Abstract
Purpose
While in the era of precision medicine, the right drug for each patient is selected based on molecular tumor characteristics, most novel oral targeted anticancer agents are still being administered using a one-size-fits-all fixed dosing approach. In this review, we discuss the scientific evidence for dose individualization of oral targeted therapies in oncology, based on therapeutic drug monitoring (TDM).
Methods
Based on literature search and our own experiences, seven criteria for drugs to be suitable candidates for TDM will be addressed: (1) absence of an easily measurable biomarker for drug effect; (2) long-term therapy; (3) availability of a validated sensitive bioanalytical method; (4) significant variability in pharmacokinetic exposure; (5) narrow therapeutic range; (6) defined and consistent exposure-response relationships; (7) feasible dose-adaptation strategies.
Results
All of these requirements are met for most oral targeted therapies in oncology. Also, prospective studies have already shown TDM to be feasible for imatinib, pazopanib, sunitinib, everolimus, and endoxifen.
Conclusions
In order to realize the full potential of personalized medicine in oncology, patients should not only be treated with the right drug, but also at the right dose. TDM could be a suitable tool to achieve this.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many new oral targeted therapies have become available in oncology over the past two decades. As a result, the treatment paradigm has partly shifted from a one-size-fits-all approach into precision medicine, in which the right drug is selected based on molecular characteristics of the tumor.
Dose finding of these new oral targeted therapies, however, has simply been copied from classical intravenous cytotoxic drugs. In traditional phase I dose escalation studies, which generally enroll only few patients (median sample size of 26 patients [1]), doses are increased until dose-limiting toxicities occur. This maximum tolerated dose (MTD), at which typically only 3–6 patients have been treated, is then used in all further studies, leading to a one-size-fits-all fixed dosing strategy [2]. However, pharmacokinetic characteristics of these new oral targeted therapies suggest individualized dosing would be far more rational.
Although one might think drug selection based on molecular diagnoses makes any further dose individualization superfluous, it seems logical to combine these two approaches to realize the full potential of personalized medicine (Fig. 1). Currently, all patients are treated at a standard fixed dose, resulting in low pharmacokinetic exposure and thus suboptimal treatment in a substantial proportion of patients. This subtherapeutic treatment is senseless, especially with these expensive drugs. Therefore, we believe that the current fixed dosing paradigm should be left. Therapeutic drug monitoring (TDM), which is individualized dosing based on measured plasma concentrations of the drug, can be used to select the right dose for each individual patient. In case of pharmacokinetic exposure below the predefined efficacy threshold and acceptable toxicities, pharmacokinetically guided interventions will be performed. These could include absolute dose increments or alternative interventions to increase pharmacokinetic exposure (i.e., concomitant intake with food in case of a clinically relevant food effect [3] or splitting intake moments in case of saturable absorption [4]). Although TDM is widely applied in clinical practice for many drug classes, such as antibiotics, anticonvulsants, and immunosuppressants, it is still being very limitedly applied in oncology.
Previous reviews have summarized the literature for TDM of individual oral anticancer drugs [5,6,7,8,9]. In this review, we will address the scientific evidence for dose individualization by TDM of oral targeted therapies in general. Table 1 provides an overview of approved oral targeted therapies in oncology.
Criteria for rational use of therapeutic drug monitoring
For drugs to be suitable candidates for TDM, the following requirements have previously been proposed [10,11,12,13,14]:
-
1.
absence of an easily measurable biomarker for drug effect;
-
2.
long-term therapy;
-
3.
availability of a validated sensitive bioanalytical method;
-
4.
significant variability in pharmacokinetic exposure;
-
5.
narrow therapeutic range;
-
6.
defined and consistent exposure-response relationships;
-
7.
feasible dose-adaptation strategies.
In the following paragraphs, each of these requirements will be discussed and it will be assessed whether they are met in the case of oral targeted therapies in oncology.
1. Absence of an easily measurable biomarker for drug effect
If more convenient, accurate, and precocious biomarkers for drug response would be available, these would make TDM superfluous. However, while toxicity can easily be measured, for efficacy, these biomarkers are generally not available (yet) and response evaluations with regard to antitumor efficacy are often based on radiological assessments, which are not performed timely enough to be a good biomarker. Imaging is usually performed every 8 to 12 weeks, while ideally dose adjustments should be made at an early stage (i.e., within 14 days). Also, once tumor progression is observed on radiological scans, resistant clones of tumor cells have already emerged and dose adjustments will probably be too late at this moment. Although for some tumor types blood-based tumor markers exist (e.g., cancer antigen 125 in ovarian cancer or carcinoembryonic antigen in colorectal cancer), these are not accurate enough to predict treatment response and to base treatment decisions upon [15]. The same holds true for other potential biomarkers available for oral targeted therapies including diastolic blood pressure for axitinib and skin rash for epidermal growth factor receptor inhibitors such as erlotinib and gefitinib [16,17,18]. Complete cytogenetic response in case of hematologic malignancies and prostate-specific antigen (PSA) in the case of prostate cancer are the only examples of biomarkers that can accurately predict response to treatment and that are used in clinical practice for this purpose [19, 20]. Apart from these exceptions, the first requirement for TDM is met for most combinations of targeted therapies and tumor types.
2. Long-term therapy
Treatment should be long enough to allow sufficient time for dose adjustments to be made. As the mean treatment duration of targeted therapies is several months, while only few days to weeks are needed to reach steady-state concentrations, there is sufficient time to perform TDM. The time to steady-state concentrations depends on the elimination half-life (t1/2) of a drug, which is typically around 20–30 hours for most oral anticancer drugs, although for some compounds, this is markedly longer (e.g., enzalutamide (± 6 days [21]) and endoxifen, which is the active metabolite of tamoxifen (± 2 weeks [22])). After four to five times the t1/2, steady-state concentrations have been attained.
3. Availability of a validated sensitive bioanalytical method
In order to perform dose individualization based on pharmacokinetic exposure, bioanalytical assays to measure plasma concentrations should be available. Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is usually applied for quantification of these drugs and validated assays are available for almost all oral anticancer drugs at a reasonable price. Since LC-MS/MS is a labor-intensive method and many different targeted therapies will be used in routine clinical practice, combining multiple drugs into one bioanalytical assay might be useful [23,24,25]. To implement TDM into routine clinical practice, an adequate infrastructure for sample collection and shipment should be in place, with a short turn-over and reporting time. In addition, dried blood spot (DBS) sampling could offer a more patient friendly sampling approach, as patients can obtain their blood samples themselves at home instead of having to visit the hospital. Whole blood samples can be collected by a finger prick at a paper DBS card, which can then be send to the laboratory by regular mail. DBS assays are already available for several oral anticancer drugs [26,27,28,29,30,31,32,33]. Also, commercial automated immunoassays could facilitate measurement in routine clinical practice, for example of imatinib [34].
4. Significant variability in pharmacokinetic exposure
The fourth requirement for TDM comprises a marked variability in pharmacokinetic exposure. Otherwise, when pharmacokinetic exposure would be predictable and similar for all patients, there would be no need for dose individualization.
Oral targeted therapies typically exhibit a large interindividual variability in pharmacokinetic exposure in the range of 24–84%, providing a strong rationale for TDM [35,36,37,38,39,40]. Reasons for this high interindividual variability include differences in absorption, which could be influenced by the poor bioavailability of these drugs, potential food effects, or the use of drugs that alter the stomach pH (i.e., proton pump inhibitors and H2 receptor antagonists); interactions with concomitant medication (e.g., via cytochrome P450 enzymes such as CYP3A4); pharmacogenetics (i.e., patients harboring polymorphisms of cytochrome P450 enzymes or ABC-transporters); hepatic and renal function; body composition and patient adherence [2, 41].
While data on interindividual variability are widely available, reports on intra-individual variability are sparse [42]. Poor formulations of most oral targeted therapies result in a low bioavailability and thus a high inter- and intra-individual variability [43, 44]. The intra-individual variability should be judged taking into account the interindividual variability as well. For example, abiraterone has an intra-individual variability of 33%, while the interindividual variability is higher (i.e., 46%) [37]. The same holds true for vemurafenib, which has an intra- and interindividual variability of 28% and 41%, respectively [38]. Unfortunately, these data are not available for all oral targeted therapies. Therefore, Chatelut et al. advocate intra-individual variability should ultimately be characterized before registration of new drugs [42]. Although assessment of the intra-individual variability for registration purposes might be challenging, especially in the context of oncological patients with potentially fluctuating (patho-)physiological states, we do propose that efforts should be made to quantify the intra-individual variability.
It is important to take the source of variability into account when deciding on the interval of sampling. When the major source of variability is interindividual variability, a single measurement or rare measurements would be sufficient. When the main source of variability is intra-individual variability, it depends on the origin. If the origin of intra-individual variability is random from dose to dose (e.g., due to poor formulation), TDM might not be useful, as a single sample would then be of limited value. If the intra-individual variability is caused by an identifiable reason (e.g., concomitant medication or fluctuations in (patho-)physiological conditions), more frequent sampling might be needed. In this case, the sampling interval should be oriented at the change of the condition (e.g., new concomitant medication). Regardless of the source of variability, it is important to continue sampling throughout therapy, since many factors that can influence pharmacokinetic exposure may vary over time (e.g., drug-drug interactions and compliance).
To conclude, variability in pharmacokinetic exposure of oral targeted therapies is definitely sufficiently high to meet the requisite.
5. Narrow therapeutic range
When the window between therapeutic and toxic concentrations is small, dose titration is important to minimize the risk of either ineffective treatment or unnecessary toxicities. The fact that > 50% of the oral targeted therapies have a recommended dose equal to the maximum tolerated dose (MTD), indicates these drugs have a narrow therapeutic index [45]. An exception to this is drugs with a plateau in the exposure-response curve that are dosed at the flat end of this curve, as might be the case for cabozantinib and pazopanib [46, 47]. At the currently used fixed doses, ± 30% of patients are being under dosed (e.g., for abiraterone, imatinib, pazopanib, sunitinib, and vemurafenib), associated with decreased efficacy, while ± 15% of patients are being over dosed, causing unnecessary toxicities [35, 37, 38, 48,49,50]. These numbers illustrate the significant proportion of patients being treated outside the therapeutic window in the absence of dose titration.
6. Defined and consistent exposure-response relationships
TDM is only rational if defined and consistent exposure-response relationships have been demonstrated for both efficacy and toxicity. For this purpose, exposure can be interpreted as minimum plasma concentration (Cmin), maximum plasma concentration (Cmax), or area under the plasma concentration-time curve (AUC). Extensive reviews summarizing the available literature on exposure-response relationships for each specific oral targeted therapy have previously been published [5,6,7,8,9]. For many of these drugs, exposure-response relationships have been demonstrated and pharmacokinetic targets could be identified (e.g., imatinib, pazopanib, and sunitinib [51,52,53,54]). For other drugs, pharmacokinetic targets based on exposure-efficacy analyses are not well established yet (e.g., dabrafenib, lenvatinib, and palbociclib [5]), but based on their mechanism of action, exposure-response relationships are to be expected. In these cases, the mean or median exposure could be taken as a reference. In previous analyses, we have demonstrated that targets based on exposure-efficacy analyses amounted to 82% (± 17%) and 85% (± 19%) of the average exposure in the population for kinase inhibitors and oral anti-hormonal drugs, respectively [5,6,7]. Therefore, targeting the mean or median exposure generally leads to efficacious concentrations (as the real exposure-efficacy threshold is expected to be lower). The fact that the exposure-efficacy threshold is generally lower than the average exposure in the population is not a surprising finding, since the efficacy of these drugs has been proven in phase III trials indicating that the mean exposure should be sufficient to generate an antitumor response.
The magnitude of exposure-response relationships can be illustrated by pazopanib, for which a clear exposure-efficacy relationship exists, with progression-free survival (PFS) being significantly longer in patients with Cmin ≥ 20.5 mg/L (52.0 weeks versus 19.6 weeks [53]). The PFS of patients with an exposure below this target is even comparable with placebo (4.2 months) [55], making treatment at an inadequate pharmacokinetic exposure as ineffective as no treatment at all.
To overcome resistance, newer generation kinase inhibitors have been designed that block their target irreversibly (e.g., osimertinib, ibrutinib, and afatinib) [56,57,58]. It still has to be elucidated how this affects exposure-response relationships, but based on their irreversible mechanism of action, it could be expected that these agents are relatively overdosed due to the MTD paradigm currently still used in dose finding studies. Since these drugs bind their target covalently, inhibition endures even after the drug has been cleared from the systemic circulation. Therefore, the efficacy threshold could be lower than the mean pharmacokinetic exposure at the recommended dose. So far, for none of these agents clear exposure-response relationships have been identified. For example, for osimertinib, a retrospective analysis of 780 subjects showed no association between exposure and response [59].
At the time new oral targeted therapies are approved, in most cases, insufficient data is available to draw conclusions on exposure-response relationships, while typically hundreds of patients have been treated with these drugs in the dose-finding and pivotal studies. However, data on pharmacokinetic exposure is often not structurally being collected in all patients. It is of great value to incorporate these pharmacokinetic analyses in the early stages of clinical development of these new drugs to ensure patients can be treated at a dose giving them adequate exposure.
Thus, for many oral targeted therapies defined and consistent exposure-response relationships exist, for others it can be reasonably expected while awaiting conclusive data, while for some exposure-response relationships might not be expected based on their irreversible mechanism of action and relatively high dose administered.
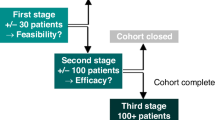
7. Feasible dose-adaptation strategy
For drugs to be suitable candidates for TDM, feasible dose-adaptation strategies should exist, leading to target attainment without additional toxicities. Prospective clinical studies have already shown TDM to be feasible for pazopanib [48, 49], sunitinib [48, 50], imatinib [48, 60], everolimus [61], and endoxifen [62]. Table 2 provides a summary of the results of these studies. In clinical practice, the dose-adaptation strategies used in these prospective studies could be applied (i.e., the same pharmacokinetic target and dose levels could be used). Also, algorithms describing dose-adaptation schedules for other oral targeted therapies have been published previously [6]. Figure 2 provides a schematic overview of pharmacokinetically guided dose individualization, in which pazopanib is used as an example. Patients start treatment at the standard fixed dose. At regular time intervals, pharmacokinetic sampling is performed (e.g., 4, 8, and 12 weeks after start of treatment, and every 12 weeks thereafter). In case of pharmacokinetic exposure below the predefined target and acceptable toxicities, the dosage can be increased with one dose level.
Dose-adaptation strategies should take into account the MTD of the drug, or—when the MTD has not been reached—the highest dose tested in phase I dose escalation trials, when deciding on the maximum dose level. Although it could be argued that pharmacokinetically guided dose escalation above the MTD could be safe as well (since this dose escalation will only be done in patients with a low pharmacokinetic exposure), this should only be considered with careful monitoring of side effects.
Pharmacokinetically guided interventions do not necessarily have to include absolute dose escalations, as for some oral targeted therapies, other options to increase pharmacokinetic exposure are available as well. For oral targeted therapies with a clinically significant food effect (e.g., abiraterone, lapatinib, and pazopanib), careful concomitant intake with food could be used as a first step in case of low pharmacokinetic exposure [3]. Besides, for drugs with a saturable absorption profile (e.g., pazopanib and everolimus), splitting intake moments could provide a cost-neutral solution to attain adequate pharmacokinetic exposure [4, 63].
Another important consideration is the fact that progressive disease is irreversible. Therefore, it is important to attain an adequate pharmacokinetic exposure in each individual patient as soon as possible. In addition, it could be argued that dose reductions should only be made in case of intolerable toxicities, and not solely based on pharmacokinetic exposure (i.e., patients with high pharmacokinetic exposure, but without any side effects). On this aspect, TDM in oncology differs significantly from other disciplines, where it is often aimed at preventing toxicities as well due to its small therapeutic window.
To summarize, the feasibility of dose-adaptation strategies has been prospectively studied for several oral targeted therapies [48,49,50, 60,61,62]. All of these studies have shown TDM to be feasible, at least for a subset of patients. For other oral targeted therapies, possible dose-adaptation strategies have been described in literature or could be set up taking into account the mentioned considerations, while awaiting additional prospective studies [6].
Discussion
In this concise review article, we discussed the conditions that should be fulfilled for oral targeted therapies in oncology to be suitable candidates for TDM. Apart from some exceptions (e.g., osimertinib or cabozantinib), for most oral targeted therapies all of these requirements are met, providing a strong rationale for TDM.
A practical advantage is that most oral anticancer drugs are administered at a once or twice daily basis, making the timing of sampling more convenient compared with intermittent dosing (e.g., classical chemotherapy or immunotherapy). TDM targets are generally based on trough concentrations (Cmin). While ideally trough samples would be drawn, this is not always possible in routine clinical practice. In this case, samples could be drawn at a random time point and Cmin can be estimated using several algorithms like the method proposed by Wang et al [64] or by Bayesian forecasting. In addition, a number of powerful pharmacokinetic computer tools are available for this purpose [65].
Even though convincing evidence supports dose individualization of oral targeted therapies, TDM is still being scarcely applied in daily clinical care. One of the reasons for this is that randomized controlled trials (RCTs), demonstrating the added value of TDM on clinical treatment outcomes, are lacking. However, it is highly unlikely that these RCTs could ever be performed. First, high numbers of patients would be needed, while most oral targeted therapies are indicated for rare tumor types or for a small subset of patients. For example, a randomized phase 3 study of TDM in patients with gastro-intestinal stromal tumors (GIST) treated with imatinib has been terminated prematurely due to slow accrual [66]. Second, it is difficult to secure (sufficient) funding for these types of studies. Furthermore, it is questionable whether it is ethical to fail to perform dose adjustments for some patients, when clear exposure-response relationships exist. Only a few RCTs of fixed dosing versus PK-guided dosing have ever been completed in oncology, all with chemotherapy [67,68,69,70].
Therefore, we are currently performing a large multi-center prospective study, in which we investigate the feasibility and efficacy of TDM for 23 different oral targeted therapies in more than 600 patients (www.trialregister.nl; NTR 6866 [71]). Patients starting regular treatment with one of these drugs can be included in this study. For each drug, pharmacokinetic targets and dose levels have been defined and are described in the protocol. Pharmacokinetic sampling and dose adaptations are performed according to the strategy depicted in Fig. 2. Primary outcome is to halve the proportion of patients with pharmacokinetic exposure below the target after 12 weeks (compared with historical data). Secondary outcomes are the safety, feasibility, and efficacy of pharmacokinetically guided dosing and physician adherence to the tailored treatment recommendations. If this study underscores the results of previous retrospective studies and prospective feasibility studies, this will further support the implementation of pharmacokinetically guided dose optimization as the new standard [48,49,50, 60,61,62, 72].
As can be seen in Table 2, results of PK-guided dose individualization studies are currently not being reported in a uniform way, making mutual comparisons difficult. Therefore, we propose that future studies should at least report the following:
-
Proportion of patients with low pharmacokinetic exposure;
-
Proportion of patients in whom PK-guided interventions were applied;
-
Reasons why these were not applied in other patients (e.g., toxicity, physician adherence);
-
-
Proportion of patients in which PK-guided interventions were successful, thus in which adequate PK-exposure was attained without intolerable toxicities.
In this way, study results could be compared more easily and potentially be combined in a meta-analytical approach.
It is essential to convince treating physicians of the importance of TDM, as they need to implement the treatment recommendations into clinical practice. Unwillingness of treating physicians to follow these treatment recommendations was the main reason that a previous randomized controlled trial could not demonstrate the benefit of TDM for imatinib [60].
Apart from the apparent advantages of TDM in optimizing pharmacokinetic exposure to improve treatment outcomes, TDM could serve several other purposes as well. First, it could play a role in detecting nonadherence to therapy. This is especially important in the case of long-term therapy, as compliance drastically decreases over time (e.g., for tamoxifen adherence was only 50% after 4 years of therapy [73]). Second, TDM could be helpful in the management of drug-drug interactions, since pharmacokinetic exposure to many oral targeted therapies is affected by concomitant use of CYP3A4 inhibitors/inducers or gastric acid-suppressive agents [74]. Last, measuring plasma drug concentrations could also support dose titration in patients with renal or hepatic impairment.
Conclusion
The pharmacokinetic characteristics of (most) oral targeted therapies in oncology support dose individualization by therapeutic drug monitoring. To realize the full potential of personalized medicine, we should not only treat each patient with the right drug, but also at the right dose.
References
Brummelen EMJ, Huitema ADR, Werkhoven E et al (2016) The performance of model-based versus rule-based phase I clinical trials in oncology. J Pharmacokinet Pharmacodyn 43:235–242. https://doi.org/10.1007/s10928-016-9466-0
Mathijssen RHJ, Sparreboom A, Verweij J (2014) Determining the optimal dose in the development of anticancer agents. Nat Rev Clin Oncol 11:272–281. https://doi.org/10.1038/nrclinonc.2014.40
Willemsen AEACB, Lubberman FJE, Tol J et al (2016) Effect of food and acid-reducing agents on the absorption of oral targeted therapies in solid tumors. Drug Discov Today 21:962–976. https://doi.org/10.1016/j.drudis.2016.03.002
Yu H, van Erp N, Bins S, Mathijssen RHJ, Schellens JHM, Beijnen JH, Steeghs N, Huitema ADR (2017) Development of a pharmacokinetic model to describe the complex pharmacokinetics of pazopanib in cancer patients. Clin Pharmacokinet 56:293–303. https://doi.org/10.1007/s40262-016-0443-y
Verheijen RB, Yu H, Schellens JHM, Beijnen JH, Steeghs N, Huitema ADR (2017) Practical recommendations for therapeutic drug monitoring of kinase inhibitors in oncology. Clin Pharmacol Ther 102:765–776. https://doi.org/10.1002/cpt.787
Yu H, Steeghs N, Nijenhuis C et al (2014) Practical guidelines for therapeutic drug monitoring of anticancer tyrosine kinase inhibitors: focus on the pharmacokinetic targets. Clin Pharmacokinet 53:305–325. https://doi.org/10.1007/s40262-014-0137-2
Groenland SL, Van Nuland M, Verheijen RB et al (2019) Therapeutic drug monitoring of oral anti- hormonal drugs in oncology. Clin Pharmacokinet 58:299–308. https://doi.org/10.1007/s40262-018-0683-0
Widmer N, Bardin C, Chatelut E, Paci A, Beijnen J, Levêque D, Veal G, Astier A (2014) Review of therapeutic drug monitoring of anticancer drugs part two - targeted therapies. Eur J Cancer 50:2020–2036. https://doi.org/10.1016/j.ejca.2014.04.015
De Wit D, Guchelaar HJ, Den Hartigh J et al (2015) Individualized dosing of tyrosine kinase inhibitors: are we there yet? Drug Discov Today 20:18–36. https://doi.org/10.1016/j.drudis.2014.09.007
Mcleod HL (1997) Therapeutic drug monitoring opportunities in cancer therapy. Pharmacol Ther 74:39–54. https://doi.org/10.1016/S0163-7258(96)00201-X
Galpin AJ, Evans WE (1993) Therapeutic drug monitoring in cancer management. Clin Chem 39:2419–2430
Massoni E, Zamboniz WC (1997) Pharmacokinetic optimisation of cancer chemotherapy - effect on outcomes. Clin Pharmacokinet 32:324–343. https://doi.org/10.2165/00003088-199732040-00005
Hon YY, Evans WE (1998) Making TDM work to optimize cancer chemotherapy : a multidisciplinary team approach. Clin Chem 400:388–400
De Jonge ME, Huitema ADR, Schellens JHM et al (2005) Individualised cancer chemotherapy: strategies and performance of prospective studies on therapeutic drug monitoring with dose adaptation: a review. Clin Pharmacokinet 44:147–173. https://doi.org/10.2165/00003088-200544020-00002
Rustin GJS, Van Der Burg MEL, Griffin CL et al (2010) Early versus delayed treatment of relapsed ovarian cancer (MRC OV05/EORTC 55955): a randomised trial. Lancet 376:1155–1163. https://doi.org/10.1016/S0140-6736(10)61268-8
Rini BI, Melichar B, Ueda T, Grünwald V, Fishman MN, Arranz JA, Bair AH, Pithavala YK, Andrews GI, Pavlov D, Kim S, Jonasch E (2013) Axitinib with or without dose titration for first-line metastatic renal-cell carcinoma: a randomised double-blind phase 2 trial. Lancet Oncol 14:1233–1242. https://doi.org/10.1016/S1470-2045(13)70464-9
Steffens M, Paul T, Hichert V, Scholl C, von Mallek D, Stelzer C, Sörgel F, Reiser B, Schumann C, Rüdiger S, Boeck S, Heinemann V, Kächele V, Seufferlein T, Stingl J (2016) Dosing to rash? - the role of erlotinib metabolic ratio from patient serum in the search of predictive biomarkers for EGFR inhibitor-mediated skin rash. Eur J Cancer 55:131–139. https://doi.org/10.1016/j.ejca.2015.11.022
Perez CA, Song H, Raez LE, Agulnik M, Grushko TA, Dekker A, Stenson K, Blair EA, Olopade OI, Seiwert TY, Vokes EE, Cohen EEW (2012) Phase II study of gefitinib adaptive dose escalation to skin toxicity in recurrent or metastatic squamous cell carcinoma of the head and neck. Oral Oncol 48:887–892
Jabbour E, Kantarjian H, O’Brien S et al (2011) The achievement of an early complete cytogenetic response is a major determinant for outcome in patients with early chronic phase chronic myeloid leukemia treated with tyrosine kinase inhibitors. Blood 118:4541–4547
Armstrong AJ, Saad F, Phung D, Dmuchowski C, Shore ND, Fizazi K, Hirmand M, Forer D, Scher HI, Bono JD (2017) Clinical outcomes and survival surrogacy studies of prostate-specific antigen declines following enzalutamide in men with metastatic castration-resistant prostate cancer previously treated with docetaxel. Cancer 123:2303–2311. https://doi.org/10.1002/cncr.30587
Food and Drug Administration (2012) Center for Drug Evaluation and Research Enzalutamide clinical pharmacology and biopharmaceutics review. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/203415Orig1s000ClinPharmR.pdf. Accessed 15 January 2019
Summary of product characteristics - tamoxifen. https://www.medicines.org.uk/emc/product/2248/smpc. Accessed 15 January 2019
Herbrink M, De VN, Rosing H et al (2016) Quantification of 11 therapeutic kinase inhibitors in human plasma for therapeutic drug monitoring using liquid chromatography coupled with tandem mass spectrometry. Ther Drug Monit 38:649–656. https://doi.org/10.1097/FTD.0000000000000349
Herbrink M, De Vries N, Rosing H et al (2018) Development and validation of a liquid chromatography – tandem mass spectrometry analytical method for the therapeutic drug monitoring of eight novel anticancer drugs. Biomed Chromatogr 32:1–9. https://doi.org/10.1002/bmc.4147
Van NM, Venekamp N, De VN et al (2019) Development and validation of an UPLC-MS / MS method for the therapeutic drug monitoring of oral anti-hormonal drugs in oncology. J Chromatogr B 1106–1107:26–34. https://doi.org/10.1016/j.jchromb.2019.01.001
Jager NGL, Rosing H, Linn SC, Schellens JHM, Beijnen JH (2015) Dried blood spot self-sampling at home for the individualization of tamoxifen treatment: a feasibility study. Ther Drug Monit 37:833–836. https://doi.org/10.1097/ftd.0000000000000224
Verheijen RB, Bins S, Thijssen B, Rosing H, Nan L, Schellens JHM, Mathijssen RHJ, Lolkema MP, Beijnen JH, Steeghs N, Huitema ADR (2016) Development and clinical validation of an LC-MS/MS method for the quantification of pazopanib in DBS. Bioanalysis 8:123–134. https://doi.org/10.4155/bio.15.235
De Wit D, Den Hartigh J, Gelderblom H et al (2015) Dried blood spot analysis for therapeutic drug monitoring of pazopanib. J Clin Pharmacol 55:1344–1350. https://doi.org/10.1002/jcph.558
Antunes MV, Raymundo S, Wagner SC, Mattevi VS, Vieira N, Leite R, Reginato F, Capra MZ, Fogliatto L, Linden R (2015) DBS sampling in imatinib therapeutic drug monitoring: from method development to clinical application. Bioanalysis 7:2105–2117. https://doi.org/10.4155/bio.15.101
Verheijen RB, Thijssen B, Atrafi F, Schellens JHM, Rosing H, de Vries N, Beijnen JH, Mathijssen RHJ, Steeghs N, Huitema ADR (2019) Validation and clinical application of an LC-MS/MS method for the quantification of everolimus using volumetric absorptive microsampling. J Chromatogr B 1104:234–239. https://doi.org/10.1016/j.jchromb.2018.11.030
Willemsen AECAB, Knapen LM, de Beer YM, Brüggemann RJM, Croes S, van Herpen CML, van Erp NP (2018) Clinical validation study of dried blood spot for determining everolimus concentration in patients with cancer. Eur J Clin Pharmacol 74:465–471. https://doi.org/10.1007/s00228-017-2394-0
Boons CCLM, Chahbouni A, Schimmel AM, Wilhelm AJ, den Hartog YM, Janssen JJWM, Hendrikse NH, Hugtenburg JG, Swart EL (2017) Dried blood spot sampling of nilotinib in patients with chronic myeloid leukaemia: a comparison with venous blood sampling. J Pharm Pharmacol 69:1265–1274. https://doi.org/10.1111/jphp.12757
Nijenhuis CM, Huitema ADR, Marchetti S, Blank C, Haanen JBAG, van Thienen JV, Rosing H, Schellens JHM, Beijnen JH (2016) The use of dried blood spots for pharmacokinetic monitoring of vemurafenib treatment in melanoma patients. J Clin Pharmacol 56:1307–1312. https://doi.org/10.1002/jcph.728
Beumer JH, Kozo D, Harney RL, Baldasano CN, Jarrah J, Christner SM, Parise R, Baburina I, Courtney JB, Salamone SJ (2016) Automated imatinib immunoassay. Ther Drug Monit 37:486–492. https://doi.org/10.1097/FTD.0000000000000178
Lankheet N, Knapen L, Schellens J et al (2014) Plasma concentrations of tyrosine kinase inhibitors imatinib, erlotinib, and sunitinib in routine clinical outpatient cancer care. Ther Drug Monit 36:326–334. https://doi.org/10.1097/FTD.0000000000000004
Verheijen RB, Swart LE, Beijnen JH, Schellens JHM, Huitema ADR, Steeghs N (2017) Exposure-survival analyses of pazopanib in renal cell carcinoma and soft tissue sarcoma patients: opportunities for dose optimization. Cancer Chemother Pharmacol 80:1171–1178. https://doi.org/10.1007/s00280-017-3463-x
Carton E, Noe G, Huillard O, Golmard L, Giroux J, Cessot A, Saidu NEB, Peyromaure M, Zerbib M, Narjoz C, Guibourdenche J, Thomas A, Vidal M, Goldwasser F, Blanchet B, Alexandre J (2017) Relation between plasma trough concentration of abiraterone and prostate-specific antigen response in metastatic castration-resistant prostate cancer patients. Eur J Cancer 72:54–61. https://doi.org/10.1016/j.ejca.2016.11.027
Nijenhuis CM, Huitema ADR, Blank C, Haanen JBAG, van Thienen JV, Rosing H, Schellens JHM, Beijnen JH (2016) Clinical pharmacokinetics of vemurafenib in BRAF-mutated melanoma patients. J Clin Pharmacol 57:125–128. https://doi.org/10.1002/jcph.788
Ouellet D, Gibiansky E, Leonowens C, O’Hagan A, Haney P, Switzky J, Goodman VL (2014) Population pharmacokinetics of dabrafenib, a BRAF inhibitor: effect of dose, time, covariates, and relationship with its metabolites. J Clin Pharmacol 54:696–706. https://doi.org/10.1002/jcph.263
Ouellet D, Kassir N, Chiu J, Mouksassi MS, Leonowens C, Cox D, DeMarini DJ, Gardner O, Crist W, Patel K (2016) Population pharmacokinetics and exposure-response of trametinib, a MEK inhibitor, in patients with BRAF V600 mutation-positive melanoma. Cancer Chemother Pharmacol 77:807–817. https://doi.org/10.1007/s00280-016-2993-y
van Leeuwen R, van Gelder T, Mathijssen R, Jansman F (2014) Drug-drug interactions with tyrosine-kinase inhibitors: a clinical perspective. Lancet Oncol 15:e315–e326. https://doi.org/10.1016/S1470-2045(13)70579-5
Chatelut E, Bruno R, Ratain MJ (2018) Intraindividual pharmacokinetic variability : focus on small- molecule kinase inhibitors. Clin Pharmacol Ther 103:956–958. https://doi.org/10.1002/cpt.937
Herbrink M, Nuijen B, Schellens JHM, Beijnen JH (2015) Variability in bioavailability of small molecular tyrosine kinase inhibitors. Cancer Treat Rev 41:412–422. https://doi.org/10.1016/j.ctrv.2015.03.005
Herbrink M, Nuijen B, Schellens JHM, Beijnen JH (2017) High-tech drugs in creaky formulations. Pharm Res 34:1751–1753. https://doi.org/10.1007/s11095-017-2185-4
Bullock JM, Rahman A, Liu Q (2016) Lessons learned: dose selection of small molecule – targeted oncology drugs. Clin Cancer Res 22:2630–2639. https://doi.org/10.1158/1078-0432.CCR-15-2646
Lacy S, Nielsen J, Yang B, Miles D, Nguyen L, Hutmacher M (2018) Population exposure – response analysis of cabozantinib efficacy and safety endpoints in patients with renal cell carcinoma. Cancer Chemother Pharmacol 81:1061–1070. https://doi.org/10.1007/s00280-018-3579-7
Hurwitz HI, Dowlati A, Saini S, Savage S, Suttle AB, Gibson DM, Hodge JP, Merkle EM, Pandite L (2009) Phase I trial of pazopanib in patients with advanced cancer. Clin Cancer Res 15:4220–4227. https://doi.org/10.1158/1078-0432.CCR-08-2740
Lankheet N, Desar I, Mulder S et al (2017) Optimizing the dose in cancer patients treated with imatinib, sunitinib and pazopanib. Br J Clin Pharmacol 83:2195–2204. https://doi.org/10.1111/bcp.13327
Verheijen RB, Bins S, Mathijssen RHJ, Lolkema MP, van Doorn L, Schellens JHM, Beijnen JH, Langenberg MHG, Huitema ADR, Steeghs N, on behalf of the Dutch Pharmacology Oncology Group (2016) Individualized pazopanib dosing: a prospective feasibility study in cancer patients. Clin Cancer Res 22:5738–5746. https://doi.org/10.1158/1078-0432.CCR-16-1255
Lankheet N, Kloth J, Gadellaa-van Hooijdonk C et al (2014) Pharmacokinetically guided sunitinib dosing: a feasibility study in patients with advanced solid tumours. Br J Cancer 110:2441–2449. https://doi.org/10.1038/bjc.2014.194
Larson RA, Druker BJ, Guilhot F, O’Brien SG, Riviere GJ, Krahnke T, Gathmann I, Wang Y, for the IRIS (International Randomized Interferon vs STI571) Study Group (2008) Imatinib pharmacokinetics and its correlation with response and safety in chronic-phase chronic myeloid leukemia: a subanalysis of the IRIS study. Blood 111:4022–4028. https://doi.org/10.1182/blood-2007-10-116475
Demetri GD, Wang Y, Wehrle E, Racine A, Nikolova Z, Blanke CD, Joensuu H, von Mehren M (2009) Imatinib plasma levels are correlated with clinical benefit in patients with unresectable/metastatic gastrointestinal stromal tumors. J Clin Oncol 27:3141–3147. https://doi.org/10.1200/JCO.2008.20.4818
Suttle A, Ball H, Molimard M et al (2014) Relationships between pazopanib exposure and clinical safety and efficacy in patients with advanced renal cell carcinoma. Br J Cancer 111:1909. https://doi.org/10.1038/bjc.2014.503
Houk BE, Bello CL, Poland B, Rosen LS, Demetri GD, Motzer RJ (2009) Relationship between exposure to sunitinib and efficacy and tolerability endpoints in patients with cancer: results of a pharmacokinetic/pharmacodynamic meta-analysis. Cancer Chemother Pharmacol 66:357–371. https://doi.org/10.1007/s00280-009-1170-y
Sternberg CN, Davis ID, Mardiak J, Szczylik C, Lee E, Wagstaff J, Barrios CH, Salman P, Gladkov OA, Kavina A, Zarbá JJ, Chen M, McCann L, Pandite L, Roychowdhury DF, Hawkins RE (2010) Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol 28:1061–1068. https://doi.org/10.1200/JCO.2009.23.9764
Food and Drug Administration (2015) Center for Drug Evaluation and Research. Osimertinib clinical pharmacology and biopharmaceutics review. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2015/208065Orig1s000ClinPharmR.pdf. Accessed 15 January 2019
Food and Drug Administration. Center for Drug Evaluation and Research. Clinical pharmacology and biopharmaceutics review ibrutinib. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/205552orig1s000ClinPharmR.pdf. Accessed 15 January 2019
Food and Drug Administration (2012) Center for Drug Evaluation and Research. Clinical pharmacology and biopharmaceutics review afatinib https://www.accessdata.fda.gov/drugsatfda_docs/nda/2013/201292Orig1s000ClinPharmR.pdf. Accessed 15 January 2019
Brown K, Comisar C, Witjes H, Maringwa J, de Greef R, Vishwanathan K, Cantarini M, Cox E (2017) Population pharmacokinetics and exposure-response of osimertinib in patients with non-small cell lung cancer. Br J Clin Pharmacol 83:1216–1226
Gotta V, Widmer N, Decosterd LA, Chalandon Y, Heim D, Gregor M, Benz R, Leoncini-Franscini L, Baerlocher GM, Duchosal MA, Csajka C, Buclin T (2014) Clinical usefulness of therapeutic concentration monitoring for imatinib dosage individualization: results from a randomized controlled trial. Cancer Chemother Pharmacol 74:1307–1319. https://doi.org/10.1007/s00280-014-2599-1
Krueger DA, Care MM, Holland K, Agricola K, Tudor C, Mangeshkar P, Wilson KA, Byars A, Sahmoud T, Franz DN (2010) Everolimus for subependymal giant-cell astrocytomas in tuberous sclerosis. N Engl J Med 363:1801–1811. https://doi.org/10.1056/NEJMoa1001671
Fox P, Balleine RL, Lee C, Gao B, Balakrishnar B, Menzies AM, Yeap SH, Ali SS, Gebski V, Provan P, Coulter S, Liddle C, Hui R, Kefford R, Lynch J, Wong M, Wilcken N, Gurney H (2016) Dose escalation of tamoxifen in patients with low endoxifen level: evidence for therapeutic drug monitoring - the TADE study. Clin Cancer Res 22:3164–3171. https://doi.org/10.1158/1078-0432.CCR-15-1470
Verheijen RB, Atrafi F, Schellens JHM, Beijnen JH, Huitema ADR, Mathijssen RHJ, Steeghs N (2018) Pharmacokinetic optimization of everolimus dosing in oncology: a randomized crossover trial. Clin Pharmacokinet 57:637–644. https://doi.org/10.1007/s40262-017-0582-9
Wang Y, Chia Y, Nedelman J et al (2009) A therapeutic drug monitoring algorithm for refining the imatinib trough level obtained at different sampling times. Ther Drug Monit 31:579–584. https://doi.org/10.1097/FTD.0b013e3181b2c8cf
Fuchs A, Csajka C, Thoma Y, Buclin T, Widmer N (2013) Benchmarking therapeutic drug monitoring software: a review of available computer tools. Clin Pharmacokinet 52:9–22. https://doi.org/10.1007/s40262-012-0020-y
Study of dose escalation versus no dose escalation of imatinib in metastatic gastrointestinal stromal tumors. http://clinicaltrials.gov/ct2/show/NCT01031628. Accessed 15 January 2019
Evans W, Relling M, Rodman J et al (1998) Conventional compared with individualized chemotherapy for childhood acute lymphoblastic leukemia. N Engl J Med 338:499–505. https://doi.org/10.1056/NEJM199802193380803
Joerger M, Von Pawel J, Kraff S et al (2016) Open-label, randomized study of individualized, pharmacokinetically (PK)-guided dosing of paclitaxel combined with carboplatin or cisplatin in patients with advanced non-small-cell lung cancer (NSCLC). Ann Oncol 27:1895–1902. https://doi.org/10.1093/annonc/mdw290
Gamelin E, Delva R, Jacob J, Merrouche Y, Raoul JL, Pezet D, Dorval E, Piot G, Morel A, Boisdron-Celle M (2008) Individual fluorouracil dose adjustment based on pharmacokinetic follow-up compared with conventional dosage: results of a multicenter randomized trial of patients with metastatic colorectal cancer. J Clin Oncol 26:2099–2105. https://doi.org/10.1200/JCO.2007.13.3934
Fety R, Rolland F, Barberi-Heyob M, Hardouin A, Campion L, Conroy T, Merlin JL, Rivière A, Perrocheau G, Etienne MC, Milano G (1998) Clinical impact of pharmacokinetically-guided dose adaptation of 5-fluorouracil: results from a multicentric randomized trial in patients with locally advanced head and neck carcinomas. Clin Cancer Res 4:2039–2045
Netherlands Trial Register NTR6866. Therapeutic drug monitoring for oral anti-cancer drugs. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=6866. Accessed 15 January 2019
De WD, Van ENP, Den HJ et al (2015) Therapeutic drug monitoring to individualize the dosing of pazopanib: a pharmacokinetic feasibility study. Ther Drug Monit 37:331–338. https://doi.org/10.1097/FTD.0000000000000141
Partridge AH, Wang PS, Winer EP, Avorn J (2003) Nonadherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol 21:602–606. https://doi.org/10.1200/JCO.2003.07.071
Hussaarts KGAM, Veerman GDM, Jansman FGA, van Gelder T, Mathijssen RHJ, van Leeuwen RWF (2019) Clinically relevant drug interactions with multikinase inhibitors: a review. Ther Adv Med Oncol 11:1–34. https://doi.org/10.1177/1758835918818347
Author information
Authors and Affiliations
Contributions
Conception and design of this review were performed by SG, AH, and NS; SG wrote the manuscript; RM, JB, AH, and NS critically reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Groenland, S.L., Mathijssen, R.H.J., Beijnen, J.H. et al. Individualized dosing of oral targeted therapies in oncology is crucial in the era of precision medicine. Eur J Clin Pharmacol 75, 1309–1318 (2019). https://doi.org/10.1007/s00228-019-02704-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02704-2