Abstract
Purpose
This review article aims to discuss the pathophysiology, clinical presentation, and neuroimaging of cerebral venous thrombosis (CVT). Different approaches for diagnosis of CVT, including CT/CTV, MRI/MRV, and US will be discussed and the reader will become acquainted with imaging findings as well as limitations of each modality. Lastly, this exhibit will review the standard of care for CVT treatment and emerging endovascular options.
Methods
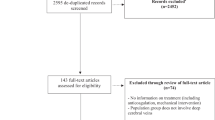
A literature search using PubMed and the MEDLINE subengine was completed using the terms “cerebral venous thrombosis,” “stroke,” and “imaging.” Studies reporting on the workup, imaging characteristics, clinical history, and management of patients with CVT were included.
Results
The presentation of CVT is often non-specific and requires a high index of clinical suspicion. Signs of CVT on NECT can be divided into indirect signs (edema, parenchymal hemorrhage, subarachnoid hemorrhage, and rarely subdural hematomas) and less commonly direct signs (visualization of dense thrombus within a vein or within the cerebral venous sinuses). Confirmation is performed with CTV, directly demonstrating the thrombus as a filling defect, or MRI/MRV, which also provides superior characterization of parenchymal abnormalities. General pitfalls and anatomic variants will also be discussed. Lastly, endovascular management options including thrombolysis and mechanical thrombectomy are discussed.
Conclusions
CVT is a relatively uncommon phenomenon and frequently overlooked at initial presentation. Familiarity with imaging features and diagnostic work-up of CVT will help in providing timely diagnosis and therapy which can significantly improve outcome and diminish the risk of acute and long-term complications, optimizing patient care.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Background
Cerebral venous thrombosis (CVT) is an uncommon condition that accounts for 0.5 to 1% of all strokes in the adult population [1]. It is frequently underdiagnosed, as clinical manifestations are not specific and include a wide range of symptoms such as headache, focal neurological deficits, seizures, and altered mental status [2]. Therefore, high clinical suspicion is required to avoid misdiagnosis, and imaging is fundamental in accurately detecting CVT and possible associated complications that could modify the prognosis and the therapeutic approach [1, 3]. The diagnosis of CVT can be challenging because of the diversity of the underlying risk factors, variable clinical presentation, and non-specific imaging findings on initial routine head computed tomography (CT). Prompt diagnosis is essential as it can lead to a more effective treatment, whereas a delayed recognition of this condition is often associated with high morbidity and mortality [3, 4].
There are numerous imaging techniques that can be used to detect CVT, such as non-enhanced head CT (NECT), CT venography (CTV), magnetic resonance imaging (MRI), MR venography (MRV), ultrasound (US), and angiography. Angiography was previously considered the gold standard; however, the contemporary utility is often limited to cases where thrombolysis is required, having been largely replaced by CTV, MRI, and MRV as the modern gold standard [2, 3, 5]. Ultimately each imaging modality has different advantages, and specific investigations should be tailored to the clinical suspicion, taking into account the individual characteristics of each patient [2].
The aim of this work is to review the cerebral venous anatomy, the epidemiology, and clinical manifestations of CVT and to analyze the associated imaging features within various modalities including NECT, CTV, MRI, MRV, US, and angiography. In addition, the advantages and pitfalls of each imaging technique will be compared to provide a general guideline to help radiologists in the selection of the most appropriate investigatory tool in each specific case. This will be followed by an overview of treatment options for CVT, including endovascular techniques.
Risk factors and epidemiology of CVT
According to a recent population-based study, the estimated incidence of CVT in adults is 13 cases per million population per year, comparative to bacterial meningitis. This incidence is higher than previous reports, presumably due to advances within the imaging techniques during recent decades [6]. Based on the Canadian Pediatric Ischemic Stroke Registry data, CVT was previously believed to be more frequent in the pediatric population than in adults; however, the incidence of CVT in adults has recently been found to be twice those in children [6]. CVT in adult demographics tends to have a younger age of presentation relative to other types of strokes, as it most commonly occurs between the ages of 20–50, occurring infrequently in patients older than 65. There is also a female predominance (2.9:1) due to gender-related factors involved in the pathophysiology of CVT [5, 6].
There is a large number of predisposing risk factors that play an important role in the development of CVT [5]. These include all parameters that influence the composition of blood, specifically those that can induce an alteration in the vascular endothelium or blood stasis can attribute to CVT (Virchow triad) [1, 3, 5]. These factors include pro-thrombotic conditions (genetic or acquired), autoimmune diseases, oral contraceptive use, hormonal replacement therapy, puerperium or pregnancy states, dehydration (particularly in the pediatric population), cardiac failure, head trauma, intracranial tumors, malignancy (particularly hematological diseases), and infections [1, 5, 7]. Frequently, CVT occurs due to a combination of inherent individual risk factors and acquired precipitants; nevertheless, 20–35% of the cases are idiopathic [5, 8, 9].
Clinical manifestations
The clinical presentation of CVT is highly variable and often non-specific, attributing to a delayed diagnosis [1]. Moreover, symptoms may vary due to differing degrees of venous hypertension, recanalization, and concomitant thrombosis, causing fluctuations in clinical presentation [3, 10]. Common signs and symptoms include as follows: headache, which is the most frequent presenting symptom (i.e., 75–95% of patients), papilledema, seizures, focal neurological deficits, and altered mental status. Other symptoms described during the onset of CVT include occipital and neck pain that are generally associated with sigmoid sinus involvement [5, 11]. Acute (i.e., < 2 days), subacute (i.e., 2 days to 1 month), and chronic presentation (i.e., > 1 month) are seen in 30, 50, and 20% of patients, respectively [8, 12]. The clinical presentation may vary depending on the extent of the thrombosis, on the structures involved and on concurrent clinical circumstances [1, 11]. Furthermore, certain risk factors such as pregnancy, thrombosis of a large sinus, and hypertension at presentation are associated with intracerebral hemorrhage and with poor prognosis [13].
CVT should be considered in the differential diagnosis of patients with idiopathic intracranial hypertension, in cases of severe unexplained headache, and in young patients presenting with stroke symptoms, due to the overlapping clinical presentation of these conditions [1, 2]. For example, up to 40% of the patients with CVT present with headache and papilledema, which are commonly described with intracranial hypertension [14]. Since the presentation of CVT ranges from asymptomatic or non-specific symptoms such as headache to focal neurological deficits and comatose states, it should be considered during most if not all neuroimaging tests [1, 2].
It is not certain that the different phases of CVT correlate well with patient management and outcome. The timing for the management of CVT is different than that of arterial ischemia, which usually occurs within 1–2 weeks after onset of symptoms. Rather, it is mainly the severity of the venous congestion and mass effect from parenchymal swelling, edema, and hemorrhage that inflict the major damage.
Cerebral venous anatomy
The clinical presentation and outcome of CVT depend on the location and extent of the thrombosis, as well as on the presence of functional collateral circulation [1, 3]. CVT is cited to occur in multiple locations in up to 90% of patients, with frequent involvement of the contiguous sigmoid and transverse sinuses [15]. Thus, a familiarity with the major routes of drainage and anatomic variants is imperative to accurately identify CTV [3].
The cerebral venous system includes the deep venous system and the superficial venous system [16]. The superficial venous system drains into the dural sinuses and shows a significant anatomic variability. Despite this morphological and topological variability, the anatomic origins from which they derive are relatively constant (Fig. 1).
Axial and oblique illustrations demonstrate the major dural venous sinuses and deep cerebral veins. It is important to be familiar with the major routes of drainage and anatomic variations, such as differences in size of sinuses between the left and right sides for accurate interpretation of CT or MR venography
The deep venous system drains the hemispheric white matter and comprises the medullary and subependymal veins, the vein of Rosenthal, the internal cerebral veins, the vein of Galen, and their tributaries (Fig. 2). This system is responsible for the venous drainage of the thalamus, basal ganglia, upper brainstem, upper brainstem, corpus callosum, and the deep white matter of the parietal, temporal, and frontal lobes. The thalamic tributaries drain directly into the internal cerebral veins; therefore, the thalamus is commonly affected when there is parenchymal involvement secondary to CVT of the deep venous system [17]. Finally, the cavernous sinus is connected with the basal dural sinuses, and the sigmoid sinus and jugular bulb connect with numerous emissary channels in the skull base [8].
The site and extent of parenchymal lesions secondary to CVT depend on the vein or veins affected, extent of clot, and presence of collateral drainage pathways. The presence of hemorrhage or vasogenic edema in locations shown on the illustration, near a major venous sinus or deep cerebral vein, should raise suspicion for possibility of CVT
Material and methods
A literature search using PubMed and the MEDLINE subengine was completed using the terms “cerebral venous thrombosis,” “stroke,” and “imaging.” Studies reporting on the workup, imaging characteristics, clinical history, and management of patients with CVT were included.
Results
Diagnostic imaging approach to CVT
Neuroimaging plays a fundamental role in the diagnosis of CVT, thereby influencing the prognosis and outcome of the patient [11]. Radiological findings are diverse and contingent on the chosen imaging modality. Essentially, these findings can be divided into direct and indirect signs, depending on the capacity of demonstrating either the thrombus itself or illustrating associated findings such as intracranial hemorrhage or ischemia [11].
There are different imaging techniques that can be used in the diagnostic approach of CVT [3, 11]. NECT is widely used as the initial exam of choice for most patients with non-specific neurological symptoms, as it provides pertinent information with rapid acquisition time; therefore, it is often the first investigation performed on patients with CVT [4, 8]. Direct or indirect signs of venous thrombosis can be seen on NECT (with an estimated sensitivity of 64.6% and specificity of 97.2%). It is also useful to rule out intracranial hemorrhage. Moreover, it has a high sensitivity to detect ischemic changes, beyond demonstrating herniation syndromes and hydrocephalus [2, 4, 18]. However, neurovascular imaging (i.e., CTV or MRV) may be performed immediately after NECT if there is a strong clinical suspicion or the findings detected on routine NECT are highly suggestive of CVT [18].
Neurovascular techniques can confirm the diagnosis of CVT by demonstrating filling defects within the involved vessel, whereas routine NECT and MRI have a more limited diagnostic value as they may only show indirect signs of thrombosis, with varying presentation dependent on the stage of presentation [11, 19]. Both CTV and MRV are adequate vascular imaging modalities in the setting of CVT, and the decision on selecting the most appropriate option depends on numerous variables including the accessibility to the different equipment facilities and patient’s condition. The use of CTV is often reserved for situations where a more accurate CVT diagnosis is required; however, it is arguable that MRV with MRI may provide superior additional information including complications and associated findings that can modify the therapeutic approach and that may help to predict the prognosis [2, 8, 20, 21]. The advantages and disadvantages of each modality, as well as the direct and indirect signs of CVT, are discussed in Tables 1 and 2, respectively.
In practice, the radiological findings of CVT on CT and MRI are indirect and help to detect secondary complications, and complex cases may require the use of both modalities to reach an adequate evaluation of the patient. As aforementioned, catheter angiography was previously the gold standard in the diagnosis of CVT, but due to the improvement of other neuroimaging techniques during the last decades, it is now rarely required outside the context of endovascular treatment (Fig. 3) [5].
Imaging algorithm for work-up of CVT. Neurovascular imaging may be performed immediately if there is strong clinical suspicion for CVT or alternatively after suspicious findings on routine non-enhanced head CT (NECT). Both CTV and MRI with MRV are acceptable initial diagnostic modalities for evaluation of suspected CVT, depending on accessibility as well as the patient’s clinical status and stability for undergoing MRI. The advantages and disadvantages of each modality are discussed in a following table. The findings on CT and MRI partly complement one another and in complex cases both may be performed for optimal diagnostic evaluation. Given the potential pitfalls of MR and reliability of CTV, we suggest CTV for patients with papilledema or hyperdense SSS clot on NECT. For non-specific/low clinical suspicious cases, conventional CT can be used for reasons of cost and rapidity. Catheter angiography is rarely performed for diagnosis of CVT anymore but may be performed as a therapeutic intervention in rare cases of extensive thrombosis requiring endovascular treatment
Non-enhanced CT
Non-enhanced CT is the initial imaging modality of choice for patients with neurological complaints [2].
The classic feature of CVT in NECT is hyperattenuation of the affected venous sinus (Fig. 4); however, less than one third of CVT cases present with direct visualization of thrombus as it depends on the attenuation of the clot [4]. Thrombosis of the posterior aspect of the superior sagittal sinus may appear as a hyperattenuating triangle, what is known as a filled delta sign [1]. Occasionally, a superficial cord-like linear hyperdensity can be visualized to depict a thrombosed cortical vein (Fig. 5); this is commonly referred to as a “cord sign”; however, it is only seen in 5% of cases [3, 22].
Parenchymal abnormalities in CVT on CT and MRI obtained on the same day from a 38-year-old female patient. The NECT images (a, b) demonstrate lobar hemorrhage in the right parietal lobe extending to junction with temporal lobe with a dense SSS (arrow) highly suspicious for CVT. MRI has much greater sensitivity for parenchymal abnormalities, and the FLAIR images (c, d) demonstrate additional mixed signal abnormalities secondary to vasogenic edema (arrows) not clearly visible on the CT. These are in non-contiguous locations involving multiple vascular territories and do not conform to any typical large arterial territory infarct. This combination of findings consisting of a mix of hemorrhage and vasogenic edema in this pattern is highly suspicious for CVT
Different CT appearances of clot and potential pitfalls on CTV. NECT images from a patient with CVT demonstrate very high density clot on day 1 (a; arrow) but less dense appearance of clot on day 6 in the same patient undergoing treatment (b; arrow). Based on the venogram alone, the acute clot mimics normally opacified sinus (c; arrow). Axial images obtained without (d) and with contrast (CTV) at the vertex from a patient with extensive CVT are shown and are almost indistinguishable, again demonstrating how dense acute clot may mimic opacified sinus. Note the dense thrombosed cortical veins on the NECT (arrows; cord sign). Two additional CT venogram images (f, g) are shown demonstrating the somewhat less dense appearance of subacute clot (arrow; f) enabling clear distinction from contrast at the level of torcular (equivalent of empty delta sign in the SSS) as well as hypodense appearance of late subacute to chronic clot in the right transverse sinus (arrow; g)
If a hyperdense sinus is identified, further investigation with CTV and/or MRI/MRV should be performed [3]. Measurement of the venous sinus density and Hounsfield unit-to-hematocrit (H:H) ratio has been proven to increase the sensitivity in diagnosing CVT, as attenuation of 62 HU and higher is suggestive of thrombosis [4].
It is important to consider that in the majority of cases NECT will only show indirect signs of CVT such as diffuse brain edema or intracerebral hemorrhage [1]. Diffuse brain edema (seen in 50% of cases) can secondarily cause decrease of the ventricular size and effacement of cerebral sulci; this finding may be difficult to distinguish from normally small ventricles in young adults [8]. However, in some cases, the ventricular size may be increased due to hydrocephalus resulting from increased CSF production and decreased resorption from increased venous pressure. In both cases, comparison with prior examinations may be necessary to detect the subtle acute change. Indirect (e.g., juxtacortical edema) signs occur more commonly, though not exclusively, when thrombosis extends to cortical veins. Among the indirect signs of CVT in NECT, venous infarction is the most specific finding and may or may not be associated with intracerebral hemorrhage [8]. This is identified most commonly when there is a hypodense area that spans more than one arterial territory or spares the cortex with infarction of the adjacent subcortical white matter; the presence of multiple isolated lesions should also raise suspicion of venous infarction [8]. While a majority of infarctions will present with hemorrhage, edema without hemorrhage is seen is 8% of cases on CT [23,24,25,26]. The site and extent of parenchymal lesions secondary to CVT depend on the vessel affected, extent of the clot, and presence of collateral drainage pathways [8]. The presence of hemorrhage or edema near a major venous sinus or deep cerebral vein should raise suspicion of CVT [8]. For instance, intracerebral hemorrhage or edema in the internal capsule, thalami, or basal ganglia suggests deep venous CVT [3, 8]. On the other hand, parasagittal abnormality may suggest thrombosis of the sagittal sinus, and temporal lobe involvement usually occurs secondary to thrombosis of the vein of Labbe [8].
Contrast-enhanced CT (CECT) and CT venography (CTV)
The most readily touted advantage of CECT and CTV is their widespread availability. CECT is not usually performed when CVT is suspected, but it is usually used as a screening investigation for other clinical entities, leading to identification of thrombosis as an incidental finding [8]. CTV (as multidetector CT angiography, MDCTA) has recently been proven to be as accurate as time-of-flight (TOF) MRV [21, 27] in the visualization of the cerebral venous sinuses, with superior assessment of the inferior sagittal sinus and of the non-dominant transverse sinus [2]. It allows direct visualization of the thrombosed sinus as a filling defect [8].
CTV is less sensitive in the evaluation of the deep cerebral veins than in that of the cerebral venous sinuses; this can be improved by performing multiplanar reformations, which increases the sensitivity of CTV beyond angiography [2]. Maximum intensity projection (MIP) image generation occasionally suffers from inadvertent sinus exclusion from bone-subtracting algorithms; however, this can be improved with specific software for mask bone elimination (Fig. 6) [3].
CTV 3D reconstruction after bone mask extraction. Bone mask extraction algorithms may help to define the vascular structures without extracting those vessels that are adjacent to the skull base or calvarium. In this case, superior sagittal sinus thrombosis (arrow) was clearly demonstrated on CTV 3D images after bone extraction. Contamination by arterial structures is present, which can be ameliorated by bolus timing and algorithmic subtraction. Importantly, such contamination with contamination may relate itself to increased venous pressures
CECT and CTV provide both direct and indirect signs. The most common direct sign is a filling defect within a dural sinus, known as the “empty delta” sign [8]. This sign can manifest anytime from the acute to chronic phase, more often presenting between day 5 to 2 months after onset, and may be associated with development of collaterals which provide peripheral enhancement surrounding the filling defect [8]. In approximately 20% of cases, indirect signs secondary to dural hyperemia can be seen; these changes are related to collateral circulation and hemostasis, what is visualized as dural enhancement most commonly involving the falx cerebri and tentorium [8]. Additionally, gyral enhancement can eventually be seen extend into the white matter, what is more evident in CECT [8]. However, as many as 30% of CECT examinations will be falsely negative for CVT, and thus, dedicated CTV should be strongly considered when clinical suspicion is high [8, 21, 28]. In the context of cortical vein thrombosis, the resolution of CTV is superior to MRI, particularly for single-vein pathology.
MRI
Unenhanced MRI is a more sensitive technique for detecting CVT than NECT [3]. Patent dural sinuses can be seen as flow voids on MRI, and thus, venous thrombosis can often be visualized directly even without specific venogram sequences [8]. Usually, detection is more successful when the acquisition imaging plane is orthogonal to the blood flow trajectory [8]. For this reason, thrombosis of the sigmoid, sagittal, and transverse sinuses is better appreciated in coronal plane [8]. However, the parallel plane will be more useful in assessing the extent of thrombosis [8]. In the setting of superior sagittal sinus thrombosis, a sagittal T1-weighted image (T1WI) may demonstrate the thrombus extent as an area of high signal intensity (Fig. 7) (this is better seen in subacute thrombosis, when most of the clot contains methemoglobin that is intrinsically hyperintense on T1WI) [8].
Flow void absence or abnormal flow signal is a frequent sign of CVT in MRI, and assessment of the abnormal flow in different sequences is fundamental to confirm presence of CVT [3, 8]. The signal intensity of the clot is similar to a hematoma, showing the same evolving signal changes and expected age; the progressive intensity changes observed in the clot are related to the paramagnetic proprieties of the hemoglobin molecule and its secondary products [3, 8, 29]. Acute thrombus (first 5 days) may be isointense on T1WI and hypointense on T2-weighted image (T2WI), as it is rich in desoxyhemoglobin. This can lead to misdiagnosis as it is similar to normal flow [3]. Between days 6 and 15, the clot may appear hyperintense on T1WI and T2WI due to its high content in methemoglobin [3, 30]. After 15 days, the diagnosis of CVT may be challenging as chronic thrombosis shows partial recanalization and the signal of the clot is iso- to hyperintense on T2WI and isointense on T1WI; this can be overlooked [3, 23, 30, 31]. After 4 months, no signal abnormality is seen on T1WI or DWI; however, subtle changes can be seen in T2WI or FLAIR (Fig. 8) [32].
T2WI (a) and FLAIR (b) on axial and sagittal images, respectively, and 3D reconstructions of MRV with gadolinium (c, d). There is absence of flow void on the superior sagittal sinus (a), suggestive of venous sinus thrombosis. This abnormality was confirmed on FLAIR (b) that demonstrates an extensive hyperintense clot with absence of the expected flow void and a concave superior pituitary border which is commonly seen in increased intracranial pressure. These findings are confirmed on CE-MRV that showed a filling defect along the superior sagittal sinus (arrow) and prominent collateral circulation (c, d)
T2*-weighted gradient-recalled echo (GRE) images are extremely useful in detecting CVT, as deposited blood breakdown products (i.e., hemosiderin, methemoglobin, deoxyhemoglobin) can cause exaggerated signal drop-out, helping in depicting intraluminal thrombi in stages where the clot can be subtle in other sequences [3]. The majority of CVT cases show subacute thrombi at presentation, which fortunately has the most conspicuous characteristics (Fig. 9) [30]. GRE images also empower the radiologist as thrombus often exhibits significant susceptibility blooming artifact (Fig. 10). This can also be applied effectively to cortical vein thrombosis but may be ineffective for single-vein thrombosis. Small juxtacortical hemorrhage may also be identified in this way.
Axial ADC (a) and DWI (b) maps demonstrate mixed diffusion signal in the right parietal lobe. There is very cortical diffusion restriction (arrows) but elevated diffusion in adjacent subcortical matter. This pattern is highly atypical of arterial infarction and instead consistent with vasogenic edema syndrome as seen in CVT (c–d)
Gradient recalled echo (a) or susceptibility weighted images (b) can be very useful adjunctive sequences for demonstrating clots within dural venous sinuses or cortical veins. In a, there is blooming artifact from clot within the SSS and cortical veins. In b, there is extensive SSS and cortical vein thrombosis mixed with subarachnoid hemorrhage
SWI is a complementary T2* GRE sequence to evaluate CVT. The exaggeration of magnetic susceptibility effect (MSE) facilitates identification of subtle thrombosis, as it is present in 90% of cases, and it also shows venous stasis, collateral circulation, and possible associated intracranial hemorrhage [32, 33]. This is particularly useful in acute onset, when other sequences may not demonstrate the clot [33]. Additionally, SWI shows a blooming artifact better defined than regular T2* GRE sequences, allowing a more accurate localization of the clot or bleeding [33]. Isolated cortical vein thrombosis is uncommon and subtle and can be missed in most of MRI sequences [33]. These findings may be easier to see on the maximum-intensity projections (MIPs) of SWI compared to dedicated venous imaging [34].
Diffusion-weighted imaging techniques are useful in the detection of CVT, as hyperintensity with decreased apparent diffusion coefficient (ADC) has been described in approximately 41% of cases of sinus thrombosis [3]. Patients with restriction on DWI show longer recovery time and lower probability of complete thrombus recanalization. Findings on DWI therefore can be a prognostic factor [3, 35]. DWI also allows sensitive detection of edema, which can further be differentiated as cytotoxic edema by decreased ADC values and vasogenic edema with increased ADC values (Fig. 9) [31]. Edema as manifested by T2 hyperintensity is thought to not only relate to reversible venous congestion and pressure-driven interstitial edema but also can belie blood-brain-barrier breakdown, which can reflect a greater degree of venous hypertension. In the latter scenario, parenchymal enhancement can also be seen. The former occurs in the setting of cell death, whereas the latter proceeds from venous congestion. Even in the presence of cytotoxicity and hemorrhage, these changes are frequently reversible [24]. Parenchymal changes are most commonly associated with low ADC values, yet these patients can also experience resolution of edema in some cases [36].
The indirect findings on MRI are the same as those on CT, namely infarction with or without hemorrhage and brain swelling [8]. Swelling without any additional indirect sign may occur in nearly half of CVT cases [23], and therefore, the radiologist must be vigilant for sulcal effacement and reduction of the CSF spaces suggestive of cerebral edema [8]. MR is more sensitive than CT for the detection of parenchymal lesions [3, 37] and in particular, demonstrates focal edema in 25% of cases compared to 8% on CT [24,25,26]. Conventional MRI is sensitive to the parenchymal changes of CVT secondary to venous occlusion, such as thalamic edema. When these findings are observed, CTV or MRV should be performed to confirm the diagnosis [3].
MR venography
MRV is useful for not only documentation of thrombus but also assessment for recanalization following therapy and in the setting of chronic thrombosis with partial recanalization [8]. Complete recanalization is not required for symptomatic recovery, and the presence of collateral pathways may also be identified on MRV [3, 8, 10]. MRV may be performed without contrast using TOF technique or phase contrast technique or with contrast-enhanced technique. MRV with gadolinium allows for a direct assessment of luminal filling similar to that of CTV, with comparable sensitivity and specificity. Moreover, both CTV and contrast-enhanced MRV are superior to the TOF and phase contrast techniques, as complex flow can produce artifact in these sequences [38, 39]. TOF-MRV has a low sensitivity to small vessels with slow flow, limiting the assessment of the exam [2].
Nevertheless, TOF is still the most common technique used to identify CVT and is fundamental in certain clinical settings, such as pregnant or breastfeeding patients, as well as in case of severe renal failure. 2D TOF in particular is superior to its 3D counterpart due to a relative lack of saturation effects and superior sensitivity in the setting of slow flow (Fig. 11) [38]. One significant potential pitfall of 2D TOF is that same-plane acquisition can produce false positive results from saturation and subsequent signal nulling, as this technique is most sensitive to orthogonal flow. Intravascular gadolinium is not subject to this and furthermore is less affected by venous sinus turbulence compared to TOF [21, 38]. 3D phase contrast (PC) MRV may be employed to benefit as a result of improved ability to detect slow flow and may differentiate between slow flow and thrombus.
Static contrast-enhanced 3D MRV allows a better characterization of the intracranial venous anatomy; however, it may have limitation in chronic dural sinus thrombosis as the clot may enhance, simulating an opened sinus [19]. Therefore, time-resolved 3D MRV (4D MRV) can be used to obtain images with different delays for better depiction of the clot [19]. 4D MRV has higher sensitivity to detect CVT than T2WI, T2* GRE, and TOF MRV; moreover, it has higher specificity than TOF MRV, and it allows to detect chronic CVT [19]. A significant disadvantage of MRV compared to CTV is that acquisition times are long, and motion artifacts may occur in patients with low level of consciousness [2]. CTV and MRV are compared in Table 2.
Ultrasound
US should be considered as the initial test of choice when CVT is suspected in neonates and infants with opened fontanelles. It is a useful technique to not only demonstrate echogenic thrombus but also initially identify intracranial hemorrhage, cerebral edema, venous infarcts, hydrocephalus, and secondary leukomalacic changes [40]. Frequently, these findings are subsequently confirmed with MRI and MRV, as it is considered the gold standard technique [41]. US allows only limited assessment of brain parenchyma and depending on the size of the fontanelle, the area visualized may vary (Figs. 12 and 13) [42].
The presence of echogenic thrombus in intracranial veins, particularly within the midline venous structures owing to proximity to an open anterior or posterior fontanelle, or in the sigmoid and transverse sinuses visualized through the mastoid fontanelle, should be interpreted as CVT. Doppler US is helpful in detecting areas with absent or severely reduced blood flow and is also useful in monitoring CVT [40]. The complete extent of thrombosis and associated parenchymal changes are best assessed on MRI; however, US is a useful screening method to demonstrate brain edema and to rapidly assess for possible complications. It is important to consider that between one and two thirds of children may develop intraparenchymal lesions including intraparenchymal hemorrhage and ischemia [43]. Given the propensity towards normal physiologic enhancement in the inner dural border zone, investigation with Doppler US can troubleshoot equivocal cross-sectional cases and avoid unnecessary treatment.
Imaging pitfalls
As with many clinical indications, the detection of CVT is fraught with potential pitfalls. It is essential the radiologist be familiar with normal anatomic variants, ranging from normal filling defects such as intrasinus septa or arachnoid granulations, to occlusion mimics such as sinus duplication, occipital sinuses, and hypoplastic and atretic sinuses [44, 45]. Indeed, the transverse sinus may be completely or partially unpaired in up to 20% of cases and asymmetrical in nearly half [11]. Bearing in mind the limitations in any individual modality described above, it may be necessary to utilize multiple modalities or at the very least multiple sequences to troubleshoot findings. The pitfalls of various imaging modalities are illustrated in Table 3.
Unenhanced CT
The most common thrombosis mimic on unenhanced CT is increased attenuation of the blood within the venous structures, which can be seen in dehydration, polycythemia, or increased hematocrit ratio. It is worthwhile to mention that children may normally show hyperdense blood within patent dural sinuses and this should not be mistaken for thrombosis [3, 46]. In general, hyperdensity that affects all vessels equally rather than isolated vessels are likely to be related to systemic conditions and not thrombosis. Different densities between venous and arterial structures in NECT may be helpful in detecting CVT. A thrombosed vein should appear relatively hyperdense when compared to an artery; if there is a hemoconcentrated state that is increasing the density of the blood within the vessels, no global difference will be observed between arteries and veins [3, 46].
The most common distinguishing characteristics of a real venous thrombus are an asymmetric hyperdense vein, heterogeneity of the involved vessel, and an isolated area of dural sinus involvement [22]. With a mind to symmetry, hyperdense blood can also be distinguished from a subdural hematoma in this manner and additional favor can be given to CVT by correlating with the expected anatomic position of the dural sinuses. For instance, subdural hematoma will stay lateral to the boundary of the transverse sinus [22]. Challenging cases can be assessed with MR, where flow voids belie patent sinuses and MRV usually removes any doubt [3].
Importantly, direct sinus injury or secondary venous stasis can induce CVT in a patient with subdural hematoma [3]. Therefore, the presence of hyperdensity in the region of a dural sinus, particularly within the posterior fossa, may suggest concomitant CVT. It is worthy to mention that contrast material from a previous examination in the setting of slow venous flow is a possible CVT mimic, but such slow transit may also predispose to CVT [8].
Contrast-enhanced CT and CT venography
A split or fenestrated sinus and intrasinus septa may cause a filling defect indistinguishable from the classic empty delta sign, simulating a thrombus [22]. Moreover, this mimic is just as ambiguous on MRI and MRV. Therefore, is it imperative that these anatomical variants are considered during the assessment of the exam [8]. There are two situations that may lead to false-negative results in CECT and CTV. Acute thrombus that are spontaneously hyperattenuated (cord sign) could be misinterpreted for a patent enhanced vein in CTV; to avoid this pitfall, evaluation of NECT has to be performed together with the CTV images [2]. Additionally, chronic organized thrombus can enhance after contrast injection and may not demonstrate a filling defect [2].
MRI
There are several pitfalls to consider in the interpretation of MRI as they can affect the diagnosis of CVT [2]. Venous thrombosis may show a complex appearance with variable signal intensity, and expert radiological assessment might be required to appropriately detect the thrombus [2].
The seeming flow void of a patent sinus can be mimicked on T2-weighted MR by subacute hemorrhage, which can exhibit marked hypointensity. Conversely, a subacute thrombus that predominantly contains methemoglobin might simulate real flow on T1WI TOF MRV, or a patent sinus on gadolinium-enhanced exams due to its intrinsic hyperintensity on T1WI [2]. Slow flow may mimic occlusion and manifest as loss of flow void without a culprit thrombus [19]. If in doubt, this can be clarified with contrast enhanced images.
MR venography
TOF MR and other unenhanced techniques are susceptible to false-positive results from flow that has a parallel or complex direction with the acquisition plane [19]. Subacute and chronic thrombosis might not be apparent on MRI. To this end, a phase contrast study can be employed to detect the clot (Fig. 13) [19]. Stenotic, hypoplastic, or aplastic venous sinuses can mimic CVT on any modality, and this is more frequently seen in a patient who also possesses a hypoplastic jugular foramen. This may manifest on TOF MRV as a flow gap in the hypoplastic/aplastic sinus [3].
Particular care should be taken to interpreting TOF-MRV in isolation, as the physiologic alteration in flow in this area can lead to a loss of flow signal. Unenhanced MRI images will demonstrate no sign of thrombosis, and gadolinium-enhanced MR or CTV will show smooth enhancement and without filling defect [19]. Source images should be always analyzed to detect possible pitfalls that are not visible on 3D reconstructions.
All modalities
Pacchinionian granulations are arachnoid outpouchings that may mimic CVT and are a common incidental finding on brain imaging [3]. They are the most common filling defect in dural venous sinuses that may be misinterpreted as thrombus. They are often relatively round and adhere to one side of the wall of the dural venous sinuses. On contrast enhanced images, they may show central and inhomogeneous contrast enhancement [47].
Another potentially complicated scenario is of tumor compression of a venous sinus vs venous invasion [19]. While tumors undoubtedly mimic CVT by direct mass effect upon a venous sinus, this naturally may precipitate true CVT due to venous flow obstruction and stasis [19].
Subarachnoid hemorrhage can be a presentation of dural venous thrombosis, most commonly of the convexal type [48]. In such cases, careful review of the images may show abnormal signal in the lumen of the affected dural sinus, consistent with concurrent venous thrombus; other indirect signs such as venous infarctions may be present [2]. MRI and MRV can be used to confirm the presence of extensive dural sinus thrombosis by showing loss of flow void and filling defects [3].
Lastly, partial recanalization and partial thrombosis represent important pitfalls. The former is affected by poor agreement on degree of recanalization, but its presence is felt to have a classic appearance. Namely, they consist of muralized thrombus which is T2 hyperintense to gray matter and possess serpiginous intrathrombus flow void which enhances on post-contrast imaging. In the setting of partial occlusion, CTV is felt to be the most sensitive to the slow flow this state imparts. When detection by TOF is possible, overestimation is common; however, the technique may still be used.
Endovascular management
With respect to management of CVT, heparin continues to remain the gold standard treatment. In keeping with contemporary literature [49, 50], current recommendations from the European Federation of Neurological Societies endorses low molecular-weight heparin (LMWH) in the management of acute CVT [51]. Furthermore, a 2017 Cochrane review suggests that treatment with a LMWH or heparinoid following acute ischemic strokes may yield lower rates of deep vein thrombosis (DVT) relative to unfractionated heparin (UFH) [52]. Resultant outcomes in neurologic deficit and functional disability between LWMH and UFH appear to be equivalent [53].
Endovascular mechanical thrombectomy (EMT) such as suction (Fig. 14) and AngioJet thrombectomy as well as thrombolysis have arisen as viable options for medically-refractory CVT. In comparing EMT versus thrombolysis, a non-randomized study by Siddiqui et al. determined that when adjusting for admission neurological dysfunction, both treatment arms had comparable mortality, discharge neurological dysfunction, and intermediate to long-term morbidity [54]. When combining both interventions, research by Li and colleagues illustrated complete and partial recanalization rates of 87 and 6%, respectively, in patients with severe CVT [55]. Furthermore, a systematic review evaluating EMT with and without sinus thrombolysis in CVT, with AngioJet as the most common device, illustrated near-complete to complete recanalization in 74% of cases [56]. This is comparable to recent systematic reviews assessing concurrent use of both modalities, citing complete radiologic resolution of CVT in 69% of cases [57]. When evaluated independently, a systematic review of systemic thrombolysis in the management of CVT found that 88% of patients regained functional independence, with partial or complete recanalization rates and mortality rates of 61.5 and 7.7% of evaluated cases [58]. Ultimately, with systemic anticoagulation and concurrent endovascular treatment in 49% of evaluated cases, a 2017 study by Salottolo et al. demonstrated rates of successful recanalization and full recovery at 61 and 60%, respectively, with the authors suggesting hormonal etiology, history of migraine, and cerebral edema as indications in which favorable prognosis was more likely [59]. The degree of venous hypertension is likely an influencing factor in success of any form of CVT intervention.
Follow-up
Clinical information on recanalization and outcome is lacking, but individuals with previous CVT have greater risk for a new event relative to the general population. Moreover, documentation of recanalization and its degree may help to determine whether new neurological complaints relate to progression/recurrence. The AHA/ASA recommends an early follow-up CTV or MRV in patients with persisting or evolving symptoms and possibly a 3–6 month follow-up in stable patients. As pial fistula may occur following CVT, multiphasic imaging can be considered for new complaints. However, high-quality evidence is not available.
Conclusions
The key underlying pathophysiology of CVT is venous congestion/hypertension and the degree of elevated venous pressure. These factors influence the clinical presentation, abnormal imaging findings, treatment selection options, and the outcome of therapeutic intervention. The severity of venous congestion (from mild to severe) can be reflected by imaging, ranging from only brain swelling to parenchymal abnormalities, which may include edema, parenchymal hyperintensity, ischemia, and hemorrhage. Timely diagnosis of CVT requires a high index of suspicion and adequate neuroimaging examination to confirm the presence of venous thrombosis. Recognition of certain patterns of parenchymal abnormalities and hemorrhage that are distinct from other diseases is key for early recognition and work-up of CVT. Both CTV and MRI with MRV are excellent methods to diagnose CVT and to detect possible complications (Fig. 15). These techniques are also complementary and may be combined for optimal evaluation in complex or equivocal cases, including US in pediatric cases. MRI enables better delineation of parenchymal abnormalities compared to CT; however, NECT is usually the initial screening technique for patients presenting with non-specific complaints, as it is widely available and has short acquisition times. Familiarity with signs of CVT on conventional sequences is key for optimal evaluation and to avoid pitfalls that may be encountered by relying on the angiographic sequences alone.
Asterisk = right internal jugular vein. Black arrow = sigmoid sinus. White arrow = torcular herophili. a and b Source images of CTV. Thrombus in IJV and sigmoid sinus was seen as filling defect. Note the collateral veins (star) arising from the right IJV. c Sagittal planar reconstruction of CTV showed thrombus extending from right IJV into the sigmoid sinus, correlating well with conventional venography (Fig. 4e. d T1W MR image showed sigmoid sinus thrombosis, as loss of flow void. e Conventional venogram showed thrombus as filling defects. Note the collateral veins at the region of the right IJV, also shown by CTV. f Venography after suction thrombectomy showed improved patency in the right IVJ and lateral sinus
References
Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, Cushman M, deVeber G, Ferro JM, Tsai FY, on behalf of the American Heart Association Stroke Council and the Council on Epidemiology and Prevention (2011) Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42:1158–1192. https://doi.org/10.1161/STR.0b013e31820a8364
Linn J, Ertl-Wagner B, Seelos KC, Strupp M, Reiser M, Brückmann H, Brüning R (2007) Diagnostic value of multidetector-row CT angiography in the evaluation of thrombosis of the cerebral venous sinuses. AJNR Am J Neuroradiol 28:946–952
Leach JL, Fortuna RB, Jones BV, Gaskill-Shipley MF (2006) Imaging of cerebral venous thrombosis: current techniques, spectrum of findings, and diagnostic pitfalls. Radiographics 26:S19–S41. https://doi.org/10.1148/rg.26si055174
Buyck P-J, De Keyzer F, Vanneste D, Wilms G, Thijs V, Demaerel P (2013) CT density measurement and H:H ratio are useful in diagnosing acute cerebral venous sinus thrombosis. Am J Neuroradiol 34:1568–1572. https://doi.org/10.3174/ajnr.A3469
Coutinho JM (2015) Cerebral venous thrombosis. J Thromb Haemost 13:S238–S244. https://doi.org/10.1111/jth.12945
Coutinho JM, Zuurbier SM, Aramideh M, Stam J (2012) The incidence of cerebral venous thrombosis: a cross-sectional study. Stroke 43:3375–3377. https://doi.org/10.1161/STROKEAHA.112.671453
Stam J (2003) Cerebral venous and sinus thrombosis: incidence and causes. Adv Neurol 92:225–232
Poon CS, Chang J-K, Swarnkar A, Johnson MH, Wasenko J (2007) Radiologic diagnosis of cerebral venous thrombosis: pictorial review. Am J Roentgenol 189:S64–S75. https://doi.org/10.2214/AJR.07.7015
van Gijn J (2009) Cerebral venous thrombosis: pathogenesis, presentation and prognosis. J R Soc Med 93:230–233. https://doi.org/10.1177/014107680009300504
Leach JL, Wolujewicz M, Strub WM (2007) Partially recanalized chronic dural sinus thrombosis: findings on MR imaging, time-of-flight MR venography, and contrast-enhanced MR venography. AJNR Am J Neuroradiol 28:782–789
Chiewvit P, Piyapittayanan S, Poungvarin N (2011) Cerebral venous thrombosis: diagnosis dilemma. Neurol Int 3:e13. https://doi.org/10.4081/ni.2011.e13
Masuhr F, Mehraein S, Einhaupl K (2004) Cerebral venous and sinus thrombosis. J Neurol 251:11–23. https://doi.org/10.1007/s00415-004-0321-7
Kumral E, Polat F, Uzunkopru C, Calli C, Kitis O (2012) The clinical spectrum of intracerebral hematoma, hemorrhagic infarct, non-hemorrhagic infarct, and non-lesional venous stroke in patients with cerebral sinus-venous thrombosis. Eur J Neurol 19:537–543. https://doi.org/10.1111/j.1468-1331.2011.03562.x
Bousser MG (2000) Cerebral venous thrombosis: diagnosis and management. J Neurol 247:252–258. https://doi.org/10.1007/s004150050579
Soleau SW, Schmidt R, Stevens S, Osborn A, MacDonald JD (2003) Extensive experience with dural sinus thrombosis. Neurosurgery 52:534–544 discussion 542-534
Simonds GR, Truwit CL (1994) Anatomy of the cerebral vasculature. Neuroimaging Clin N Am 4:691–706
Oka K, Rhoton AL Jr, Barry M, Rodriguez R (1985) Microsurgical anatomy of the superficial veins of the cerebrum. Neurosurgery 17:711–748. https://doi.org/10.1227/00006123-198511000-00003
Roland T, Jacobs J, Rappaport A, Vanheste R, Wilms G, Demaerel P (2010) Unenhanced brain CT is useful to decide on further imaging in suspected venous sinus thrombosis. Clin Radiol 65:34–39. https://doi.org/10.1016/j.crad.2009.09.008
Meckel S, Reisinger C, Bremerich J, Damm D, Wolbers M, Engelter S, Scheffler K, Wetzel SG (2010) Cerebral venous thrombosis: diagnostic accuracy of combined, dynamic and static, contrast-enhanced 4D MR venography. AJNR Am J Neuroradiol 31:527–535. https://doi.org/10.3174/ajnr.A1869
Lee SK, terBrugge KG (2003) Cerebral venous thrombosis in adults: the role of imaging evaluation and management. Neuroimaging Clin N Am 13:139–152. https://doi.org/10.1016/S1052-5149(02)00095-3
Ozsvath RR, Casey SO, Lustrin ES, Alberico RA, Hassankhani A, Patel M (1997) Cerebral venography: comparison of CT and MR projection venography. AJR Am J Roentgenol 169:1699–1707. https://doi.org/10.2214/ajr.169.6.9393193
Provenzale JM, Kranz PG (2011) Dural sinus thrombosis: sources of error in image interpretation. Am J Roentgenol 196:23–31. https://doi.org/10.2214/AJR.10.5323
Tsai FY, Wang AM, Matovich VB, Lavin M, Berberian B, Simonson TM, Yuh WT (1995) MR staging of acute dural sinus thrombosis: correlation with venous pressure measurements and implications for treatment and prognosis. AJNR Am J Neuroradiol 16:1021–1029
Yoshikawa T, Abe O, Tsuchiya K, Okubo T, Tobe K, Masumoto T, Hayashi N, Mori H, Yamada H, Aoki S, Ohtomo K (2002) Diffusion-weighted magnetic resonance imaging of dural sinus thrombosis. Neuroradiology 44:481–488. https://doi.org/10.1007/s00234-002-0772-4
Lovblad KO, Bassetti C, Schneider J, Ozdoba C, Remonda L, Schroth G (2000) Diffusion-weighted MRI suggests the coexistence of cytotoxic and vasogenic oedema in a case of deep cerebral venous thrombosis. Neuroradiology 42:728–731. https://doi.org/10.1007/s002340000395
Bergui M, Bradac GB, Daniele D (1999) Brain lesions due to cerebral venous thrombosis do not correlate with sinus involvement. Neuroradiology 41:419–424. https://doi.org/10.1007/s002340050775
Liauw L, van Buchem MA, Spilt A, de Bruïne FT, van den Berg R, Hermans J, Wasser MNJM (2000) MR angiography of the intracranial venous system. Radiology 214:678–682. https://doi.org/10.1148/radiology.214.3.r00mr41678
Wetzel SG, Kirsch E, Stock KW, Kolbe M, Kaim A, Radue EW (1999) Cerebral veins: comparative study of CT venography with intraarterial digital subtraction angiography. AJNR Am J Neuroradiol 20:249–255
Kajtazi NI, Zimmerman VA, Arulneyam JC, Al-Shami SY, Al-Senani FM (2009) Cerebral venous thrombosis in Saudi Arabia. Clinical variables, response to treatment, and outcome. Neurosciences (Riyadh) 14:349–354
Bergui M, Bradac GB (2003) Clinical picture of patients with cerebral venous thrombosis and patterns of dural sinus involvement. Cerebrovasc Dis 16:211–216. https://doi.org/10.1159/000071118
Walecki J, Mruk B, Nawrocka-Laskus E, Piliszek A, Przelaskowski A, Sklinda K (2015) Neuroimaging of cerebral venous thrombosis (CVT)—old dilemma and the new diagnostic methods. Pol J Radiol 80:368–373. https://doi.org/10.12659/PJR.894386
Idbaih A, Boukobza M, Crassard I, Porcher R, Bousser MG, Chabriat H (2006) MRI of clot in cerebral venous thrombosis: high diagnostic value of susceptibility-weighted images. Stroke 37:991–995. https://doi.org/10.1161/01.STR.0000206282.85610.ae
Mittal S, Wu Z, Neelavalli J, Haacke EM (2009) Susceptibility-weighted imaging: technical aspects and clinical applications. Part 2. AJNR Am J Neuroradiol 30:232–252. https://doi.org/10.3174/ajnr.A1461
Majoie CB, van Straten M, Venema HW, den Heeten GJ (2004) Multisection CT venography of the dural sinuses and cerebral veins by using matched mask bone elimination. AJNR Am J Neuroradiol 25:787–791
Favrole P, Guichard JP, Crassard I, Bousser MG, Chabriat H (2004) Diffusion-weighted imaging of intravascular clots in cerebral venous thrombosis. Stroke 35:99–103. https://doi.org/10.1161/01.STR.0000106483.41458.AF
Ducreux D, Oppenheim C, Vandamme X, Dormont D, Samson Y, Rancurel G, Cosnard G, Marsault C (2001) Diffusion-weighted imaging patterns of brain damage associated with cerebral venous thrombosis. AJNR Am J Neuroradiol 22:261–268
Isensee C, Reul J, Thron A (1994) Magnetic resonance imaging of thrombosed dural sinuses. Stroke 25:29–34. https://doi.org/10.1161/01.STR.25.1.29
Farb RI, Scott JN, Willinsky RA, Montanera WJ, Wright GA, terBrugge KG (2003) Intracranial venous system: gadolinium-enhanced three-dimensional MR venography with auto-triggered elliptic centric-ordered sequence--initial experience. Radiology 226:203–209. https://doi.org/10.1148/radiol.2261020670
Rollins N, Ison C, Reyes T, Chia J (2005) Cerebral MR venography in children: comparison of 2D time-of-flight and gadolinium-enhanced 3D gradient-echo techniques. Radiology 235:1011–1017. https://doi.org/10.1148/radiol.2353041427
Yang JYK, Chan AKC, Callen DJA, Paes BA (2010) Neonatal cerebral sinovenous thrombosis: sifting the evidence for a diagnostic plan and treatment strategy. Pediatrics 126:e693–e700. https://doi.org/10.1542/peds.2010-1035
Monteiro AMV, Lima CMAO, Ribeiro ÉB, Lins MC, Miranda S, Miranda LE (2010) Diagnóstico por imagem e aspectos clínicos da trombose venosa cerebral em recém-natos a termo sem dano cerebral: revisão em 10 anos. Radiol Bras 43:149–153. https://doi.org/10.1590/S0100-39842010000300004
Hashmi M, Wasay M (2011) Caring for cerebral venous sinus thrombosis in children. J Emerg Trauma Shock 4:389–394. https://doi.org/10.4103/0974-2700.83870
Dlamini N, Billinghurst L, Kirkham FJ (2010) Cerebral venous sinus (sinovenous) thrombosis in children. Neurosurg Clin N Am 21:511–527. https://doi.org/10.1016/j.nec.2010.03.006
Cure JK, Van Tassel P, Smith MT (1994) Normal and variant anatomy of the dural venous sinuses. Semin Ultrasound CT MR 15:499–519. https://doi.org/10.1016/S0887-2171(05)80019-8
Widjaja E, Griffiths PD (2004) Intracranial MR venography in children: normal anatomy and variations. AJNR Am J Neuroradiol 25:1557–1562
Black DF, Rad AE, Gray LA, Campeau NG, Kallmes DF (2011) Cerebral venous sinus density on noncontrast CT correlates with hematocrit. AJNR Am J Neuroradiol 32:1354–1357. https://doi.org/10.3174/ajnr.A2504
Mamourian AC, Towfighi J (1995) MR of giant arachnoid granulation, a normal variant presenting as a mass within the dural venous sinus. AJNR Am J Neuroradiol 16:901–904
Oppenheim C, Domigo V, Gauvrit JY, Lamy C, Mackowiak-Cordoliani MA, Pruvo JP, Méder JF (2005) Subarachnoid hemorrhage as the initial presentation of dural sinus thrombosis. AJNR Am J Neuroradiol 26:614–617
Choudhri O, Feroze A, Marks MP, Do HM (2014) Endovascular management of cerebral venous sinus thrombosis. Neurosurg Focus 37:1. https://doi.org/10.3171/2014.V2.FOCUS14186
Star M, Flaster M (2013) Advances and controversies in the management of cerebral venous thrombosis. Neurol Clin 31:765–783. https://doi.org/10.1016/j.ncl.2013.03.013
Ferro JM, Bousser M-G, Canhão P, Coutinho JM, Crassard I, Dentali F, di Minno M, Maino A, Martinelli I, Masuhr F, Aguiar de Sousa D, Stam J, the European Stroke Organization (2017) European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis—endorsed by the European Academy of Neurology. Eur J Neurol 24:1203–1213. https://doi.org/10.1111/ene.13381
Sandercock PA, Leong TS (2017) Low-molecular-weight heparins or heparinoids versus standard unfractionated heparin for acute ischaemic stroke. Cochrane Database Syst Rev 4:CD000119. https://doi.org/10.1002/14651858.CD000119.pub4
Afshari D, Moradian N, Nasiri F, Razazian N, Bostani A, Sariaslani P (2015) The efficacy and safety of low-molecular-weight heparin and unfractionated heparin in the treatment of cerebral venous sinus thrombosis. Neurosciences (Riyadh) 20:357–361. https://doi.org/10.17712/nsj.2015.4.20150375
Siddiqui FM, Banerjee C, Zuurbier SM, Hao Q, Ahn C, Pride GL, Wasay M, Majoie CBLM, Liebeskind D, Johnson M, Stam J (2014) Mechanical thrombectomy versus intrasinus thrombolysis for cerebral venous sinus thrombosis: a non-randomized comparison. Interv Neuroradiol 20:336–344. https://doi.org/10.15274/INR-2014-10032
Li G, Zeng X, Hussain M, Meng R, Liu Y, Yuan K, Sikharam C, Ding Y, Ling F, Ji X (2013) Safety and validity of mechanical thrombectomy and thrombolysis on severe cerebral venous sinus thrombosis. Neurosurgery 72:730–738. https://doi.org/10.1227/NEU.0b013e318285c1d3
Siddiqui FM, Dandapat S, Banerjee C, Zuurbier SM, Johnson M, Stam J, Coutinho JM (2015) Mechanical thrombectomy in cerebral venous thrombosis: systematic review of 185 cases. Stroke 46:1263–1268. https://doi.org/10.1161/STROKEAHA.114.007465
Ilyas A, Chen C-J, Raper DM, Ding D, Buell T, Mastorakos P, Liu KC (2017) Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: a systematic review. J Neurointerv Surg 9:1086–1092. https://doi.org/10.1136/neurintsurg-2016-012938
Viegas LD, Stolz E, Canhão P, Ferro JM (2014) Systemic thrombolysis for cerebral venous and dural sinus thrombosis: a systematic review. Cerebrovasc Dis 37:43–50. https://doi.org/10.1159/000356840
Salottolo K, Wagner J, Frei DF, Loy D, Bellon RJ, McCarthy K, Jensen J, Fanale C, Bar-Or D (2017) Epidemiology, endovascular treatment, and prognosis of cerebral venous thrombosis: US center study of 152 patients. J Am Heart Assoc 6(6):e005480. https://doi.org/10.1161/JAHA.117.005480
Acknowledgements
The authors would like to thank Drs. Reza Forghani and Almudena Perez of the Jewish General Hospital, McGill University, for case and illustration contributions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Key points
• The empty delta sign more frequent presents between day 5 to 2 months after onset and may be associated with development of collaterals which provide peripheral enhancement surrounding the filling defect.
• Detection is more successful on unenhanced MRI when the imaging plane is orthogonal to the blood flow trajectory. For this reason, thrombosis of the sigmoid, sagittal, and transverse sinuses is better appreciated in coronal plane.
• T1WI high signal intensity of a superior sagittal sinus thrombosis is better seen in subacute thrombosis, due to methemoglobin thrombus composition.
• After 15 days, the diagnosis of CVT via MRI may be challenging as chronic thrombosis shows partial recanalization and the signal of the clot is iso- to hyperintense on T2WI and isointense on T1WI.
• TOF is a useful alternative to CE-MRV in pregnant or breastfeeding patients, as well as in case of severe renal failure. 2D TOF is superior to its 3D TOF due to low saturation effects and sensitivity with slow flow states.
• In neonates and infants, US is a useful screening method to demonstrate brain edema and to rapidly assess for possible complications from CVT. Between one and two thirds of children may develop intraparenchymal hemorrhage and ischemia.
• Given the propensity towards normal physiologic enhancement in the inner dural border zone in children, investigation with Doppler US can troubleshoot equivocal cases.
• On unenhanced CT, if there is a hemoconcentrated state that is increasing the density of the blood, arterial and venous structures will be equally affected,
• With CECT and CTV, a split or fenestrated sinus and intrasinus septa may cause a filling defect indistinguishable from the classic empty delta sign.
Rights and permissions
About this article
Cite this article
Dmytriw, A.A., Song, J.S.A., Yu, E. et al. Cerebral venous thrombosis: state of the art diagnosis and management. Neuroradiology 60, 669–685 (2018). https://doi.org/10.1007/s00234-018-2032-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-018-2032-2