Abstract
Ho: YAG laser lithotripsy is widely used for urinary stone treatment, but concerns persist regarding its thermal effects on renal tissues. This study aimed to monitor intrarenal temperature changes during kidney stone treatment using retrograde intrarenal surgery with Ho: YAG laser. Fifteen patients were enrolled. Various laser power settings (0.8 J/10 Hz, 1.2 J/12 Hz) and irrigation modes (10 cc/min, 15 cc/min, 20 cc/min, gravity irrigation, and manual pump irrigation) were used. A sterile thermal probe was attached to a flexible ureterorenoscope and delivered into the calyceal system via the ureteral access sheath. Temperature changes were recorded with a T-type thermal probe with ± 0.1 °C accuracy. Laser power significantly influenced mean temperature, with a 4.981 °C difference between 14 W and 8 W laser power (p < 0.001). The mean temperature was 2.075 °C higher with gravity irrigation and 2.828 °C lower with manual pump irrigation (p = 0.038 and p = 0.005, respectively). Body mass index, laser power, irrigation model, and operator duty cycle explained 49.5% of mean temperature variability (Adj. R2 = 0.495). Laser power and operator duty cycle positively impacted mean temperature, while body mass index and specific irrigation models affected it negatively. Laser power and irrigation rate are critical for intrarenal temperature during Ho: YAG laser lithotripsy. Optimal settings and irrigation strategies are vital for minimizing thermal injury risk. This study underscores the need for ongoing research to understand and mitigate thermal effects during laser lithotripsy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retrograde intrarenal surgery (RIRS) is a minimally invasive procedure used to treat urinary stones located within the kidney and upper urinary tract and has become increasingly popular as a first-line treatment for many patients [1]. Its success in achieving high stone clearance rates with minimal morbidity has contributed to its growing popularity and widespread adoption in clinical practice. Since its introduction in the 1990s, the Holmium: Yttrium-Aluminum-Garnet (Ho: YAG) laser has emerged as a standard tool in urological practice for intracorporeal treatment of urinary stone disease, displaying efficacy in fragmenting stones of various compositions [2].
With technological advancements, high-power laser systems have emerged as alternatives to traditional low-power laser systems in endourology. High-power Ho: YAG laser and Thulium Fiber Laser (TFL) systems are particularly noteworthy due to their high-frequency settings, which enable effective stone dusting and result in less retropulsion, making them ideal alternatives [3, 4]. The main concern regarding using these high-power laser systems is the increased risk of thermal tissue damage due to their ability to deliver higher energy transfer than traditional low-power laser settings [5]. TFLs offer advantages over other types of lasers due to their wavelength and mode of operation. However, it’s important to note that thermal tissue damage can still occur with TFL procedures if the laser parameters are not properly controlled or if excessive energy is delivered to the tissue. Careful attention to settings and technique is necessary to ensure optimal outcomes and minimize adverse effects.
When laser energy is applied to the stone, it causes rapid vaporization of water molecules within the stone, leading to the generation of a shock wave that fragments the stone into smaller pieces. Additionally, laser energy absorbed by the calyceal fluid increases temperature locally.The main concern regarding the use of the Ho: YAG laser is its potential thermal effects on the surrounding urothelium and kidney tissue [6]. The extent of temperature increase depends on factors like laser power settings, laser application duration, irrigation rate, stone characteristics, and composition and volume of the calyceal fluid.
An increase in the intrarenal temperature (IRT) during laser lithotripsy of urinary system stones has been demonstrated in animal models and 3D modelling studies, with discussions on the effective parameters and outcomes of temperature increase [7,8,9,10,11,12,13,14,15,16,17,18,19]. However, the clinical significance of this temperature increase is still a topic of debate. While moderate temperature increases are generally well tolerated by the surrounding tissues, excessive heat could cause thermal injury to the renal parenchyma or surrounding structures. Studies have been designed with 43 °C as the threshold temperature value, based on research showing protein denaturation at 43 °C in the porcine urinary system [20]. Currently, few clinical studies have addressed the monitoring of IRT during laser lithotripsy for kidney stones [21,22,23].
The primary aim of this study was to monitor IRT changes during Ho: YAG laser treatment of kidney stones, while the secondary aim was to investigate the effects of different variables on the mean temperature.
Patients and methods
Patients undergoing flexible ureteroscopic Ho: YAG laser lithotripsy at our center from March to August 2023 were enrolled after ethics approval (Approval no. 2023/13). The inclusion criteria were as follows: (1) 18 years or older, (2) diagnosed with kidney stones, and (3) whose longest diameter of the stone was less than 2 cm. The exclusion criteria were (1) pediatric patients, (2) patients with congenital kidney/ureter anomalies, (3) patients with ureteral stricture or concurrent ureteral stone, and (4) patients who were pregnant or lactating. Informed consent was obtained from eligible patients before inclusion in the study.
Surgery was performed 7–10 days after inserting a 6/26 DJ stent (Boston Scientific, USA) to improve ureteral access sheath insertion success and reduce ureteral damage risk. All patients had a sterile urine culture five days before surgery. A single experienced surgeon (Y.B.) performed all operations.
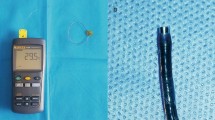
We used a thermometer (model 88,598 4ch K SD Logger) capable of recording data at 1-second intervals for the temperature measurement system. The measurement range of the thermometer was − 200 °C to + 350 °C, with a measurement accuracy of ± 0.1 °C. It employs a T-type thermal probe with a diameter of 0.3 mm. To measure the IRT during the operation, the thermal probe was attached to a disposable flexible ureterorenoscope (WiScope®, Germany) with its tip 10 mm from the distal end (Fig. 1) and inserted into the collecting system with a flexible ureterorenoscope through a 13/15 single lumen ureteral access sheath (Navigator™ HD, Boston Scientific, USA).
We utilized a holmium laser system (Sphinx Jr., Promed, Germany) equipped with a 272 μm laser fibre (FlexiFib, LISA Laser Products, Germany) to carry out lithotripsy. Each patient underwent lithotripsy using saline solution at room temperature (25.41 ± 2.82 °C). The experimental protocol included mechanical pump irrigation, specifically using a serum infusion pump, at flow rates of 10 ml/min, 15 ml/min, and 20 ml/min. The laser employed for this purpose was 8 W (0.8 J/10 Hz). In addition to the mechanical pump irrigation models, gravity (60 cm above the operating table) and manual pump (pumping as needed to enhance visualization quality) irrigation models were employed for the 14 W (1.2 J/12 Hz) laser setting.
When the flexible ureterorenoscope reached the calyceal system, temperature measurements began. The measurements ended when no clinically significant residual fragments (< 3 mm) were confirmed by endoscopic or fluoroscopic examination. For each study model, many characteristics were recorded, including lasing time (the duration of the active laser pedal on time), lithotripsy time (the time interval from the beginning of laser activation to the conclusion of the final laser activation, considering the durations of pedal on and off), operator duty cycle (ODC) (lasing time/lithotripsy time), total energy, and IRT.
Statistical analysis
The data were analysed using the Statistics Package for Social Sciences version 25 (IBM SPSS®, Armonk, NY). The Shapiro‒Wilk test was used to verify normal distribution compliance. Normally distributed data are presented as the mean ± standard deviation, while nonnormally distributed data are presented as the median (minimum-maximum). For normally distributed data, repeated measures analysis of variance was used to compare the effects of different irrigation modes across different laser working modes, with multiple comparisons performed using the Bonferroni correction. For nonnormally distributed data, the Friedman test was used to compare the effects of different irrigation modes across different laser working modes, with multiple comparisons conducted using the Dunn test. Generalized linear mixed models were used to assess the effects of the independent variables on the mean temperature, with multiple comparisons performed using the Bonferroni correction. Linear regression analysis was used to identify predictors of mean temperature. p < 0.05 was considered to indicate statistical significance.
Results
Overall, 15 patients were included in our study. Table 1 shows the clinical and perioperative characteristics of the patients. The mean age was 51,27 ± 15,50 years, and the mean body mass index (BMI) was 26,43 ± 4,47 kg/m2. The mean stone size was 139.49 ± 15.07 mm2, and the stone location was the renal pelvis in 60% of patients.
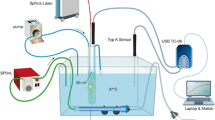
For demonstration, the intrarenal temperature‒time graph of “patient 2” is shown in Fig. 2. The IRT sharply decreased with irrigation before laser lithotripsy began, increased with decreasing irrigation rate at 8 W, and decreased with increasing irrigation rate at 14 W. There was a sharp decrease in IRT when transitioning from the gravity irrigation model to the manual pump irrigation model.
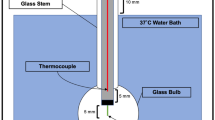
We analyzed temperature records from cases with around forty seconds of continuous laser activation, investigating different laser powers and irrigation settings. As the laser power increased and the irrigation rate decreased, the calyceal fluid heated more rapidly and eventually reached a plateau temperature. It was also noted that the time to reach the plateau temperature was prolonged with a similar relationship between the laser power and irrigation model (Fig. 3).
The overall surgical parameters are summarized in Table 2. In the 8 W working model, the lowest minimum, mean, and maximum IRT were obtained in the 20 ml/min irrigation model (27.5 ± 2.8 °C, 30.2 ± 2.2 °C, and 31.7 ± 2.1 °C; p = 0.017, p = 0.002, and p = 0.001, respectively). In the 14 W working model, while the minimum and mean IRT values were lowest in the manual pump irrigation model (median 26.76 °C and 31.80 °C, respectively; p < 0.001), the lowest maximum IRT was obtained in the 20 ml/min irrigation model (35.21 ± 2.30 °C; p = 0.005). The total energy values in the 8 W and 14 W working models were comparable.
The effects of demographic and operative variables on the mean IRT are shown in Table 3. In the univariate analysis examining the purification effects, age, sex, stone size, stone computed tomography (CT) value, laser power, irrigation model, and ODC were the parameters that significantly affected the mean IRT. In the multiple analysis evaluating the interactions of parameters, unlike the results of the univariate analysis, sex was not found to have a significant effect on the mean temperature (p = 0.616). In contrast, total energy had a significant effect (p = 0.012). According to the standardized β coefficients, the laser power had the most significant effect on the mean IRT, with the mean IRT being 4.981 °C greater for the 14 W laser power than for the 8 W laser power (p < 0.001). Compared to the 20 ml/min irrigation model, the mean IRT value was 2.075 °C higher in the gravity irrigation model and 2.828 °C lower in the manual pump irrigation model (p = 0.038 and p = 0.005, respectively).
A multiple linear regression model was constructed to predict the mean IRT based on BMI, laser power, the irrigation model, and ODC (Table 4). The calculated regression model was statistically significant (p < 0.001). While laser power and ODC had positive effects on the mean IRT, increases in BMI and irrigation were expected to decrease the mean IRT. The current variables could explain approximately 49.5% of the mean IRT (Adj. R2 = 0.495).
In the 8 W laser power treatment group, none of the irrigation treatments reached the threshold of 43 °C. Additionally, in the 14 W laser power group, one patient reached an IRT of 43 °C in the 10 ml/min irrigation model, and one patient reached this IRT in the gravity irrigation model.
Discussion
Our study revealed that in patients who underwent RIRS with a Ho: YAG laser, the laser power, irrigation model and ODC affect and predict the IRT. To our knowledge, this is the first clinical study to investigate the effects of variables other than laser power and irrigation models in RIRS patients treated with the Ho: YAG laser.
According to the essential laws of thermodynamics, in a constant environment, the amount of heat energy per unit time should remain constant, thus resulting in a constant temperature change (Q = mcΔT). Our study revealed that a continuous active laser could be used for forty seconds without interruption, i.e., when a constant amount of heat energy could be produced in a unit, the IRT increased for a period and then reached a plateau (Fig. 3). In this model, where the environment is not constant, the attainment of a plateau can be explained by the inflow of unheated irrigation fluid into the caliceal system and the outflow of heated irrigation fluid from the caliceal system. This phenomenon is consistent with previous studies reported in the literature [8, 19, 23, 24]. The fact that the IRT reaches a plateau at constant irrigation rates suggests that the mean IRT is a more important parameter than the peak IRT in clinical studies.
The laser settings are personalized. The pulse energy can then be gradually increased until an effective dusting or fragmentation effect is achieved. In our study, the laser power was the most effective parameter for determining the mean IRT. In the regression analysis evaluating predictors, it is predicted that there will be a 4.74 °C increase in the mean IRT with a one-unit increase in laser power (Table 4). In an experimental study by Aldoukhi et al., the highest temperature (70.3 °C) was reached with 40 W laser power and no irrigation mode among laser powers ranging from 5 W to 40 W [8]. In the pig model study of Peteinaris et al., which considered 54 °C as the thermal threshold, the threshold value was reached with laser powers above 40 W in the gravity irrigation model. In contrast, a safe thermal range was maintained with 20 W and 40 W laser powers [25]. In the pig model study conducted by Noureldin et al., the IRT remained within safe ranges at 20 W laser power when an access sheath was used, and in the gravity irrigation model, threshold temperature values that could cause thermal damage in the urinary system were reached with higher laser powers [17].
The irrigation model has emerged as an influential parameter of IRT. According to a survey study conducted among urologists interested in endourology in 2019, 46% preferred manual pump irrigation, and 27% preferred gravity irrigation as an irrigation method [26]. In this study, the highest mean IRT values were obtained in the gravity irrigation model compared to those in the other irrigation models, while the lowest mean IRT was obtained in the manual irrigation model (Table 3). In the study by Peteinaris et al., the thermal threshold was reached in the gravity irrigation model at 40 W and 60 W laser powers with 30 s of laser activation, while the safe thermal range was maintained in the manual pump irrigation model under similar laser settings [27]. In another in vivo porcine model study, hazardous IRT values were reached in the gravity irrigation model at laser powers exceeding 40 W, regardless of the use of a ureteral access sheath. However, the manual pump irrigation model only reached the thermal threshold with 100 W laser power and without using a ureteral access sheath [25].
In daily practice, suspending irrigation flow can prevent stone retropulsion during lithotripsy. However, careful attention must be paid during this manoeuvre. In one patient in our study, the IRT increased by 9 °C in a very short period of 5 s during lithotripsy when irrigation was inadvertently closed, which is not known. An in vitro study by Buttice et al. demonstrated that irrigation limits temperature increase when any laser setting is used, and rapid increases occur when irrigation is closed [10]. Another experimental ureteroscopy model by Wolin et al. reached the threshold thermal value in all laser power models ranging from 3.6 W to 20 W without continuous irrigation [28]. Hein et al. reported that laser application without irrigation led to a rapid temperature increase of up to ∆28 K, reaching 68 °C at 100 W [24]. Considering all these findings, continuous irrigation flow is essential for maintaining a safe thermal range.
Louters et al.‘s in vitro study investigating the effect of ODC on temperature showed that as ODC increased, higher temperatures were reached in shorter periods [29]. In an in vitro study by Aldoukhi et al., the thermal injury threshold was reached in as little as 9 s with 50% ODC at 40 W laser power [7]. An in vitro experiment suggested utilizing ODC as a method to restrict the increase in temperature in small cavities, such as the ureter or minor calyxes [30]. Pauchard et al.‘s review on intrarenal temperature and pressure during RIRS suggested halting laser activation to mitigate the risk of high temperatures [31]. In our study, consistent with the literature, when laser activation was stopped during transitions between each working model, we observed a dramatic decrease in the IRT (Fig. 2). Additionally, according to both univariate and multivariate analyses, ODC had a positive effect on the mean IRT (Table 3).
In our study, the thermal threshold was not reached in any irrigation model at 8 W laser power. In contrast, at 14 W laser power, an IRT of 43 °C was reached in the 10 ml/min and gravity irrigation models. An in vitro study by Maxwell et al. modelled the human urinary system using laser powers ranging from 5 to 40 W and irrigation modes, including no irrigation, 15 ml/min, and 40 ml/min. Laser activation was performed for 60 s. Consistent with our study, they found that the thermal threshold was not reached with a laser power of 20 W or less and irrigation rates of 15 ml/min above [14]. Similarly, Teng et al. reported that in their clinical study, the IRT remained within a safe thermal range with low laser power (< 20 W) and an irrigation rate of at least 15 ml/min [23]. In a clinical study by Æsøy et al. utilizing a Thulium fibre laser, similar findings were reported where temperatures of 43 °C were not reached with laser powers of 5 W and 10 W and an irrigation rate of 15 ml/min [22]. Currently, there is no defined optimal laser setting or irrigation model for RIRS. However, low laser power (< 20 W) and moderate irrigation flow (15–30 ml/min) appear to be feasible options for managing the IRT [31].
We are aware that laser frequency is an important parameter affecting IRT. In an in-vitro study by Aldoukhi et al., it was found that at 20 Hz, only 52% of emitted pulses reached the stone, while at 50 Hz and 80 Hz, only 23% and 4% reached the stone, respectively [32]. Thus, with increased frequency, more energy will be absorbed in the liquid medium, leading to higher IRT. In their experimental ureteroscopic lithotripsy model, Liang et al. reported that higher frequencies at the same laser powers resulted in more heat production [33]. In an in-vitro study comparing low-frequency high single-pulse energy with high-frequency, low single-pulse energy models, Hein et al. associated higher frequency settings with 3.5% and 8.8% higher temperatures at low and high laser powers, respectively [24]. In a porcine model study by Gallegos et al., the IRT value was measured at the beginning of the study and one minute after laser use, and the difference between these two measurements was defined as delta temperature (DT). Energy, frequency, use of ureteral access sheath, and liquid height were found to be parameters significantly affecting DT, with a predicted increase of 2.1 °C in DT at 15 Hz frequency compared to 5 Hz [34]. Maxwell et al. conducted a study with laser powers ranging from 5 to 40 W and different irrigation models, finding that peak temperature values were nearly the same at the same laser powers regardless of frequency and pulse setting [14].
Does IRT truly matter in clinical practice? Aldoukhi et al. performed intrarenal laser activation with a Ho: YAG laser at 40 W power for 60 s, without irrigation, and with low- and high-flow-rate irrigation in four in vivo pig models and achieved maximum IRTs of 84.8 °C, 63.9 °C and 43.6 °C, respectively. On histopathological examination, gross macroscopic changes were observed in the no-irrigation model. At the same time, it was reported that there were minimal changes in low-flow irrigation and no signs of thermal damage in high-flow irrigation [9]. Molina et al. created a ureteral stone model in ex vivo porcine models using manual irrigation, a Ho: YAG laser (6.4 W and 21 W), and a spTFL (6.4 W and 20 W). Both systems remained below the threshold temperature (43 °C). According to histopathological examination, there was no thermal damage to the ureters after lithotripsy [15]. Peteinaris et al. created a kidney stone model in two in vivo porcine models and performed laser lithotripsy using an 8 W Thulium fibre laser for 60 min. The IRT was between 44 °C and 46 °C in both models. The kidneys were histopathologically examined on the 7th and 14th days. On the 7th day, severe histopathological findings such as hemorrhagic areas, separated urothelium, fibrin accumulation, and inflammation in the lamina propria were observed, while on the 14th day, histopathology was reported as “minimal changes” [35]. Therefore, it is not easy to provide a definitive answer when evaluating these findings in light of the study findings. However, given the lack of sufficient evidence regarding the long-term effects of high temperatures, a lower IRT appears safer.
The thermal cytotoxic effect occurring in living tissues can be explained by the temperature and duration of exposure. Sapareto and Dewey developed an equation known as the cumulative equivalent minutes at 43 °C (CEM43) to assess the thermal dose, which is calculated based on an exposure time at a reference temperature of 43 °C [36]. Animal studies have shown that protein denaturation occurs in the urinary system at 43 °C [20], and a CEM43 duration exceeding 70 min leads to significant kidney damage [37]. Since there is no defined safe thermal dose for the human urinary system, we adopted 43 °C as the thermal threshold for our study based on the current literature.
During RIRS, delivering the probe to the calyceal system either retrogradely or percutaneously is necessary to enable IRT monitoring. Despite its fine calibration, which may influence irrigation flow and misrepresent actual IRT readings, the retrograde approach appears less morbid than percutaneous access. The retrograde method, contingent upon using a ureteral access sheath, is reliable. However, there is a need for more clinical studies regarding routine IRT monitoring during RIRS. Currently, flexible ureterorenoscopes capable of intrarenal pressure monitoring are used in clinical practice during RIRS [38], yet an instrument that facilitates IRT monitoring has yet to be developed. Future research in this area will inevitably involve the use of thermal probes.
The present study has several limitations. First, our study has a small sample size, which may introduce bias when estimating population means. Second, since each patient’s calyceal anatomy and volume may vary, different IRT results may have been obtained with similar variables. Third, since it is not always possible to keep the laser fibre at the same distance from the stone and from the thermal probe, different IRT results may have been obtained with similar variables. Fourth, a multipoint thermal probe could not be utilized, and the temperature of each major calyx could not be measured; thus, the recorded temperature might not have accurately reflected the mean IRT. Fifth, as the recording device monitor could not provide real-time temperature information, laser activation was continued in cases where critical temperatures were reached. Sixth, due to the lack of chemical stone analysis, the possible effect on the temperature profile could not be investigated.
Conclusion
This preliminary study investigated the impact of Ho: YAG laser lithotripsy on intrarenal calyceal fluid temperature, focusing on the influence of laser power and irrigation rate. The results revealed that the Ho: YAG laser power and irrigation rate had opposite effects on the average temperature, with the laser power being the most influential parameter for temperature elevation. Continuous irrigation at a minimum rate of 15 ml/min helps maintain temperatures within the safe range, particularly at moderate laser powers. Furthermore, this study revealed ODC as a significant parameter affecting IRT, suggesting the importance of the periodic cessation of laser activation. These findings underscore the necessity for further clinical studies with larger populations to elucidate additional factors impacting IRT dynamics during laser lithotripsy.
Data availability
No datasets were generated or analysed during the current study.
References
Zeng G, Zhao Z, Mazzon G, Pearle M, Choong S, Skolarikos A et al (2022) European Association of Urology Section of Urolithiasis and International Alliance of Urolithiasis Joint Consensus on Retrograde Intrarenal surgery for the management of Renal stones. Eur Urol Focus 8(5):1461–1468 Epub 2021/11/28. https://doi.org/10.1016/j.euf.2021.10.011
Knudsen BE (2019) Laser fibers for Holmium:YAG lithotripsy: what is important and what is New. Urol Clin North Am 46(2):185–191 Epub 2019/04/10. https://doi.org/10.1016/j.ucl.2018.12.004
Traxer O, Keller EX (2020) Thulium fiber laser: the new player for kidney stone treatment? A comparison with Holmium:YAG laser. World J Urol 38(8):1883–1894 Epub 2019/02/08. https://doi.org/10.1007/s00345-019-02654-5
Traxer O, Rapoport L, Tsarichenko D, Dymov A, Enikeev D, Sorokin N et al (2018) V03-02 first clinical study on superpulse thulium fiber laser for lithotripsy. J Urol 199(4S):e321–e2
White C, Aziz M (1985) Energy deposition, heat flow, and rapid solidification during laser and electron beam irradiation of materials. Oak Ridge National Lab
Lopes ACN, Dall’Aqua V, Carrera RV, Molina WR, Glina S (2021) Intra-renal pressure and temperature during ureteroscopy: does it matter? Int Braz J Urol 47(2):436–442 Epub 2020/12/08. https://doi.org/10.1590/s1677-5538.Ibju.2020.0428
Aldoukhi AH, Dau JJ, Majdalany SE, Hall TL, Ghani KR, Hollingsworth JM et al (2021) Patterns of laser activation during ureteroscopic lithotripsy: effects on Caliceal Fluid temperature and thermal dose. J Endourol 35(8):1217–1222 Epub 2021/01/06. https://doi.org/10.1089/end.2020.1067
Aldoukhi AH, Ghani KR, Hall TL, Roberts WW (2017) Thermal response to high-power holmium laser lithotripsy. J Endourol 31(12):1308–1312. https://doi.org/10.1089/end.2017.0679PubMed PMID: 29048216 Epub 2017/10/20
Aldoukhi AH, Hall TL, Ghani KR, Maxwell AD, MacConaghy B, Roberts WW (2018) Caliceal Fluid Temperature during High-Power Holmium laser lithotripsy in an in vivo Porcine Model. J Endourol 32(8):724–729 Epub 2018/06/16. https://doi.org/10.1089/end.2018.0395
Butticè S, Sener TE, Proietti S, Dragos L, Tefik T, Doizi S et al (2016) Laser Usage? J Endourol 30(5):574–579 Epub 2016/02/04. https://doi.org/10.1089/end.2015.0747. Temperature Changes Inside the Kidney: What Happens During Holmium:Yttrium-Aluminium-Garnet
Dau JJ, Hall TL, Maxwell AD, Ghani KR, Roberts WW (2021) Effect of chilled irrigation on Caliceal Fluid temperature and Time to Thermal Injury threshold during laser lithotripsy: in Vitro Model. J Endourol 35(5):700–705 Epub 2020/11/13. https://doi.org/10.1089/end.2020.0896
Gallegos H, Bravo JC, Sepúlveda F, Astroza GM (2021) Intrarenal temperature measurement associated with holmium laser intracorporeal lithotripsy in an ex vivo model. Cent Eur J Urol 74(4):588–594 Epub 2022/01/28. https://doi.org/10.5173/ceju.2021.0092
Kallidonis P, Kamal W, Panagopoulos V, Vasilas M, Amanatides L, Kyriazis I et al (2016) Thulium Laser in the Upper urinary tract: does the Heat Generation in the Irrigation Fluid pose a risk? Evidence from an in vivo experimental study. J Endourol 30(5):555–559 Epub 2016/01/06. https://doi.org/10.1089/end.2015.0768
Maxwell AD, MacConaghy B, Harper JD, Aldoukhi AH, Hall TL, Roberts WW (2019) Simulation of laser lithotripsy-Induced Heating in the urinary tract. J Endourol 33(2):113–119 Epub 2018/12/27. https://doi.org/10.1089/end.2018.0485
Molina WR, Carrera RV, Chew BH, Knudsen BE (2021) Temperature rise during ureteral laser lithotripsy: comparison of super pulse thulium fiber laser (SPTF) vs high power 120 W holmium-YAG laser (Ho:YAG). World J Urol 39(10):3951–3956 Epub 2021/02/20. https://doi.org/10.1007/s00345-021-03619-3
Molina WR, Silva IN, Donalisio da Silva R, Gustafson D, Sehrt D, Kim FJ (2015) Influence of saline on temperature profile of laser lithotripsy activation. J Endourol 29(2):235–239 Epub 2014/08/27. https://doi.org/10.1089/end.2014.0305
Noureldin YA, Farsari E, Ntasiotis P, Adamou C, Vagionis A, Vrettos T et al (2021) Effects of irrigation parameters and access sheath size on the intra-renal temperature during flexible ureteroscopy with a high-power laser. World J Urol 39(4):1257–1262 Epub 2020/06/20. https://doi.org/10.1007/s00345-020-03287-9
Winship B, Terry R, Boydston K, Carlos E, Wollin D, Peters C et al (2019) Holmium:Yttrium-Aluminum-Garnet laser pulse type affects irrigation temperatures in a Benchtop Ureteral Model. J Endourol 33(11):896–901 Epub 2019/08/17. https://doi.org/10.1089/end.2019.0496
Winship B, Wollin D, Carlos E, Peters C, Li J, Terry R et al (2019) The rise and fall of high temperatures during Ureteroscopic Holmium laser lithotripsy. J Endourol 33(10):794–799 Epub 2019/04/25. https://doi.org/10.1089/end.2019.0084
Van Rhoon GC, Samaras T, Yarmolenko PS, Dewhirst MW, Neufeld E, Kuster N (2013) CEM43° C thermal dose thresholds: a potential guide for magnetic resonance radiofrequency exposure levels? Eur Radiol 23:2215–2227
Wu Z, Wei J, Sun C, Huangfu Q, Wang B, Huang G et al (2023) Temperature changes of renal calyx during high-power flexible ureteroscopic Moses Holmium laser lithotripsy: a case analysis study. Int Urol Nephrol 55(7):1685–1692 Epub 2023/05/05. https://doi.org/10.1007/s11255-023-03611-3
Æsøy MS, Juliebø-Jones P, Beisland C, Ulvik Ø (2024) Temperature Measurements During Flexible Ureteroscopic Laser Lithotripsy: A Prospective Clinical Trial. J Endourol. Epub 2024/01/08. https://doi.org/10.1089/end.2023.0660. PubMed PMID: 38185920
Teng J, Wang Y, Jia Z, Guan Y, Fei W, Ai X (2021) Temperature profiles of calyceal irrigation fluids during flexible ureteroscopic Ho:YAG laser lithotripsy. Int Urol Nephrol. ;53(3):415-9. Epub 2020/09/30. https://doi.org/10.1007/s11255-020-02665-x. PubMed PMID: 32989671
Hein S, Petzold R, Schoenthaler M, Wetterauer U, Miernik A (2018) Thermal effects of Ho: YAG laser lithotripsy: real-time evaluation in an in vitro model. World J Urol. ;36(9):1469-75. Epub 2018/04/25. https://doi.org/10.1007/s00345-018-2303-x. PubMed PMID: 29691640
Peteinaris A, Pagonis K, Vagionis A, Adamou C, Tsaturyan A, Ballesta Martínez B et al (2022) What is the impact of pulse modulation technology, laser settings and intraoperative irrigation conditions on the irrigation fluid temperature during flexible ureteroscopy? An in vivo experiment using artificial stones. World J Urol 40(7):1853–1858. https://doi.org/10.1007/s00345-022-04002-6
Pietropaolo A, Bres-Niewada E, Skolarikos A, Liatsikos E, Kallidonis P, Aboumarzouk O et al (2019) Worldwide survey of flexible ureteroscopy practice: a survey from European Association of Urology sections of young academic urologists and uro-technology groups. Cent Eur J Urol 72(4):393–397 Epub 2020/02/06. https://doi.org/10.5173/ceju.2019.0041
Peteinaris A, Faitatziadis S, Tsaturyan A, Pagonis K, Liatsikos E, Kallidonis P (2022) MOSES™ pulse modulation technology versus conventional pulse delivery technology: the effect on irrigation fluid temperature during flexible ureteroscopy. Urolithiasis 50(5):613–618. https://doi.org/10.1007/s00240-022-01342-1
Wollin DA, Carlos EC, Tom WR, Simmons WN, Preminger GM, Lipkin ME (2018) Effect of laser settings and Irrigation Rates on Ureteral Temperature during Holmium laser lithotripsy, an in Vitro Model. J Endourol 32(1):59–63 Epub 2017/10/20. https://doi.org/10.1089/end.2017.0658
Louters MM, Dau JJ, Hall TL, Ghani KR, Roberts WW (2022) Laser operator duty cycle effect on temperature and thermal dose: in-vitro study. World J Urol 40(6):1575–1580 Epub 2022/02/28. https://doi.org/10.1007/s00345-022-03967-8
Rezakahn Khajeh N, Hall TL, Ghani KR, Roberts WW (2022) Pelvicaliceal volume and fluid temperature elevation during laser lithotripsy. J Endourol 36(1):22–28 Epub 2021/07/14. https://doi.org/10.1089/end.2021.0383
Pauchard F, Ventimiglia E, Corrales M, Traxer O (2022) A Practical Guide for Intra-Renal Temperature and Pressure Management during Rirs: What Is the Evidence Telling Us. J Clin Med. ;11(12). Epub 2022/06/25. https://doi.org/10.3390/jcm11123429. PubMed PMID: 35743499; PubMed Central PMCID: PMCPMC9224584
Aldoukhi A, Hall T, Ghani K, Roberts W (2020) Analysis of laser fiber to stone distance during different modes of laser lithotripsy. Eur Urol Open Sci 19:e340–e1
Liang H, Liang L, Yu Y, Huang B, Chen J, Wang C et al (2020) Thermal effect of holmium laser during ureteroscopic lithotripsy. BMC Urol 20:1–4
Gallegos H, Bravo JC, Sepúlveda F, Astroza GM (2021) Intrarenal temperature measurement associated with holmium laser intracorporeal lithotripsy in an ex vivo model. Cent Eur J Urol 74(4):588
Peteinaris A, Tsaturyan A, Bravou V, Tatanis V, Faria-Costa G, Pagonis K et al (2023) High-power laser lithotripsy - do we treat or harm? Histological evaluation of temperature effects in an in vivo study with thulium fiber laser. Cent Eur J Urol 76(1):44–48 Epub 2023/04/18. https://doi.org/10.5173/ceju.2023.24
Sapareto SA, Dewey WC (1984) Thermal dose determination in cancer therapy. Int J Radiat Oncol Biol Phys 10(6):787–800 Epub 1984/06/01. https://doi.org/10.1016/0360-3016(84)90379-1
Yarmolenko PS, Moon EJ, Landon C, Manzoor A, Hochman DW, Viglianti BL et al (2011) Thresholds for thermal damage to normal tissues: an update. Int J Hyperth 27(4):320–343 PubMed PMID: 21591897; PubMed Central PMCID: PMCPMC3609720
Bhojani N, Koo KC, Bensaadi K, Halawani A, Wong VK, Chew BH (2023) Retrospective first-in-human use of the LithoVue™ Elite ureteroscope to measure intrarenal pressure. BJU Int 132(6):678–685 Epub 2023/09/05. https://doi.org/10.1111/bju.16173
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
E.K.: Conceptualization, data curation, investigation, methodology, writing-orginal draft. Y.B.: Conceptualization, data curation, methodology, writing-review and editing. M.G.: Data curation, formal analysis. F.S.: Resources, data curation, formal analysis. O.K. and E.O.: Data curation, writing-review and editing. Y.K.Y.: Supervision, writing-review and editing. S.S.: Supervision, writing-review and editing. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kose, E., Bostanci, Y., Gulsen, M. et al. Monitoring Intrarenal temperature changes during Ho: YAG laser lithotripsy in patients undergoing retrograde intrarenal surgery: a novel pilot study. Urolithiasis 52, 86 (2024). https://doi.org/10.1007/s00240-024-01592-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00240-024-01592-1