Abstract
Proper assessment of fluid responsiveness using accurate predictors is crucial to guide fluid therapy and avoid the serious adverse effects of fluid overload. The main objective of this study was to investigate the accuracy of respiratory variations in inferior vena cava diameter (∆IVC) to predict fluid responsiveness in mechanically ventilated children. This prospective single-center study included 32 children (median age and weight of 17 months and 10 kg, respectively) who received a fluid infusion of 10 ml kg–1 of crystalloid solutions over 10 min. ∆IVC and respiratory variation in aortic blood flow peak velocity (∆Vpeak) were determined over one controlled respiratory cycle before and after fluid loading. Thirteen (41%) participants were fluid-responders. ∆IVC, ∆Vpeak, stroke volume index, and cardiac index were found to be predictors of fluid responsiveness. However, the area under the ROC curve of ∆IVC was smaller when compared to ∆Vpeak (0.709 vs. 0.935, p < 0.012). The best cut-off values were 7.7% for ∆IVC (sensitivity, 69.2%; specificity 78.9%, positive predictive value, 69.2%; and negative predictive value, 78.9%) and 18.2% for ∆Vpeak (sensitivity, 84.6%; specificity, 89.5%; positive predictive value, 84.6%; negative predictive value, 89.5%). Changes in stroke volume were positively correlated with ∆IVC (ρ = 0.566, p < 0.001) and ∆Vpeak (ρ = 0.603, p < 0.001). A significant correlation was also found between changes in MAP and ∆Vpeak (ρ = 0.382; p = 0.031), but the same was not observed with ∆IVC (ρ = 0.011; p = 0.951). In conclusion, ∆IVC was found to have a moderate accuracy in predicting fluid responsiveness in mechanically ventilated children and is an inferior predictor when compared to ∆Vpeak.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Fluid resuscitation is the mainstay of therapy in children with hypovolemic or septic shock. However, fluid bolus administration is not without risk or harm. Misguided fluid therapy can lead to fluid overload, which has been independently associated with poor in-hospital outcomes, such as impaired renal function, acute respiratory distress syndrome, prolonged mechanical ventilation, longer PICU stay, and increased mortality [1]. The main objective of fluid loading is to increase cardiac output. Unfortunately, only about 50% of children who receive a fluid loading have a significant increase in their stroke volume (SV) [2]. This low rate highlights the limited ability of attending physicians to predict the hemodynamic effects of fluid loading and the need for more accurate methods for hemodynamic assessment. Commonly used static variables, such as heart rate, blood pressure, or central venous pressure, have been shown to be poor predictors of fluid responsiveness in children [2]. Although dynamic variables based on heart–lung interactions are more accurate predictors than static variables, they are not widely available. In addition, the use of dynamic variables is limited in children, as the most studied methods require arterial lines and/or central venous catheterization [2,3,4].
Point-of-care ultrasound (POCUS) has been proposed as a valuable method for hemodynamic assessment in critical care patients. The respiratory variation of inferior vena cava diameters (ΔIVC) is among the most popular POCUS techniques used to predict fluid responsiveness. The IVC is a thin-walled vessel with very high compliance which diameter is affected by central venous pressure and cyclic changes variable for fluid responsiveness prediction. High values of ΔIVC suggest that the cardiovascular system is operating in the ascending portion of the Frank-Starling curve and will benefit from fluid loading [5, 6]. Conversely, patients whose IVC has low respiratory variability are unlikely to increase their SV with fluid infusion.
The first studies investigating the ΔIVC were published in 2004 and since then there has been an intense debate about the reliability of its measurements [5,6,7]. Although initial data showed good accuracy, a recent meta-analysis found extremely discordant results and concluded that ΔIVC does not seem to be an accurate method [7]. It was also pointed out that few studies have evaluated this technique in pediatric populations. Due to their reduced anatomic dimensions, accurately measuring IVC diameters can be challenging in children. Furthermore, we demonstrated in our previous study that IVC respiratory displacements can substantially impact measurements performed by M-mode ultrasound [8]. Therefore, the purpose of the present study was to investigate whether ΔIVC obtained by two-dimensional ultrasound (B-mode) can accurately predict fluid responsiveness in children under invasive mechanical ventilation.
Methods
Study Design, Subjects, and Setting
This prospective cohort study was conducted in the PICU of the Clinics Hospital of the State University of Campinas (UNICAMP), Sao Paulo, Brazil, between May and October 2021. The study was approved by the local institutional review board (UNICAMP's Research and Ethics Committee, approval #12894719.8.0000.5404), and written informed consent was obtained from the participants' legal guardians.
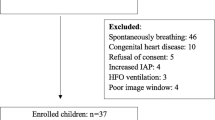
Children under invasive mechanical ventilation who required fluid loading at discretion of the attending physician were consecutively assessed for eligibility. The decision to give fluid was taken based on signs of inadequate tissue perfusion such as tachycardia, delayed capillary refilling, hypotension, oliguria, or hemodynamic instability despite vasoactive agents. Patients were included if they met the following criteria: (1) tidal volume of 8–10 ml kg–1; (2) positive end-expiratory pressure of 5–6 cmH2O; (3) absence of spontaneous breathing; (4) sinus rhythm. Exclusion criteria were as follows: (1) congenital heart diseases; (2) left ventricular systolic dysfunction (ejection fraction < 50%); (3) skin lesions or bandages at the sites of ultrasound or echocardiography exams; (4) poor echocardiographic windows; (5) operator or ultrasound machine unavailability.
Study Protocol
Participants received a fluid infusion of 10 ml kg–1of crystalloid solutions (normal saline or Ringer’s lactate solution) over 10 min. Data collection was performed before and immediately after fluid loading, and included: (1) heart rate, (2) blood pressure, (3) SV, (4) respiratory variation in aortic blood flow peak velocity (∆Vpeak), and (5) ΔIVC. Infusions of sedatives, analgesics and vasoactive drugs remained unchanged throughout the study period. After fluid infusion, participants were considered fluid responsive when their SV increased by more than 15% from baseline and were classified as “responders”, otherwise they were classified as “non-responders”. Likewise, increases in mean arterial pressure (MAP) greater than or equal to 10% were considered significant [9, 10].
Echocardiography Measurements
Transthoracic echocardiography (TTE) was performed using an ultrasound machine (Vivid Q; GE Healthcare, Tirat Carmel, Israel) equipped with a phased array transducer (3.5–8 MHz). Although both exams were performed at the same time, the calculations of ΔIVC, ΔVpeak, and SV were performed later. Thus, the operator was unaware of these variables during the data collection period. All echocardiographic examinations were performed by an experienced pediatric ultrasound instructor from the Brazilian Society of Intensive Care, with 7 years of experience in pediatric point-of-care ultrasound.
IVC diameters were measured in the longitudinal plane using B-mode, 1 cm distal to the hepatic vein-IVC confluence, during both inspiration and expiration. The decision to use B-mode instead of M-mode was made to avoid the influence of IVC craniocaudal respiratory displacements on the measurements [8]. Thus, the IVC diameters were measured at the same point along its length during the respiratory cycle. ΔIVC was calculated as follows: \(\Delta IVC\, = \,\frac{{\frac{{\left( {Diameter \,m\acute{a}x - Diameter \,min} \right)}}{{\left( {Diameter\, m\acute{a}x + Diameter \,min} \right)}}}}{2}\, \times \,100\).
SV was determined by measuring the aortic diameter (Da) and the aortic velocity–time integral (VTI). The Da was measured at the level of the aortic annulus by the parasternal long-axis view, while the VTI was measured by the apical five-chamber view using pulsed wave Doppler, with the sample volume positioned at the level of the left ventricular outflow tract. The highest and the lowest VTI obtained during a single respiratory cycle were determined through automatically traced envelopes, and the mean value was registered. The VTI was measured in triplicate and the mean value was considered for SV calculation. Both diameter and VTI were determined in centimeters. Finally, the SV was calculated using the following standard formula: \(SV{ }\left( {ml} \right) = { }\left( {\pi \, \times Da^{2} /4} \right)\, \times \,VTI\).
Maximal and minimal values of aortic blood flow peak velocities were determined beat-to-beat over a single respiratory cycle. ∆Vpeak was calculated as follows: \(\Delta Vpeak\, = \,\frac{{\frac{{\left( {Vpeak~m\acute{a}x - Vpeak~min} \right)}}{{\left( {Vpeak~m\acute{a}x + Vpeak~min} \right)}}}}{2}\, \times \,100.\) The average of three ∆Vpeak measurements was considered for analysis purposes.
Statistical Analysis
The normality of the data distribution was assessed using the Kolmogorov–Smirnov and Shapiro–Wilk tests. Continuous variables were expressed as medians and interquartile ranges (IQR), while categorical variables were expressed as absolute numbers (%). After fluid loading, participants were divided into two groups: responders and non-responders. The groups were compared using the Mann–Whitney test (continuous variables) and the chi-square or Fisher's exact test (categorical variables). Variables collected before and after fluid loading were compared using Wilcoxon rank-sum test. Receiver Operating Characteristic (ROC) curves were constructed to assess the accuracy of predictors and their areas under the curve were compared using the non-parametric technique proposed by DeLong et al. [11]. The optimal cut-off points were defined according to the optimal Youden's J statistic using univariable analysis. Spearman’s correlation coefficient (ρ) was used to estimate and test the relationship between continuous variables. p-values < 0.05 were considered significant.
Assuming a fluid responsiveness rate of 33%, we determined that 30 measurements would be needed to detect a difference of 0.30 between the area under the ROC curve (AUROC) of ∆Vpeak and the null hypothesis (AUROC = 0.5; i.e., no discriminating power), with an 80% power and type I error of 5%. Statistical analysis and sample size calculation were performed using MedCalc Statistical Software version 19.8 (MedCalc Software bvba, Ostend, Belgium).
Results
Thirty-two patients were enrolled and included in the final analysis. Median age and weight were 17 months (5.5–61) and 10 kg (5.4–19), respectively. Demographic characteristics of participants are presented in Table 1.
Thirteen subjects (41%) were responders to fluid loading. At baseline, responders and non-responders were similar in age, blood pressure, heart rate, vasoactive drugs use, and mechanical ventilation settings. However, the "responder" group had higher weight (13.5 kg vs 9.0 kg, p = 0.048), higher ΔVpeak (22.2% vs 7.3%, p = 0.001), higher ΔIVC (9.0% vs 2.4%, p = 0.046), lower Ci (2.27 L min−1 m−2 vs 3.47 L min−1 m−2, p = 0.009), and lower SVi (15.82 mL m−2 vs 22.87 mL m−2, p = 0.003).
The variables ΔIVC, ΔVpeak, SVi and Ci were predictors of fluid responsiveness (See Fig. 1). However, ΔVpeak was found to be more accurate than ΔIVC in the ROC curve analysis (AUROC of 0.935 vs 0.709, respectively, p = 0.012). No other significant differences were observed in the pairwise analysis of the AUROC of the predictors. The best cut-off value of ∆IVC found was 7.7%, which had a sensitivity of 69.2%, specificity of 78.9%, positive predictive value (PPV) of 69.2% and negative predictive value (NPV) of 78.9%. A ∆Vpeak of > 18.2% was able to predict fluid responsiveness with a sensitivity of 84.6%, specificity of 89.5%, PPV of 84.6%, and NPV of 89.5%. The complete analysis of the ROC curves is presented in Table 2.
Areas under the ROC curves of the evaluated predictors of fluid responsiveness. ΔVpeak was found to be more accurate than ΔIVC in the ROC curve analysis (AUROC of 0.935 vs 0.709, respectively, p = 0.012). No other significant differences were observed in the pairwise analysis of the AUROC of the predictors
Fluid loading significantly changed heart rate and MAP in both groups. However, diastolic blood pressure, SVi, Ci, ΔVpeak were changed only in the “responder” group, while systolic blood pressure changed only in the “non-responder” group. ΔIVC did not change significantly in either group. A 10% increase in MAP was observed in 61% (8/13) of participants in the "responder" group as well as in 37% (7/19) of participants in the "non-responder" group (See Fig. 2). There was no association between the proportion of participants who had an increase in MAP (61%) and those who were fluid responders (41%) (p = 0.233), and no significant correlation was found between changes in MAP and SVi (ρ = 0.191, p = 0.294). Hemodynamic variables before and after fluid loading in both groups are shown in Table 3.
SVi changes were positively correlated with ∆IVC (ρ = 0.566, p < 0.001) and ∆Vpeak (ρ = 0.603, p < 0.001). A significant positive linear correlation was also found between changes in MAP and ∆Vpeak (ρ = 0.382; p = 0.031), but the same was not observed with ∆IVC (ρ = 0.011; p = 0.951).
Discussion
In the present study, the ∆IVC presented an acceptable accuracy for predicting fluid responsiveness in mechanically ventilated children. However, its accuracy was significantly lower than ∆Vpeak. Also, Ci and SVi had higher AUROC values than ∆IVC, but no statistical difference was observed. The best ∆IVC cutoff value found was 7.7%, which has a sensitivity of 69.2% and a specificity of 78.9%. This threshold is much lower than previously found in similar studies. Some methodological particularities may be responsible for the discrepancies between the results herein reported and those previously published [12,13,14,15,16,17,18,19,20,21].
The main differentiating feature of our study is the method used to determine the IVC diameters. While the other pediatric studies used M-mode, we determined the IVC diameters using two-dimensional ultrasound. This approach was chosen to mitigate the impact of IVC respiratory displacements on diameter measurements. Only two-dimensional ultrasonography allows the maximum and minimum IVC diameters to be measured at the same distance from the hepatic vein. When using M-mode, the IVC diameters are registered at different locations along its length, since the ultrasound beam is static and the vessel has a significant respiratory displacement in the craniocaudal direction [8]. Thus, the M-mode can register structural changes in IVC diameters rather than only the respiratory variability [22]. As a matter of fact, there is an interesting debate about which is the best method and location for measuring IVC diameter in adults, and this discussion also needs to take place in pediatrics [23,24,25].
In our previous study, we observed a large discrepancy between the ∆IVC values obtained by M-mode and two-dimensional ultrasound when evaluating the same respiratory cycle [8]. The median values of the ∆IVC obtained by two-dimensional ultrasound were about half of those obtained by M-mode (11.45% vs 21.82%, p < 0.001) [8]. Therefore, it is not surprising that we found a cut-off point much lower than those previously published. While the best IVC cutoff value in our study was only 7.7%, other authors reported values ranging from 12.3% to 28.5% [12,13,14,15,16,17,18,19,20,21]. The IVC respiratory displacements may be a major contributor to the disagreement between both methods for ∆IVC measurements. Accurately measuring IVC diameters can be challenging in children, especially younger ones, so future studies should perform measurements using two-dimensional ultrasonography to reduce inaccuracies.
The use of ∆IVC as a predictor of fluid responsiveness gained popularity in critical care medicine after early studies demonstrated its high accuracy in adults [5, 6]. However, the same exciting results were not found in similar later studies. A meta-analysis including adults and children found a pooled sensitivity and specificity of 63% and 73%, respectively (pooled AUROC of 0.79) [26]. In addition, the test performance appears to be better when patients are ventilated with a tidal volume ≥ 8 ml kg–1 and positive end-expiratory pressure ≤ 5 cmH2O. This aspect is especially important for mechanically ventilated patients in whom lung protective strategies are applied. Thus, a transient increase in tidal volume when performing the test may increase its accuracy, which has been called "tidal volume challenge". In children the accuracy of ∆IVC varies widely across studies, with sensitivity ranging from 47 to 100% and specificity ranging from 33 to 100% [12,13,14,15,16,17,18,19,20,21, 27].
In our study, ∆Vpeak was shown to be a more reliable predictor of fluid responsiveness when compared to ∆IVC, with sensitivity and specificity of 84.6% and 89.5%, respectively. Similar results were found by other authors [12, 13, 27]. A recent meta-analysis of pediatric studies evaluating ∆Vpeak found a pooled sensitivity of 84% and pooled specificity of 82% [27]. However, despite its good accuracy, the use of ∆Vpeak is often limited in intensive care patients due to suboptimal acoustic windows caused by mechanical ventilation, dressings, interfering incisions, and positioning difficulties [28]. In addition, obtaining ∆Vpeak can be challenging for inexperienced operators as it requires specific skills and training. Even so, its use should be encouraged due to the good results presented in several studies.
Blood pressure is perhaps the most determining hemodynamic variable in making decisions about fluid infusions, as well as in assessing the response to such an intervention. In clinical practice, patients are often considered fluid responders when they experience increased blood pressure after fluid loading [29]. However, in our study the percentage of patients who increased their MAP after volume expansion was similar between fluid responders and non-responders. The absence of an association between fluid bolus-induced changes in MAP and Ci (or SV) has also been reported in other studies involving children [9, 10, 30]. Furthermore, the adverse effects of volume expansion are not limited to fluid overload. Ranjit et al. found that some children experienced hemodynamic deterioration soon after the end of fluid infusion, with reduced MAP, reduced pulse pressure, and increased use of vasoactive drugs [9, 10]. Although blood pressure is an important hemodynamic variable for organ perfusion, it should not be used as a surrogate of SV when assessing response to fluid loading.
The present study has some limitations that need to be pointed out. First, participants were not receiving neuromuscular blocking agents. However, they were under sedation and the absence of spontaneous breathing was verified clinically and on ventilator monitoring. Second, fluid responsiveness was not assessed using gold standard techniques such as thermodilution or the direct Fick method. Nevertheless, the use of TTE for Ci measurements has been widely studied in children, proving to be accurate, precise and reproducible [31]. Third, both fluid responsiveness and ∆Vpeak were determined using the same echocardiographic method (TTE). With this, the index test and the standard reference criteria were not independent, which may have led to an overestimation of diagnostic accuracy. Fourth, obtaining ∆Vpeak by TTE is subject to technical artifacts caused by chest wall movements during breathing. This limitation can be overcome by transesophageal echocardiography; however, this method is not available in most PICUs. Fifth, our study included a specific population of children under invasive mechanical ventilation. Therefore, the results reported here should not be extrapolated to other populations, such as spontaneously breathing children.
Conclusion
The ∆IVC has limited accuracy to identify children who will increase their SV after fluid loading. The use of ∆Vpeak should be preferred over ∆IVC whenever possible, as it seems to be a better predictor of fluid responsiveness in mechanically ventilated children.
Data Availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Code Availability
Not applicable.
Abbreviations
- ΔIVC:
-
Respiratory variation of inferior vena cava diameters
- ∆Vpeak:
-
Respiratory variation in aortic blood flow peak velocity
- AUROC:
-
Area under the ROC curve
- Ci:
-
Cardiac index
- Da:
-
Aortic diameter
- IQR:
-
Interquartile range
- IVC:
-
Inferior vena cava
- MAP:
-
Mean arterial pressure
- NPV:
-
Negative predictive value
- PICU:
-
Pediatric intensive care unit
- POCUS:
-
Point-of-care ultrasound
- PPV:
-
Positive predictive value
- ROC curve:
-
Receiver operating characteristic curve
- SV:
-
Stroke volume
- SVi:
-
Stroke volume index
- TTE:
-
Transthoracic echocardiography
- VTI:
-
Velocity–time integral
References
Alobaidi R, Morgan C, Basu RK et al (2018) Association between fluid balance and outcomes in critically ill children: a systematic review and meta-analysis. JAMA Pediatr 172:257–268. https://doi.org/10.1001/jamapediatrics.2017.4540
Gan H, Cannesson M, Chandler JR, Ansermino JM (2013) Predicting fluid responsiveness in children: a systematic review. Anesth Analg 117:1380–1392. https://doi.org/10.1213/ANE.0b013e3182a9557e
Luo D, Liu F, Dai W et al (2021) Diagnostic accuracy of stroke volume variation for predicting fluid responsiveness in children undergoing cardiac surgery: a systematic review and meta-analysis. Pediatr Anesth 31:755–762. https://doi.org/10.1111/PAN.14195
Yi L, Liu Z, Qiao L et al (2017) Does stroke volume variation predict fluid responsiveness in children: a systematic review and meta-analysis. PLoS One 12:e0177590. https://doi.org/10.1371/JOURNAL.PONE.0177590
Feissel M, Michard F, Faller J-P, Teboul J-L (2004) The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med 30:1834–1837. https://doi.org/10.1007/s00134-004-2233-5
Barbier C, Loubieres Y, Schmit C et al (2004) Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med 30:1740–1746. https://doi.org/10.1007/s00134-004-2259-8
Orso D, Paoli I, Piani T et al (2018) Accuracy of ultrasonographic measurements of inferior vena cava to determine fluid responsiveness: a systematic review and meta-analysis. J Intensive Care Med. https://doi.org/10.1177/0885066617752308
de Souza TH, Giatti MP, Nogueira RJN et al (2020) Inferior vena cava ultrasound in children: comparing two common assessment methods. Pediatr Crit Care Med 21:E186–E191. https://doi.org/10.1097/PCC.0000000000002240
Ranjit S, Natraj R, Kissoon N et al (2020) Variability in the physiologic response to fluid bolus in pediatric patients following cardiac surgery. Crit Care Med 48:E1062–E1070. https://doi.org/10.1097/CCM.0000000000004621
Ranjit S, Natraj R, Kissoon N et al (2021) Variability in the hemodynamic response to fluid bolus in pediatric septic shock. Pediatr Crit Care Med 22:E448–E458. https://doi.org/10.1097/PCC.0000000000002714
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Choi YA, Kwon H, Lee JH et al (2018) Comparison of sonographic inferior vena cava and aorta indexes during fluid administered in children. Am J Emerg Med 36:1529–1533. https://doi.org/10.1016/J.AJEM.2018.01.010
Byon H-J, Lim C-W, Lee J-H et al (2013) Prediction of fluid responsiveness in mechanically ventilated children undergoing neurosurgery. Br J Anaesth 110:586–591. https://doi.org/10.1093/bja/aes467
El-Halimi K, Negadi M, Bouguetof H et al (2015) Respiratory variations in aortic blood flow velocity and inferior vena cava diameter as predictors of fluid responsiveness in mechanically ventilated children using transthoracic echocardiography in a pediatric PICU. Crit Care 19:S62–S63. https://doi.org/10.1186/CC14261
Weber T, Wagner T, Neumann K, Deusch E (2015) Low predictability of three different noninvasive methods to determine fluid responsiveness in critically ill children. Pediatr Crit Care Med 16:e89-94. https://doi.org/10.1097/PCC.0000000000000364
Achar SK, Sagar MS, Shetty R et al (2016) Respiratory variation in aortic flow peak velocity and inferior vena cava distensibility as indices of fluid responsiveness in anaesthetised and mechanically ventilated children. Indian J Anaesth 60:121–126. https://doi.org/10.4103/0019-5049.176285
Long E, Duke T, Oakley E et al (2018) Does respiratory variation of inferior vena cava diameter predict fluid responsiveness in spontaneously ventilating children with sepsis. Emerg Med Australas 30:556–563. https://doi.org/10.1111/1742-6723.12948
El-Nawawy AA, Omar OM, Hassouna HM (2021) Role of inferior vena cava parameters as predictors of fluid responsiveness in pediatric septic shock: a prospective study. J Child Sci 11:E49–E54. https://doi.org/10.1055/S-0041-1724034
Shostak E, Shochat T, Manor O et al (2021) Fluid responsiveness predictability in immediate postoperative pediatric cardiac surgery. Is the old slandered central venous pressure back again? Shock 56:927–932. https://doi.org/10.1097/SHK.0000000000001786
Singh A, Kumar B, Puri GD et al (2022) Utility of transfontanelle ultrasound in predicting the fluid responsiveness in children after repair of congenital heart diseases: a prospective observational study. J Cardiothorac Vasc Anesth. https://doi.org/10.1053/J.JVCA.2022.01.035
Xiong Z, Zhang G, Zhou Q et al (2022) Predictive value of the respiratory variation in inferior vena cava diameter for ventilated children with septic shock. Front Pediatr. https://doi.org/10.3389/FPED.2022.895651
Blehar DJ, Resop D, Chin B et al (2012) Inferior vena cava displacement during respirophasic ultrasound imaging. Crit Ultrasound J 4:18. https://doi.org/10.1186/2036-7902-4-18
Wallace DJ, Allison M, Stone MB (2010) Inferior vena cava percentage collapse during respiration is affected by the sampling location: an ultrasound study in healthy volunteers. Acad Emerg Med 17:96–99. https://doi.org/10.1111/J.1553-2712.2009.00627.X
Finnerty NM, Panchal AR, Boulger C et al (2017) Inferior vena cava measurement with ultrasound: what is the best view and best mode? West J Emerg Med 18:496. https://doi.org/10.5811/WESTJEM.2016.12.32489
Yamanoʇlu NGÇ, Yamanoʇlu A, Parlak I et al (2015) The role of inferior vena cava diameter in volume status monitoring; the best sonographic measurement method? Am J Emerg Med 33:433–438. https://doi.org/10.1016/J.AJEM.2014.12.014
Long E, Oakley E, Duke T, Babl FE (2017) Does respiratory variation in inferior vena cava diameter predict fluid responsiveness: a systematic review and meta-analysis. Shock 47:550–559. https://doi.org/10.1097/SHK.0000000000000801
Carioca FL, de Souza FM, de Souza TB et al (2022) Point-of-care ultrasonography to predict fluid responsiveness in children: A systematic review and meta-analysis. Pediatr Anaesth 00:1–14. https://doi.org/10.1111/PAN.14574
Ibarra-Estrada M, López-Pulgarín JA, Mijangos-Méndez JC et al (2015) Respiratory variation in carotid peak systolic velocity predicts volume responsiveness in mechanically ventilated patients with septic shock: a prospective cohort study. Crit Ultrasound J 7:1–9. https://doi.org/10.1186/S13089-015-0029-1
Pierrakos C, Velissaris D, Scolletta S et al (2012) Can changes in arterial pressure be used to detect changes in cardiac index during fluid challenge in patients with septic shock? Intensive Care Med 38:422–428. https://doi.org/10.1007/S00134-011-2457-0
de Souza TB, Rubio AJ, de Siqueira FI et al (2022) Carotid doppler ultrasonography as a method to predict fluid responsiveness in mechanically ventilated children. Pediatr Anesth. https://doi.org/10.1111/PAN.14513
Chew MS, Poelaert J (2003) Accuracy and repeatability of pediatric cardiac output measurement using doppler: 20-year review of the literature. Intensive Care Med 29:1889–1894. https://doi.org/10.1007/s00134-003-1967-9
Acknowledgements
Thanks to Carolina Grotta Ramos Telio for her review of the article. We also thank the nursing, technical staff, and the pediatric intensive care residents.
Funding
No external funding for this manuscript.
Author information
Authors and Affiliations
Contributions
NC and LdL: responsible for data collection, drafting and critical revision of the manuscript. IF, RN, and MB: responsible for critical revision of the manuscript for important intellectual content. TdS: responsible for the study concept and design, data collection, analysis and interpretation of data.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this study to disclose.
Ethics Approval
The study was approved by the local institutional review board (UNICAMP’s Research and Ethics Committee, approval number 12894719.8.0000.5404).
Informed Consent
Written informed consent was obtained from the participants’ legal guardian.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Campos, N.B., de Lima, L.B., Ferraz, I.d. et al. Accuracy of Respiratory Variation in Inferior Vena Cava Diameter to Predict Fluid Responsiveness in Children Under Mechanical Ventilation. Pediatr Cardiol 45, 1326–1333 (2024). https://doi.org/10.1007/s00246-023-03115-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-023-03115-y