Abstract
Pediatric ECG standards have been defined without echocardiographic confirmation of normal anatomy. The Pediatric Heart Network Normal Echocardiogram Z-score Project provides a racially diverse group of healthy children with normal echocardiograms. We hypothesized that ECG and echocardiographic measures of left ventricular (LV) dimensions are sufficiently correlated in healthy children to imply a clinically meaningful relationship. This was a secondary analysis of a previously described cohort including 2170 digital ECGs. The relationship between 6 ECG measures associated with LV size were analyzed with LV Mass (LVMass-z) and left ventricular end-diastolic volume (LVEDV-z) along with 11 additional parameters. Pearson or Spearman correlations were calculated for the 78 ECG-echocardiographic pairs with regression analyses assessing the variance in ECG measures explained by variation in LV dimensions and demographic variables. ECG/echocardiographic measurement correlations were significant and concordant in 41/78 (53%), though many were significant and discordant (13/78). Of the 6 ECG parameters, 5 correlated in the clinically predicted direction for LV Mass-z and LVEDV-z. Even when statistically significant, correlations were weak (0.05–0.24). R2 was higher for demographic variables than for echocardiographic measures or body surface area in all pairs, but remained weak (R2 ≤ 0.17). In a large cohort of healthy children, there was a positive association between echocardiographic measures of LV size and ECG measures of LVH. These correlations were weak and dependent on factors other than echocardiographic or patient derived variables. Thus, our data support deemphasizing the use of solitary, traditional measurement-based ECG markers traditionally thought to be characteristic of LVH as standalone indications for further cardiac evaluation of LVH in children and adolescents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Electrocardiograms (ECGs) are a primary screening test for cardiac disease in children. In most studies, ECG standards in healthy populations have been defined by normal clinical examination or limited echocardiographic confirmation of normal cardiac anatomy [1,2,3]. Historically, data correlating ECG measurements with a racially diverse population and a range of left ventricular (LV) dimensions over the pediatric age group are scant [4], with most data limited to ECGs from more focused disease specific cohorts.
The database from the Pediatric Heart Network (PHN) Normal Echocardiogram Z-score Project provides a racially diverse, age/sex classified group of 3215 healthy children with normal echocardiograms and no systemic disease [5]. Echocardiograms were matched with contemporaneous digitally acquired ECGs, when available (N = 2170), allowing synchronous comparison and pre-planned sub-analyses of echocardiogram and ECG correlations in this large, diverse, and healthy pediatric cohort. An initial analysis of this dataset evaluated the age, sex and racial distinctions among common ECG measurements [6] and found that the potential measures of left ventricular hypertrophy (LVH), such as R wave amplitude in V5 and V6, QRS axis and S wave amplitude in V1 had both statistical and potentially clinically important sex and race dependent differences that were most notable in the older age groups.
Using data from the PHN Echocardiogram Z-Score and ECG Database, it was possible to evaluate how much of the variation in the ECG measures commonly used to identify LVH in normal patients is explained by echocardiographic measures of LV size which includes individual measures of LV mass, LV dimension and LV geometry, as opposed to other measured or unmeasured patient factors. We hypothesized that echocardiographically derived z-scores of LV size and ECG measures [5] commonly used to identify LVH are correlated in this healthy population of infants, children and adolescents. Specifically, this study aimed to evaluate the direction and strength of correlations between common ECG measures of LVH and validated echocardiographic measurements of LV dimensions and mass in a healthy heterogeneous North American pediatric cohort.
Methods
Study Design
Demographic and clinical data, echocardiographic images and ECGs were collected from the records of healthy children at 19 centers in the PHN under the Echocardiogram Z-Score and ECG Database protocol. Because all data and images were collected retrospectively and were de-identified before submission, most children were enrolled under a waiver of consent after Institutional Review Board (IRB) or Research Ethics Board (REB) approval was obtained at each participating center. Race/ethnicity information was not routinely obtained at 1 center and was collected prospectively for eligible subjects after local regulatory approval. Some centers were able to perform research echocardiograms without charge and prospectively enrolled healthy children under Institutional Review Board approval and informed consent. This was done primarily to increase the number of infants with validated racial classifications.
Study Population and Measures
The study population represents a convenience sample subset of the Echocardiogram Z-Score and ECG Database study. Healthy children ≤ 18.0 years old with echocardiograms performed after January 2008 and with documentation of age, height, weight, sex, and self-reported race were eligible for this study. Healthy children were identified by having a normal echocardiogram and no evidence of cardiac, inherited or medical disease on review of the available medical records. Children were excluded for evidence of acquired or congenital heart disease, corrected gestational age < 37 weeks, obesity (BMI > 95%), acute or systemic disorder typically associated with cardiovascular manifestations, first-degree relative with a non-ischemic cardiomyopathy, first-degree relative with a left-sided obstructive congenital heart lesion, or ECG waveforms that did not meet minimum digital standards or were inadequate for analysis.
Age groups were pre-specified in the protocol. Self-reported race and ethnicity were divided into three categories for the study: White, African-American, and other (Hispanic, Asian, Pacific Islander, Native American, and multiracial). Available ECGs with minimum standards of 12 leads, 10-s recording, sampling rate > 500 Hz, and 150 Hz bandwidth in exportable digital format (MUSE, GE Healthcare, Waukesha, WI or Philips Healthcare, Andover, MA) were collected closest to the date of the echocardiogram and included in the analysis. Children enrolled in the PHN Echocardiogram Z-Score and ECG Database Project who had a digital 12-lead ECG (N = 2619) uploaded to the database were included in this analysis. Details of both the echocardiogram [5] and the ECG data [6] have been previously published. The indications for the echocardiogram or the ECG were not recorded.
This is a secondary analysis of the Echocardiogram Z-Score and ECG Database study. The writing committee a priori identified 6 common ECG measures historically associated with increasing LV size (Table 1) and the Z-scores [5] of 13 echocardiographic measurements of LV size, volume and geometry (Table 2). The Echocardiogram Z-Score and ECG Database primary outcome measures were pre-specified as LV mass Z-score (LVMass-z) and LV end diastolic volume Z-score (LVEDV-z). ECG voltage measurements had an inter-reader variability of 0.15 mv [6] and echo measurements had a reported margin of error of 0.045–0.075 [5]. Prior analysis had evaluated the relationships between sex, age and race on ECG measurements [6]. Additional analysis was performed to evaluate the effect of BSA on ECG measurements of LVH. The hypothesis was that ECG measurements are affected in similar fashion to echocardiographic BSA Z-scores [5]; therefore, subjects with greater BSA will have higher voltage amplitudes for ECG measurements, even after accounting for effects of age.
Statistical Methods
Plots were developed for ECG measures vs. echocardiographic Z-scores, with locally weighted scatterplot smoothing (LOESS) curve fitting. Correlations were computed, either Pearson correlation (if a linear relationship) or Spearman correlation (if non-linear). There are 78 potential ECG-Echocardiographic Z-score pairs. Of the 6 ECG measures, 3 (RV6, RV5 and RV6+ the absolute value of SV1) would be expected to have positive correlations with increasing measurements of LV size and mass. The remainder (SV1, QIII and frontal plane QRS axis) are typically viewed as more negative values correlating with increasing LV dimensions. For clarity, correlations in the expected direction are referred to as concordant correlations and those in the unexpected direction (e.g. a negative correlation of RV6 and LV mass-z) are discordant correlations.
Regression models were developed to fit ECG measures as the outcome and echocardiographic Z-scores as the main predictor, with appropriate transformations as required. Other potential predictors included patient demographics: age group (< 1 month, 1 month to < 3 years, 3 to < 6 years, 6 to < 12 years, 12 to < 16 years, 16 to 18 years), sex, race, and body surface area (BSA; calculated by Haycock method). Based on LOESS curve fitting, BSA was treated as piece-wise linear in its associations with ECG measures. As age and BSA are highly correlated, in preliminary analysis, effects of age group vs. BSA were compared to determine which was more associated with ECG measures. The more associated factor, based on comparison of R2 (amount of variance explained), was chosen for further modelling.
The R2 of 3 models was calculated to assess how much variance in ECG measures was explained by these predictors: (1) echocardiographic Z-score as the only predictor, (2) patient demographics as the only predictors, and (3) echocardiographic Z-score plus patient demographics. This allowed a comparison of the relative contributions of echocardiographic Z-scores vs. patient demographics on ECG measures.
Results
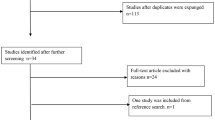
As previously reported, among 2619 ECGs uploaded to the PHN data grid, the core lab excluded 219 due to inadequate quality of waveforms, leaving 2400 available for this analysis. Intra-reader variability was < 2 ms for all intervals and < 0.10 mV for all amplitudes [6]. The echocardiographic images came from 3215 in the primary cohort which had adequate images. Effective unique-paired ECG-echocardiographic measurements were available on 2170 which was the cohort analyzed. ECG and Echos were obtained within 30 days in 95% of the subjects, with 0.5% obtained more than a year apart. By design, each of the six age groups had a target of at least 60 participants of each race and sex combination. While not all targets were met, there were 28–106 participants of each age/sex/race combination, with 253–477 participants in each age group (median 7.5 years, mean 8.2 years) and 47% female 6. Race data revealed 35% White, 31% African-American, and 34% other. The “other” classification was accepted because bin sizes for any additional subclassification were reliably small. Ethnicity data revealed 25% Hispanic, 70% non-Hispanic, and 5% unknown. Height ranged from 45.0 to 207.2 cm (median 125.0 cm), weight from 2.3 to 122.6 kg (median 31.8 kg), and BSA from 0.18 to 2.67 (median 0.93). Intraobserver variability at the Echocardiographic Core Laboratory was low with an intraclass correlation coefficient of 1.00 and Pearson correlations > 0.99 for all 5 parameters [5].
The ECG and echocardiographic measurement correlations were significant and in the concordant direction in 41/78 (53%) but significant and discordant in 13/78 (17%) of the paired measures and had no significant correlation in 24/78 (31%) pairs (Table 3). Of the 6 available ECG measures of LV size, 5 correlated in the clinically concordant direction with the primary echocardiographic outcome measures of LVMass-z and LVEDV-z (Table 3). The Q wave amplitude in Lead III correlated with those measures; however, the direction of the correlation was opposite of what would be expected with increasing LV dimensions. While many correlations were statistically significant, the magnitudes of the associations were low (0.05–0.24). The positive correlation between R wave amplitude in V5 and LVEDV-z was the single most strongly correlated pair with a correlation of 0.244 (p < 0.001). Figure 1 highlights both the statistically strong but practically and clinically weak pattern of these associations.
Positive concordant correlation between R wave amplitude in V5 and left ventricular end diastolic volume Z-score. This scatter graph with LOESS curve fitting between R wave amplitude in V5 and left ventricular end diastolic volume Z-score shows the strongest single correlation identified. This highlights both the statistically strong but clinically weak correlation
ECG measurements using lateral R wave amplitudes (RV6, RV5 and RV6 + SV1) correlated with the most echocardiographic measures of LV dimensions (Table 3), with 8/13 correlated in concordant fashion and 2/13 in discordant fashion. The Q amplitude in Lead III was least frequently correlated with concordant correlations in only 5/13 measures and discordant correlations in 2/13.
While the two primary echocardiographic outcomes measures, LVmass-z and LVEDV-z, had concordant correlations with 5 of 6 ECG measures there was more variability in the strength of the ECG-echocardiographic correlation with other echocardiographic measures and some had no significant or generally discordant correlations to ECG measures. Three of the echo measures that were highly discordant were calculated ratios (LVMTV-z. LVTTD-z and LVSI-z). With these, 13/18 ECG measures were significant but discordant and 5/18 were not correlated.
Although BSA is a significant predictor of some ECG parameters, age group explained slightly more of the variance in ECG parameters and addition of BSA to age group explained only minimally more of the variance (e.g., an additional 2% for RV6; an additional 1% for SV1). Therefore, age group was selected for further consideration in modelling of demographic factors.
Linear regression modeling for influences of echocardiographic measure of size, dimension and geometry on ECG measures yielded low R2, with a maximum of 0.06 (Table 4). Modelling for influences of demographics explained more variance in ECG measures, with R2 of 0.09–0.15. Addition of echocardiographic Z-scores to models with demographics explained little to no additional variance.
Discussion
The presumption that certain ECG measures may be used as a proxy for LV size is well accepted in cardiology. Low cost, ease of acquisition, ready availability and long history have assured widespread ECG use for screening normal populations of children and in clinical situations where the prior probability of heart disease is similar to the general population (e.g., preoperatively and prior to prescription of certain drugs. There is clearly a significant positive correlation between conventional measures of LVH such as lateral R wave and posteriorly directed S wave amplitudes, particularly for LVMass-z and LVEDV-z. Many of the potential relationships were statistically strong, as expected given the large available sample size. However, they may not be clinically important since the relations between ECG and echocardiographic metrics of LV size were remarkably weak (correlations under 0.25, explaining little of the ECG and anatomic variance). This finding applies to echocardiographic measures of LV mass, wall thickness, dimensions or geometry.
The current analysis included only healthy children with normal echocardiograms, and thus provides a useful reference metric but not a true predictive data set capable of identifying pathological thresholds. Several analyses of the modern ECG that include patients with clinically proven LVH support our observation that the correlation between ECG measurements and LV mass is weak, even outside the range of normal. Bratincsak [7] compared children with normal echocardiograms to those known to have LVH in a 3:1 ratio and demonstrated no correlation of RV6 and other common ECG measures and LV mass. The P2C2 cohort [4] examined 148 children with paired echocardiographic/ECG measures who had a 7% incidence of elevated LV mass. They reported no significant correlation for RV6 in neonates after adjusting for BSA and age, although they did note a weak but unspecified correlation for SV1. Czosek analyzed correlations between RV6 and SV1 and LV mass in athletic adolescents presenting for screening. Their correlations were similar to ours, ranging from 0.002 to 0.18 [8]. Focusing on collegiate athletes, with 11 of 196 athletes meeting echocardiographic criteria for LVH, the correlation for left ventricular LV mass ranged from 0.18 to 0.3 [9]. Finally Tague and colleagues evaluated a large clinical experience that included children with both increased LV mass and LV dilation; and found similar data. The correlations between RV6 and LVEDV-z and indexed LV mass were poor at 0.14 and 0.24, respectively [10]. Taken together, clinical use of the ECG even in cohorts with a higher frequency of pathology had no more than a weak association with increased LV size.
Additional difficulties in development of ECG standards are the differences in testing acquisition. Recent analyses of pediatric ECGs, including the present study, used high frequency digital acquisition. As a result, voltage measurements were higher for those measures classically used to determine LVH and may partially explain the poor correlations from recent studies [3, 6] compared with the historically widely used study reported by Davignon [1]. For example, the 98%ile for R wave amplitude in V6 for boys aged 12–16 years increased from 24.1 mV [1] to 30.5 mV [3] to 33.57 mV [6], with similar increases in mean amplitudes. Davignon acquired signals at 250 Hz followed by digital to analog conversion at 333/s. Rijnbeck acquired signals at 1200 Hz, then used a proprietary program to create an averaged signal. That approach effectively both increases the high pass filter and then inserts a lower high pass filter by averaging. The modern GE systems used by the majority of centers samples at 16,000 Hz and then analyzes and exports signals at 500 Hz. The Philips systems used by the remainder of the groups acquires at 4 MHz and then down samples to 500 Hz. As recently as 2001 the recommended minimal sampling rate was 150 Hz [11]. Each increase in sampling decreases the variability of measurements, however the same changes increase the potential to record high frequency components of those waves and increase the peak measurement (and the error in that measurement) [12]. The values that were obtained in this study are very comparable to the age and sex based Z-score analysis Bratincsak et al. developed using an alternative analysis strategy, while similarly using modern GE equipment [13]. Differences between printed and digitally displayed tracings have yet another source of practical variability in clinical practice. Hence, the technical processing of acquiring the wave form, post-acquisition processing and then display of the wave forms clearly impact the final determination of signal amplitude.
The correlations, while weak, are concordant for the 5 precordial lead combinations analyzed with the primary echocardiographic endpoints of LVMass-Z and LVEDV-z, arguing for at least some relationship between ECG voltage and echocardiographic parameters of LV mass/size. Unfortunately, 4 of the echocardiographic measures had minimal or even discordant/inverse relationships with ECG measures underscoring the difficulty in dependence on ECG for LV size at least within healthy patients. Three of those measures were ratios as opposed to direct measurements. As ECG voltages reflect the net electrical force in that lead and do not reliably have a direct relationship to a specific anatomic location, opposing changes in LV size may produce offsetting vectors.
The exceptionally low correlation between echocardiographic measurements of the LV and ECG measures implies that other patient features have a substantial role in the variability. The role of age, race and sex on ECG voltages was previously confirmed in this cohort [6]. In contrast, these factors did not influence echocardiographic Z-scores [5], after accounting for effects of BSA. The current analysis suggests that unlike echocardiographic Z-scores, BSA has negligible predictive power on ECG parameters after accounting for age group. Therefore, BSA does not need to be incorporated into the previously published mean ± SD and 2nd/98th percentiles for ECG parameters or other population norms. Our analysis for confounding interactions between age group, sex, and race or BSA failed to identify additional correlation. Those data are concordant with Bratincsak’s analysis of the role of BSA (personal communication) [13].
Variability in the ECG lead placement may explain some variance. At a basic physiology and measurement level, the precordial voltages are surface representations of the ventricular mass at the apex of the essentially conical reflection of the region of myocardium that can be viewed as a solid angle of electrical activity [14]. Clinically these concerns are clearly reflected in variation in the ECG. Systematic analysis of different limb lead positions showed that more proximal placement resulted in rightward axis shifts and increased precordial voltages that would support LVH (S V1/RV5, V6) [15]. Voltage differences of 0.1 to 0.5 millivolts may occur over 1 cm spatial differences, which is a 20–40% difference in the magnitude of adolescent lateral R waves [16]. While the samples are small, studies in adults using chest radiographs, cardiac MRI and chest computed tomography show anatomic variation in the cardiac axis of 10°–30° with low correlation between the QRS electrical axis on ECG and the measured anatomic axis [17, 18]. This adds yet another source of variation in the ECG that would not be included in either this study or standard clinical practice. Current guidelines for standardized interpretation of ECG [19] raise the concerns of the influence of body habitus and daily variation voltage as other potential contributors to variation in ECG measures. This routine technical and anatomic variation may have effects on the ECG that are comparable to the underlying cardiac anatomy and actual LV mass.
Limitations
Since this cohort included only healthy children with a normal echocardiogram and specifically excluded obese children, and those with hypertension it may not be generalizable to other populations. The original PHN cohort, while actively recruited to have sufficient African-American subjects for meaningful analysis, was not able to identify sufficient numbers of children with any other racial identification. This was at least in part because the participating hospitals did not reliably code for the standard NIH racial and ethnic group classification. While the matched ECGs and echocardiograms were contemporaneous, the indication for neither the ECG nor the echocardiogram were recorded. It is likely that some echocardiograms may have been ordered because of ECG abnormalities. This analysis was also limited by its focus on simpler ECG measures associated with LV dominance; V7 and right precordial leads were not analyzed. The study design was based on a traditional reading of the ECG focusing on axis and leftward directed voltages as reflecting left ventricular dimensions. No attempt was made to use innovative machine learning based techniques [20] nor to expand the analysis to QRS-T angle or integrals [21]. These ECGs were obtained using standard clinical practice in a wide range of settings. No data were collected to ensure proper lead placement.
Conclusions
In a large, heterogeneous cohort of healthy children, there was a positive association between the echocardiographic measures of LV size and most of the commonly accepted ECG measures that focus on LVH. The correlations for LV dimensions were weak and little of the variability was explained by echocardiographic measurements nor by the addition of the factors of age, sex, race, or body surface area. This is despite prior relevant analysis of these data focusing entirely on the ECG measurements which demonstrated both higher amplitudes than older standards, and potentially clinically significant racial, ethnic and gender differences. While, by definition, the cohort analyzed here had no LVH, these data are completely in agreement with several recent analyses [7, 8, 13] selected to include echo documented LVH. Thus, our data support deemphasizing the use of solitary, traditional measurement-based ECG markers traditionally thought to be characteristic of LVH as standalone indications for further cardiac evaluation of LVH in children and adolescents.
The combinations of a weak relationship between anatomic aspects of LV dimensions and ECG voltages, increasing ECG voltages over the past 50 years related to technical shifts in ECG acquisition, and the complex and likely clinically meaningful relationship between age, race, sex and QRS amplitudes support the concept that more analytically demanding approaches like AI may be better suited to effectively use ECGs as a screening tool in a low prevalence setting.
References
Davignon A, Rautaharju P, Boisselle E, Soumis F (1979) Normal ECG standards for infants and children. Pediatr Cardiol 1:123–131
Rijnbeek PR, Witsenburg M, Hess J, Kors JA (2000) Continuous age-dependent normal limits for the pediatric electrocardiogram. J Electrocardiol 33(Suppl):199–201
Rijnbeek PR, Witsenburg M, Schrama E, Hess J, Kors JA (2001) New normal limits for the paediatric electrocardiogram. Eur Heart J 22:702–711
Rivenes SM et al (2003) Usefulness of the pediatric electrocardiogram in detecting left ventricular hypertrophy: results from the prospective pediatric pulmonary and cardiovascular complications of vertically transmitted HIV infection (P2C2 HIV) multicenter study. Am Heart J 145:716–723
Lopez L et al (2017) Relationship of echocardiographic z scores adjusted for body surface area to age, sex, race, and ethnicity: the Pediatric Heart Network Normal Echocardiogram Database. Circ Cardiovasc Imaging 10:979
Saarel EV et al (2018) Electrocardiograms in Healthy North American Children in the Digital Age. Circ Arrhythm Electrophysiol 11:e005808
Bratincsak A, Williams M, Kimata C, Perry JC (2015) The electrocardiogram is a poor diagnostic tool to detect left ventricular hypertrophy in children: a comparison with echocardiographic assessment of left ventricular mass. Congenit Heart Dis 10:E164–E171
Czosek RJ et al (2014) Relationship between echocardiographic LV mass and ECG based left ventricular voltages in an adolescent population: related or random? Pacing Clin Electrophysiol 37:1133–1140
Hedman K et al (2020) Limitations of electrocardiography for detecting left ventricular hypertrophy or concentric remodeling in athletes. Am J Med 133:123–132
Tague L et al (2018) Comparison of left ventricular hypertrophy by electrocardiography and echocardiography in children using analytics tool. Pediatr Cardiol 39:1378–1388
Rijnbeek PR, Kors JA, Witsenburg M (2001) Minimum bandwidth requirements for recording of pediatric electrocardiograms. Circulation 104:3087–3090
Bailey JJ et al (1990) Recommendations for standardization and specifications in automated electrocardiography: bandwidth and digital signal processing. A report for health professionals by an ad hoc writing group of the Committee on Electrocardiography and Cardiac Electrophysiology of the Council on Clinical Cardiology, American Heart Association. Circulation 81:730–739
Bratincsak A et al (2020) Electrocardiogram standards for children and young adults using Z-Scores. Circ Arrhythm Electrophysiol 13:e008253
Holland RP, Arnsdorf MF (1977) Solid angle theory and the electrocardiogram: physiologic and quantitative interpretations. Prog Cardiovasc Dis 19:431–457
Farrell RM, Syed A, Syed A, Gutterman DD (2008) Effects of limb electrode placement on the 12- and 16-lead electrocardiogram. J Electrocardiol 41:536–545
Kania M et al (2014) The effect of precordial lead displacement on ECG morphology. Med Biol Eng Comput 52:109–119
Engblom H et al (2005) The relationship between electrical axis by 12-lead electrocardiogram and anatomical axis of the heart by cardiac magnetic resonance in healthy subjects. Am Heart J 150:507–512
Hoekema R, Uijen GJ, van Erning L, van Oosterom A (1999) Interindividual variability of multilead electrocardiographic recordings: influence of heart position. J Electrocardiol 32:137–148
Hancock EW et al (2009) AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol 53:992–1002
Pollard JD et al (2021) Electrocardiogram machine learning for detection of cardiovascular disease in African Americans: the Jackson Heart Study. Eur Heart J Digit Health 2:137–151
Biering-Sorensen T et al (2018) Global ECG measures and cardiac structure and function: The ARIC Study (Atherosclerosis Risk in Communities). Circ Arrhythm Electrophysiol 11:e005961
Funding
The study was supported by grants (HL135680, HL135685, HL135683, HL135689, HL135646, HL135665, HL135678, HL135682, HL135666, HL135691, HL068270) from the National Heart, Lung, and Blood Institute, NIH. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official views of the National Heart, Lung, and Blood Institute, no other disclosures.
Author information
Authors and Affiliations
Consortia
Contributions
MEA prepared the main manuscript and tables with RG and FLT performing statistical analysis and preparing the figures. The overall study design was developed by LM, JK, EVS, MEA, RC and JT and approved by all members of the writing committee prior to analysis. MTF, TP and EVS managed the ECG core lab and LM managed the echocardiographic core lab. Additional editorial review was provided by the remaining members of the writing committee as well as written formal acceptance of the manuscript. In addition the PHN committee for publications reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alexander, M.E., Gongwer, R., Trachtenberg, F.L. et al. Limited Relationship Between Echocardiographic Measures and Electrocardiographic Markers of Left Ventricular Size in Healthy Children. Pediatr Cardiol 45, 1055–1063 (2024). https://doi.org/10.1007/s00246-024-03448-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-024-03448-2