Abstract
There are numerous options for breast reconstruction after mastectomy, and the final reconstructive option is often influenced by patient preference. This study surveyed plastic surgeons regarding their personal preferences for breast reconstruction after mastectomy to identify the impact of gender and age on reconstructive preference. An anonymous online survey was distributed to plastic surgeons in the American Society of Plastic Surgeons member directory and current plastic surgery residents. Female surgeons were asked to select reconstructive options for themselves as patients, while male surgeons were asked to answer the same questions as if advising a loved one. After unilateral mastectomy, 60.2 % of respondents preferred implant-based reconstruction, increasing to 67.8 % after bilateral mastectomy. Top reasons for selecting implant-based reconstruction were recovery time (78.0 %) and hospital length of stay (54.5 %). In contrast, respondents who preferred abdominal flap-based autologous reconstruction cited the longevity (83.3 %) and the aesthetic appearance of the final result (82.7 %) as top reasons. Female surgeons were significantly more likely to choose implant-based reconstruction than male surgeons (68.7 vs. 56.6 %, p = 0.001). Younger male surgeons preferred autologous reconstruction (58.8 %). Plastic surgeons’ reconstructive choices parallel current patient-based surveys favoring breast reconstruction with implants. Respondents’ reasons for selecting one reconstructive method over another are consistent with prior patient-based surveys. Female plastic surgeons prefer implant-based reconstruction to a greater extent than male plastic surgeons. This survey identifies the need for further prospective study of physician perspectives of patient experiences.
Level of Evidence: Not ratable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing breast reconstruction have several reconstructive options following mastectomy. In the last 20 years, the field of breast reconstruction has made significant advances with the advent of the perforator flap in the 1990s and the use of acellular dermal matrix and fat grafting in implant-based reconstruction effectively expanding reconstructive options for women post-mastectomy. The increase in available options has increased the complexity of the decision-making for post-mastectomy patients. The discussion between patient and surgeon must be tailored to address the patient’s medical history, anticipated recovery, and aesthetic goals while allowing for adjuvant cancer treatments. Unfortunately, as separate studies have shown, patients often do not fully comprehend the scope of the recovery and the nature of the complications even after extensive counseling [1, 2].
Plastic surgeons have performed the same procedures they would undergo themselves for their own breast reconstruction or recommend for their loved ones. Plastic surgeons have the most informed perspective possible. This prompted the author’s current investigation to determine if medical knowledge and experience with reconstruction would affect the decision of reconstructive method in the setting of diverse clinical backgrounds.
The purpose of this study is to determine the type of breast reconstruction female plastic surgeons would choose for themselves (women) or male plastic surgeons would recommend for their loved ones (men) through a survey of members of the American Society of Plastic Surgeons. In addition, the authors seek to identify any relationship that plastic surgeons’ gender and/or age has on their particular preferred method of breast reconstruction.
Material and Methods
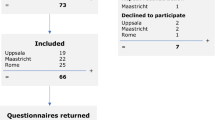
After institutional review board approval, an anonymous online survey was beta-tested at an outside institution. The updated survey was distributed to 6089 plastic surgeons in the American Society of Plastic Surgeons member directory and current plastic surgery residents in October 2013. Potential participants were sent an email that included a link to the survey as well as a brief cover letter explaining the purpose of the survey. Participation was voluntary and respondents were not provided compensation for their participation.
The survey included multiple-choice questions about respondents’ demographics, preferences for unilateral and bilateral breast reconstruction, preference for reconstruction after radiation, preference for prophylactic mastectomy, and preference for genetic testing. Female surgeons were asked to select reconstructive options considering themselves as patients when responding, while male surgeons were asked to answer the same questions as if they were advising a loved one when responding to the survey. Participants were asked to select their reasons for making certain decisions and could select multiple reasons for their decisions. Frequencies were obtained for all variables, and chi-square analyses were performed for categorical variables.
Results
A total of 467 responses were collected of the 6089 American Society of Plastic Surgeons members (response rate of 8 %). Of the 805 female members, 118 completed the survey for a 15 % response rate. Three hundred and forty-two of the 5284 male American Society of Plastic Surgeons members completed the survey (7 % response rate). About one-quarter of the respondents were female (26 %). All age groups and levels of training were represented in our sample (Table 1).
After unilateral mastectomy, 60 % of all respondents preferred implant-based reconstruction, 34 % preferred autologous abdominal flap-based reconstruction, 2 % preferred reconstruction with a latissimus dorsi flap and implant, and 4 % preferred no reconstruction. When asked about their reconstructive preferences after bilateral reconstruction, an even greater proportion of all respondents selected implant-based reconstruction (68 %, p = 0.001).
Female surgeons were significantly more likely to choose implant-based reconstruction than male surgeons after unilateral mastectomy (69 vs. 57 %, p = 0.001). This trend toward implant-based reconstruction increased when the plastic surgeon respondents were younger in age, with 70 % of females aged 25 to 34 preferring implant-based reconstruction and 41 % of males aged 25 to 34 preferring implant-based reconstruction (p = 0.236).
Reconstructive choice by age trended toward significance with younger surgeons preferring implant-based reconstruction at higher rates as compared to more experienced surgeons (p = 0.053). Middle-aged female surgeons were noted to have an increasing preference for autologous reconstruction (Fig. 1). In contrast, male plastic surgeons were noted to have a decreasing preference for autologous reconstruction with increasing age (Fig. 2). Males aged 25 to 34 were the only sub-group of all respondents that preferred autologous-based reconstruction to implant-based reconstruction (59 vs. 41 %).
Results of breast reconstruction preferences of male plastic surgeon respondents (n = 342) after unilateral mastectomy separated by age of male plastic surgeon respondent. Younger male plastic surgeons prefer autologous abdominal flap-based reconstruction over implant-based reconstruction, but that preference decreases with increasing age of the male plastic surgeon respondent, whereas implant-based reconstruction is preferred at higher rates
Respondents who selected implant-based reconstruction cited recovery time (78 %), hospital length of stay (55 %), and aesthetic appearance of the final result (40 %) as the top reasons for their choice. When separated by gender, the male respondents’ choices mirrored these reasons, while female respondents chose implant-based reconstruction due to recovery time (76 %), hospital length of stay (49 %), and fear of donor site weakness (43 %). Only 33 % of women who preferred implant-based reconstruction selected aesthetic appearance of the final result as one of their reasons for selecting implant-based reconstruction.
In contrast, male and female respondents who preferred autologous reconstruction selected the same top three reasons for this preference regardless of gender: aesthetic appearance of the final result (female respondents 77 %, male respondents 84 %), longevity of result (female respondents 85 %, male respondents 83 %), and preference for autologous tissue (female respondents 46 %, male respondents 69 %).
The smaller subset of participants who chose latissimus dorsi flap with implant reconstruction reported the aesthetic appearance of the final result (100 %), the desire for additional soft tissue coverage of the implant (89 %), and the longevity of the result (67 %) as their reasons for selecting this method of reconstruction. In total, 55 % of respondents stated that the aesthetic appearance of the final result was important in selecting a method of breast reconstruction.
When asked about their preferences for reconstruction if radiation would be required, 40 % selected delayed autologous reconstruction, 27 % selected immediate tissue expander placement followed by implant after radiation, 14 % selected “other”, and 12 % selected delayed latissimus dorsi flap with expander and staged implant reconstruction. The most common response of those who selected “other” was immediate tissue expander placement and delayed autologous tissue flap after radiation (n = 31). When all responses for autologous flap-based reconstructions were combined (immediate, delayed, and “other” responses), 55 % of plastic surgeons would prefer autologous flap-based reconstructions in the setting of breast radiation. Delayed autologous reconstruction, with or without tissue expander placement, was preferred over immediate autologous reconstruction (48 vs. 7 %).
A majority of plastic surgeons (75 %) would undergo or recommend genetic testing for breast cancer. These respondents selected a strong family history (87 %), having additional information to help with decision-making (83 %), and using the results to help decide between unilateral and bilateral mastectomy (73 %) as their top reasons for undergoing or recommending genetic testing.
A total of 45 % of respondents would undergo or recommend contralateral prophylactic mastectomy if genetic testing results were negative. Reasons for selecting contralateral prophylactic mastectomy included the desire to avoid a potential second treatment experience (87 %), symmetry concerns (83 %), and anxiety (73 %).
Discussion
Mastectomy rates are increasing nationwide with 38 % of women diagnosed with breast cancer undergoing mastectomy in 2008 [3]. With more women undergoing mastectomies, the need for breast reconstruction is ever growing [3]. Total reconstruction rates increased by 4 % per year from 1998 to 2008 [4, 5]. Rates of all forms of breast reconstruction increased during this period, with the rate of implant-based reconstruction consistently outpacing autologous reconstruction since 2002 [4].
The results of this national survey of plastic surgeons follow the public trend currently favoring implant-based reconstruction over abdominal flap-based reconstruction. Nearly two-thirds of the 467 respondents selected implant-based reconstruction. The reasons for their choice of implant-based reconstruction versus autologous reconstruction are also similar to the literature on patient preference. In this cohort of plastic surgeons, we found that recovery time (78 %), hospital length of stay (55 %), and esthetic appearance of the final result (40 %) were the most important factors in deciding to pursue or recommend implant-based reconstruction. Plastic surgeons who selected autologous-based reconstruction made their decision based on longevity (83 %), the aesthetic appearance of the final result (83 %), and a preference for autologous tissue (65 %). Prior studies have shown that patients who select implant-based reconstruction desire shorter procedure times, shorter recovery times, and hope to avoid donor site scars, while patients who select autologous-based reconstruction prioritize the durability of their result, the use of their own tissue, the avoidance of implant complications, and the added advantage of abdominoplasty [6, 7]. If a patient prioritizes a short recovery time with little morbidity over the final aesthetic outcome, then her plastic surgeon may recommend implant-based reconstruction over autologous-based reconstruction.
Implant reconstruction was preferred to a greater extent after bilateral mastectomy in this study (Figs. 3 and 4). This preference for implants for bilateral reconstruction may be due to symmetry concerns with matching the contralateral ptotic breast [8, 9]. In addition, the risk of abdominal wall weakness is greater with bilateral versus unilateral autologous reconstruction which makes implant-based reconstruction a more desirable option from a functional perspective [10].
Results of breast reconstruction preferences of female plastic surgeon respondents (n = 118) after bilateral mastectomy separated by age of female plastic surgeon respondent. Implant-based reconstruction is strongly favored by female plastic surgeon respondents of all ages. Although middle-aged female plastic surgeons have an increasing preference for autologous abdominal flap-based reconstruction, it does not overcome the preference in those age groups for implant-based reconstruction
Results of breast reconstruction preferences of male plastic surgeon respondents (n = 342) after bilateral mastectomy separated by age of male plastic surgeon respondent. Implant-based reconstruction is strongly favored by male plastic surgeon respondents of all ages, with the exception of the youngest male plastic surgeons with an equivalent preference for implant and autologous flap-based reconstruction. With increasing age of male plastic surgeon respondent, a decreasing preference is seen for autologous flap-based reconstruction, while the preference for implant-based reconstruction increases with respondent age
Female plastic surgeons in our study had a greater preference for implant-based reconstruction after unilateral mastectomy when compared with their male counterparts (69 vs. 57 %). The reasons cited by both gender groups include recovery time and hospital length of stay. They differ in that female plastic surgeons more frequently cited donor site weakness as a concern during recovery whereas their male counterparts reported that the favorable aesthetic benefits of implant-based reconstruction as a major reason for their selection.
A reason for this difference may be the inherent differences between the two groups surveyed in this model. Specifically, the longer recovery and introduction of potential donor site morbidity associated with abdominal flap-based breast reconstruction may be of greater concern to female plastic surgeons who would undergo the procedures themselves compared to their male counterparts recommending the procedures for a loved one. The female surgeons choosing implant-based reconstruction clearly place a premium on returning to work as expediently as possible, as aesthetic appearance of the final result was not among the top three reasons female respondents selected this reconstructive method. This is in contrast to male respondents for whom aesthetic appearance of the final result was the third most common reason for choosing this reconstructive method.
Younger plastic surgeons favored implant-based reconstruction at higher rates than more experienced surgeons with similar reasons for their selections between groups surveyed. These results support prior studies that have shown that women who choose implant-based reconstruction tend to be younger than women who choose autologous-based reconstruction.7, 8 Previous studies have speculated that younger women prefer implant-based reconstruction because younger women may have inadequate donor tissue for autologous reconstruction or may wish to avoid prolonged recovery times and donor site morbidity [3, 7].
Differences in reconstructive preference by gender varied with surgeon age in our analysis. With increasing age, female plastic surgeons showed an increasing preference for autologous abdominal flap-based reconstruction over implants while male plastic surgeons demonstrated a decreasing preference for autologous abdominal flap-based reconstruction in favor of implant-based reconstruction. This trend was true for both unilateral and bilateral mastectomies and was especially prominent for young plastic surgeons. Seventy percent of females aged 25 to 34 preferred implant-based reconstruction, while only 41 % of their age-matched male counterparts had the same preference after unilateral mastectomy.
All gender and age groups cited recovery time and hospital length of stay as the top reasons when selecting implant-based reconstruction. Appearance of the final result was a top reason for older females (ages 65 and over) and younger males (ages 64 and younger). When selecting autologous tissue for reconstruction, all gender and age groups noted longevity of the result, aesthetic appearance of the final result, and a preference for autologous tissue as their top three choices.
This trend of younger female respondents selecting implants over autologous reconstruction is consistent with previous studies evaluating patient preferences as stated above; however, the converse relationship among male respondents has not been previously reported [6, 7]. In similar fashion to studies on patient preferences, aesthetics and longevity of the result were more commonly a priority for respondents selecting autologous reconstruction, whereas minimizing recovery time and donor site morbidity was a focus for those selecting implants across all gender and age subsets in this analysis. When considering radiation and breast reconstruction, a majority of plastic surgeons selected autologous-based reconstruction (55 %). Delayed autologous reconstruction was preferred over immediate autologous reconstruction (48 vs. 7 %), and implant placement after radiation was preferred to implant placement before radiation (27 vs. 8 %). Our results support the current literature demonstrating a preference for autologous tissue and delayed reconstruction in irradiated patients [11–16].
Over three-quarters of surveyed plastic surgeons would undergo or recommend genetic testing if diagnosed with breast cancer. It is interesting that nearly half (45 %) of plastic surgeons would undergo or recommend contralateral prophylactic mastectomy with negative genetic testing results. This is higher than previous studies that have shown a 24–37 % rate of contralateral prophylactic mastectomy in BRCA1/BRCA2 negative patients [17, 18]. This increased preference for contralateral prophylactic mastectomy may be secondary to plastic surgeons’ stronger desire to avoid becoming a patient again. This is supported by our results, which show that 87 % of respondents would undergo or recommend contralateral prophylactic mastectomy to avoid a second treatment experience. Although not necessarily recommended from an oncologic perspective, this decision arises from the perspective of achieving symmetry in the final reconstructive result as well as the avoidance of (low) risk of cancer in contralateral breast. Thus, an increased number of plastic surgeons compared to the public prefer simultaneous contralateral mastectomy even with negative genetic testing.
This survey study design revealed similarities and differences between surveyed plastic surgeons and previous reports on patient preferences for breast reconstruction. An overall preference for implant-based reconstruction and the reasons for doing so were consistent with those of prior patient studies on breast reconstruction decision-making. A recent study demonstrated that full-time working women and women who make >$100,000 per year have an increased preference for implant-based reconstruction [19]. Female plastic surgeons fall into both of these demographic categories and further support their preference for implant-based reconstruction. However, a greater portion of plastic surgeons would proceed with prophylactic mastectomy without positive genetic testing than prior studies with their knowledge of risks, benefits, and surgical outcomes.
Young male plastic surgeons more commonly preferred autologous reconstruction than implant-based reconstruction citing durability and aesthetics as their reasons for their selection with this difference waning as respondent age increased.
This finding has not been previously reported and was rendered by the unique study design that included male respondents. Although this required the gender groups being compared to answer different questions on about their roles in surgical decisions for oneself versus a loved one, it was relevant to the goals of the study to include the perspectives of both groups who are quite uniquely informed about breast reconstruction.
The quality of the survey data was found to be an appropriate sampling of the American Society of Plastic Surgeons with all age groups and genders represented. The subset analyses for age and gender did not have equal numbers between groups potentially underpowering this portion of the analysis but trends could be identified. The survey response rate of 8 % is greater than that of the Tracking Operations and Outcomes for Plastic Surgeons database—the national self-reporting plastic surgery metric for quality and outcomes. This finding implies that an 8 % response rate in this study population is reasonable and expected [20].
Future studies may be warranted to address surgeons’ personal experiences and comfort level with performing different types of breast reconstruction. Specifically addressing surgeon experience and comfort with free flap breast reconstruction may help to further explain the differences in surgeon preferences demonstrated in this article.
Conclusions
As breast cancer affects one in eight women, our results have the potential to impact a large number of patients. Patients would truly benefit from the knowledge of what the most informed patients (plastic surgeons) would choose for their own breast reconstruction, with the understanding that this study group has a known bias for selecting a reconstructive option with a quicker return to a physically rigorous work schedule. While decision-making for breast reconstruction necessarily takes into account patient specific variables such as body habitus, history of radiation, and patient preference, the results of this study will be very helpful during preoperative counseling. Taking on the patient perspective is a valuable exercise to aid plastic surgeons in their discussions with patients. As our knowledge of patient perspectives grows, we will increasingly be able to advise patients more accurately on the most appropriate breast reconstruction tailored to meet their individual needs.
References
Lloyd AJ (2001) The extent of patients’ understanding of the risk of treatments. Qual Health Care 10(Suppl 1):i14–i18
Weinstein ND (1989) Optimistic biases about personal risks. Science 246:1232–1233
Albornoz CR, Bach PB, Mehrara BJ, et al. (2013) A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 131(1):15–23
Reuben BC, Manwaring J, Neumayer L (2009) Recent trends and predictors in immediate breast reconstruction after mastectomy in the United States. Am J Surg 198(2):237–243
Hernandez-Boussard T, Zeidler K, Barzin A, et al. (2013) Breast reconstruction national trends and healthcare implications. Breast J 19(5):463–469
Nelson J, Tchou J, Domchek S, et al. (2012) Breast reconstruction in bilateral prophylactic mastectomy patients: factors that influence decision making. J Plast Reconstr Aesthet Surg 65(11):1481–1489
Gopie JP, Hilhorst MT, Kleijne A, et al. (2011) Women’s motives to opt for either implant or DIEP-flap breast reconstruction. J Plast Reconstr Aesthetic Surg 64:1062–1067
Leone MS, Priano V, Franchelli S, et al. (2011) Factors affecting symmetrization of the contralateral breast: a 7-year unilateral postmastectomy breast reconstruction experience. Aesthetic Plast Surg 35:446–451
Losken A, Carlson GW, Bostwick J, et al. (2002) Trends in unilateral breast reconstruction and management of the contralateral breast: the Emory experience. Plast Reconstr Surg 110:89–97
Vyas RM, Dickinson BP, Fastekjian JH, et al. (2008) Risk factors for abdominal donor-site morbidity in free flap breast reconstruction. Plast Reconstr Surg 121(5):1519–1526
Berry T, Brooks S, Sydow N, et al. (2010) Complication rates of radiation on tissue expander and autologous tissue breast reconstruction. Ann Surg Oncol 17(Suppl 3):202–210
Evans GR, Schusterman MA, Kroll SS, et al. (1995) Reconstruction and the radiated breast: is there a role for implants? Plast Reconstr Surg:1111–1115 discussion, 1116–1118
Williams JK, Carlson GW, Bostwick J, et al. (1997) The effects of radiation treatment after TRAM flap breast reconstruction. Plast Reconstr Surg 100:1153–1160
Rogers NE, Allen RJ (2002) Radiation effects on breast reconstruction with the deep inferior epigastric perforator flap. Plast Reconstr Surg 109:1919–1924 discussion 1925-1926
Kronowitz SJ, Robb GL (2004) Breast reconstruction and adjuvant therapies. Semin Plast Surg 18(2):105–115
Spear SL, Onyewu C (2000) Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg 105:930–942
Schwartz MD, Lerman C, Brogan B, et al. (2004) Impact of BRCA1/BRCA2 counseling and testing on newly diagnosed breast cancer patients. J Clin Oncol 22(10):1823–1829
Howard-Mcnatt M, Schroll RW, Hurt GJ, et al. (2011) Contralateral prophylactic mastectomy in breast cancer patients who test negative for BRCA mutations. Am J Surg 202:298–302
Weichman KE, Broer PN, Thanik VD, et al. (2015) Patient-reported satisfaction and quality of life following breast reconstruction in this patients: a comparison between microsurgical and prosthetic implant recipients. Plast Reconstr Surg 136(2):213–220
American Society of Plastic Surgeons (2014) Tracking operations and outcomes for plastic surgeons. https://tops.plasticsurgery.org/. Accessed 11 Mar 2014
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Shruti C. Tannan, Shawna R. Kleban, Wendy M. Novicoff, Chris A. Campbell declare that they have no conflict of interest.
Ethical standards
For this type of article formal consent from a local ethics committee is not required.
Funding
None
Rights and permissions
About this article
Cite this article
Tannan, S.C., Kleban, S.R., Novicoff, W.M. et al. The influence of plastic surgeon age and gender on decision-making in breast reconstruction: a national survey of American plastic surgeons. Eur J Plast Surg 40, 103–110 (2017). https://doi.org/10.1007/s00238-016-1229-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-016-1229-z