Abstract
Purpose
The existence of gender differences in the management of statin therapy among patients with chronic heart failure (HF) is still poorly investigated. We aimed at exploring the effect of gender on statin prescription rates and adequacy of dosing and on the association between statin therapy and all-cause 1-year mortality, after HF hospitalization in a community setting.
Methods
Statin prescription rates, adequacy of dosing (estimated as a PDD/DDD ratio >0.80), and 1-year mortality were retrospectively assessed in 2088 consecutive patients discharged from 5 local community hospitals with a definite diagnosis of HF after a mean length of stay of 7.6 days. The effect of gender was explored using multivariable logistic and Cox analyses adjusting to confounders.
Results
Women showed a lower statin prescription rate (25.7 vs 35.3 %, P < 0.0001) and a lower prevalence of adequate statin dose (32.6 vs 42.3 %, P < 0.0001) than men. Female gender was independently associated with a 24 % lower probability of statin prescription and a 48 % higher probability of inadequate statin dose. Statin prescription and adequacy of dosing were associated with 35 and 44 % decreases in the risk of 1-year mortality, respectively, irrespective of gender. A nested case/control analysis confirmed that adequate statin dose was associated with 48 % lower 1-year mortality, again without interaction with gender.
Conclusions
In patients with chronic HF, female gender is independently associated with lower statin prescription rates and higher probability of inadequate dose. Statin therapy in these subjects is associated with improved 1-year survival in both men and women. This prognostic benefit is not affected by gender.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last years, the prognostic role of statin therapy in patients with chronic heart failure (HF) has been largely debated. An improved clinical outcome associated with statin therapy was reported by several studies in the overall HF population [1] and in various HF subcategories, including severe HF [2], HF with preserved ejection fraction [3], ischemic HF [4], non-ischemic HF [5], and HF in the elderly [6]. However, two large randomized controlled trials showed that rosuvastatin therapy did not improve clinical outcome in subjects with systolic HF [7, 8]. The results of these two trials were challenged by two metanalyses that confirmed that statins may reduce clinical symptoms, improve cardiac function, and favour ventricular remodelling in patients with systolic HF, suggesting that a reduction in mortality and rehospitalisation in these patients can be observed in particular subsets, namely those under 65 years and those treated with atorvastatin [9, 10]. In addition, a recent collaborative metaanalysis of unpublished data from major randomized trials found that statins reduced the risk of HF death and non-fatal HF hospitalization, independently on the underlying ischemic etiology [11].
Based on these considerations, assessing the potential existence of gender differences in statin prescription rate among HF patients may be of potential clinical interest. The rationale for this analysis is based on previous evidences reporting a tendency towards lower prescription rates in women than men for several cardiovascular medications in different settings [12, 13]. However, available data for patients with HF are limited to two studies that analysed the unadjusted prevalence of prescriptions for several agents, reporting opposite results for the comparison of statin prescription rates between men and women [14, 15]. A focused gender comparison of statin prescription rate in this population, adjusting for expected confounding variables, has not been critically evaluated. Moreover, the impact of gender on the adequacy of statin dose in HF patients has still not been investigated.
The aim of this study was to investigate gender differences in statin prescription rate and adequacy of dosing, and in the association of statin therapy with overall 1-year mortality, in a large cohort of hospitalized subjects discharged with a diagnosis of HF.
Material and methods
Study population
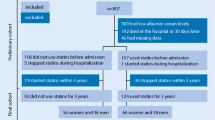
-
All residents in the geographic area of the Local Health Authority of Florence, Italy, consecutively discharged over a 12-month period from 5 local community hospitals with a definite diagnosis of HF and who remained alive 30 days after discharge, were included in this study. The Local Health Authority of Florence is the largest health authority of Tuscany, provides care for 850,000 inhabitants, and includes four high-volume hospitals with full cardiac interventional capabilities and two low-volume peripheral hospitals with non-invasive cardiologic services. For unambiguous definition of HF diagnosis, subjects were identified through the Regional Hospital Discharge System by considering an International Classification of Diseases - 9th revision, clinical modification (ICD-9 CM) discharge code 428, corresponding to HF.
Prescriptions and adequacy of dosing
Data on statin prescriptions were obtained from the Local Pharmaceutical Service database, which systematically monitors all pharmacological prescriptions by local physicians and collects all records from local pharmacies in the Florence area. For the assessment of adequacy of statin dose, we considered the ratio between the prescribed daily dose (PDD) and the defined daily dose (DDD). The PDD corresponds to the average daily dose actually prescribed to the patient, calculated on the basis of the number of pharmacological prescriptions over a given span of time [16]. The DDD of a drug is a measure of consumption corresponding to the assumed average maintenance dose per day in adults [17]. The PDD/DDD ratio is often used in cohort studies as a surrogate measure for adequacy of dosing. For the calculation of PDD/DDD ratio, we adopted the following DDD values in accordance with WHO recommendations [18]: atorvastatin, 20 mg; rosuvastatin, 10 mg; fluvastatin, 60 mg; lovastatin, 45 mg; pravastatin and simvastatin, 30 mg. As previously described, we considered a PDD/DDD ratio <0.80 as an index of inadequate dose, suggesting poor adherence to therapy [19].
Clinical outcome
The predefined clinical endpoint of this study was all-cause mortality at 1 year after discharge. Information on vital status was obtained by consulting the Florence Registry Office, which collects complete and updated records of all subjects living within city boundaries. For those who had moved away, specific queries were sent to the Registry Office of the new city of residence.
Statistical analysis
Data were expressed as median (interquartile range) for continuous variables and number (percentage) for categorical variables. Comparisons of variables were performed using the Mann-Whitney U test or the chi-square test, as appropriate. The inclusion of patients who were still alive 30 days after discharge was predefined to account for the risk of immortal time bias. Logistic regression models were used to explore the determinants of statin prescription and adequacy of dosing. The model goodness-of-fit was assessed using the Hosmer-Lemeshow test [20]. Cox proportional hazard regression models were built to explore the independent impact of statin use on 1-year mortality. Risk-adjusted event-free survival curves were plotted using separate Cox models for males and females. The proportional hazard assumption and model goodness-of-fit were tested using the methods of Grambsch-Therneau [21] and May-Hosmer [22], respectively. All covariates listed in Table 1, showing a p < 0.10 in univariable analyses, were tested into multivariable models (logistic or Cox regression) using a forward selection procedure.
An additional analysis was obtained using a nested case-control study. For each death, three controls were randomly chosen from those members of the cohort who were alive at the failure time of the case, considering age quartiles and propensity score deciles as matching criteria. The propensity score was calculated for each patient by multivariable logistic regression, including all significant predictors of statin use at baseline (shown in Table 2) without regard to clinical outcome. The significance level was set at 0.05. All tests were two-tailed. Analyses were performed using Stata statistical package (version 11.0, Stata Corporation, Texas, 2009).
Results
General characteristics
A total of 2088 patients (50.7 % women) met the selection criteria and entered the study population. Baseline characteristics at discharge are shown in Table 1. Compared to women, men were younger and showed a significantly higher prevalence of comorbidities, including hyperlipemia, diabetes mellitus, coronary artery disease, chronic kidney disease, peripheral artery disease, and chronic obstructive pulmonary disease. Men also showed higher prevalences of percutaneous coronary intervention and discharge from cardiologic departments during the index hospitalization. Beta/blockers and antiplatelet agents were more commonly prescribed in men than women, whereas prescription of nitrates was more common in women.
Gender and statin prescriptions
Overall, 643 subjects (248 women, 38.6 %) received statin prescriptions during the period of study. Statins were prescribed more frequently in men (38.4 %, 95 % confidence interval (CI) 35.4, 41.4) than women (23.4 %, 95 % CI 20.4, 26.0; P < 0.0001). This difference was still evident using age-adjusted rates (men 35.3 %, 95 % CI 32.5, 38.2; women 25.7 %, 95 % CI 23.0, 28.4; P < 0.0001) and was consistently observed across all age classes (Supplementary file 1). Univariable logistic regression showed that female gender was associated with a reduced probability of statin prescription (odds ratio 0.49, 95 % CI 0.41, 0.59; P < 0.0001). In a multivariable logistic model adjusting for confounders, female gender remained independently associated with a 24 % lower probability of statin prescription (Table 2).
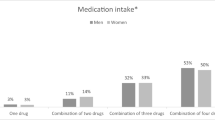
Gender and adequacy of statin dose
In the group of patients who received statin prescriptions, the proportion of subjects prescribed with adequate statin dose was lower in women than men (Fig. 1). Multivariable logistic analysis confirmed that female gender was independently associated with a 48 % relative increase in the risk of inadequate statin dose (Table 2).
Gender, statins, and clinical outcome
In the study population, cardiovascular death accounted for 57.2 % of all deaths observed over the 1-year follow-up (53.4 % in men vs 61.5 % in women, p < 0.0001). Multivariable Cox regression adjusting for confounders showed that statin prescription was independently associated with a relative 35 % decrease in the risk of death at 1 year (hazard ratio 0.65, 95 % CI 0.51, 0.83; P < 0.001). Gender showed no association with the clinical endpoint (hazard ratio 0.89, 95 % CI 0.75, 1.07; P = 0.22), and no interaction between gender and statin prescription was found. Adjusted survival curves showing the impact of statin prescription on clinical outcome in men and women are shown in Fig. 2.
When a similar model was built by substituting statin prescription with adequacy of statin dose among the independent variables, an adequate statin dose was associated with a 44 % relative reduction in the risk of death at 1 year (Table 3). Again, gender showed no association with outcome (hazard ratio 0.89, 95 % CI 0.74, 1.07; P = 0.20), and no interaction between gender and adequacy of statin dose was found. The nested case/control analysis confirmed that adequate statin dose was associated with a 48 % lower 1-year mortality, with no independent association of gender with outcome and no evidence of gender-adequacy of dosing interaction.
The overall prevalence of rehospitalization during the follow-up was 51.3 %. This prevalence was lower among patients who received than those who did not receive statin prescriptions (45.9 vs 61.4 %, p < 0.0001). In stepwise multivariable Cox analysis, only age (hazard ratio 1.008, 95 % CI 1.002, 1.014, p = 0.013) and chronic pulmonary obstructive disease (hazard ratio 1.26, 95 % CI 1.10, 1.45; P = 0.0010) were found to be independent predictors of rehospitalization, with no effect of either statin treatment or gender.
Discussion
Main findings
This study explored gender differences in statin prescription rate, adequacy of statin dose, and the association between statin therapy and clinical outcome in a cohort of hospitalized patients discharged with a diagnosis of HF. Our results showed that in this population: (1) female gender was independently associated with a reduced probability of statin prescription and a higher probability of inadequate statin dose; (2) statin therapy and adequate statin dose were associated with improved 1-year survival independently of gender.
Impact of gender on statin prescription rate and adequacy of dosing
Two studies previously explored gender differences in the rate of statin prescription among patients with HF, providing conflicting data. In the GIPSI study [14], an Italian registry that collected data on 530 patients considered at risk for HF and 227 patients with overt HF in a primary care setting, the unadjusted rate of statin prescription in women was found to be lower than that observed in men among patients at risk for HF (5.6 vs 12.4 %), but higher than that observed in men among patients with overt HF (17.9 vs 10.5 %). Another study, retrospectively performed on 206 men and 94 women consecutively admitted with a primary diagnosis of HF to a tertiary care hospital, reported a higher in-hospital prescription rate of statins in men than women (48.5 vs 22.3 %) [15]. Both studies were designed to provide data about the prescription rates of major pharmacological classes in men and women with HF with no specific focus on statins and did not explore the independent impact of gender by adjusting analyses for the observed clinical differences between the female and male population with HF. As a novel contribution, we found that female gender was associated with lower probability of statin prescriptions in a large cohort of hospitalized patients discharged with a diagnosis of HF and that this difference was independent of confounders including age, clinical variables, and concomitant cardiovascular therapy. These findings agree with previous evidence showing that significant gender discrepancies in the management of patients with cardiovascular diseases still exist and that women are less likely to receive appropriate diagnostic examinations and prescriptions of evidence-based medications than men [23–25].
Our findings also provide evidence of an independent association between female gender and reduced probability of adequate statin dose in HF patients. This result may be in accordance with previous reports of lower adherence to guideline-recommended therapies among women than men in other cardiovascular settings [26, 27]. In this regard, it should be considered that poor adherence to statin therapy depends on complex interaction between patient’s and physician’s attitudes, comorbidities potentially affecting statin intolerance, ageing, clinical inertia, co-existence of coronary artery disease, family history of cardiovascular events, type of statin, and socioeconomic factors including the levels of co-payments, their changes over time, the cost and type of medication (e.g. generic or branded), the availability of alternative drugs, and the level of health services utilization [28–30]. Age and comorbidities, in particular, can favour the probability of adverse effects of statins, particularly at high dose, potentially leading physicians to avoid statin prescriptions or to prescribe them at low doses, and patients to interrupt treatment or to self-reduce the medication dose. However, it is interesting to note that in our population, women were older but showed lower prevalences of comorbidities as compared to men. On the other hand, in our population, women also showed lower prevalences of hyperlipemia and coronary artery disease, which are common indications to statin treatment in daily practice. Although the effect of gender in our population was found to be independent from these variables, it cannot be excluded that a residual confounding effect might have favoured lower prescription rates and inadequate doses in women.
Impact of gender on the association between statin therapy and outcome
In our population of patients with HF, we found that not only statin prescription but also the adequacy of statin dose was independently associated with more favourable clinical outcome and that these associations were not affected by gender. It should also be stressed that as a result of the retrospective and observational nature of our analysis, the prognostic benefit observed in this study must be considered with caution. The prognostic value of statin therapy in patients with HF is still controversial, and inconsistencies across studies are likely to be affected by a high variability in several key factors, including age of the study population, HF etiology distribution, proportion of HF patients with preserved or reduced ejection fraction, prevalence of hyperlipemia, specific statin considered in the study, concomitant medications, differences in the exclusion criteria, and potential confounding role of different types of bias [31]. Regardless of these discrepancies, several mechanisms have been proposed to explain the existence of a potential benefit associated with statin therapy in patients with HF, including anti-inflammatory properties, neurohormonal modulation, restoration of endothelial function, and favourable electrophysiological changes [32–34]. With this in mind, our findings might suggest that a potential prognostic benefit of statin therapy in HF patients could occur independently of the established gender differences in the pathophysiology and clinical features of chronic HF and in the lipoprotein responses to statins [35]. This may be in accordance with previous evidence showing that in secondary prevention, statins are equally effective in both genders [36].
Clinical implications and study limitations
From a practical point of view, the findings of this study suggest that physicians should give particular attention to evaluate the potential indication for statin prescription in women with HF and to correctly identify the adequate dose. Also, searching for ways to encourage female patients to persist with statin therapy might also contribute to fill the gap related to lower adherence to therapy. This may be of particular importance after initiation of statin therapy, as recent evidence suggests that the decision on long-term continuation of statin use is often taken during the first year of treatment [37]. Moreover, since statin prescription and adequate dose were both associated with better outcome in our study population, a prognostic benefit might be expected by appropriate interventions aimed at motivating physicians to consider patient’s compliance as a clinically relevant target, and patients to adequately assume therapy and correctly interpret potential adverse drug reactions [38]. The practical utility of prediction models for the identification of patients with high risk of non-adherence to statin therapy could also be taken into account [39]. On the other hand, it should be considered that successful implementation of strategies aimed at improving patients’ adherence to their statin medication may not be easy to obtain in the real world [40]. Moreover, considering the lower baseline risk of cardiovascular disease in women and the potential increase in the risk of cognitive impairment, insulin resistance, and type-2 diabetes related to statin therapy [41], it may be reasonable to take into account the cost-effectiveness of these strategies [42] and to base treatment decisions on the level of cardiovascular risk as recommended by current guidelines [43, 44]. Lastly, it should be pointed out that some studies previously found that lowering cholesterol levels might not be beneficial but could even increase mortality in chronic HF [45, 46]. This strictly suggests that the role of statins in these patients is worthy of further exploration.
Several limitations should be considered in this study. This study was carried out in a single Italian region so that caution is required to generalize findings to other settings and populations. We only considered all-cause 1-year mortality as the clinical endpoint. Extending the analyses to other endpoints such as cardiac rehospitalization and the amount of primary care would have been of clinical interest. We were not able to assess the prevalence of adverse effect to statins or surrogate measures—e.g. the number of orthopaedic consultations related to symptoms believed to depend on bone-related pain, but actually related to statin-induced myositis—which may have played a role in affecting gender discrepancies. Other important variables involved in affecting the probability of statin therapy or in the prognostic benefit of statins—e.g. a family history of coronary artery disease or the temporal trend of C-reactive protein levels—were not available in our database. This study was not powered enough to allow for analyses in subsets with different types of HF (e.g. reduced vs preserved ejection fraction). Differences in pharmacokinetic aspects, efficacy, and tolerability exist between different statins [47]. Assessing the impact of gender on the prescription rate and adequacy of dosing for different statins would have provided further information, but the sample size of our study precluded this additional analysis. In our study, we did not consider the use of other lipid lowering agents since statins are the most commonly medications used to lower cholesterol in our region. However, the prevalence of use of statins and other lipid lowering agents might be different in other Countries. Lastly, other indexes of therapeutic adherence and compliance to therapy (e.g. self-reported questionnaires) would have been useful to better explore the impact of gender on statin prescription patterns.
In conclusion, in a population of patients discharged with a diagnosis of chronic HF, female gender was independently associated with lower statin prescription rates and higher probability of inadequate dose. Statin therapy in these subjects was associated with improved 1-year survival in both men and women. This prognostic benefit was not affected by gender.
References
Go AS, Lee WY, Yang J et al (2006) Statin therapy and risks for death and hospitalization in chronic heart failure. JAMA 296:2105–11
Mozaffarian D, Nye R, Levy WC (2004) Statin therapy is associated with lower mortality among patients with severe heart failure. Am J Cardiol 93:1124–9
Shah R, Wang Y, Foody JM (2008) Effect of statins, angiotensin-converting enzyme inhibitors, and beta blockers on survival in patients > or = 65 years of age with heart failure and preserved left ventricular systolic function. Am J Cardiol 101:217–22
Cleland JG, McMurray JJ, Kjekshus J, CORONA Study Group et al (2009) Plasma concentration of amino-terminal pro-brain natriuretic peptide in chronic heart failure: prediction of cardiovascular events and interaction with the effects of rosuvastatin: a report from CORONA (Controlled Rosuvastatin Multinational Trial in Heart Failure). J Am Coll Cardiol 54:1850–9
Domanski M, Coady S, Fleg J et al (2007) Effect of statin therapy on survival in patients with nonischemic dilated cardiomyopathy (from the Beta-blocker Evaluation of Survival Trial [BEST]). Am J Cardiol 99:1448–50
Foody JM, Shah R, Galusha D et al (2006) Statins and mortality among elderly patients hospitalized with heart failure. Circulation 113:1086–92
Kjekshus J, Apetrei E, Barrios V et al (2007) Rosuvastatin in older patients with systolic heart failure. N Engl J Med 357:2248–61
Tavazzi L, Maggioni AP, Marchioli R et al (2008) Effect of rosuvastatin in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet 372:1231–9
Zhang L, Zhang S, Jiang H et al (2011) Effects of statin treatment on cardiac function in patients with chronic heart failure: a meta-analysis of randomized controlled trials. Clin Cardiol 34:117–23
Zhang S, Zhang L, Sun A et al (2011) Efficacy of statin therapy in chronic systolic cardiac insufficiency: a meta-analysis. Eur J Intern Med 22:478–84
Preiss D, Campbell RT, Murray HM et al (2015) The effect of statin therapy on heart failure events: a collaborative meta-analysis of unpublished data from major randomized trials. Eur Heart J 36:1536–46
Smolina K, Ball L, Humphries KH, Khan N, Morgan SG (2015) Sex disparities in post-acute myocardial infarction pharmacologic treatment initiation and adherence: problem for young women. Circ Cardiovasc Qual Outcomes
Lauffenburger JC, Robinson JG, Oramasionwu C, Fang G (2014) Racial/ethnic and gender gaps in the use of and adherence to evidence-based preventive therapies among elderly Medicare Part D beneficiaries after acute myocardial infarction. Circulation 129:754–63
Gronda E, Aronica A, Visconti M et al (2010) Gender differences of at risk patients with overt heart failure in the real world of general practice. Data from the GIPSI (Gestione Integrata Progetto Scompenso in Italia) registry. G Ital Cardiol 11:233–8
Assiri AS (2011) Effect of gender difference in management of heart failure patients in Aseer, Saudi Arabia. Heart Views 12:18–21
Hartz I, Sakshaug S, Furu K et al (2011) Aspects of statin prescribing in Norwegian counties with high, average and low statin consumption—an individual-level prescription database study. BMC Clin Pharmacol 7:14
Deambrosis P, Saramin C, Terrazzani G et al (2007) Evaluation of the prescription and utilization patterns of statins in an Italian local health unit during the period 1994–2003. Eur J Clin Pharmacol 63:197–203
WHO Collaborating Centre for Drug Statistics Methodology. http://www.whocc.no/atcddd/ Accessed August 19th, 2015
Andrade SE, Kahler KH, Frech F et al (2006) Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf 15:565–74
Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S (1997) A comparison of goodness-of-fit tests for the logistic regression model. Stat Med 16:965–80
Grambsch P, Therneau TM (1994) Proportional hazards tests and diagnostics based on weighted residuals. Biometrika 81:515–26
May S, Hosmer DW (1998) A simplified method of calculating an overall goodness-of-fit test for the Cox proportional hazards model. Lifetime Data Anal 4:109–20
Daly C, Clemens F, Lopez Sendon JL, Euro Heart Survey Investigators et al (2006) Gender differences in the management and clinical outcome of stable angina. Circulation 113:490–8
Wallach-Kildemoes H, Hansen EH (2015) Sociodemographic and diagnostic characteristics of prescribing a second-line lipid-lowering medication: ezetimibe used as initial medication, switch from statins, or add-on medication. Eur J Clin Pharmacol
Rosano GM, Lewis B, Agewall S, et al (2015) Gender differences in the effect of cardiovascular drugs: a position document of the working group on pharmacology and drug therapy of the ESC. Eur Heart J
Macías Saint-Gerons D, de la Fuente Honrubia C, Montero Corominas D, Gil MJ, de Andrés-Trelles F, Catalá-López F (2014) Standard and intensive lipid-lowering therapy with statins for the primary prevention of vascular diseases: a population-based study. Eur J Clin Pharmacol 70:99–108
Chaudhry HJ, McDermott B (2008) Recognizing and improving patient nonadherence to statin therapy. Curr Atheroscler Rep 10:19–24
Mauskop A, Borden WB (2011) Predictors of statin adherence. Curr Cardiol Rep 13:553–8
Citarella A, Kieler H, Sundström A et al (2014) Family history of cardiovascular disease and influence on statin therapy persistence. Eur J Clin Pharmacol 70:701–7
Simoens S, Sinnaeve PR (2014) Patient co-payment and adherence to statins: a review and case studies. Cardiovasc Drugs Ther 28:99–109
Danaei G, Tavakkoli M, Hernán MA (2012) Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol 175:250–62
Krum H, Ashton E, Reid C et al (2007) Double-blind, randomized, placebo-controlled study of high-dose HMG CoA reductase inhibitor therapy on ventricular remodeling, pro-inflammatory cytokines and neurohormonal parameters in patients with chronic systolic heart failure. J Card Fail 13:1–7
Sola S, Mir MQ, Lerakis S et al (2006) Atorvastatin improves left ventricular systolic function and serum markers of inflammation in nonischemic heart failure. J Am Coll Cardiol 47:332–7
Strey CH, Young JM, Lainchbury JH et al (2006) Short-term statin treatment improves endothelial function and neurohormonal imbalance in normocholesterolaemic patients with non-ischaemic heart failure. Heart 92:1603–09
Mombelli G, Bosisio R, Calabresi L et al (2015) Gender-related lipid and/or lipoprotein responses to statins in subjects in primary and secondary prevention. J Clin Lipidol 9:226–33
Mercuro G, Deidda M, Bina A, Manconi E, Rosano GM (2011) Gender-specific aspects in primary and secondary prevention of cardiovascular disease. Curr Pharm Des 17:1082–9
Upmeier E, Korhonen MJ, Rikala M, Helin-Salmivaara A, Huupponen R (2014) Older statin initiators in Finland—cardiovascular risk profiles and persistence of use. Cardiovasc Drugs Ther 28:263–72
Chaipichit N, Krska J, Pratipanawatr T, Uchaipichat V, Jarernsiripornkul N (2014) A qualitative study to explore how patients identify and assess symptoms as adverse drug reactions. Eur J Clin Pharmacol 70:607–15
Galema-Boers JM, Lenzen MJ, van Domburg RT et al (2014) Predicting non-adherence in patients with familial hypercholesterolemia. Eur J Clin Pharmacol 70:391–7
Mitka M (2010) Improving medication adherence promises great payback, but poses tough challenge. JAMA 303:825
Planchon SM (2014) Abrogating the induction of type 2 diabetes mellitus secondary to statin therapy. Cardiovasc Drugs Ther 28:393–4
Macchia A, Mariani J, Romero M et al (2015) On the hypothetical universal use of statins in primary prevention: an observational analysis on low-risk patients and economic consequences of a potential wide prescription rate. Eur J Clin Pharmacol 71:449–59
Stone NJ, Robinson JG, Lichtenstein AH, American College of Cardiology/American Heart Association Task Force on Practice Guidelines et al (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63:2889–934
Myerson M, Rosenson RS (2014) 2013 ACC/AHA Guideline: a guideline for the population—without evidence from the population. Cardiovasc Drugs Ther 28:203–4
Horwich TB, Hamilton MA, Maclellan WR, Fonarow GC (2002) Low serum total cholesterol is associated with marked increase in mortality in advanced heart failure. J Card Fail 8:216–24
Rauchhaus M, Clark AL, Doehner W et al (2003) The relationship between cholesterol and survival in patients with chronic heart failure. J Am Coll Cardiol 42:1933–40
Birmingham BK, Bujac SR, Elsby R et al (2015) Impact of ABCG2 and SLCO1B1 polymorphisms on pharmacokinetics of rosuvastatin, atorvastatin and simvastatin acid in Caucasian and Asian subjects: a class effect? Eur J Clin Pharmacol 71:341–55
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental File 1
Prevalences of patients receiving statin prescriptions in the study population, stratified by gender and age class (PPT 37 kb)
Rights and permissions
About this article
Cite this article
Ballo, P., Balzi, D., Barchielli, A. et al. Gender differences in statin prescription rates, adequacy of dosing, and association of statin therapy with outcome after heart failure hospitalization: a retrospective analysis in a community setting. Eur J Clin Pharmacol 72, 311–319 (2016). https://doi.org/10.1007/s00228-015-1980-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1980-2