were used to quantify the volume of BAT (cm3) as the sum of voxel volumes within suspected BAT regions where SUV ≥ 1.5 and HU are between − 190 and − 10 [19]. Analyses were performed using PET-CT Viewer shareware [26].
Statistical analysis
Statistical analysis was performed using JMP statistical software version 12.0 (SAS Institute Inc., Cary, NC.). The Shapiro–Wilk test was used to test normality of distribution. Variables that were not normally distributed were log transformed for Cox proportional hazard models. BAT volume, age, and BMI were entered as continuous variables, and sex and tumor type were coded were entered as categorical variables.
The primary outcome of interest was first tumor recurrence after PET/CT or tumor-associated mortality, whichever came first. Cox proportional hazard models were used to explore the longitudinal association between BAT and tumor recurrence/mortality. Univariate and multivariate analyses of tumor recurrence/mortality were performed using Cox’s regression models, and the results are presented as hazard ratios (HR) with 95% confidence interval (CI). Multivariate analysis was performed to control for factors that have been shown to influence BAT activity, such as outside temperature at time of PET/CT, sex, age, BMI, serum glucose, and tumor type [27, 28]. Data are shown as mean ± standard deviation for normally distributed data and as median (interquartile range) for non-normally distributed data. Statistical significance was defined as a two-tailed p < 0.05.
Results
We identified 132 patients who underwent PET/CT for cancer staging or surveillance and who were BAT-positive (mean age 50 ± 16 years, range 20 to 88 years). Of the 132 patients, 116 were women and 16 were men. Median BMI was 24 kg/m2 (IQR 22–27 kg/m2; range 16 to 49 kg/m2) and median outside temperature at time of PET/CT was 47 °F (IQR 37–69 °F). Mean serum glucose was 101 ± 12 mg/dL. Thirty-five patients had lymphoma, 22 lung cancer, 18 gastrointestinal cancer, 16 breast cancer, 12 melanoma, 10 genitourinary cancer, 10 thyroid cancer, and 9 sarcoma/carcinoma of unknown origin. PET/CT was performed for staging in 80 patients and for surveillance in 52 patients.
There were 55 tumor recurrences/tumor-related deaths over a median follow-up period of 71 months (IQR 33–110 months). Median time from PET/CT to tumor recurrence/tumor-related death was 13 months (IQR 4–22 months).
Median BAT volume was 9.1 mL (IQR 3.5–73.2 mL). There was a trend of higher BAT volume and an increased likelihood of tumor recurrence/tumor-associated mortality with an uncorrected HR of 1.15 (95% CI 0.93–1.68, p = 0.1). Correcting for outside temperature did not change the association (p = 0.1). Serum glucose was positively associated with BAT (r = 0.21, p = 0.02).
In the univariate analyses, there was no association between variables that can influence BAT, such as sex (p = 0.9), age (p = 0.3), or BMI (p = 0.7), and tumor recurrence/tumor-associated mortality. There was a trend of an association between tumor type and increased likelihood of tumor recurrence/tumor-associated mortality (p = 0.05).
In the multivariate model, higher BAT volume was associated with an increased likelihood of tumor recurrence/tumor-associated mortality after adjustment for sex, age, BMI, and tumor type (HR of 1.49, 95% CI 1.05–2.22, p = 0.03). Adding serum glucose to the model increased the significance of BAT (HR of 1.58, 95% CI 1.07–2.45, p = 0.02) (Fig. 1).
Fifty-two patients had follow-up PET/CTs (mean 2, range 1–11). Of the 52 patients with subsequent PET/CTs, 29 had tumor recurrence/tumor-associated mortality and 23 had no tumor recurrence and were alive. Of the 29 patients with tumor recurrence/tumor-associated mortality, BAT remained positive on subsequent PET/CTs in 23 patients (79%). Of the 23 patients without tumor recurrence, BAT decreased or resolved on subsequent PET/CTs in 21 patients (91%).
Discussion
Our study showed that BAT volume, assessed using routine PET/CT, is a positive predictor of tumor recurrence/tumor-associated mortality in patients with cancer, independent of other risk factors, such as sex, age, BMI, or tumor type. Moreover, in a group of patients with subsequent PET/CTs BAT stayed positive in 79% of patients who developed tumor recurrence/tumor-associated mortality while 91% of patients without tumor recurrence showed a decrease or resolution of BAT on subsequent studies.
Recent studies have identified an important role of adipose tissue in cancer biology. Adipose tissue does not only store energy but also secretes adipokines, inflammatory cytokines, growth factors, and free fatty acids, which can contribute to tumor growth and cancer progression [1, 4, 6]. Tumors can also reprogram adipocytes, thereby promoting disease progression. In a study by Wu et al., culturing tumor cells with adipocytes induced an aggressive phenotype, in part through increased differentiation of beige/brown fat and reprogramming of surrounding adipocytes [29]. A study in Brca1 mutant mice showed 50-fold increased UCP-1 in the mammary gland, associated with increased vascularity, compared to the wild type [30]. Also, implantation of tumors into BAT leads to accelerated tumor growth in mice [18]. Human studies have shown higher BAT activity and BAT volume associated with higher cancer stage [9,10,11] .
While most studies on BAT in cancer have been cross-sectional, our study focused on the role of BAT on cancer progression longitudinally, over a mean period of 75 months. We found a trend of higher BAT volume and an increased likelihood of tumor recurrence/tumor-associated mortality in univariate analyses. There was no association between age, sex, or BMI and tumor recurrence/tumor-associated mortality, while there was a trend of an association with tumor type. However, in the multivariate analyses, BAT was a positive predictor of tumor recurrence/cancer-related mortality, independent of factors that can influence BAT activity such as age, BMI, sex, and tumor type. In addition, our data were controlled for outside temperature at time of scan, which can influence BAT activity [14, 31].
Recent animal studies have suggested a role of BAT in the development of cancer cachexia [12]. Cancer cachexia is a complex syndrome, characterized by loss in adipose tissue and muscle, and carries a poor prognosis [32]. In mouse models, WAT browning and increased thermogenic activity contributed to accelerated energy expenditure and propagation of cachexia [12, 33]. It is possible that BAT-induced development of cancer cachexia was a contributing factor of our observed increase in cancer-related mortality in patients with high BAT volume.
Our study had several limitations: first is the retrospective nature of our study and the dependency on medical records for clinical information. Second, PET/CT is an imperfect standard of reference given its heterogeneity of response and sensitivity to experimental or environmental factors [34]. We therefore only included patients who underwent our standard clinical PET/CT protocol, prior to which patients quietly rested in reclined seat with room temperature of 75 °F. Third, because we only included BAT-positive patients, there was a significantly higher proportion of women, due to the known higher prevalence of BAT in women, which might limit generalizability of our results. Strengths of our study include the large number of BAT-positive patients with quantification of BAT volume and long-term outcome data.
In conclusion, our study showed that increased BAT volume is a positive predictor of cancer progression or tumor-related mortality, independent of other risk factors, such as age, sex, BMI, or tumor type. Our findings suggest that BAT may play a role in modulating the tumor microenvironment and could serve as novel biomarkers for outcome and mortality in patients with cancer, who often undergo PET/CT as part of staging or surveillance.
References
Dittmer J, Leyh B. Paracrine effects of stem cells in wound healing and cancer progression (review). Int J Oncol. 2014;44(6):1789–98.
Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438(7069):820–7.
Peinado H, Zhang H, Matei IR, Costa-Silva B, Hoshino A, Rodrigues G, et al. Pre-metastatic niches: organ-specific homes for metastases. Nat Rev Cancer. 2017;17(5):302–17.
Himbert C, Delphan M, Scherer D, Bowers LW, Hursting S, Ulrich CM. Signals from the adipose microenvironment and the obesity-cancer link-a systematic review. Cancer Prev Res (Phila). 2017;10(9):494–506.
Nieman KM, Kenny HA, Penicka CV, Ladanyi A, Buell-Gutbrod R, Zillhardt MR, et al. Adipocytes promote ovarian cancer metastasis and provide energy for rapid tumor growth. Nat Med. 2011;17(11):1498–503.
Nieman KM, Romero IL, Van Houten B, Lengyel E. Adipose tissue and adipocytes support tumorigenesis and metastasis. Biochim Biophys Acta. 2013;1831(10):1533–41.
Klopp AH, Zhang Y, Solley T, Amaya-Manzanares F, Marini F, Andreeff M, et al. Omental adipose tissue-derived stromal cells promote vascularization and growth of endometrial tumors. Clin Cancer Res. 2011;18(3):771–82.
Zhang Y, Daquinag A, Traktuev DO, Amaya-Manzanares F, Simmons PJ, March KL, et al. White adipose tissue cells are recruited by experimental tumors and promote cancer progression in mouse models. Cancer Res. 2009;69(12):5259–66.
Bos SA, Gill CM, Martinez-Salazar EL, Torriani M, Bredella MA. Preliminary investigation of brown adipose tissue assessed by PET/CT and cancer activity. Skelet Radiol. 2019;48(3):413–9.
Cao Q, Hersl J, La H, Smith M, Jenkins J, Goloubeva O, et al. A pilot study of FDG PET/CT detects a link between brown adipose tissue and breast cancer. BMC Cancer. 2014;14:126.
Huang YC, Chen TB, Hsu CC, Li SH, Wang PW, Lee BF, et al. The relationship between brown adipose tissue activity and neoplastic status: an (18)F-FDG PET/CT study in the tropics. Lipids Health Dis. 2011;10:238.
Kir S, Spiegelman BM. Cachexia and brown fat: a burning issue in cancer. Trends Cancer. 2016;2(9):461–3.
Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev. 2004;84(1):277–359.
Cypess AM, Lehman S, Williams G, Tal I, Rodman D, Goldfine AB, et al. Identification and importance of brown adipose tissue in adult humans. N Engl J Med. 2009;360(15):1509–17.
Barbatelli G, Murano I, Madsen L, Hao Q, Jimenez M, Kristiansen K, et al. The emergence of cold-induced brown adipocytes in mouse white fat depots is determined predominantly by white to brown adipocyte transdifferentiation. Am J Physiol Endocrinol Metab. 2010;298(6):E1244–53.
Walden TB, Hansen IR, Timmons JA, Cannon B, Nedergaard J. Recruited vs. nonrecruited molecular signatures of brown, “brite,” and white adipose tissues. Am J Physiol Endocrinol Metab. 2012;302(1):E19–31.
Lim S, Honek J, Xue Y, Seki T, Cao Z, Andersson P, et al. Cold-induced activation of brown adipose tissue and adipose angiogenesis in mice. Nat Protoc. 2012;7(3):606–15.
Lim S, Hosaka K, Nakamura M, Cao Y. Co-option of pre-existing vascular beds in adipose tissue controls tumor growth rates and angiogenesis. Oncotarget. 2016;7(25):38282–91.
Chen KY, Cypess AM, Laughlin MR, Haft CR, Hu HH, Bredella MA, et al. Brown adipose reporting criteria in imaging STudies (BARCIST 1.0): recommendations for standardized FDG-PET/CT experiments in humans. Cell Metab. 2016;24(2):210–22.
Sampath SC, Sampath SC, Bredella MA, Cypess AM, Torriani M. Imaging of brown adipose tissue: state of the art. Radiology. 2016;280(1):4–19.
Grignol VP, Smith AD, Shlapak D, Zhang X, Del Campo SM, Carson WE. Increased visceral to subcutaneous fat ratio is associated with decreased overall survival in patients with metastatic melanoma receiving anti-angiogenic therapy. Surg Oncol. 2015;24(4):353–8.
Shin DY, Kim A, Byun BH, Moon H, Kim S, Ko YJ, et al. Visceral adipose tissue is prognostic for survival of diffuse large B cell lymphoma treated with frontline R-CHOP. Ann Hematol. 2016;95(3):409–16.
Veld J, O’Donnell EK, Reagan MR, Yee AJ, Torriani M, Rosen CJ, et al. Abdominal adipose tissue in MGUS and multiple myeloma. Skelet Radiol. 2016;45(9):1277–83.
Veld J, Vossen JA, De Amorim Bernstein K, Halpern EF, Torriani M, Bredella MA. Adipose tissue and muscle attenuation as novel biomarkers predicting mortality in patients with extremity sarcomas. Eur Radiol. 2016;26:4649–55.
Bredella MA, Gill CM, Rosen CJ, Klibanski A, Torriani M. Positive effects of brown adipose tissue on femoral bone structure. Bone. 2014;58:55–8.
Barbaras L, Tal I, Palmer MR, Parker JA, Kolodny GM. Shareware program for nuclear medicine and PET/CT PACS display and processing. AJR Am J Roentgenol. 2007;188(6):W565–8.
Cronin CG, Prakash P, Daniels GH, Boland GW, Kalra MK, Halpern EF, et al. Brown fat at PET/CT: correlation with patient characteristics. Radiology. 2012;263(3):836–42.
Steinberg JD, Vogel W, Vegt E. Factors influencing brown fat activation in FDG PET/CT: a retrospective analysis of 15,000+ cases. Br J Radiol. 2017;90(1075):20170093.
Wu C, Cheng W, Sun Y, Dang Y, Gong F, Zhu H, et al. Activating brown adipose tissue for weight loss and lowering of blood glucose levels: a microPET study using obese and diabetic model mice. PLoS One. 2014;9(12):e113742.
Jones LP, Buelto D, Tago E, Owusu-Boaitey KE. Abnormal mammary adipose tissue environment of Brca1 mutant mice show a persistent deposition of highly vascularized multilocular adipocytes. J Cancer Sci Ther. 2011; 8(Suppl 2). pii:004. https://phstwlp2.partners.org:2052/pmc/articles/PMC3851023/
Ouellet V, Routhier-Labadie A, Bellemare W, Lakhal-Chaieb L, Turcotte E, Carpentier AC, et al. Outdoor temperature, age, sex, body mass index, and diabetic status determine the prevalence, mass, and glucose-uptake activity of 18F-FDG-detected BAT in humans. J Clin Endocrinol Metab. 2011;96(1):192–9.
Argiles JM, Busquets S, Stemmler B, Lopez-Soriano FJ. Cancer cachexia: understanding the molecular basis. Nat Rev Cancer. 2014;14(11):754–62.
Dalal S. Lipid metabolism in cancer cachexia. Ann Palliat Med. 2019;8(1):13–23.
Cypess AM, Haft CR, Laughlin MR, Hu HH. Brown fat in humans: consensus points and experimental guidelines. Cell Metab. 2014;20(3):408–15.
Funding
This study was supported by NIH grants K24 DK-109940 and P30DK040561.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived for this retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chu, K., Bos, S.A., Gill, C.M. et al. Brown adipose tissue and cancer progression. Skeletal Radiol 49, 635–639 (2020). https://doi.org/10.1007/s00256-019-03322-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03322-w