Abstract
In pediatric echocardiography, cardiac dimensions are often normalized for weight, height, or body surface area (BSA). The combined influence of height and weight on cardiac size is complex and likely varies with age. We hypothesized that increasing weight for height, as represented by body mass index (BMI) adjusted for age, is poorly accounted for in Z scores normalized for weight, height, or BSA. We aimed to evaluate whether a bias related to BMI was introduced when proximal aorta diameter Z scores are derived from bivariate models (only one normalizing variable), and whether such a bias was reduced when multivariable models are used. We analyzed 1,422 echocardiograms read as normal in children ≤18 years. We computed Z scores of the proximal aorta using allometric, polynomial, and multivariable models with four body size variables. We then assessed the level of residual association of Z scores and BMI adjusted for age and sex. In children ≥6 years, we found a significant residual linear association with BMI-for-age and Z scores for most regression models. Only a multivariable model including weight and height as independent predictors produced a Z score free of linear association with BMI. We concluded that a bias related to BMI was present in Z scores of proximal aorta diameter when normalization was done using bivariate models, regardless of the regression model or the normalizing variable. The use of multivariable models with weight and height as independent predictors should be explored to reduce this potential pitfall when pediatric echocardiography reference values are evaluated.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In pediatric echocardiography, cardiac dimensions must be adjusted for body size, and Z score is currently the method of choice to normalize cardiac dimensions for body size [6]. The long-known linear relationship between body surface area (BSA) and cardiac output [21] has led many authors to normalize echocardiography dimensions for BSA [5, 24]. However, the choice of the normalizing variable (age, weight, height, or BSA) remains controversial. The various equations for BSA estimation do not differentiate between fat and muscle mass [14, 15, 22, 25], and some authors have argued that normalization for BSA may obscure the effect of obesity, especially on echocardiographic estimations of left ventricular mass [12, 13].
The influence of height and weight on cardiac size is complex and likely varies with age. Accurately predicting cardiac size based on measures of height and weight can be difficult. Nevertheless, most available nomograms are based on a single variable: height, weight, age, or a combined body size variable like BSA [24]. We have empirically observed that the effect of increasing weight for height on cardiac size changes with age. Consequently, we hypothesized that increasing weight for height, as represented by body mass index (BMI) adjusted for age and sex, is not well accounted for in Z scores normalized for weight, height, or BSA.
Our aim was to evaluate whether a bias related to BMI was introduced when proximal aorta diameter Z scores are derived from a single body size variable (bivariate models), and whether such a bias is reduced when multivariable models are used.
Materials and Methods
Population
Study subjects were children ≤18 years old attending the cardiology outpatient clinic of the Sainte-Justine University Hospital for murmur, chest pain, or palpitations. From 2002 until 2011, we collected normal echocardiographic data on left ventricular outflow tract and ascending aorta (AscAo) diameter. This clinical dataset included studies interpreted as being “normal” by the attending pediatric cardiologist for patients with unremarkable clinical examination, medical history, and ECG (except for a benign physiological murmur). Proximal aorta dimensions were measured using a standardized protocol and measurements were entered prospectively in the dataset. The study was approved by the institutional ethics review committee. For this study, the ethics review committee waived the need for informed consent for the interrogation of this clinical database.
Age, weight, height, and sex were also recorded at the time of the study. BSA was estimated using the formula proposed by Haycock et al. [22]. BMI was calculated as height (m)/weight (kg)2 and was normalized for age and sex according to standard values of the World Health Organization [10, 11]. Lean body weight (LBM) was estimated using the equations proposed by Foster et al. [17].
Echocardiographic Measurements
Proximal aorta dimensions were measured in the parasternal long axis according to the recommended guidelines [23]. Aortic valve (AoV) diameter was measured at the level of the valve insertion hinge point. Sinus of Valsalva (SoV) diameter was measured at the maximal diameter between the valve insertion and the sino-tubular junction. AscAo was measured at the level of the right pulmonary artery. All dimensions were taken in early-mid systole on the frame of their maximal diameter and were measured from inner edge to inner edge.
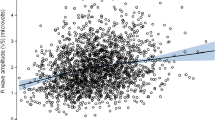
Influence of Body Mass Index
The influence of increasing BMI-for-age Z scores on proximal aorta dimension Z scores was tested by plotting the proximal aorta dimension Z scores against BMI-for-age Z scores and using linear regression to detect statistically significant slopes. Subjects were also categorized according to their BMI-for-age Z scores in order to measure variation of the mean proximal aorta Z scores according to BMI.
Normalization
Z scores for AoV and SoV diameters were first computed using two previously published equations. The equation proposed by Pettersen et al. was based on a third-order polynomial model with log-transformation of the echocardiographic dimension [28]. The sex-specific equations proposed by Gauthier et al. were based on a log–log model [20].
Proximal aorta diameter Z scores normalized for weight, height, or LBM were not available in the recent scientific literature [24]. Thus, we elected to compute our own set of bivariate Z scores. Our detailed approach to producing Z score equations is described in the online supplement. In brief, several bivariate prediction models [9, 24, 26, 30] were tested against four body size measurements: height, weight, BSA, and LBM. To account for heteroskedasticity, the standard deviation of the residual values was also modeled for body size [1], and Z scores were calculated according to the following equation:
With a view to exploring models that include both height and weight as independent predictors, a multivariable model was also built using stepwise inclusion. Independent variables were introduced one by one in the model in the following order: √height, √weight, height, weight, height2, and weight2. We elected to use polynomial regression up to the third degree because, we—as well as others [28]—have often observed that echocardiographic diameter measurements are best described using a polynomial regression of the third order. Variables were kept in the model if the Wald χ 2 statistic for that variable yielded a p value <0.05.
All the newly computed Z score equations were tested for residual association with the independent variable used for normalization, for residual heteroscedasticity, and for potential departure from the normal distribution. This approach is detailed in the online supplement.
In a preliminary analysis, sex was found to have a strong statistically significant influence on all Z scores models with mean Z score differences ranging from 0.25 to 0.36 between sexes with p values <0.0001. All Z scores were thus computed for males and females independently.
Bootstrap Validation
Because the multivariable model contained up to 4 terms, bootstrap cross-validation was used to evaluate the possibility of over-fitting. We created 1,000 samples of 560 male subjects randomly selected with replacement from the original database. The model was fitted on each new sample, and adjusted R 2 was calculated. The new parameter estimates from each of the new samples were also applied to the original database, and the adjusted R 2 was again calculated on the original dataset. Over-fitting is considered more likely when the mean difference between the adjusted R 2 from the new samples and the original sample increases [2].
Statistical Analysis
We used SAS for Windows version 9.3 for all analyses (SAS Institute Inc., Cary, NC, USA). PROC NLIN was used for non-linear regression and PROC GENMOD for linear regression. Mean Z scores were compared using Student’s t test. The t statistic was used to estimate p values for slopes. Departure from a normal distribution was evaluated by visual assessment (normal probability plot) and by using the Anderson–Darling test. A p value <0.05 was considered statistically significant.
Results
Study Sample
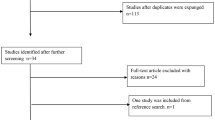
A total of 1,422 echocardiographic studies were available in our database. Of these studies, 8 were excluded because of missing anthropometric information, and 18 were identified as obvious outliers. The remaining 1,396 subjects constituted the study cohort. Measurements for AoV, SoV, and AscAo were available for 1,359, 1,337, and 1,275 subjects, respectively. Forty-six percent of subjects were females. Figure 1 shows the subjects’ distribution by age (panel A) and by BMI-for-age Z score (panel B). To determine Z score equations, only subjects with BMI-for-age within the 2nd and the 98th percentiles were included (1,257 subjects).
Newly Computed Z Score Equations (Bivariate)
AoV, SoV, and AscAo diameters had clear non-linear association with all body size measurements. There was also significant heteroskedasticity for all three measurements (data not shown). Z score equations derived from linear and allometric models had significant departure from the normal distribution and significant residual association with their independent variable (data not shown). Such models were not further explored. The gamma function model produced Z scores virtually identical to the polynomial model with a square root term (data not shown). The latter being less complex, the gamma function model was not further explored.
Z score equations derived from polynomial models including a square root term (y = ax + √bx + c and y = ax 2 + bx + √cx + d) yielded the best possible fit with all four body size measurements. Table 1 lists AoV Z score equations for all four body size variables. Z score equations for SvS and AscAo may be found in the online supplement. All equations given in Table 1 yielded good symmetry of the residual values around the mean, little residual association, and no significant departure from the normal distribution. AoV diameter-predicted mean and Z score boundaries for all four body size measurements are presented in Fig. 2. Results for SoV and AscAo were comparable (data not shown).
Scatter plot of aortic valve (AoV) diameter with Z score boundaries based on bivariate models against weight, height, body surface area, and lean body mass. Solid blue line predicted mean (Z = 0). Dashed blue lines Z = 1.0 and −1.0. Solid red lines Z = 2.0 and −2.0. Dashed red lines Z = 3.0 and −3.0
Influence of BMI
In a preliminary analysis, the association of BMI-for-age with proximal aorta Z score was different in pre-school children compared to that of older children. Hence, the study cohort was divided into two groups using 6 years of age as the cut-off. A preliminary analysis also indicated that, overall, SoV, and AscAo diameters yielded similar results to AoV diameter.
Table 2 lists the regression slopes and p values of AoV Z scores versus BMI-for-age according to the various models. Results are categorized for subjects ≤6 years old, >6 years old including obese, and >6 years old excluding obese. Figure 3 presents the box-plots of previously published AoV Z score equations [20, 28] according to BMI-for-age categories. For subjects aged >6 years, there was a strong statistically significant negative relationship between AoV Z scores from the previously published equations and BMI-for-age (i.e., subjects with higher BMI had lower AoV Z scores). This association was less pronounced for children ≤6 years old.
Similar results were observed for Z score equations from this study, and a statistically significant slope was identified between BMI-for age and Z scores normalized for weight, height, BSA, and LBM (Table 2; Fig. 4). The slope was negative for Z scores normalized on weight, LBM, and BSA, and positive for Z scores normalized on height. Obese subjects (BMI-for-age >2.0) had a significant influence on the magnitude of all slopes, except for the slope of Z scores normalized on height. However, the association of BMI with Z scores remained statistically significant even when obese subjects were excluded from the analysis (Table 2).
Multivariable Model
We assessed if a regression model in which weight and height are included as independent predictors of AoV diameter could reduce the association between Z scores and BMI. Three orders of the variable height (√height, height, and height2) contributed significantly to the model. Weight was also a significant predictor, but addition of second or third orders of weight did not add significantly to the model fit and were consequently not included in the final model. The final multivariable model equation is shown in Table 1. Aortic valve diameter Z scores computed with the multivariable model did not display any residual association with height, weight, BSA, or LBM. Figure 5 shows that AoV Z scores were evenly distributed around zero across the entire range of height, weight, BSA, and LBM. Figure 6 shows the distribution of Z scores closely approaching a normal distribution.
When the AoV Z score normalized using multivariable model was tested against BMI, there was a statistically significant negative association in subjects >6 years old, but not in younger subjects (Table 2). This association was, however, almost exclusively due to obese subjects with BMI-for-age Z scores >2.0 (Table 2; Fig. 7). There was no significant association between AoV Z scores and BMI, when obese subjects were excluded.
Bootstrap Cross-Validation
Bootstrap cross-validation was performed on the multivariable to detect possible over-fitting that could be present because as many as four terms were included in the regression model. The bootstrap cross-validation method yielded a R 2 mean difference between the original dataset and the resampled datasets of only 0.38 % indicating that over-fitting was unlikely.
Discussion
We have demonstrated that most attempts to normalize proximal aorta measurements using only one body size variable (bivariate models) resulted in significant residual association with BMI adjusted for age and sex. When weight and BSA were used to normalize proximal aorta diameters, higher BMI-for-age was systematically associated with lower mean proximal aorta Z scores. This was also true for LBM, although the effect was smaller. The opposite relationship was observed when diameters were normalized for height. Only a multivariable model in which weight and height were treated as independent predictors could attenuate this association.
The association of higher BMI-for-age Z scores with lower proximal aorta Z scores when normalized for weight or BSA suggests one of two possibilities. Either the dimension of the proximal aorta is actually smaller in subjects with higher BMI-for-age, or the normalization for BSA or weight with bivariate models has introduced a bias. Although the design of our study cannot refute the former explanation, it is unlikely to be the case from a physiological perspective.
Our preliminary analysis showed that weight was a strong predictor of proximal aorta diameter in young children. However, as children approached adolescence, height influenced aortic diameter more significantly, and the effect of weight became less important. This was observed during the construction of our stepwise multivariable model in which the independent contribution of weight as an explanatory variable diminished as height parameters were entered into the model.
The complex interaction of height and weight on cardiac dimension renders any normalization approach using weight or height alone quite imperfect. BSA has often been seen as a solution to this problem. However, measuring the true BSA of a patient is not practical. The available equations used to estimate BSA all “impose” a fixed relationship for weight and height when BSA is included in any bivariate regression. In a given individual, a higher BSA can be the result of increased weight, height, or both, all of which affect cardiac dimension differently. Normalization using BSA does not take into account the fact that the relative predictive effect of weight compared to height seems to diminish as children grow. This limitation of normalization using BSA is addressed by our multivariable model in which height and weight act as independent predictors.
For example, in two patients measuring 115 cm, a 5-kg difference would significantly increase the estimated BSA. This weight difference, applied to a BSA-based polynomial model, would result in a difference of 1.0 mm in mean predicted AoV diameters. This stands in contrast with our multivariable model in which the effect of such a weight increase on predicted AoV diameters is minimal (0.2 mm). For a given height, an increase in weight could be due to increases in muscle mass, fat mass, or both. The metabolic demands of muscle tissue and adipose tissue are very dynamic, but their overall influence on heart size is likely different [19]. An increase in weight could be mainly attributable to muscle mass in some subjects. In this situation, one would expect to see a larger proximal aorta diameter. That being said, in the majority adolescent individuals in our population, the increase in weight is more likely to be explained by an increase in adipose tissue. Our retrospective data did not allow for the determination of the proportion of fat vs. muscle mass in the subjects studied. Our results, however, support the fact that the weaker influence of weight on aorta dimension in older children may be due to an increase in tissues with lower metabolic demand, such as adipose tissues.
Regardless of the regression model used for normalization, a systematic bias was observed for obese subjects with BMI-for-age above the 98th percentile when weight was included in the model. When an echocardiographic dimension adjustment is considered for such patients, Z scores must be viewed with caution because of the distortion introduced by the important contribution of fat mass to such subjects’ weight. In our preliminary analyses, a weight correction subtracting weight in excess of the 85th BMI percentile yielded promising results, but numbers were too small for this method to be generalized.
The choice of the best independent variable to normalize heart size is a source of much debate. Two recent reviews discussing normalization in pediatric echocardiography have reported that methods of normalization and selection of independent variables were very heterogeneous and that statistical validity was not always properly assessed [5, 24]. We previously observed that, among the many publications pertaining to reference values in pediatric echocardiography, BSA was most often used to normalize cardiac dimensions, with some authors favoring weight in infants and height in adolescents [24]. Others have also used multivariable regressions as a way to normalize echocardiographic dimensions [27, 29].
Recently, Foster et al. reported that, when compared to LBM, BSA outperformed height as a scaling variable to adjust left ventricular mass for body size in children [18]. They too observed that significant residual association with BMI-for-age was present when left ventricular mass is adjusted for height or BSA and that this residual association may lead to an increase in the proportion of false positives and false negatives. They concluded that BSA, despite being an imperfect scaling factor, is preferable to height, and also suggested that LBM may be preferable when dealing with obese patients. They did not, however, test a multivariable model.
In our study, we showed that the estimation of LBM from the same team [17] introduced a residual association with BMI-for-age, although of lesser magnitude than BSA. This was to be expected since their equation for estimating LBM includes a BMI-for-age term and consequently offered better adjustment for BMI. Nonetheless, in our analysis, only the multivariable model yielded a Z score free of residual association with BMI-for-age in non-obese patients. Similar conclusions were drawn in adult studies in which left ventricular mass (measured by magnetic resonance imaging) had a better prognostic value when normalization was done using weight and height independently in a multivariable model compared to bivariate allometric models using height or BSA [3, 4].
In this study, we used parametric weighted regression to normalize echocardiographic measurement for body size. The LMS method, a robust non-parametric approach described by Cole and Green in the 1990s [7, 8], is increasingly being used for normalization for body size, including in echocardiography [16]. Although it has many advantages, its principal drawback is that it can only normalize for one body size measurement (bivariate) and thus cannot accommodate multivariable models.
Our study has some potential limitations. First, BMI is an imperfect estimation of the relationship between weight and height. Further studies using more direct measurements of body composition (e.g., skin fold, waist circumference) should be undertaken to clarify the role of adiposity on cardiac size. Second, our multivariable model equation included four terms (up to the third degree for height), which could lead to over-adjustment. We elected to use up to the third order of height mainly because of previous observations that great vessel diameters often adopt a third-order relationship with height or BSA in bivariate analyses [28]. Bootstrap cross-validation indicated that over-adjustment was unlikely. Third, our multivariable model is based on an empirical statistical approach and not on fluid dynamic principles. Regression models based on physiological principles, such as allometric and gamma-function models, were assessed in this study but most did not meet our criteria of a statistically valid Z score (the absence of residual association and normal distribution). Fourth, we chose to include children with BMI-for-age Z scores between 1.0 and 2.0 even though they are considered overweight according to published WHO standards. We elected to include these children in order to obtain realistic reference values that can be generalized to the population routinely seen in the echocardiography laboratory. Finally, this was a retrospective analysis of echocardiographic studies performed for a clinical indication. Our results should be confirmed on a “true” control population of children who have no indication for echocardiography.
Conclusion
In this study, we have identified a potential bias related to BMI in proximal aorta Z scores normalized on only one body size measurement. This bias is reduced when a multivariable regression is used. This should be viewed as a proof of concept that bivariate models may be insufficient as a normalization tool in pediatric echocardiography. We thus advocate that multivariable models should be explored for proximal aorta dimension. This may also be true for other echocardiographic measurements, but further studies should be initiated to clarify the effect of measurable adiposity versus muscle mass on pediatric echocardiographic cardiac dimensions.
References
Altman DG (1993) Construction of age-related reference centiles using absolute residuals. Stat Med 12(10):917–924
Babu GJ (2011) Resampling methods for model fitting and model selection. J Biopharm Stat 21(6):1177–1186
Bluemke DA, Kronmal RA, Lima JA, Liu K, Olson J, Burke GL, Folsom AR (2008) The relationship of left ventricular mass and geometry to incident cardiovascular events: the MESA (multi-ethnic study of atherosclerosis) study. J Am Coll Cardiol 52(25):2148–2155
Brumback LC, Kronmal R, Heckbert SR, Ni H, Hundley WG, Lima JA, Bluemke DA (2010) Body size adjustments for left ventricular mass by cardiovascular magnetic resonance and their impact on left ventricular hypertrophy classification. Int J Cardiovasc Imaging 26(4):459–468
Cantinotti M, Scalese M, Molinaro S, Murzi B, Passino C (2012) Limitations of current echocardiographic nomograms for left ventricular, valvular and arterial dimensions in children: a critical review. J Am Soc Echocardiogr 25(2):142–152
Colan SD (2013) The why and how of Z scores. J Am Soc Echocardiogr 26(1):38–40
Cole TJ (1990) The LMS method for constructing normalized growth standards. Eur J Clin Nutr 44(1):45–60
Cole TJ, Green PJ (1992) Smoothing reference centile curves: the LMS method and penalized likelihood. Stat Med 11(10):1305–1319
Dallaire F, Dahdah N (2011) New equations and a critical appraisal of coronary artery Z scores in healthy children. J Am Soc Echocardiogr 24(1):60–74
de Onis M, Garza C, Victora CG, Bhan MK, Norum KR (2004) The WHO multicentre growth reference study (MGRS): rationale, planning, and implementation. Food Nutr Bull 25(Suppl. 1):S3–S84
de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J (2007) Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 85(9):660–667
de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, Alderman MH (1992) Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol 20(5):1251–1260
de Simone G, Devereux RB, Maggioni AP, Gorini M, de Divitiis O, Verdecchia P (2005) Different normalizations for body size and population attributable risk of left ventricular hypertrophy: the MAVI study. Am J Hypertens 18(10):1288–1293
Du Bois D, Du Bois EF (1916) Clinical Calorimetry: Tenth Paper - A Formula to Estimate the Approximate Surface Area if Height and Weight be Known. Arch Intern Med 17(6–2):863–871
Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 5(5): 303–311; discussion 312–303
Foster BJ, Mackie AS, Mitsnefes M, Ali H, Mamber S, Colan SD (2008) A novel method of expressing left ventricular mass relative to body size in children. Circulation 117(21):2769–2775
Foster BJ, Platt RW, Zemel BS (2012) Development and validation of a predictive equation for lean body mass in children and adolescents. Ann Hum Biol 39(3):171–182
Foster BJ, Gao T, Mackie AS, Zemel BS, Ali H, Platt RW, Colan SD (2012) Limitations of expressing left ventricular mass relative to height and to body surface area in children. J Am Soc Echocardiogr 26(4):410–418
Frayn KN, Karpe F, Fielding BA, Macdonald IA, Coppack SW (2003) Integrative physiology of human adipose tissue. Int J Obes Relat Metab Disord 27(8):875–888
Gautier M, Detaint D, Fermanian C, Aegerter P, Delorme G, Arnoult F, Milleron O, Raoux F, Stheneur C, Boileau C, Vahanian A, Jondeau G (2010) Nomograms for aortic root diameters in children using two-dimensional echocardiography. Am J Cardiol 105(6):888–894
Grollman A (1929) Physiologic variations in the cardiac output in man. Am J Physiol 90:210–217
Haycock GB, Schwartz GJ, Wisotsky DH (1978) Geometric method for measuring body surface area: a height-weight formula validated in infants, children, and adults. J Pediatr 93(1):62–66
Lopez L, Colan SD, Frommelt PC, Ensing GJ, Kendall K, Younoszai AK, Lai WW, Geva T (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23(5):465–495 quiz 576-467
Mawad W, Drolet C, Dahdah N, Dallaire F (2013) A review and critique of the statistical methods used to generate reference values in pediatric echocardiography. J Am Soc Echocardiogr 26(1):29–37
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317(17):1098
Nevill AM, Bate S, Holder RL (2005) Modeling physiological and anthropometric variables known to vary with body size and other confounding variables. Am J Phys Anthropol Suppl 41:141–153
Overbeek LI, Kapusta L, Peer PG, de Korte CL, Thijssen JM, Daniels O (2006) New reference values for echocardiographic dimensions of healthy Dutch children. Eur J Echocardiogr 7(2):113–121
Pettersen MD, Du W, Skeens ME, Humes RA (2008) Regression equations for calculation of Z scores of cardiac structures in a large cohort of healthy infants, children, and adolescents: an echocardiographic study. J Am Soc Echocardiogr 21(8):922–934
Roman MJ, Devereux RB, Kramer-Fox R, O’Loughlin J (1989) Two-dimensional echocardiographic aortic root dimensions in normal children and adults. Am J Cardiol 64(8):507–512
Sluysmans T, Colan SD (2005) Theoretical and empirical derivation of cardiovascular allometric relationships in children. J Appl Physiol 99(2):445–457
Acknowledgments
FD is a member of the Fonds de Recherche Santé Québec-funded Centre de Recherche du Centre hospitalier universitaire de Sherbrooke (CRCHUS).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Dallaire, F., Bigras, JL., Prsa, M. et al. Bias Related to Body Mass Index in Pediatric Echocardiographic Z Scores. Pediatr Cardiol 36, 667–676 (2015). https://doi.org/10.1007/s00246-014-1063-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-014-1063-7