Abstract
Background
Achieving an aesthetic outcome following postmastectomy breast reconstruction is both an important goal for the patient and plastic surgeon. However, there is currently an absence of a widely accepted, standardized, and validated professional aesthetic assessment scale following postmastectomy breast reconstruction.
Methods
A systematic review was performed to identify all articles that provided professional assessment of the aesthetic outcome following postmastectomy, implant- or autologous tissue-based breast reconstruction. A modified version of the Scientific Advisory Committee’s Medical Outcomes Trust (MOT) criteria was used to evaluate all professional aesthetic assessment scales identified by our systematic review. The criteria included conceptual framework formation, reliability, validity, responsiveness, interpretability, burden, and correlation with patient-reported outcomes.
Results
A total of 120 articles were identified: 52 described autologous breast reconstruction, 37 implant-based reconstruction, and 29 both. Of the 12 different professional aesthetic assessment scales that exist in the literature, the most commonly used scale was the four-point professional aesthetic assessment scale. The highest score on the modified MOT criteria was assigned to the ten-point professional aesthetic assessment scale. However, this scale has limited clinical usefulness due to its poor responsiveness to change, lack of interpretability, and wide range of intra- and inter-rater agreements (Veiga et al. in Ann Plast Surg 48(5):515–520, 2002).
Conclusions
A “gold standard” professional aesthetic assessment scale needs to be developed to enhance the comparability of breast reconstruction results across techniques, surgeons, and studies to aid with the selection of procedures that produce the best aesthetic results from both the perspectives of the surgeon and patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breast reconstruction has become an important part of the surgical care for breast cancer patients.1 Breast reconstruction with a satisfactory aesthetic outcome can have a positive effect on the psychological recovery of the patient following mastectomy.2,3 A standardized measure of aesthetic outcome after reconstruction would enable comparisons of breast reconstruction outcomes for clinical and research purposes. A previous review by Potter et al. failed to identify a well-accepted, standardized, and validated aesthetic assessment scale following postmastectomy breast reconstruction.4 Numerous criteria have been proposed for what constitutes the ideal professional aesthetic assessment scale for breast reconstruction.5–8 Munshi et al. noted that the ideal professional aesthetic assessment scale should be based on quantitative measures that are easy to understand, reproducible, and have a good correlation with the patient-reported outcome (PRO).6 Potter et al. proposed that the core outcomes for assessing aesthetics involve a multidisciplinary approach, and that in addition to meeting the minimal validity and reliability criteria applied to other measurement systems, there would be an additional PRO domain to capture the perspective of the patient.4
Because a large number of professional aesthetic assessment scales currently exist for breast reconstruction, and there is no one ideal measurement tool, choosing the optimal professional aesthetic scale is challenging. A professional aesthetic assessment scale was defined as a scale to evaluate the aesthetic result by a healthcare professional.4 The goal of this paper, therefore, was to review systematically all of the existing aesthetic assessment scales by healthcare professionals for breast reconstruction. In addition, we are the first group to evaluate all the professional aesthetic assessment scales using well-established quality criteria for measurement properties.
Methods
Search and Selection Process
A computerized bibliographic search was performed in AMED, CINAHL, Cochrane, EMBASE, MEDLINE, PsychINFO, and PubMed in February of 2013. Search items were: (breast reconstruction OR mammoplasty) AND (aesthetic OR esthetic OR cosme*), and the search was limited to English articles published in 1990 or after. Duplicates were removed and two independent reviewers included articles evaluating patients undergoing postmastectomy breast reconstruction, both implant-based, and autologous reconstruction based on title and abstract. The two independent reviewers were Saskia Maass (first author) and Toni Zhong (senior author). Excluded were articles with no primary data, expert opinions, letters to the editor, and conference reports. For the second selection, articles were evaluated based on their full-text and were excluded when they did not contain a professional aesthetic assessment scale or only contained a patient-reported aesthetic assessment. Discrepancies between review authors were solved by reaching consensus. References of the articles were hand-searched to identify additional relevant papers.
Data Extraction
Included papers were reviewed for the following data: (1) study population, (2) type of reconstruction, (3) profession of the observer, (4) method of evaluation, and (5) the characteristics of the assessment scale. If insufficient information about the professional aesthetic assessment scale was provided, then the cited references were evaluated for additional information.
Medical Outcomes Trust Criteria to Evaluate each Professional Aesthetic Assessment Scale
To determine the methodological quality of each aesthetic assessment tool, both reviewers evaluated each aesthetic assessment scale using the Medical Outcomes Trust (MOT) criteria developed by the Scientific Advisory Committee (SAC).9–15 All methodological information was obtained directly from papers that first described the scales as well as from the papers that subsequently used and evaluated the scales. Each professional aesthetic assessment scale was graded according to the seven MOT criteria. One point was assigned when the aesthetic assessment scale fulfilled the criterion, half a point was given when most of the criterion was met, and zero points were assigned when the scale did not meet the criterion. Six out of the 7 criteria were based on the original MOT criteria and these included: (1) the underlying conceptual framework, (2) reliability, (3) validity, (4) responsiveness, (5) interpretability, and (6) burden for the professional and the patient. The conceptual framework criterion reflects the process of development of the scale. One point was assigned if this was clearly developed for patients undergoing postmastectomy breast reconstruction. Reliability refers to the degree to which scores reflect the underlying phenomenon. Both the intraclass correlation coefficient (ICC), which determines the degree of concordance between test and retest, and the internal consistency measured by the Cronbach’s alpha are common statistics for reliability.16 For research purposes, a measure should achieve a reliability coefficient of at least 0.70.17 One point was assigned for a kappa higher than 0.40 or a coefficient above 0.70. Validity is the degree to which an instrument measures what it is purported to measure. An aesthetic assessment scale with a Spearman ρ > 0.70 was assigned 1 point. Responsiveness is the ability of an instrument to distinguish clinically important changes from measurement error over time even if these changes are small, and this is measured by the responsiveness ratio (RR).10,18 When the RR was at minimum 1.96, this criterion was assigned a point. Interpretability is defined as the degree to which one can assign qualitative meaning to quantitative scores.9 One point was assigned if information was given on the means and standard deviation of the population. The burden for professional and patient evaluates the overall time burden. One point was assigned when burden was deemed to be low from the professional and patient. A seventh criterion is to assess the relationship between the professional aesthetic assessment scale and PRO as advocated by Potter et al., and 1 point was assigned when the correlation was >0.71.4 Because all the aesthetic outcome scales were described in English only, and we are only evaluating those scales intended for professional assessment, the two additional criteria of the MOT “alternatives modes of administration” and “cultural and language adaptations or translations” were found not to be applicable in our review. Table 1 provides a summary of the seven modified MOT criteria used.
Results
Search Results
A total of 5,845 citations were generated from the database search, and of these 3,214 duplicates were excluded, leaving a number of 2,631 articles. Based on the titles and abstracts, articles that did not evaluate patients undergoing postmastectomy breast reconstruction were excluded. Also excluded were records with no primary data, expert opinions, letters to the editor, and conference reports; this totaled 1,753 citations. The full-text of 878 articles was reviewed and 763 articles were excluded, because they did not use a professional aesthetic assessment scale. An additional 5 articles were found after reviewing the full text and references. A total number of 120 articles were included in the review. The search and selection process is summarized in Fig. 1.
Study Characteristics
(1) Study population: From the 120 articles selected, 95 described outcomes exclusively following breast reconstruction, 13 included only outcomes following breast-conserving therapy (BCT), and 12 contained both breast reconstruction and BCT.
(2) Type of reconstruction: Fifty-two articles included only patients following autologous breast reconstruction, 37 included implant-based reconstructions, 29 included both autologous and implant-based reconstruction, and 2 articles did not specify the reconstruction method.
(3) Observer: The aesthetic assessment was performed exclusively by plastic surgeons in 65 studies, whereas another 39 studies contained assessments by other medical professionals, such as nurses, residents, fellows, and other house-staff. Fifteen of the reviewed articles used a combination of professionals and nonprofessionals to perform the aesthetic assessments. The profession of the observer was unknown in 19 articles.
(4) Professional aesthetic assessment scale: For 67 articles, the aesthetic assessment was performed by means of photographs, 9 were based on clinical assessments, 8 were based on both clinical and photographic assessments, and 36 studies failed to state details. Table 2 presents an overview of the current professional aesthetic assessment scales used in each study, organized from most to least commonly used.19
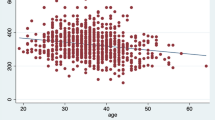
(5) Specific characteristics of the professional aesthetic assessment scales: The number of properties per scale varied from 1 to 12 items, with a median of 4 properties for all the reviewed articles. These specific properties included: shape, overall aesthetics, symmetry, volume, scars, inframammary fold, nipple-areola complex, contour, position, areola, color, consistency, ptosis, mobility, and rippling. Of all the articles that we reviewed, a total of 48 articles included a measure of patient satisfaction with the professional aesthetic assessment scale (Fig. 2).
MOT Criteria
Table 3 presents the summary of our evaluation of the 12 professional aesthetic assessment scales as prescribed by the MOT and the score that we assigned to each of the 7 modified MOT criteria. The four-point professional aesthetic assessment scale is the most commonly used method of aesthetic evaluation. The ten-point scoring scale fulfills over four of the seven criteria ascribed by the MOT. Below is a more detailed description of each of the 12 professional aesthetic assessment scales with respect to its adherence to the modified MOT criteria.
Four-Point Scale
This scale has not been validated in the breast reconstruction population.20 The reliability of the four-point scale was modest, with an inter-rater agreement κ of 0.55.21 Its validity has not been proven, and the Spearman coefficient for the postoperative scoring has been found to be 0.57.22 The weighted kappa to calculate the intraobserver agreement was 0.70 according to Vrieling et al.21 The correlation with the patient’s assessment was analyzed by Schuster et al. and found to be good.23 A score of 3 out of 7 was assigned.
Five-Point Scale
The reliability measured with the inter-rater agreement was good, the validation of the scale was fair, and the questionnaire burden is low.24 The total score was 2 out of 7.
Garbay/Lowery Scale
The Garbay assessment scale has been analyzed in detail by Lowery and often is referred to as the Lowery scale.8,25 Lowery et al. assessed the reliability and found kappa values from 0.19 to 0.63.21 The intra-rater agreement kappa values were from 0.21 to 0.67 for the subscales. Carlson et al. found inter-rater agreement kappa values from 0.31 to 0.72.26 The total was 2 out of 7 points.
Three-Point Scale
The reliability, validity, responsiveness, and correlation with the patients’ assessment have not been tested. One point out of 7 was assigned for low questionnaire burden.
Baker Scale
The Baker scale was intended to assess capsular contractures for patients after augmentation mammoplasty.27 Spear and Baker et al. modified the capsular contracture scale in 1995 for patients who had implant-based breast reconstruction.28 Spearman correlation coefficient was calculated to evaluate the correlation between the professional’s and patient’s scores, which was 0.40 and considered low.29,30 The scale was assigned 1 out of 7 points for low questionnaire burden.
Ten-Point Scale
Visser et al. showed an inter-rater agreement for the ten-point scale of 0.848.31 Validity tested using the Spearman coefficient ranged from 0.70–0.83. Veiga found an inter-rater agreement from 0.17 to 1.00; the intra-rater agreement ranged from 0.06 to 0.80.1 Five articles described a significant or close correlation between the patient aesthetic assessment scores and the evaluation by professionals.3,29,31–33 The total score was 4.5 out of 7.
Harris Scale
This professional aesthetic assessment scale also is referred to as the Rose or Harvard scale.34–36 It was developed to monitor the effects or radiotherapy on the aesthetic outcome in BCT patients, and not for postmastectomy breast reconstruction. The inter-rater agreement was 0.66 as found by Preuss et al.37 The total score was 2 out of 7 for low burden and good correlation with PRO.
Linear Numeric Analogue Score
Song et al. evaluated the 0–100 linear numeric analogue scale.38 The inter-rater agreement ranged from 0.23 to 0.38, the Cronbach α was 0.89, and the intra-rater agreement was 0.81.38,39 Salgarello et al. found a close correlation between the patients’ and professional assessment of the aesthetic outcome.40 The score was 4 out of 7.
Two-Point Scale
A two-point scale was used by Chawla et al. to score the aesthetic assessment either as good-excellent or fair-poor.41 The total score was 1 out of 7 points for low burden.
Six-Point Scale
A six-point scale scored 1 point for low burden of use.
Cohen Scale
Cohen et al. developed and statistically analyzed the Cohen Scale.7 The inter-rater agreement was κ 0.0–0.39, the Cronbach was α 0.92, and the intra-rater agreement was κ 0.25 to 0.66.21,42 There was a moderate correlation with the patient assessment; the Spearman coefficient was 0.36–0.53.22 The total score was 3 out of 7.
Seven-Point Scale
The inter-rater agreement of a seven-point scale with 6 subscales had a κ that ranged from 0.36 to 0.56.43 The total score was 1 out of 7.
Discussion
Our systematic review of 120 published articles identified 12 different aesthetic assessment scales by professionals for breast reconstruction. The common deficiencies shared by all the existing professional aesthetic assessment scales include their limited responsiveness and interpretability. Both of these attributes are important requirements in a clinically useful measurement tool. In other words, for the aesthetic assessment to be clinically relevant, it needs to be responsive to detect possible changes in the breast reconstruction aesthetic outcome over time. Furthermore, the numerical grading from the professional aesthetic assessment scale should lend qualitative meaning and provide information on what change in score would be considered clinically meaningful. In addition, the lack of an existing criterion standard for a subjective phenomenon, such as aesthetic outcome makes assessment of validity challenging. Of the 12 different professional aesthetic assessment scales that we evaluated, the ten-point professional aesthetic assessment scale was found to have the most rigorous measurement properties.9 The strengths are the significant correlation with the patient aesthetic evaluation, and the scale’s validity demonstrated by a high Spearman coefficient of 0.70–0.83.3,29,31–33 The primary weaknesses associated with this scale are the wide range of inter-rater agreements (0.17–1.0) and intra-rater agreements (0.06–0.80).1
Ideal Professional Aesthetic Assessment Scale
It is important to have a single reliable and responsive professional aesthetic assessment scale to measure aesthetic outcomes following breast reconstruction that is validated in this population, and supported by PRO. The development of this ideal aesthetic assessment tool would enhance the comparability of breast reconstruction results across techniques, surgeons, and studies to aid with the selection of procedures that produce the best aesthetic results. The ideal aesthetic assessment scale or “gold standard” for the professional aesthetic evaluation after breast reconstruction should ideally adhere to all seven of the modified MOT criteria.9
1. Conceptual framework formation: The professional aesthetic assessment scale should be at least analyzed for patients undergoing breast reconstruction after mastectomy.
2 and 4. Reliability and responsiveness: Both the inter-rater and intra-rater agreement of the scale should at least have a fair to good agreement. Fortin et al. recommends a panel of three evaluators for the evaluation of the aesthetic outcome.44
3. Validity: The validity of the ideal professional aesthetic assessment scale should be analyzed and have good correlation for all criteria.
5. Interpretability: The quantitative value on the assessment scale should have qualitative meaning, and the developers of the scale should provide information about what change scores should be considered clinically meaningful.45
6. Burden: The scale should pose a low burden on both the patient and the professional.6
7. Patient assessment: The scale should have a good agreement with the patient assessment of the aesthetic outcome.7
Limitation
To improve inter-rater agreement, all assessment scales should ideally be performed by healthcare professionals with the same level of expertise. However, as demonstrated by our review, healthcare professional is a widely used term, from an unknown observer with unknown experience, to an experienced plastic surgeon. This has shown to lead to different results.46 Furthermore, in some studies the assessor was the operating surgeon, which could lead to significant bias. Another significant limitation of our review was that only 18 of the 120 articles that we reviewed actually provided methodological information on the aesthetic assessment scales that were used.
Conclusions
Of the 12 different professional aesthetic assessment scales, the ten-point professional aesthetic assessment scale was found to have the highest quality as evaluated by the modified version of the MOT criteria set by SAC.9 However, this scale has limited clinical usefulness due to its poor responsiveness to change, lack of interpretability, and wide range of intra- and inter-rater agreements.1 A “gold standard” professional aesthetic assessment scale needs to be developed to enhance the comparability of breast reconstruction results across techniques, surgeons, and studies to aid with the selection of procedures that produce the best aesthetic results from both the perspectives of the surgeon and patients.
References
Veiga DF, Neto MS, Garcia EB, et al. Evaluations of the aesthetic results and patient satisfaction with the late pedicled TRAM flap breast reconstruction. Ann Plast Surg. 2002;48(5):515–20.
Eltahir Y, Werners LL, Dreise MM, et al. Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg. 2013;132(2):201e–9e.
Haekens CM, Enajat M, Keymeulen K, Van der Hulst RR. Self-esteem and patients’ satisfaction after deep inferior epigastric perforator flap breast reconstruction. Plast Surg Nurs. 2011;31(4):160–6.
Potter S, Harcourt D, Cawthorn S, et al. Assessment of cosmesis after breast reconstruction surgery: a systematic review. Ann Surg Oncol. 2011;18(3):813–23.
Kim MS, Sbalchiero JC, Reece GP, Miller MJ, Beahm EK, Markey MK. Assessment of breast aesthetics. Plast Reconstr Surg. 2008;121(4):186e–94e.
Munshi A, Kakkar S, Bhutani R, Jalali R, Budrukkar A, Dinshaw KA. Factors influencing cosmetic outcome in breast conservation. Clin Oncol (R Coll Radiol). 2009;21(4):285–93.
Cohen M, Evanoff B, George LT, Brandt KE. A subjective rating scale for evaluating the appearance outcome of autologous breast reconstruction. Plast Reconstr Surg. 2005;116(2):440–9.
Lowery JC, Wilkins EG, Kuzon WM, Davis JA. Evaluations of aesthetic results in breast reconstruction: an analysis of reliability. Ann Plast Surg. 1996;36(6):601–6; discussion 607.
Lohr KN, Aaronson NK, Alonso J, et al. Evaluating quality-of-life and health status instruments: development of scientific review criteria. Clin Ther. 1996;18(5):979–92.
Terwee CB, Bot SD, de Boer MR, et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42.
Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002;11(3):193–205.
Andresen EM. Criteria for assessing the tools of disability outcomes research. Arch Phys Med Rehabil. 2000;81(12 Suppl 2):S15–20.
McDowell I. Measuring health: a guide to rating scales and questionnaires. Oxford: Oxford University Press; 2006.
Lundberg M, Grimby-Ekman A, Verbunt J, Simmonds MJ. Pain-related fear: a critical review of the related measures. Pain Res Treat. 2011;2011:494196.
Cano SJ, Browne JP, Lamping DL, Roberts AH, McGrouther DA, Black NA. The Patient Outcomes of Surgery-Head/Neck (POS-head/neck): a new patient-based outcome measure. J Plast Reconstr Aesthet Surg. 2006;59(1):65–73.
Streiner DL, Norman GR. Health measurement scales: a practical guide to their development and use. Oxford: Oxford University Press; 2008.
Nunnally J, Bernstein I. Psychometric theory, 3rd edn. New York: McGraw-Hill; 1994.
Guyatt GH, Deyo RA, Charlson M, Levine MN, Mitchell A. Responsiveness and validity in health status measurement: a clarification. J Clin Epidemiol. 1989;42(5):403–8.
Baxter NN, Rothenberger DA, Lowry AC. Measuring fecal incontinence. Dis Colon Rectum. 2003;46(12):1591–605.
Vrieling C, Collette L, Bartelink E, et al. Validation of the methods of cosmetic assessment after breast-conserving therapy in the EORTC “boost versus no boost” trial. EORTC Radiotherapy and Breast Cancer Cooperative Groups. European Organization for Research and Treatment of Cancer. Int J Radiat Oncol Biol Phys. 1999;45(3):667–76.
Fleiss JL. Statistical methods for rates and proportions. 2nd edn. New York: Wiley; 1981.
Siegel S, Castellan NJ. Nonparametric statistics for the behavioral sciences. New York: McGraw-Hill; 1988.
Schuster RH, Kuske RR, Young VL, Fineberg B. Breast reconstruction in women treated with radiation therapy for breast cancer: cosmesis, complications, and tumor control. Plast Reconstr Surg. 1992;90(3):445-52; discussion 453–4.
Thomson HJ, Potter S, Greenwood RJ, et al. A prospective longitudinal study of cosmetic outcome in immediate latissimus dorsi breast reconstruction and the influence of radiotherapy. Ann Surg Oncol. 2008;15(4):1081–91.
Garbay JR, Rietjens M, Petit JY. Esthetic results of breast reconstruction after amputation for cancer. 323 cases. J Gynecol Obstet Biol Reprod (Paris). 1992;21(4):405–12.
Carlson GW, Losken A, Moore B, et al. Results of immediate breast reconstruction after skin-sparing mastectomy. Ann Plast Surg. 2001;46(3):222–8.
Baker DG, Leith JT. Protection of the skin of mice against irradiation with cyclotron-accelerated helium ions by 2-mercaptoethylamine. Acta Radiol Ther Phys Biol. 1975;14(6):561–71.
Spear SL, Baker JL, Jr. Classification of capsular contracture after prosthetic breast reconstruction. Plast Reconstr Surg. 1995;96(5):1119–23; discussion 1124.
Ramon Y, Ullmann Y, Moscona R, et al. Aesthetic results and patient satisfaction with immediate breast reconstruction using tissue expansion: a follow-up study. Plast Reconstr Surg. 1997;99(3):686–91.
Mukaka MM. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71.
Visser NJ, Damen TH, Timman R, Hofer SO, Mureau MA. Surgical results, aesthetic outcome, and patient satisfaction after microsurgical autologous breast reconstruction following failed implant reconstruction. Plast Reconstr Surg. 2010;126(1):26–36.
Gui GP, Tan SM, Faliakou EC, Choy C, A’Hern R, Ward A. Immediate breast reconstruction using biodimensional anatomical permanent expander implants: a prospective analysis of outcome and patient satisfaction. Plast Reconstr Surg. 2003;111(1):125–38; discussion 139–40.
Nicholson RM, Leinster S, Sassoon EM. A comparison of the cosmetic and psychological outcome of breast reconstruction, breast conserving surgery and mastectomy without reconstruction. Breast. 2007;16(4):396–410.
Rose MA, Olivotto I, Cady B, et al. Conservative surgery and radiation therapy for early breast cancer. Long-term cosmetic results. Arch Surg. 1989;124(2):153–7.
Harris JR, Levene MB, Svensson G, Hellman S. Analysis of cosmetic results following primary radiation therapy for stages I and II carcinoma of the breast. Int J Radiat Oncol Biol Phys. 1979;5(2):257–61.
Harris JR. Breast-conserving therapy as a model for creating new knowledge in clinical oncology. Int J Radiat Oncol Biol Phys. 1996;35(4):641–8.
Preuss J, Lester L, Saunders C. BCCT.core—can a computer program be used for the assessment of aesthetic outcome after breast reconstructive surgery? Breast. 2012;21(4):597–600.
Song AY, Fernstrom MH, Scott JA, Ren DX, Rubin JP, Shestak KC. Assessment of TRAM aesthetics: the importance of subunit integration. Plast Reconstr Surg. 2006;117(1):15–24.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8.
Salgarello M, Farallo E. Immediate breast reconstruction with definitive anatomical implants after skin-sparing mastectomy. Br J Plast Surg. 2005;58(2):216–22.
Chawla AK, Kachnic LA, Taghian AG, Niemierko A, Zapton DT, Powell SN. Radiotherapy and breast reconstruction: complications and cosmesis with TRAM versus tissue expander/implant. Int J Radiat Oncol Biol Phys. 2002;54(2):520–6.
Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334.
Gahm J, Edsander-Nord A, Jurell G, Wickman M. No differences in aesthetic outcome or patient satisfaction between anatomically shaped and round expandable implants in bilateral breast reconstructions: a randomized study. Plast Reconstr Surg. 2010;126(5):1419–27.
Fortin AJ, Cheang M, Latosinsky S. Cosmetic outcomes following breast conservation therapy: in search of a reliable scale. Breast Cancer Res Treat. 2006;100(1):65–70.
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15.
Munhoz AM, Montag E, Arruda EG, et al. The role of the lateral thoracodorsal fasciocutaneous flap in immediate conservative breast surgery reconstruction. Plast Reconstr Surg. 2006;117(6):1699–710.
Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124(2):345–53.
Al-Ghazal SK, Blamey RW. Subcutaneous mastectomy with implant reconstruction: cosmetic outcome and patient satisfaction. Eur J Surg Oncol. 2000;26(2):137–41.
Bacilious N, Cordeiro PG, Disa JJ, Hidalgo DA. Breast reconstruction using tissue expanders and implants in Hodgkin’s patients with prior mantle irradiation. Plast Reconstr Surg. 2002;109(1):102–7.
Bassiouny MM, Maamoun SI, El-Shazly Sel D, Youssef OZ. TRAM flap for immediate post mastectomy reconstruction: comparison between pedicled and free transfer. J Egypt Natl Canc Inst. 2005;17(4):231–8.
Crisera CA, Chang EI, Da Lio AL, Festekjian JH, Mehrara BJ. Immediate free flap reconstruction for advanced-stage breast cancer: is it safe? Plast Reconstr Surg. 2011;128(1):32–41.
Delay E, Gratadour AC, Jorquera F, Zlatoff P, Bremond A. Immediate autologous latissimus breast reconstruction after skin sparing mastectomy. Eur J Plast Surg. 1999;22(2/3):111–8.
Delay E, Jorquera F, Pasi P, Gratadour AC. Autologous latissimus breast reconstruction in association with the abdominal advancement flap: a new refinement in breast reconstruction. Ann Plast Surg. 1999;42(1):67–75.
Denewer A, Setit A, Farouk O. Outcome of pectoralis major myomammary flap for post-mastectomy breast reconstruction: extended experience. World J Surg. 2007;31(7):1382–6.
Disa JJ, McCarthy CM, Mehrara BJ, Pusic AL, Cordeiro PG. Immediate latissimus dorsi/prosthetic breast reconstruction following salvage mastectomy after failed lumpectomy/irradiation. Plast Reconstr Surg. 2008;121(4):159e–64e.
Drucker-Zertuche M, Robles-Vidal C. A 7 year experience with immediate breast reconstruction after skin sparing mastectomy for cancer. Eur J Surg Oncol. 2007;33(2):140–6.
Drucker-Zertuche M, Bargallo-Rocha E, Zamora-Del RR. Radiotherapy and immediate expander/implant breast reconstruction: should reconstruction be delayed? Breast J. 2011;17(4):365–70.
Fan LJ, Jiang J, Yang XH, et al. A prospective study comparing endoscopic subcutaneous mastectomy plus immediate reconstruction with implants and breast conserving surgery for breast cancer. Chin Med J (Engl). 2009;122(24):2945–50.
Fayman MS, Potgieter E, Becker PJ. The pedicle tram flap: a focus on improved aesthetic outcome. Aesthetic Plast Surg. 2006;30(3):301–8.
Fersis N, Hoenig A, Relakis K, Pinis S, Wallwiener D. Skin-sparing mastectomy and immediate breast reconstruction: incidence of recurrence in patients with invasive breast cancer. Breast. 2004;13(6):488–93.
Hidalgo DA. Aesthetic refinement in breast reconstruction: complete skin-sparing mastectomy with autogenous tissue transfer. Plast Reconstr Surg. 1998;102(1):63–70; discussion 71–2.
Ho AL, Tyldesley S, Macadam SA, Lennox PA. Skin-sparing mastectomy and immediate autologous breast reconstruction in locally advanced breast cancer patients: a UBC perspective. Ann Surg Oncol. 2012;19(3):892–900.
Kroll SS, Baldwin B. A comparison of outcomes using three different methods of breast reconstruction. Plast Reconstr Surg. 1992;90(3):455–62.
Kroll SS, Schusterman MA, Reece GP, Miller MJ, Smith B. Breast reconstruction with myocutaneous flaps in previously irradiated patients. Plast Reconstr Surg. 1994;93(3):460–9; discussion 470–1.
Kroll SS, Coffey JA, Jr., Winn RJ, Schusterman MA. A comparison of factors affecting aesthetic outcomes of TRAM flap breast reconstructions. Plast Reconstr Surg. 1995;96(4):860–4.
Kronowitz SJ, Robb GL, Youssef A, et al. Optimizing autologous breast reconstruction in thin patients. Plast Reconstr Surg. 2003;112(7):1768–78.
Kronowitz SJ, Feledy JA, Hunt KK, et al. Determining the optimal approach to breast reconstruction after partial mastectomy. Plast Reconstr Surg. 2006;117(1):1–11; discussion 12–4.
Kuske RR, Schuster R, Klein E, Young L, Perez CA, Fineberg B. Radiotherapy and breast reconstruction: clinical results and dosimetry. Int J Radiat Oncol Biol Phys. 1991;21(2):339–46.
Mosahebi A, Ramakrishnan V, Gittos M, Collier DS. Envelope mastectomy and immediate reconstruction (EMIR), improving outcome without oncological compromise. J Plast Reconstr Aesthet Surg. 2006;59(10):1025–30.
Mosahebi A, Ramakrishnan V, Gittos M, Collier J. Aesthetic outcome of different techniques of reconstruction following nipple-areola-preserving envelope mastectomy with immediate reconstruction. Plast Reconstr Surg. 2007;119(3):796–803.
Munhoz AM, Aldrighi C, Montag E, et al. Optimizing the nipple-areola sparing mastectomy with double concentric periareolar incision and biodimensional expander-implant reconstruction: aesthetic and technical refinements. Breast. 2009;18(6):356–67.
Munhoz AM, Aldrighi C, Montag E, et al. Periareolar skin-sparing mastectomy and latissimus dorsi flap with biodimensional expander implant reconstruction: surgical planning, outcome, and complications. Plast Reconstr Surg. 2007;119(6):1637–49; discussion 1650–2.
Noguchi M, Saito Y, Mizukami Y, et al. Breast deformity, its correction, and assessment of breast conserving surgery. Breast Cancer Res Treat. 1991;18(2):111–8.
Noguchi M, Saito Y, Taniya T, et al. Wide resection with latissimus dorsi muscle transposition in breast conserving surgery. Surg Oncol. 1992;1(3):231–6.
Noguchi M, Earashi M, Ohta N, et al. Mastectomy with and without immediate breast reconstruction using a musculocutaneous flap. Am J Surg. 1993;166(3):279–83.
Noguchi M, Minami M, Earashi M, et al. Oncologic and cosmetic outcome in patients with breast cancer treated with wide excision, transposition of adipose tissue with latissimus dorsi muscle, and axillary dissection followed by radiotherapy. Breast Cancer Res Treat. 1995;35(2):163–71.
Papp C, Wechselberger G, Schoeller T. Autologous breast reconstruction after breast-conserving cancer surgery. Plast Reconstr Surg. 1998;102(6):1932–6; discussion 1937–8.
Roostaeian J, Pavone L, Da Lio A, Lipa J, Festekjian J, Crisera C. Immediate placement of implants in breast reconstruction: patient selection and outcomes. Plast Reconstr Surg. 2011;127(4):1407–16.
Roostaeian J, Sanchez I, Vardanian A, et al. Comparison of immediate implant placement versus the staged tissue expander technique in breast reconstruction. Plast Reconstr Surg. 2012;129(6):909e–18e.
Spear SL, Onyewu C. Staged breast reconstruction with saline-filled implants in the irradiated breast: recent trends and therapeutic implications. Plast Reconstr Surg. 2000;105(3):930–42.
Spear SL, Ducic I, Low M, Cuoco F. The effect of radiation on pedicled TRAM flap breast reconstruction: outcomes and implications. Plast Reconstr Surg. 2005;115(1):84–95.
Spear SL, Newman MK, Bedford MS, Schwartz KA, Cohen M, Schwartz JS. A retrospective analysis of outcomes using three common methods for immediate breast reconstruction. Plast Reconstr Surg. 2008;122(2):340–7.
Spear SL, Schwarz KA, Venturi ML, Barbosa T, Al-Attar A. Prophylactic mastectomy and reconstruction: clinical outcomes and patient satisfaction. Plast Reconstr Surg. 2008;122(1):1–9.
Spear SL, Slack C, Howard MA. Postmastectomy reconstruction of the previously augmented breast: diagnosis, staging, methodology, and outcome. Plast Reconstr Surg. 2001;107(5):1167–76.
Tallet AV, Salem N, Moutardier V, et al. Radiotherapy and immediate two-stage breast reconstruction with a tissue expander and implant: complications and esthetic results. Int J Radiat Oncol Biol Phys. 2003;57(1):136–42.
Tzafetta K, Ahmed O, Bahia H, Jerwood D, Ramakrishnan V. Evaluation of the factors related to postmastectomy breast reconstruction. Plast Reconstr Surg. 2001;107(7):1694–701.
Vrieling C, Collette L, Fourquet A, et al. The influence of patient, tumor and treatment factors on the cosmetic results after breast-conserving therapy in the EORTC ‘boost vs. no boost’ trial. EORTC Radiotherapy and Breast Cancer Cooperative Groups. Radiother Oncol. 2000;55(3):219–32.
Clough KB, Cuminet J, Fitoussi A, Nos C, Mosseri V. Cosmetic sequelae after conservative treatment for breast cancer: classification and results of surgical correction. Ann Plast Surg. 1998;41(5):471–81.
Clough KB, O’Donoghue JM, Fitoussi AD, Vlastos G, Falcou MC. Prospective evaluation of late cosmetic results following breast reconstruction: II. Tram flap reconstruction. Plast Reconstr Surg. 2001;107(7):1710–6.
Cordeiro PG, McCarthy CM. A single surgeon’s 12-year experience with tissue expander/implant breast reconstruction: part II. An analysis of long-term complications, aesthetic outcomes, and patient satisfaction. Plast Reconstr Surg. 2006;118(4):832–9.
Elton C, Jones SE, Jones PA. Initial experience of intramammary prostheses in breast conservation surgery. Eur J Surg Oncol. 1999;25(2):138–41.
Evans AA, Straker VF, Rainsbury RM. Breast reconstruction at a district general hospital. J R Soc Med. 1993;86(11):630–3.
Hayes AJ, Jenkins MP, Sandhu SS, Baum M. Subpectoral breast reconstruction using the biodimensional system. Ann R Coll Surg Engl. 1997;79(5):355–60.
Lossing C, Elander A, Gewalli F, Holmstrom H. The lateral thoracodorsal flap in breast reconstruction: a long-term follow up study. Scand J Plast Reconstr Surg Hand Surg. 2001;35(2):183–92.
McCarthy CM, Pusic AL, Disa JJ, McCormick BL, Montgomery LL, Cordeiro PG. Unilateral postoperative chest wall radiotherapy in bilateral tissue expander/implant reconstruction patients: a prospective outcomes analysis. Plast Reconstr Surg. 2005;116(6):1642–7.
McKeown DJ, Hogg FJ, Brown IM, Walker MJ, Scott JR, Weiler-Mithoff EM. The timing of autologous latissimus dorsi breast reconstruction and effect of radiotherapy on outcome. J Plast Reconstr Aesthet Surg. 2009;62(4):488–93.
Moran SL, Nava G, Behnam AB, Serletti JM. An outcome analysis comparing the thoracodorsal and internal mammary vessels as recipient sites for microvascular breast reconstruction: a prospective study of 100 patients. Plast Reconstr Surg. 2003;111(6):1876–82.
Nano MT, Gill PG, Kollias J, Bochner MA. Breast volume replacement using the latissimus dorsi miniflap. ANZ J Surg. 2004;74(3):98–104.
Nano MT, Gill PG, Kollias J, Bochner MA, Malycha P, Winefield HR. Psychological impact and cosmetic outcome of surgical breast cancer strategies. ANZ J Surg. 2005;75(11):940–7.
Raja MA, Straker VF, Rainsbury RM. Extending the role of breast-conserving surgery by immediate volume replacement. Br J Surg. 1997;84(1):101–5.
Ringberg A, Tengrup I, Aspegren K, Palmer B. Immediate breast reconstruction after mastectomy for cancer. Eur J Surg Oncol. 1999;25(5):470–6.
Spear SL, Parikh PM, Reisin E, Menon NG. Acellular dermis-assisted breast reconstruction. Aesthetic Plast Surg. 2008;32(3):418–25.
Carlson GW, Page AL, Peters K, Ashinoff R, Schaefer T, Losken A. Effects of radiation therapy on pedicled transverse rectus abdominis myocutaneous flap breast reconstruction. Ann Plast Surg. 2008;60(5):568–72.
Denewer A, Setit A, Hussein O, Farouk O. Skin-sparing mastectomy with immediate breast reconstruction by a new modification of extended latissimus dorsi myocutaneous flap. World J Surg. 2008;32(12):2586–92.
Denewer A, Farouk O. Can nipple-sparing mastectomy and immediate breast reconstruction with modified extended latissimus dorsi muscular flap improve the cosmetic and functional outcome among patients with breast carcinoma? World J Surg. 2007;31(6):1169–77.
Gerber B, Krause A, Dieterich M, Kundt G, Reimer T. The oncological safety of skin sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction: an extended follow-up study. Ann Surg. 2009;249(3):461–8.
Gerber B, Krause A, Reimer T, et al. Skin-sparing mastectomy with conservation of the nipple-areola complex and autologous reconstruction is an oncologically safe procedure. Ann Surg. 2003;238(1):120–7.
Giacalone PL, Rathat G, Daures JP, Benos P, Azria D, Rouleau C. New concept for immediate breast reconstruction for invasive cancers: feasibility, oncological safety and esthetic outcome of post-neoadjuvant therapy immediate breast reconstruction versus delayed breast reconstruction: a prospective pilot study. Breast Cancer Res Treat. 2010;122(2):439–51.
Li FC, Jiang HC, Li J. Immediate breast reconstruction with implants after skin-sparing mastectomy: a report of 96 cases. Aesthetic Plast Surg. 2010;34(6):705–10.
Mori H, Umeda T, Osanai T, Hata Y. Esthetic evaluation of immediate breast reconstruction after nipple-sparing or skin-sparing mastectomy. Breast Cancer. 2005;12(4):299–303.
Omranipour R, Bobin JY, Esouyeh M. Skin-sparing mastectomy and immediate breast reconstruction (SSMIR) for early breast cancer: eight years single institution experience. World J Surg Oncol. 2008;6:43.
Salgarello M, Visconti G, Barone-Adesi L. Nipple-sparing mastectomy with immediate implant reconstruction: cosmetic outcomes and technical refinements. Plast Reconstr Surg. 2010;126(5):1460–71.
Yueh JH, Houlihan MJ, Slavin SA, Lee BT, Pories SE, Morris DJ. Nipple-sparing mastectomy: evaluation of patient satisfaction, aesthetic results, and sensation. Ann Plast Surg. 2009;62(5):586–90.
Berrino P, Campora E, Leone S, Zappi L, Nicosia F, Santi P. The transverse rectus abdominis musculocutaneous flap for breast reconstruction in obese patients. Ann Plast Surg. 1991;27(3):221–31.
Bogetti P, Cravero L, Spagnoli G, et al. Aesthetic role of the surgically rebuilt inframammary fold for implant-based breast reconstruction after mastectomy. J Plast Reconstr Aesthet Surg. 2007;60(11):1225–32.
Cordeiro PG, Pusic AL, Disa JJ, McCormick B, VanZee K. Irradiation after immediate tissue expander/implant breast reconstruction: outcomes, complications, aesthetic results, and satisfaction among 156 patients. Plast Reconstr Surg. 2004;113(3):877–81.
Di G-H, Yu K-D, Wu J, et al. Immediate breast reconstruction with latissimus dorsi musculocutaneous flap: A suitable option for Chinese women after mastectomy. Chin J Cancer Res. 2006 2006;18(2):5.
Dian D, Schwenn K, Mylonas I, Janni W, Jaenicke F, Friese K. Aesthetic result among breast cancer patients undergoing autologous breast reconstruction versus breast conserving therapy. Arch Gynecol Obstet. 2007;275(6):445–50.
Enajat M, Rozen WM, Whitaker IS, Smit JM, Van Der Hulst RR, Acosta R. The deep inferior epigastric artery perforator flap for autologous reconstruction of large partial mastectomy defects. Microsurgery. 2011;31(1):12–7.
Lee JW, Chang TW. Extended latissimus dorsi musculocutaneous flap for breast reconstruction: experience in Oriental patients. Br J Plast Surg. 1999;52(5):365–72.
Tomita K, Yano K, Matsuda K, Takada A, Hosokawa K. Esthetic outcome of immediate reconstruction with latissimus dorsi myocutaneous flap after breast-conservative surgery and skin-sparing mastectomy. Ann Plast Surg. 2008;61(1):19–23.
Ueda S, Tamaki Y, Yano K, et al. Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery. 2008;143(3):414–25.
Ziswiler-Gietz J, Makrodimou M, Harder Y, Banic A, Erni D. Outcome analysis of breast reconstruction with free transverse rectus abdominis musculocutaneous (TRAM) flaps. Swiss Med Wkly. 2008;138(7-8):114–20.
Gendy RK, Able JA, Rainsbury RM. Impact of skin-sparing mastectomy with immediate reconstruction and breast-sparing reconstruction with miniflaps on the outcomes of oncoplastic breast surgery. Br J Surg. 2003;90(4):433–9.
Adams WP, Jr., Rios JL, Smith SJ. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: six-year prospective clinical study. Plast Reconstr Surg. 2006;117(1):30–6.
Aristei C, Falcinelli L, Bini V, et al. Expander/implant breast reconstruction before radiotherapy: outcomes in a single-institute cohort. Strahlenther Onkol. 2012;188(12):1074–9.
Behranwala KA, Dua RS, Ross GM, Ward A, A’Hern R, Gui GP. The influence of radiotherapy on capsule formation and aesthetic outcome after immediate breast reconstruction using biodimensional anatomical expander implants. J Plast Reconstr Aesthet Surg. 2006;59(10):1043–51.
De Lorenzi F, Lohsiriwat V, Barbieri B, et al. Immediate breast reconstruction with prostheses after conservative treatment plus intraoperative radiotherapy. long term esthetic and oncological outcomes. Breast. 2012;21(3):374–9.
Rietjens M, De Lorenzi F, Venturino M, Petit JY. The suspension technique to avoid the use of tissue expanders in breast reconstruction. Ann Plast Surg. 2005;54(5):467–70.
Castello JR, Garro L, Najera A, Mirelis E, Sanchez-Olaso A, Barros J. Immediate breast reconstruction in two stages using anatomical tissue expansion. Scand J Plast Reconstr Surg Hand Surg. 2000;34(2):167–71.
Cocquyt VF, Blondeel PN, Depypere HT, et al. Better cosmetic results and comparable quality of life after skin-sparing mastectomy and immediate autologous breast reconstruction compared to breast conservative treatment. Br J Plast Surg. 2003;56(5):462–70.
Hayes AJ, Garner JP, Nicholas W, Laidlaw IJ. A comparative study of envelope mastectomy and immediate reconstruction (EMIR) with standard latissimus dorsi immediate breast reconstruction. Eur J Surg Oncol. 2004;30(7):744–9.
Hernanz F, Regano S, Redondo-Figuero C, Orallo V, Erasun F, Gomez-Fleitas M. Oncoplastic breast-conserving surgery: analysis of quadrantectomy and immediate reconstruction with latissimus dorsi flap. World J Surg. 2007;31(10):1934–40.
Anderson PR, Hanlon AL, Fowble BL, McNeeley SW, Freedman GM. Low complication rates are achievable after postmastectomy breast reconstruction and radiation therapy. Int J Radiat Oncol Biol Phys. 2004;59(4):1080–7.
Baschnagel AM, Shah C, Wilkinson JB, Dekhne N, Arthur DW, Vicini FA. Failure rate and cosmesis of immediate tissue expander/implant breast reconstruction after postmastectomy irradiation. Clin Breast Cancer. 2012;12(6):428–32.
Bassiouny M, El-Marakby HH, Saber N, Zayed SB, Shokry A. Quadrantectomy and nipple saving mastectomy in treatment of early breast cancer: feasibility and aesthetic results of adjunctive latissmus dorsi breast reconstruction. J Egypt Natl Canc Inst. 2005;17(3):149–57.
Cassileth L, Kohanzadeh S, Amersi F. One-stage immediate breast reconstruction with implants: a new option for immediate reconstruction. Ann Plast Surg. 2012;69(2):134–8.
Zaha H, Onomura M, Nomura H, Umekawa K, Oki M, Asato H. Free omental flap for partial breast reconstruction after breast-conserving surgery. Plast Reconstr Surg. 2012;129(3):583–7.
Fernandez Delgado JM, Martinez-Mendez JR, de Santiago J, Hernandez-Cortes G, Casado C. Immediate breast reconstruction (IBR) with direct, anatomic, extra-projection prosthesis: 102 cases. Ann Plast Surg. 2007;58(1):99–104.
Hudson DA, Skoll PJ. Single-stage, autologous breast restoration. Plast Reconstr Surg. 2001;108(5):1163–71; discussion 1172–3.
Margulies AG, Hochberg J, Kepple J, Henry-Tillman RS, Westbrook K, Klimberg VS. Total skin-sparing mastectomy without preservation of the nipple-areola complex. Am J Surg. 2005;190(6):907–12.
Sacchini V, Pinotti JA, Barros AC, et al. Nipple-sparing mastectomy for breast cancer and risk reduction: oncologic or technical problem? J Am Coll Surg. 2006;203(5):704–14.
Spear SL, Davison SP. Aesthetic subunits of the breast. Plast Reconstr Surg. 2003;112(2):440–7.
Eriksen C, Lindgren EN, Frisell J, Stark B. A prospective randomized study comparing two different expander approaches in implant-based breast reconstruction: one stage versus two stages. Plast Reconstr Surg. 2012;130(2):254e–64e.
Edsander-Nord A, Brandberg Y, Wickman M. Quality of life, patients’ satisfaction, and aesthetic outcome after pedicled or free TRAM flap breast surgery. Plast Reconstr Surg. 2001;107(5):1142–53; discussion 1154–5.
Gahm J, Jurell G, Edsander-Nord A, Wickman M. Patient satisfaction with aesthetic outcome after bilateral prophylactic mastectomy and immediate reconstruction with implants. J Plast Reconstr Aesthet Surg. 2010;63(2):332–8.
Cohen BE, Casso D, Whetstone M. Analysis of risks and aesthetics in a consecutive series of tissue expansion breast reconstructions. Plast Reconstr Surg. 1992;89(5):840–3; discussion 844–5.
Lindegren A, Halle M, Docherty Skogh AC, Edsander-Nord A. Postmastectomy breast reconstruction in the irradiated breast: a comparative study of DIEP and latissimus dorsi flap outcome. Plast Reconstr Surg. 2012;130(1):10–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maass, S.W.M.C., Bagher, S., Hofer, S.O.P. et al. Systematic Review: Aesthetic Assessment of Breast Reconstruction Outcomes by Healthcare Professionals. Ann Surg Oncol 22, 4305–4316 (2015). https://doi.org/10.1245/s10434-015-4434-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4434-2