Abstract
Purpose
The aim of the study was to detect adverse drug reactions (ADRs) in pediatric inpatients using the medical administrative database “Programme de Médicalisation des Systèmes d′Information” (PMSI) and to compare these cases ADRs with those spontaneously reported to a regional PharmacoVigilance (PV) Centre.
Methods
The study was conducted from January 2008 to December 2011 in the Children University Hospital of Toulouse (Midi-Pyrénées, South-west France). From PMSI database, all discharge summaries including selected ICD-10 codes (10th International Classification of Diseases) were analyzed. All ADRs spontaneously reported by the Children Hospital of Toulouse and registered in the French PV Database (FPVDB) were included. The capture–recapture method was applied to estimate the incidence of ADRs.
Results
During the study period, we identified 60 reports from the PMSI database and 200 from the FPVDB. The rate of “serious” ADRs was higher in PMSI reports (74.6 % vs 38.9 %, p < 0.0001). The most frequent ADRs reported were musculoskeletal (12.4 %) and central (11.3 %) ADRs in PMSI database versus cutaneous (22.4 %) and general (17.5 %) ADRs in FPVDB. The most frequently suspected drugs were antineoplastic drugs (31.1 %) in PMSI database versus anti-infectives (38.2 %) in FPVDB. The estimated number of ADRs was 717 [95 % confidence interval (CI) 513, 921], and the incidence of ADRs among admissions was 0.6 % (95 % CI 0.4, 0.8).
Conclusions
Use of PMSI database improves from around 30 % detection of ADRs in children. In comparison with classical pharmacovigilance database, it also allows to detect different ADRs and drugs, thus enhancing safe medicine use for pediatric patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In pediatric population, adverse drug reactions (ADRs) are an important source of morbidity [1–6]. Drug used in children are undervalued, and off-label prescribing has been widely observed [7], that may result in an increased risk of ADRs [8]. In the later years, in Europe and the US, there were several incentives to promote drug assessment in children. Although the latest initiative has improved some therapeutic options for children, significantly, more effort will be needed to achieve a safer use of medicines in this population [9, 10]. Thus, recording and assessment of ADRs may be an important way to improve security of drug use in children [2].
Methodology of ADR detection includes several approaches. The main widely used is spontaneous reporting of a potential ADR by health professionals and patients. This method is limited by under-reporting which is particularly important in pediatrics [11]. Intensive monitoring, retrospective, or prospective chart reviews are also another ways to collect ADRs despite the fact that they are time consuming [12].
A recent strategy to improve ADR notification is computer detection in health care databases [13–16]. The principle is to look for signals suggesting the possible presence of an ADR from hospital information systems. The databases more often used are pharmacy and laboratory sources [17] but also medical administrative databases such as hospital medical information system databases. In France, the hospital discharge database, Programme de Medicalisation des Systèmes d’Information (PMSI) gives information about diagnoses and therapeutic interventions [18]. Up to now, all the studies using PMSI were performed in adults.
The aim of the present study was to detect ADRs occurred in a children university hospital using the medical administrative database PMSI and to compare the cases extracted from the PMSI database with those spontaneously reported during the same period to a regional Pharmacovigilance Centre (Midi-Pyrénées, South-west France). Simultaneous use of two data sources allows us to estimate the incidence of ADRs in our pediatric inpatient population using capture–recapture method.
Materials and methods
The study was performed in the Children’s teaching hospital of Toulouse (Midi-Pyrénées, South-west, France) with a total number of hospital admissions of 30, 000 patients per year, covering a population of more than 1,200,000 inhabitants. The study involved all children (less than 18 years) hospitalized from 1 January 2008 to 31 December 2011.
Data sources
We used data collected in the PMSI database and ADRs spontaneously reported to the Midi-Pyrénées Regional Pharmacovigilance Centre and recorded to the French PharmacoVigilance Database (FPVDB) after assessment and validation of causality.
The PMSI is the French system for case-mixed classification for the financial management of hospitals. A standardized medical outcome summary is filled in for each hospital stay. This summary contains administrative (name, gender, birthdate, and date of hospital admission/discharge) and main clinical (diagnoses and medical or surgical procedures coded using the 10th international classification of diseases (ICD 10th) data. This standard patient discharge summary is similar to the minimum data sat (MBDS) used in other countries.
Since 1985, the FPVDB has been gathering informations on ADR cases occurring in France and reported to the 31 Regional PharmacoVigilance Centres (CRPV) by health professionals and, since 2011, by patients. The Midi-Pyrénées Regional Pharmacovigilance Centre is located in the Department of Clinical Pharmacology of the Toulouse University Hospital. For each spontaneous report, data concerning patient, drug exposure, and effects are collected to assess drug causality according to the official French method [19]. All reports are anonymously registered in the FPVDB.
Case definition
An ADR is defined as a noxious and unintended event which occurs at doses generally used in humans for prophylaxis, diagnosis, therapy, or modification of physiological functions. A “serious” adverse drug reaction is “any untoward medical occurrence that at any dose results in death, requires hospital admission or prolongation of existing hospital stay, results in persistent or significant disability/incapacity, or is life threatening” [20]. All ADRs, with a date of occurrence or diagnosis during the 4-year study period (from January 2008 to December 2011) and cared in the Children’s teaching Hospital of Toulouse were analyzed. Any drug(s) suspected of causing the adverse reaction was listed as the suspect drug(s).
Numbers of ICD-10 listing—selection of cases
We selected 129 ICD-10 codes (Table 1) (10th International Classification of Diseases) related to an ADR. Then, we extracted, with the collaboration of the Department of Medical Information, PMSI patient’s records registered with one of these ICD-10 codes. We decided to exclude the codes for “fever” (because of lack of specificity of this ADR, “agranulocytosis with chemotherapeutical drugs” when they did not require admission in intensive care unit (ICU) and “drug-induced aplastic anemia” with chemotherapeutical drugs to avoid background noise due to the large number of cases and drugs involved. Hospital discharge reports of each patient were read to check out if there was any mention of an ADR. Reports with no mention of ADR were excluded.
An event was considered reportable if information necessary to analyze an ADR was provided in hospitalization summaries. If the same ADR for a patient was reported in different summaries (duplicate), it was counted as only one record. Data concerning patient, drug exposure, and event were collected to assess drug causality. All cases were checked and validated by senior pharmacologist members of staff from the Midi-Pyrénées Regional Pharmacovigilance Centre. The ADRs identified through PMSI were registered in the FPVDB.
From FPVDB, we extracted all ADRs spontaneously reported by health professionals working in Children’s teaching Hospital of Toulouse during the same study period (from 1 January 2008 to 31 December 2011).
We matched the cases in order to eliminate duplicates. Duplicates were identified between the two sources using demographic data (first name, last name, and age), characteristics of ADRs, involved drugs, and dates of hospital stay.
Capture–recapture method
The capture–recapture method was used to provide population estimates from two or more incomplete sources of information [18, 21]. It allows refinement of frequency estimations and ascertaining the exhaustiveness of monitoring systems. Its principle consists of combining data provided by several sources coming from the same population.
After identification of matches between sources, the capture–recapture method allows estimation of the number of non-identified cases by any of the sources. Thus, the total number of cases in the pediatric inpatient population during the study period can be deduced and the incidence of ADRs estimated. Underreporting was quantified by the underreporting coefficient (U) calculated as the ratio between the total number of ADRs estimated during the study period and those spontaneously reported to the regional Pharmacovigilance Centre [17].
Comparison between PMSI and FPVDB databases
For each report, we analyzed the following data concerning patients: age, gender, ADRs, and suspected drugs. The Medical Dictionary for Regulatory Activities (MedDRA®) primary System Organ Class (SOC) and the WHO Anatomical Therapeutic Chemical (ATC) classification were used to class ADRs and drugs, respectively. Comparisons between PMSI and FPVDB databases were made using the chi-square test. Statistical analyses were performed using SAS® Software v.9.2 (SAS Institute Inc., USA) with a two-sided α-level of 0.05.
Results
ADRs reports
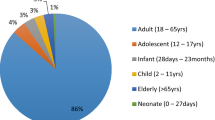
From FPVDB, we found 200 spontaneous notifications reported by health professionals working in Children’s Teaching Hospital of Toulouse during the same period, corresponding to 200 patients (49.5 % male) aged from 5 days to 17.0 years (median age, 7 years).
From PMSI database, during the study period, 1128 hospitalization reports were identified according to dates of hospital stay and preselected ICD-10 codes. As previously described in Methods, we decided to exclude the 688 cases of “agranulocytosis with chemotherapeutical drugs” or “drug-induced aplastic anemia”. Out of the 440 remaining cases, we did not find any mention of ADRs in 311 discharge reports, and in 41 cases, there was insufficient information. These 352 cases were excluded from this present analysis. A total of 28 ADRs (duplicate reports) were registered both in PMSI database and the FPVDB. Finally, 60 ADR reports were registered in the FPVDB and included in the present study corresponding to 60 patients (50 % male) aged from 0.1 to 18.0 years (median age, 9 years). Use of PMSI database increased number of ADR reports by 30 %.
Characteristics of ADRs
Figure 1 shows the distribution of ADRs by decreasing order of frequency of the primary SOC. The most frequent ADRs reported were “musculoskeletal and connective tissue disorders” and “nervous system disorders” for PMSI database and “skin and subcutaneous tissue disorders” and “general disorders and administration site conditions” for FPVDB.
Significant differences in ADR distribution (p < 0.05) were observed: “skin and subcutaneous tissue” and “general disorders” were more frequent in FPVDB reports than in PMSI reports. “Musculoskeletal and connective tissue disorders” were more frequent in PMSI database. The rate of “serious” ADRs was higher in PMSI reports (p < 0.0001).
“Suspected” drug classes
Figure 2 shows the distribution of “suspected” drugs by decreasing order of frequency according to ATC classification (first level). The most frequently suspected drugs were “antineoplastic and immunomodulating agents,” “nervous system drugs” and “systemic hormonal preparations” in PMSI database and “antiinfectives for systemic use,” and “antineoplastic and immunomodulating agents” in FPVDB.
Significant differences in the distribution of ATC classes (p < 0.05) were observed: “systemic hormonal preparations” and ATC “blood” group were more involved in PMSI reports than in FPVDB reports. Anti-infectives were more involved in FPVDB.
Capture–recapture estimates of the number of ADRs
After matching ADRs from the two databases, as previously described, we identified 28 common cases. According to the capture–recapture method, the estimated total number of ADRs was 717 (95 % CI, 513–921). During the study period (from January 2008 to December 2011), the total number of hospital admissions was 118,385. The underreporting coefficient U was estimated to be 3.6 (which means that 72.1 % of cases were not reported). The frequency of ADRs among admissions was 0.6 % (95 % CI 0.4, 0.8), excluding the reports of agranulocytosis and anemia discussed above.
Discussion
Hospital administrative databases
This study relates the quantitative and qualitative interest of the PMSI hospital administrative database for ADR detection in pediatric hospital in comparison with analysis of a PV database, a more common method in drug safety research. Previous studies demonstrated that PMSI hospital databases could be used as another source for identification of ADRs [18, 22, 23] or cases of abuse and dependence [24–26]. Up to now, no studies using this hospital administrative database have been published in children. In fact, few databases have been used previously for pediatric drug safety research and there is a need to fill this gap. The majority of databases are based on outpatient data and all described prescription or drug dispensing data [15]. Computerized monitoring system based on laboratory test results was evaluated for the detection of ADRs on a pediatric ward [14]. The study demonstrated that ADRs can be detected, but the specificity of this method was too low to make it acceptable in daily practice. Moreover, ADRs causing only clinical symptoms were not detected by this approach.
For drug safety studies, a literature survey showed that it is more appropriate to use computerized patient databases because of the available clinical information and the potential to obtain additional information [15]. Another advantage of administrative databases, such as PMSI, is that information is already available about inpatients stays in almost every hospital and in most countries. As previously described, clinical information is encoded according to the ICD-10 codes, including not only codes specifically referring to ADR but also diagnostic codes (that can improve ADR detection). When relevant ICD-10 codes are selected and medical charts computerized, this methodology of ADR detection can reduce time-consuming steps.
There are, however, some limits to this approach. For instance, one possible bias is the “coding creep”, a bias of all billing databases which more expensive codes are preferred and registered to increase the case-mix, diagnosis-related group, and consequently to increase reimbursement of that hospital [27]. Moreover, diagnoses may also be miscoded. PMSI coding is not done by a professional coding staff but by physicians who are not usually trained for this administrative (and not medical) workload.
Finally, the fact that this is a one hospital-centered study can be also a limitation. It may be interesting to perform a similar multicentric study.
Quantitative contribution of PMSI reports
In our study, using PMSI database improved the detection of ADRs: the notifications from pediatric hospital of Toulouse increased by about 30 %. This approach allowed to collect ADRs that would otherwise have not been reported. Compared to the literature, this increase appears to be low. Previous studies comparing spontaneous reporting and screening ICD codes found that more ADRs were identified by ICD codes than were spontaneously reported to a pharmacovigilance structure [28, 29]. Lugardon [18] reported twice many ADRs by interrogating the PMSI database as were reported spontaneously. A Spanish study performed on the minimum basic data set (MBDS), an administrative and clinical information database during hospitalization, and using diagnostic codes showed that implementation of this ADR notification system allowed to increase dramatically the report rate (0.36 reports per 100,000 inhabitants in 2005 to 30.9 per 100,000 inhabitants in 2006 (when the system started) [30]. A more recent study evaluated the same methodology for ADR detection through hospital administrative and clinical database and found a detection rate 46 times higher than the spontaneous reporting [12]. However, it is worth noting that the number of spontaneous reports in the two last studies was particularly low (0.36 reports per 100,000 inhabitants and 7 reports for a year, respectively). Moreover, as none of these studies were performed in pediatric patients, comparison of results may be not accurate.
A limitation of our study is the exclusion of the codes for “agranulocytosis with chemotherapeutical drugs” and “drug-induced aplastic anemia” with chemotherapeutical which reduced significantly the ADRs reporting rate. The code-creep must also be considered. As previously described in the limits of administrative hospital databases, administrative coding is first generated for reimbursement. A bias toward higher-paying diagnosis-related groups, that do not include ADRs, can frequently occur. The ADR codes are rarely used in practice [16]. A further explanation is the possibility of miscoding. Miscoding can lead to a loss of information and an underestimation of the true impact of ADRs. Another limit in this analysis was the discrepancy between coding and hospital discharge reports found in the 311 cases with no mention of ADR. Thus, to improve coding in PMSI database, the Children’s Teaching Hospital of Toulouse has hired now professional coders. These professionals and the medical staff have been made aware of the importance of reporting ADRs. This approach should be extended to allow the administrative databases to be a tool for monitoring ADRs.
Qualitative contribution PMSI reports
The findings in terms of specific body systems and suspected drugs were expected [3–6]. However, although the number of ADRs described in this study was small, we found that the two approaches detected significant different profiles of ADRs: musculoskeletal ADRs in PMSI database versus cutaneous and general ADRs in FPVDB. Similarly, suspected drugs significantly differ: systemic hormonal preparations and ATC “blood” group in PMSI database versus anti-infectives in FPVDB. This difference was also observed in the rate of “serious” ADRs, twofold higher in PMSI reports. Finally, using two different methodologies to detect ADRs, such as PMSI database and spontaneous ADR reports, allows us to detect complementary data and to provide better information on security of drug use in children.
Incidence of ADRs in a pediatric hospital: capture–recapture method
The capture–recapture method represents a helpful tool for estimating incidence when several sources of information are available and can be matched. Its application is easy and the principles of calculation are simple. This method was previously used to assess the incidence of serious ADRs in hospitalized patients using PMSI database and spontaneous reports recorded in the French Pharmacovigilance database [18]. In our study performed in hospitalized pediatric patients, the incidence of ADRs was estimated at 0.6 %. A recent systematic review on ADRs in hospitalized children found a large variation in the estimation of incidence rates reported: from 0.6 to 16.8 % [5]. Comparing ADR incidence rates is complex because the studies differ in a number of ways: data collection approaches (spontaneous reports, prospective studies,….), off-label medicine use, population characteristics, or study duration. A lower incidence of ADRs in children was mainly found in national pharmacovigilance databases that are characterized by an important under-reporting, higher in the pediatric population than in the adults [11]. Since most of hospitalized children suffered from severe diseases, doctors can also be less sensitive to ADRs. The under-reporting and the previously described methodological limitations of our study, such as exclusion of agranulocytosis, can explain this low incidence.
Conclusion
Use of PMSI database improves from around 30 % detection of ADRs in children. In comparison with classical pharmacovigilance database, it also allows to detect different ADRs and drugs. Finally, merging data from these two different databases could improve knowledge of ADRs in children, and should be used complementary for children safety enhancement.
References
Aagaard L, Christensen A, Hansen EH (2010) Information about adverse drug reactions reported in children: a qualitative review of empirical studies. Br J Clin Pharmacol 70:481–491
Choonara I (2013) Educational paper: aspects of clinical pharmacology in children (2013) pharmacovigilance and safety. Eur J Pediatr 172:577–580
Gallagher R, Mason J, Bird K, Kirkham J, Peak M, Williamsom P, Nunn A, Turner M, Pirmohamed M, Smyth R (2012) Adverse drug reactions causing admission to a paediatric hospital. PloS One 7:e50127
Impicciatore P, Choonara I, Clarkson A, Provasi D, Pandolfini C, Bonati M (2001) Incidence of adverse drug reactions in paediatric in/out patients: a systematic review and meta-analysis of prospective studies. Br J Clin Pharmacol 52:77–83
Smyth RMD, Gargon E, Kirkham J, Cresswell L, Golder S, Smyth R, Williamson P (2012) Adverse drug reactions in children—a systematic review. PloS One 7:1–24
Johann-Liang R, Wyeth J, Chen M, Cope J (2009) Pediatric drug surveillance and the food and drug administration’s adverse event reporting system: an overview of reports, 2003–2007. Pharmacoepidemiol Drug Saf 18:24–27
Autret-Leca E, Marchand MS, Cissokoa H, Beau-Salinas F, Jonville-Bera AP (2012) Pharmacovigilance in children. Arch Pediatr 19:848–855
Horen B, Montastruc JL, Lapeyre-Mestre M (2002) Adverse drug reactions and off-label drug use in paediatric outpatients. Br J Clin Pharmacol 54(6):665–670
Milne CP, Davis J (2014) The pediatric studies initiative: after 15 years have we reached the limits of the law? Clin Ther 95(1):98–109
Haslund-Krog S, Mathiasen R, Christensen HR, Holst H (2014) The impact of legislation on drug substances used off-label in paediatric wards—a nationwide study. Eur J Clin Pharmacol 70(4):448–452
Aagaard L, Weber CB, Hansen EH (2010) Adverse drug reactions in the paediatric population in Denmark: a retrospective analysis of reports made to the Danish Medicines Agency from 1998 to 2007. Drug Saf 33:327–339
Miguel A, Azevedo LF, Lopes F, Freitas A et al (2013) Methodologies for the detection of adverse drug reactions: comparison of hospital databases, charts review and spontaneous reporting. Pharmacoepidemiol Drug Saf 22:98–102
Martin-Latry K, Bégaud B (2010) Pharmacoepidemiological research using French reimbursement databases: yes we can! Pharmacoepidemiol Drug Saf 19:256–265
Neubert A, Doormann H, Weiss J, Criegge-Rieck M, Ackermann A, Levy M, Brune K, Rasher W (2006) Are computerised monitoring systems of value to improve pharmacovigilance in paediatric patients? Eur J Clin Pharmacol 62:959–965
Neubert A, Sturkenboom MC, Murray ML, Verhamme KM, Nicolosi A, Giaquinto C, Ceci A, Wong IC, TEDDY Network of Excellence (2008) Databases for pediatric medicine research in Europe—assessment and critical appraisal. Pharmacoepidemiol Drug Saf 17:1155–1167
Bates DW, Evans RS, Murff H, Stetson PD, Pizziferri L, Hripcsak G (2003) Detecting adverse events using information technology. J Am Med Inform Assoc 10:115–128
Tavassoli N, Duchayne E, Sadaba B, Desboeuf K, Sommet A, Lapeyre-Mestre M, Muoz MJ, Sie P, Honorato J, Montastruc JL, Bagheri H (2007) Detection and incidence of drug-induced agranulocytosis in hospital: a prospective analysis from laboratory signals. Eur J Clin Pharmacol 63:221–228
Lugardon S, Desboeuf K, Fernet P, Montastruc JL, Lapeyre-Mestre M (2006) Using a capture-recapture method to assess the frequency of adverse drug reactions in a French university hospital. Br J Clin Pharmacol 62:225–231
Begaud B, Evreux JC, Jouglard J, Lagier G (1985) Imputation of the unexpected or toxic effects of drugs. Actualization of the method used in France. Therapie 40:111–118
Edwards IR, Aronson JK (2000) Adverse drug reactions: definitions, diagnosis, and management. Lancet 356:1255–1259
Gallay A, Nardonnel A, Vaillant V, Desenclos JC (2002) The capture-recapture applied to epidemiology: principles, limits and application. Rev Epidemiol Sante Publique 50:219–232
Weill A, Païta M, Tuppin P, Fagot JP, Neumann A, Simon D, Ricordeau P, Montastruc JL, Allemand H (2010) Benfluorex and valvular heart disease: a cohort study of a million people with diabetes mellitus. Pharmacoepidemiol Drug Saf 19:1256–1262
Couffignal AL, Lapeyre-Mestre M, Bonhomme C, Bugat R, Montastruc JL (2000) Adverse effects of anticancer drugs: a propos of a pharmacovigilance study at a specialized oncology institution. Therapie 55:635–641
Jouanjus E, Leymarie F, Tubery M, Lapeyre-Mestre M (2011) Cannabis-related hospitalizations: unexpected serious events identified through hospital databases. Br J Clin Pharmacol 71:758–765
Jouanjus E, Pourcel L, Saivin S, Molinier L, Lapeyre-Mestre M (2012) Use of multiple sources and capture-recapture method to estimate the frequency of hospitalizations related to drug abuse. Pharmacoepidemiol Drug Saf 21:733–741
Daveluy A, Miremont-Salamé G, Kostrzewa A, Couret A, Lacoin L, Lecomte C, Moore N, Gilleron V, Haramburu F (2012) Identification of abuse and dependence cases through a hospital database. Pharmacoepidemiol Drug Saf 21:1344–1349
Seiber EE (2007) Physician code creep: evidence in Medicaid and State Employee Health Insurance billing. Health Care Financ Rev 28:83–93
Cox AR, Anton C, Goh CHF, Easter M, Langford NJ, Ferner RE (2001) Adverse drug reactions in patients admitted to hospital identified by discharge ICD-10 codes and by spontaneous reports. Br J Clin Pharmacol 52:337–339
Lapeyre-Mestre M, Gary J, Machelard-Roumagnac M, Bonhomme C, Bugat R, Montastruc JL (1997) Incidence and cost of adverse drug reactions in a French cancer institute. Eur J Clin Pharmacol 53:19–22
Salmeron-Garcia A, Cabeza Barrera J, Vergara Pavon MJ et al (2012) Detection of adverse drug reactions through the minimum basic data set. Pharm World Sci 32:322–328
Acknowledgments
We would like to thank Charlotte Benzina, Lucie Cantaloube, and Caroline Rossard for data collection.
Conflict of interest
The authors declare that they have no conflict of interest
Author contributions
Dr Durrieu conceptualized and supervised the study, drafted the initial manuscript, and reviewed and revised the manuscript. Dr Batz designed the study and carried out the initial data analysis. Dr Rousseau carried out the final analysis and reviewed the manuscript. Dr Bondon-Guitton contributed to the concept and the design of the study and reviewed the manuscript. Dr Petiot contributed to the concept of the study, extracted data from the administrative hospital database, and reviewed the manuscript. Pr Montastruc reviewed and revised the manuscript. All authors approved the final manuscript as submitted.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Durrieu, G., Batz, A., Rousseau, V. et al. Use of administrative hospital database to identify adverse drug reactions in a Pediatric University Hospital. Eur J Clin Pharmacol 70, 1519–1526 (2014). https://doi.org/10.1007/s00228-014-1763-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-014-1763-1