Abstract
The potential role of visceral adipose tissue (VAT) as a prognostic factor in patients with diffuse large B cell lymphoma (DLBCL) treated with frontline rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) immunochemotherapy was explored. Total adipose tissue and VAT were measured by analyzing positron emission tomography (PET)/computed tomography (CT) images obtained during the initial staging of patients with DLBCL. The VAT ratio was calculated as follows: VAT ratio = VAT area/total adipose tissue area. Body mass index (BMI), sex, and International Prognostic Index (IPI) were also incorporated as co-variates in the final model of multivariate Cox regression analysis for survival. A total of 156 patients with DLBCL, who were treated with frontline R-CHOP, were enrolled in our study. The median patient age was 61 years, and 81 patients were male (51.9 %). The median cycle of R-CHOP was six. The IPI risk group was a strong prognostic factor for progression-free survival (PFS) and overall survival (OS) (p < 0.001). Obese BMIs were an independent prognostic factor for PFS, but not for OS in multivariate analyses, compared to patients with normal BMIs (HR = 0.43, 95 % CI = 0.19–0.98, and p = 0.046 for PFS). A high VAT ratio (third tertile) was an independent adverse prognostic factor for PFS and OS in multivariate analyses (HR = 2.87 and 2.66, 95 % CI = 1.30–6.32 and 1.30–5.44, and p = 0.009 and 0.007 for PFS and OS, respectively). VAT ratio was an independent prognostic factor for patients with DLBCL treated with first-line R-CHOP; thus, additional large prospective studies are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse large B cell lymphoma (DLBCL) is one of the most common hematologic malignancies in the world [1]. Due to its clinical aggressiveness, initial prognostic stratification is important for making a treatment plan. One of the strongest prognostic factors to date is the International Prognostic Index (IPI), which includes the age, Eastern Cooperative Oncology Group (ECOG) performance status, Ann Arbor stage, number of extranodal disease sites, and serum level of lactate dehydrogenase (LDH) [2]. Other factors, such as gene expression profiles in tumor tissues, have been proposed as prognostic markers in DLBCL [3]. Recent research also demonstrated that obesity can be a prognostic factor in DLBCL [4, 5].
Obesity is a well-defined risk factor for many cancers [6]. In most studies of the relationship between obesity and cancer, body mass index (BMI) is a widely accepted objective measure of obesity and various studies have reported BMI as a quantitative measure of obesity in cancer patients [7, 8].
A large-scale population-based cohort study showed that increased BMIs are associated with increased risks for most cancers, including uterine, gallbladder, renal, cervical, thyroid, hepatic, colon, ovarian, and postmenopausal breast cancers [6]. The risk of DLBCL also has been studied in view of the association with BMI.
Two meta-analyses showed that increased BMIs are associated with the incidence of DLBCL, with a relative risk [RR] of 1.13 per 5 kg/m2-increase in BMI [4]. Moreover, the RR of DLBCL for obese individuals was 1.29, compared with individuals with normal BMIs [9]. The impact of BMI on the outcomes of DLBCL has been analyzed in many studies [5, 10–13]. Two studies reported that high BMIs affected unfavorable outcomes in DLBCL patients. A population-based study from the USA showed that the hazards ratio (HR) for overall survival (OS) in overweight (25–29.9 kg/m2) and obese (≥30 kg/m2) patients with DLBCL were 1.05 and 1.37, respectively [11]. An outcome study from Italy also found that a high BMI (≥28) was associated with poor survival (HR for OS and event-free survival = 2.9 and 2.8, respectively) [5] in high-risk DLBCL patients treated with high-dose sequential chemotherapy followed by autologous hematopoietic stem cell transplantation.
However, the final conclusions of reports on the correlation between BMI and DLBCL are inconsistent. Carson et al. [10] clearly showed that high BMI (overweight and obese) was independently associated with favorable outcomes in a large retrospective cohort (HR for mortality = 0.73 and 0.68 for overweight and obese BMIs, respectively). Another retrospective cohort study that included DLBCL similarly showed that overweight and obese BMI values were associated with better OS and progression-free survival (PFS) [13]. However, several studies have concluded that BMI was not significantly associated with outcomes in DLBCL [12]. The strikingly different results between studies addressing the same issue prompted us to question whether BMI is an appropriate measure of human adiposity, and if BMIs correlate with DLBCL outcomes.
Direct measurement of abdominal adipose tissue is a reasonable alternative to BMI. Quantitative measurements of total and visceral adipose tissue (VAT) have been used to assess human adiposity in various clinical settings [14]. Abdominal adipose tissue is mainly composed of two compartments, VAT and subcutaneous adipose tissue (SAT), which harbor remarkable anatomical and functional differences. VAT contains a larger number of inflammatory cells, immune cells, and adipocytes that are metabolically active and sensitive to adrenergic stimulation [15]. As a result, many investigators have proposed that VAT is an important measure of human adiposity and that VAT reflects the status of human adipose tissue adequately when predicting cancer outcomes [16]. The use of VAT as a prognostic factor has already been validated in populations with metabolic disease [17].
Several studies have addressed the association between BMIs and DLBCL prognosis; however, the results are discordant. To our knowledge, there have been no reports addressing the association between VAT and outcomes for DLBCL patients. In this study, we explored the potential role of VAT on outcomes of patients with DLBCL.
Materials and methods
Study population
Patients who were diagnosed with DLBCL and were treated with frontline rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone (R-CHOP) immunochemotherapy at the Korea Cancer Center Hospital from January 2004 to December 2014 were enrolled in our study. Patients with positive anti-HIV antibody test results or a history of organ transplantation were excluded. Primary central nervous system DLBCL patients were also excluded. Patients whose positron emission tomography (PET)/computed tomography (CT) scans at the time of the initial diagnosis were not available were also excluded. Medical records were reviewed and baseline clinical information on sex, age, ECOG performance status, serum LDH levels, Ann Arbor stage, and extranodal involvement was collected.
BMIs were calculated using the following equation: BMI = weight (kg)/square of the height (m2). BMIs were classified into five categories according to the modified WHO criteria as follows: underweight (<18.5 kg/m2), normal range (18.5–<23 kg/m2), preobese (23–<25 kg/m2), obese (25–<25 kg/m2) and superobese (≥30 kg/m2) [18, 19].
The Institutional Review Boards of Korea Cancer Center Hospital reviewed and approved this study protocol. We followed the recommendations of the Declaration of Helsinki for biomedical research involving human subjects.
Adipose tissue measurement
Non-contrast CT images of the abdomen and pelvis were extracted from PET/CT scans that were performed during the initial staging analysis of patients with DLBCL. A transverse CT image at the intervertebral disc between L4 and L5 was selected and the adipose tissue in this image was measured. Cases were excluded if the whole skin was not included in the scanned image or if there were lymphoma lesions in the image. The exact measurement of the fat area was performed using Rapidia 3D software (Infinitt, Seoul, Korea). The region of interest (ROI) encompassing total adipose tissue (TAT) and VAT was delineated using a manual method option in the Rapidia 3D package (Fig. 1). The identification of adipose tissue was performed with threshold attenuation values between −250 and −50 Hounsfield units [17]. The VAT ratio was calculated using the formula, VAT ratio = VAT area/TAT area. Calculated VAT ratios were divided into three tertiles, with the mid-tertile range as the reference range in subsequent analyses. BMI and VAT ratios were considered as ordered categorical variables.
Measurement of total and visceral adipose tissue. Regions of interest (ROIs) with a Hounsfield unit of −250 to −50 at the L4 level were drawn manually. Total adipose tissue (▲ + *) and visceral adipose tissue (VAT; *) were measured. a Representative image with low VAT ratio (7421.49/32885.52 = 0.226). b Representative image with high VAT ratio (14687.39/25679.56 = 0.572). VAT visceral adipose tissue
Statistical analysis
Statistical analyses were performed using STATA, version 13 (Stata Corp., College Station, TX, USA).
PFS was defined as the time interval between the start of R-CHOP and the time of disease progression, relapse, or death due to any cause that was first observed. OS was defined as the time interval between the initial diagnosis and death due to any cause or the date of the last clinical follow-up. PFS and OS were assessed using the Kaplan-Meier method, and the prognostic factors for OS and PFS were identified using the Cox’s proportional hazard model. A p value <0.05 (two-sided) was considered statistically significant.
Results
Patients’ characteristics
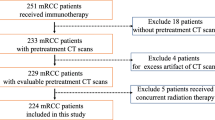
A total of 297 patients with DLBCL who were treated with frontline combination R-CHOP chemotherapy were initially screened, and a total of 156 DLBCL patients were enrolled in our study according to the predefined inclusion and exclusion criteria. The median age of the population was 61 years (range 27–86 years), and 81 patients were male (51.9 %). Twenty-four patients with poor ECOG performance status (≥2) were included in our study. Our study population was well-balanced and representative in terms of sex, Ann Arbor stage, and LDH levels (Table 1).
VAT ratio
The VAT ratios calculated in our study population ranged from 0.11 to 0.65 (Table 1). When the VAT ratios were categorized into tertiles, the values in the first tertile ranged from 0.113 to 0.294 (n = 58), mid-tertile ranged from 0.295 to 0.380 (n = 52), and the third tertile ranged from 0.381 to 0.647 (n = 46).
Frontline treatment and responses
All patients were treated with R-CHOP. The median number of R-CHOP cycles was six. Twenty-one (13.5 %) and nine (5.8 %) of the patients were also treated with consolidative external beam radiation therapy and radioimmunotherapy with 131I-rituximab, respectively (Table 2). A total of 115 patients (73.7 %) achieved complete response (CR). The CR rate was slightly lower in patients with high VAT ratio compared to those with the patients with mid-tertile range or low VAT ratio though they are not statistically significant (76.9, 75.9, and 67.4 % for 1st, mid-, and 3rd tertile range of VAT ratios, respectively, p = 0.51). The PFS according to patients’ groups with different VAT ratios showed a similar trend (Table 3).
Prognostic factors for PFS
We performed Cox regression analyses for the identification of multiple prognostic factors for survival in patients with DLBCL. Sex was not a significant prognostic factor for PFS. Well-validated prognostic factors like age, Ann Arbor stage, ECOG performance status, LDH levels, and extranodal involvement are all incorporated into the IPI scoring system; therefore, we analyzed these factors as a single categorical variable termed, the IPI risk group. The IPI risk group was a strong prognostic factor for PFS using multivariate analysis (HR = 7.02 and 23.78, 95 % confidence interval [CI] = 2.63–18.75 and 8.26–68.46, and p < 0.001 and <0.001 for intermediate- and high-risk groups, respectively). Underweight (<18.5 kg/m2) or overweight BMI (23–<25 kg/m2) was not significantly associated with PFS. However, obese BMI (25–<30 kg/m2) was a favorable prognostic factor for PFS compared to normal BMI group (18.5–<23 kg/m2) (HR = 0.40 and 0.43, 95 % CI = 0.18–0.86 and 0.19–0.98, and p = 0.020 and 0.046 for univariate and multivariate analyses, respectively).
The subgroup with low VAT ratios (first tertile) was not significantly associated with PFS, while the high VAT ratio (third tertile) subgroup was an independent prognostic factor for PFS, when the mid-tertile subgroup was set as the reference group. (HR = 2.87, 95 % CI = 1.30–6.32, and p = 0.009 in multivariate analysis; Table 4 and Fig. 2a).
Kaplan-Meier curve for PFS and OS. a Patients with high VAT ratios (third tertile group) had shorter PFS compared to those with low or intermediate VAT ratios (first or mid-tertile groups). *Results of univariate analysis. b Patients with high VAT ratios (third tertile group) had shorter OS compared to those with low or intermediate VAT ratios (first or mid-tertile groups). *Results of univariate analysis
Prognostic factors for OS
The IPI risk group was a strong prognostic factor for OS in multivariate analysis (HR = 4.75 and 14.31, 95 % CI = 2.13–10.63 and 5.70–35.92, and p < 0.001 and <0.001 for the intermediate- and high-risk groups, respectively). However, sex and BMI were not significant prognostic factors for OS. For example, obese BMIs were not a significant prognostic factor for OS (HR = 0.64 and 0.61, 95 % CI = 0.32–1.24 and 0.29–1.29, and p = 0.18 and 0.20 for univariate and multivariate analyses, respectively) compared to that for PFS.
Similar to the results from the PFS prognosticator analysis, high VAT ratios (third tertile) were an independent prognostic factor for OS (HR = 2.13 and 2.66, 95 % CI = 1.12–4.04 and 1.30–5.44, and p = 0.007 in univariate and multivariate analyses; Table 5 and Fig. 2b).
Discussion
Our study showed that high VAT ratios (third tertile, ranging from 0.381 to 0.647 in our study population) were an independent adverse prognostic factor for PFS and OS in patients with DLBCL who were treated with first-line R-CHOP. The IPI risk group is a well-characterized prognostic factor for both PFS and OS in DLBCL; therefore, we performed multivariate analyses after stratifying the study population based on the IPI risk groups. The VAT ratio was an independent prognostic factor after the effect of the IPI risk group was removed.
Previous studies on the association between survival and BMI in cancer patients have reported inconsistent observations. High BMIs (>24 kg/m2) were reported as a poor prognostic factor in Chinese premenopausal women with triple-negative breast cancers [20]. A study using the Adjuvant Colon Cancer Endpoints (ACCENT) database (n = 25,291) showed that obese men (≥35 kg/m2) had significantly poorer disease-free survival compared to overweight and normal-weight men [21]. In contrast, Sandra et al. [22] reported a positive association between high BMIs (>25 kg/m2) and survival in patients with oropharyngeal carcinoma treated with three-dimensional conformal radiotherapy or intensity-modulated radiotherapy. In addition, another study of renal cell carcinoma (RCC) reported that the association between BMI and OS varied according to histologic subtypes; increased BMI was a favorable prognostic factor for clear cell RCC, whereas in the chromophobe RCC subtype, it was an indicator of poor prognosis [23]. These differences in the correlation of BMI with cancer prognosis based on tumor types and histopathology may not be due to only the underlying differences in tumor biology, but also because BMI may not be an appropriate tool for measuring the effect of human adiposity on cancer. As alternative and more accurate measures of adiposity, SAT and VAT levels have been widely studied.
Some studies have addressed the impact of human adiposity on the prognosis of DLBCL. Previous pharmacokinetic studies suggested that obesity had a significant impact on the metabolism and clearance of drugs, including doxorubicin and rituximab [24, 25]. Modifications in tissue blood flow and phenotypic activity of hepatic metabolizing enzymes in obese patients might be an explanation for differential drug clearance [26, 27]. The altered half-life of drugs in the R-CHOP regimen, due to differential metabolism and clearance, could impact the prognosis of DLBCL, by directly altering the rates of progression and relapse. One study suggested that specific receptors expressed in adipose tissue could be associated with drug metabolism, thus indicating that the differences in distributions of fat tissue could alter drug clearance and time of drug exposure [26].
Our results showed that VAT ratios were an independent prognostic factor for both PFS and OS, while obese BMIs were an independent prognostic factor for PFS only. We propose a model in which adipose tissue, and/or the receptor expression profile therein, impacts PFS due to adiposity-driven differential drug metabolism and clearance. Moreover, in our proposed model, the VAT ratio plays an additional role in altering the OS of DLBCL patients.
DLBCL is a malignancy of B lymphocytes, one of the main types of immune cells. VAT is, in turn, conjunctly associated with immune functions [28]. Therefore, different volumes and proportions of VAT may be associated with the outcomes of DLBCL via its effect on immune function. Fatty acids released from VAT can escape hepatic metabolism and contribute to insulin resistance [29]. VAT is not merely a space-occupying building block, but a type of endocrine organ, and the cytokines secreted by adipose cells play an important role in insulin resistance and chronic inflammation associated with tumor progression [30]. VAT is associated with increased expression of adipokine receptors and elevated levels of circulating leptin and adiponectin [31, 32]. First, a VAT-mediated increase in leptin upregulates reactive oxygen species (ROS), which in turn leads to increased circulating glucose and insulin, and ultimately, inflammation.[33] Second, VAT induces hypoxic inducible factor-1α (HIF-1α), causing a hypoxic microenvironment, an important determinant of malignancy and chemo-resistance of tumors [34, 35].
There were several studies that another cellular components of adipose tissue, mesenchymal stromal/stem cells might have a protective effect against the spontaneous or drug-induced apoptosis of malignant lymphoid cells [36, 37]. Poor prognosis in patients with high VAT ratio might be associated with the function of mesenchymal stromal cells in human adipose tissue.
The last point to consider is the routinely used-dose capping rule at body surface area (BSA) of 2 m2 when to administer chemotherapeutic drugs to a patient whose BSA is more than 2 m2. So, if this rule is applied to patients, highly obese patients have a tendency to be undertreated considering their real BSA. BSAs between different groups of VAT ratio were not significantly different in our study population (mean ± SD of BSA 1.64 ± 0.20 and 1.65 ± 0.18 for mid-tertile and low VAT ratio, 1.69 ± 0.15 for high VAT ratio, respectively, p = 0.3). Furthermore, there were only five patients whose BSAs were more than 2 m2 (two patients in low VAT group, two patients in mid VAT group, one patient in high VAT group).
Based on these and our data, we propose that increased human adipose tissue, especially VAT, adversely affects the OS of DLBCL patients.
VAT has been considered a key contributor to poor cancer outcomes in terms of anthropometry.
However, absolute VAT volume is a less appropriate measure than is the VAT ratio, considering the remarkable variability in human physique [38]. Only one study has measured VAT in patients with DLBCL [39]. This study highlighted adipopenia as a prognostic factor for both PFS and OS in DLBCL. Although investigators in this study recognized VAT as a different compartment of adipose tissue, they did not use the VAT ratio as a variable in their analyses [39].
Our study does have several limitations. Our study population included a small number of DLBCL patients. The association between prognosis and the two extreme BMI subgroups (underweight and superobese BMIs) could not be analyzed due to the small number of patients within these subgroups. However, our study offers additional insight into the impact of adiposity on the prognosis of DLBCL; one novel finding is that the VAT ratio may be a better prognostic factor than BMI for DLBCL patients who are scheduled to be treated with frontline R-CHOP. Further large prospective studies are needed to confirm the relationship between measures of adiposity and prognosis of DLBCL.
References
Chihara D, Ito H, Matsuda T, Shibata A, Katsumi A, Nakamura S, Tomotaka S, Morton LM, Weisenburger DD, Matsuo K (2014) Differences in incidence and trends of haematological malignancies in Japan and the United States. Br J Haematol 164(4):536–545. doi:10.1111/bjh.12659
Wilder RB, Rodriguez MA, Medeiros LJ, Tucker SL, Ha CS, Romaguera JE, Pro B, Hess MA, Cabanillas F, Cox JD (2002) International prognostic index-based outcomes for diffuse large B-cell lymphomas. Cancer 94(12):3083–3088. doi:10.1002/cncr.10583
Rosenwald A, Wright G, Chan WC, Connors JM, Campo E, Fisher RI, Gascoyne RD, Muller-Hermelink HK, Smeland EB, Giltnane JM, Hurt EM, Zhao H, Averett L, Yang L, Wilson WH, Jaffe ES, Simon R, Klausner RD, Powell J, Duffey PL, Longo DL, Greiner TC, Weisenburger DD, Sanger WG, Dave BJ, Lynch JC, Vose J, Armitage JO, Montserrat E, Lopez-Guillermo A, Grogan TM, Miller TP, LeBlanc M, Ott G, Kvaloy S, Delabie J, Holte H, Krajci P, Stokke T, Staudt LM, Lymphoma/Leukemia Molecular Profiling P (2002) The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med 346(25):1937–1947. doi:10.1056/NEJMoa012914
Larsson SC, Wolk A (2011) Body mass index and risk of non-Hodgkin's and Hodgkin's lymphoma: a meta-analysis of prospective studies. Eur J Cancer 47(16):2422–2430. doi:10.1016/j.ejca.2011.06.029
Tarella C, Caracciolo D, Gavarotti P, Argentino C, Zallio F, Corradini P, Novero D, Magnani C, Pileri A (2000) Overweight as an adverse prognostic factor for non-Hodgkin's lymphoma patients receiving high-dose chemotherapy and autograft. Bone Marrow Transplant 26(11):1185–1191. doi:10.1038/sj.bmt.1702692
Bhaskaran K, Douglas I, Forbes H, dos-Santos Silva I, Leon DA, Smeeth L (2014) Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 384(9945):755–765. doi:10.1016/S0140-6736(14)60892-8
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371(9612):569–578. doi:10.1016/S0140-6736(08)60269-X
Tehard B, Lahmann PH, Riboli E, Clavel-Chapelon F (2004) Anthropometry, breast cancer and menopausal status: use of repeated measurements over 10 years of follow-up-results of the French E3N women's cohort study. Int J Cancer 111(2):264–269. doi:10.1002/ijc.20213
Castillo JJ, Ingham RR, Reagan JL, Furman M, Dalia S, Mitri J (2014) Obesity is associated with increased relative risk of diffuse large B-cell lymphoma: a meta-analysis of observational studies. Clin Lymphoma Myeloma Leuk 14(2):122–130. doi:10.1016/j.clml.2013.10.005
Carson KR, Bartlett NL, McDonald JR, Luo S, Zeringue A, Liu J, Fu Q, Chang SH, Colditz GA (2012) Increased body mass index is associated with improved survival in United States veterans with diffuse large B-cell lymphoma. J Clin Oncol Off J Am Soc Clin Oncol 30(26):3217–3222. doi:10.1200/JCO.2011.39.2100
Geyer SM, Morton LM, Habermann TM, Allmer C, Davis S, Cozen W, Severson RK, Lynch CF, Wang SS, Maurer MJ, Hartge P, Cerhan JR (2010) Smoking, alcohol use, obesity, and overall survival from non-Hodgkin lymphoma: a population-based study. Cancer 116(12):2993–3000. doi:10.1002/cncr.25114
Hong F, Habermann TM, Gordon LI, Hochster H, Gascoyne RD, Morrison VA, Fisher RI, Bartlett NL, Stiff PJ, Cheson BD, Crump M, Horning SJ, Kahl BS (2014) The role of body mass index in survival outcome for lymphoma patients: US intergroup experience. Ann Oncol 25(3):669–674. doi:10.1093/annonc/mdt594
Jones JA, Fayad LE, Elting LS, Rodriguez MA (2010) Body mass index and outcomes in patients receiving chemotherapy for intermediate-grade B-cell non-Hodgkin lymphoma. Leuk Lymphoma 51(9):1649–1657. doi:10.3109/10428194.2010.494315
Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, Vasan RS, Murabito JM, Meigs JB, Cupples LA, D'Agostino RB Sr, O'Donnell CJ (2007) Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham heart study. Circulation 116(1):39–48. doi:10.1161/CIRCULATIONAHA.106.675355
Ibrahim MM (2010) Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev 11(1):11–18. doi:10.1111/j.1467-789X.2009.00623.x
Clark W, Siegel EM, Chen YA, Zhao X, Parsons CM, Hernandez JM, Weber J, Thareja S, Choi J, Shibata D (2013) Quantitative measures of visceral adiposity and body mass index in predicting rectal cancer outcomes after neoadjuvant chemoradiation. J Am Coll Surg 216(6):1070–1081. doi:10.1016/j.jamcollsurg.2013.01.007
Rockall AG, Sohaib SA, Evans D, Kaltsas G, Isidori AM, Monson JP, Besser GM, Grossman AB, Reznek RH (2003) Computed tomography assessment of fat distribution in male and female patients with Cushing's syndrome. Eur J Endocrinol 149(6):561–567
WHOE Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403):157–163. doi:10.1016/S0140-6736(03)15268-3
Oh SW, Shin SA, Yun YH, Yoo T, Huh BY (2004) Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res 12(12):2031–2040. doi:10.1038/oby.2004.254
Hao S, Liu Y, Yu KD, Chen S, Yang WT, Shao ZM (2015) Overweight as a prognostic factor for triple-negative breast cancers in Chinese women. PLoS One 10(6), e0129741. doi:10.1371/journal.pone.0129741
Sinicrope FA, Foster NR, Yothers G, Benson A, Seitz JF, Labianca R, Goldberg RM, Degramont A, O'Connell MJ, Sargent DJ, Adjuvant Colon Cancer Endpoints G (2013) Body mass index at diagnosis and survival among colon cancer patients enrolled in clinical trials of adjuvant chemotherapy. Cancer 119(8):1528–1536. doi:10.1002/cncr.27938
Ottosson S, Soderstrom K, Kjellen E, Nilsson P, Zackrisson B, Laurell G (2014) Weight and body mass index in relation to irradiated volume and to overall survival in patients with oropharyngeal cancer: a retrospective cohort study. Radiat Oncol 9:160. doi:10.1186/1748-717X-9-160
Lee WK, Hong SK, Lee S, Kwak C, Oh JJ, Jeong CW, Kim YJ, Kang SH, Hong SH, Byun SS (2015) Prognostic value of body mass index according to Histologic subtype in nonmetastatic renal cell carcinoma: a large cohort analysis. Clin Genitourin Cancer 13(5):461–468. doi:10.1016/j.clgc.2015.04.012
Muller C, Murawski N, Wiesen MH, Held G, Poeschel V, Zeynalova S, Wenger M, Nickenig C, Peter N, Lengfelder E, Metzner B, Rixecker T, Zwick C, Pfreundschuh M, Reiser M (2012) The role of sex and weight on rituximab clearance and serum elimination half-life in elderly patients with DLBCL. Blood 119(14):3276–3284. doi:10.1182/blood-2011-09-380949
Rodvold KA, Rushing DA, Tewksbury DA (1988) Doxorubicin clearance in the obese. J Clin Oncol Off J Am Soc Clin Oncol 6(8):1321–1327
Hanley MJ, Abernethy DR, Greenblatt DJ (2010) Effect of obesity on the pharmacokinetics of drugs in humans. Clin Pharmacokinet 49(2):71–87. doi:10.2165/11318100-000000000-00000
Baker SD, van Schaik RH, Rivory LP, Ten Tije AJ, Dinh K, Graveland WJ, Schenk PW, Charles KA, Clarke SJ, Carducci MA, McGuire WP, Dawkins F, Gelderblom H, Verweij J, Sparreboom A (2004) Factors affecting cytochrome P-450 3A activity in cancer patients. Clin Cancer Res 10(24):8341–8350. doi:10.1158/1078-0432.CCR-04-1371
Marti A, Marcos A, Martinez JA (2001) Obesity and immune function relationships. Obes Rev 2(2):131–140
Klein S (2004) The case of visceral fat: argument for the defense. J Clin Invest 113(11):1530–1532. doi:10.1172/JCI22028
Lanthier N, Leclercq IA (2014) Adipose tissues as endocrine target organs. Best Pract Res Clin Gastroenterol 28(4):545–558. doi:10.1016/j.bpg.2014.07.002
Howard JM, Beddy P, Ennis D, Keogan M, Pidgeon GP, Reynolds JV (2010) Associations between leptin and adiponectin receptor upregulation, visceral obesity and tumour stage in Oesophageal and junctional adenocarcinoma. Br J Surg 97(7):1020–1027. doi:10.1002/bjs.7072
Cummings DE, Foster KE (2003) Ghrelin-leptin tango in body-weight regulation. Gastroenterology 124(5):1532–1535
Aggarwal BB, Vijayalekshmi RV, Sung B (2009) Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res 15(2):425–430. doi:10.1158/1078-0432.CCR-08-0149
Ye J, Gao Z, Yin J, He Q (2007) Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am J Physiol Endocrinol Metab 293(4):E1118–E1128. doi:10.1152/ajpendo.00435.2007
Feldser D, Agani F, Iyer NV, Pak B, Ferreira G, Semenza GL (1999) Reciprocal positive regulation of hypoxia-inducible factor 1alpha and insulin-like growth factor 2. Cancer Res 59(16):3915–3918
Zhang Y, Hu K, Hu Y, Liu L, Wang B, Huang H (2014) Bone marrow mesenchymal stromal cells affect the cell cycle arrest effect of genotoxic agents on acute lymphocytic leukemia cells via p21 down-regulation. Ann Hematol 93(9):1499–1508. doi:10.1007/s00277-014-2069-1
Medina DJ, Goodell L, Glod J, Gelinas C, Rabson AB, Strair RK (2012) Mesenchymal stromal cells protect mantle cell lymphoma cells from spontaneous and drug-induced apoptosis through secretion of B-cell activating factor and activation of the canonical and non-canonical nuclear factor kappaB pathways. Haematologica 97(8):1255–1263. doi:10.3324/haematol.2011.040659
Kaess BM, Pedley A, Massaro JM, Murabito J, Hoffmann U, Fox CS (2012) The ratio of visceral to subcutaneous fat, a metric of body fat distribution, is a unique correlate of cardiometabolic risk. Diabetologia 55(10):2622–2630. doi:10.1007/s00125-012-2639-5
Camus V, Lanic H, Kraut J, Modzelewski R, Clatot F, Picquenot JM, Contentin N, Lenain P, Groza L, Lemasle E, Fronville C, Cardinael N, Fontoura ML, Chamseddine A, Brehar O, Stamatoullas A, Lepretre S, Tilly H, Jardin F (2014) Prognostic impact of fat tissue loss and cachexia assessed by computed tomography scan in elderly patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Eur J Haematol 93(1):9–18. doi:10.1111/ejh.12285
Acknowledgments
This study was supported by a grant of the Korea Institute of Radiological and Medical Sciences (KIRAMS), funded by Ministry of Science, ICT and Future Planning, Republic of Korea (No. 1711021931 & 1711021780).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, DY., Kim, A., Byun, B.H. et al. Visceral adipose tissue is prognostic for survival of diffuse large B cell lymphoma treated with frontline R-CHOP. Ann Hematol 95, 409–416 (2016). https://doi.org/10.1007/s00277-015-2571-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2571-0