Abstract
Background
Little is known about the prognosis associated with statin therapy and its gender differences in older adults aged ≥80 years.
Objective
To study the mortality and survival associated with statin therapy and their gender differences in older adults aged ≥80 years.
Method
This was a historical prospective study conducted at a tertiary medical center. The medical charts of all older adults aged ≥80 years who had been admitted to a single internal medicine department during 1 year were reviewed. All-cause 3‑year mortality and survival rates following hospital admission in men and in women using statins were investigated.
Results
The final cohort included 216 patients: 122 (56.5%) women, mean age 85.3 ± 3.9 years. Overall, 66 (53.2%) women and 58 (46.8%) men used statins for 3 years or more following hospital admission. During this time 48 (39.3%) women and 48 (51.1%) men died. The all-cause 3‑year mortality rates were significantly lower only in women who had used statins compared with women who had not used statins (24.2% vs. 57.1%; relative risk = 0.2; 95% confidence interval 0.1–0.5; p < 0.0001). The 3‑year cumulative survival rates were significantly higher in women who had used statins as part of primary as well as secondary cardiovascular prevention (p < 0.0001 and p = 0.014, respectively). A Cox regression analysis showed that statin therapy was independently associated with low 3‑year cumulative mortality rates in women (hazard ratio=0.3; 95% confidence interval=0.1–0.6; p = 0.001).
Conclusion
In older adults aged ≥80 years, statin therapy is associated with high 3‑year cumulative survival rates only in women.
Zusammenfassung
Hintergrund
Über die mit einer Statintherapie assoziierte Prognose und die Geschlechtsunterschiede bei älteren Menschen (≥80 Jahre) ist wenig bekannt.
Ziel
Ziel war es, die Mortalitäts- und Überlebensrate sowie die Geschlechtsunterschiede bei einer Statintherapie bei älteren Menschen (≥80 Jahre) zu untersuchen.
Methode
Eine historische prospektive Studie wurde in einem tertiären medizinischen Zentrum durchgeführt. Es erfolgte die Überprüfung der Patientenakten aller älteren Patienten (≥80 Jahre), die im 1. Jahr einer einzelnen Abteilung für Innere Medizin zugewiesen wurden. Die 3‑Jahres-Mortalität jeglicher Ursache und die Überlebensraten nach Krankenhauseinweisung bei Männern und Frauen, die Statine einnahmen, wurden untersucht.
Ergebnisse
In die finale Kohorte wurden 216 Patienten eingeschlossen, davon 122 (56,5%) Frauen (mittleres Alter: 85,3 ± 3,9 Jahre). Insgesamt nahmen 66 (53,2%) Frauen und 58 (46,8%) Männer Statine für 3 Jahre oder länger nach einer Krankenhauseinweisung ein. Während dieser Zeit starben 48 (39,3%) Frauen und 48 (51,1%) Männer. Die 3‑Jahres-Mortalitätsrate jeglicher Ursache war nur bei Frauen, die Statine einnahmen, signifikant geringer als bei Frauen, die keine Statine einnahmen (24,2% vs. 57,1%; relatives Risiko: 0,2; 95% Konfidenzintervall [CI] 0,1–0,5; p < 0.0001). Die kumulative Überlebensrate war signifikant höher bei Frauen, die als Teil der kardiovaskulären Primär- und Sekundärprävention Statine einnahmen (p < 0,0001 bzw. p = 0,014). Eine Cox-Regressionsanalyse zeigte, dass eine Statintherapie unabhängig mit einer geringeren 3‑Jahres-Mortalitätsrate bei Frauen assoziiert war (Hazard-Ratio 0,3; 95% CI 0,1–0,6; p = 0,001).
Schlussfolgerung
Bei älteren Menschen (≥80 Jahre) ist eine Statintherapie nur bei Frauen mit einer hohen kumulativen 3‑Jahres-Überlebensrate assoziiert.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Statin therapy as part of primary and secondary cardiovascular prevention is associated with a better prognosis in adults [1]; however, very little is known about the prognosis associated with statin therapy in older adults aged 75–80 years or more, namely very old patients [2]. In this population, which is characterized by a decreased life expectancy and high number of chronic comorbidities, there are uncertainties regarding the cardiovascular risk, so that there is a need to balance the theoretical yet unproven benefits of the cardiovascular risk reduction with that of polypharmacy and statin-associated adverse events. Considering the aging of the world’s population and the disseminated use of statins, there is a clear need to demonstrate the benefits of statin therapy in very old patients.
Guidelines concerning statin therapy in older adults aged 75 years or more are vague due to conflicting evidence. Although five observational studies demonstrated an association between statin therapy and decreased all-cause mortality rates in older adults aged 75–80 years or more [3,4,5,6,7], one observational study failed to show a survival benefit from the use of statins in this population [8] and two randomized controlled trials (RCTs) had conflicting findings in slightly younger patients aged 70 years or more [9, 10]. In the clinical practice, therefore, decisions regarding statin therapy in very old patients are often left to the physician’s preference. Notably, some physicians believe that it is reasonable to prescribe statins in very old patients only if they are well-nourished. Since the early 1990 s more women and older adults have been included in RCTs concerning the prognosis associated with statin therapy [11]; however, to the best of our knowledge there are no RCTs or observational studies concerning gender differences in mortality among statin users aged 75–80 years or more.
Aim of the study
In this observational study we sought to evaluate the association between statin therapy and 3‑year mortality/survival rates in men and in women aged 80 years or more with a special emphasis on well-nourished patients.
Ethics approval
This was a historical prospective study conducted at Sheba medical center, the largest tertiary medical center in Israel. The study was approved by the local ethics committee.
Methods
Inclusion and exclusion of patients
The preliminary cohort included all (n = 807) older adults aged 80 years or more who had been admitted to a single internal medicine department (Internal Medicine E) during 1 year between January and December 2010. In the case of readmissions during that year, only the first admission was included in the analysis. All of the patients had at least another admission or an outpatient clinic visit to Sheba Medical Center within the following 3 years in which compliance to statin therapy (in statin users) or a lack of statin therapy (in patients who had not been using statins following their admission) was confirmed.
The following patients were excluded: 300 (37.2%) patients had low (<3.5 g/dl) albumin serum levels, 192 (23.8%) patients died during hospitalization or within 30 days of discharge, 46 (5.7%) patients had missing data, 34 (4.2%) statin users stopped statins within the following 3 years and 19 (2.4%) patients who had not used statins following admission started statin therapy within the following 3 years (Fig. 1). The final cohort included well-nourished older adults aged 80 years or more who had used statins (study group) or not (control group) for 3 years or more following admission.
Data
The medical charts were reviewed for the following data: age, gender, chronic comorbidities, total cholesterol (TC) serum levels, albumin serum levels, statin therapy intensity and the indications for statin therapy. The TC and albumin serum levels were routinely measured in all of the patients during hospitalization. The indications for statin therapy were classified into primary or secondary cardiovascular prevention. The secondary cardiovascular prevention group included statin users with a history of ischemic heart disease, peripheral vascular disease or stroke. All other statin users, including diabetic patients, were included in the primary cardiovascular prevention group. Statin therapy intensity was consistent with the most recent guidelines of the American Heart Association (AHA) [12]. The all-cause 3‑year mortality rates and cumulative survival rates following admission were studied using the database of the Israeli general register office.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation, median, and interquartile range (IQR). Student’s t‑test was used to compare between the mean values of continuous variables with parametric distribution, and the Mann-Whitney test was used to compare the mean values of continuous variables with non-parametric distributions. The χ2-test was used to compare between the incidence/prevalence of categorical variables. The Kaplan-Meier test was used to compare 3‑year cumulative survival rates between men and women, with and without statin therapy and as part of primary cardiovascular prevention versus secondary cardiovascular prevention. A Cox regression analysis was used to study if statin therapy was independently associated with 3‑year cumulative mortality.
Propensity score matching was performed separately in men and in women in order to control for differences in baseline clinical characteristics between patients with and without statin therapy. A logistic regression analysis was used in order to calculate the probability (propensity score) of each patient to be treated with statins. The logistic regression model included age, all chronic comorbidities, and albumin serum levels. A difference of up to 5% in the propensity score was considered adequate for matching. The matched cohorts were compared using the Wilcoxon test for continuous variables and McNemar’s test for categorical variables in order to evaluate differences following the matching process. A stratified Cox regression analysis was used to evaluate the association between statin therapy and mortality in the matched cohorts. A two-tailed p < 0.05 was considered statistically significant. The statistical analyses were carried out using the 24th version of the SPSS statistical software (SPSS, Chicago, IL).
Results
The final cohort included 216 well-nourished older adults aged 80 years or more: 122 (56.5%) women and 94 (43.5%) men. The mean age was 85.3 ± 3.9 years (median=85 years, IQR = 82–88 years) and the mean albumin serum level was 3.8 ± 0.2 g/dl (median=3.8 g/dl; IQR = 3.6–4.0 g/dl). The following chronic comorbidities were the three most prevalent: hypertension, ischemic heart disease, and atrial fibrillation (Table 1).
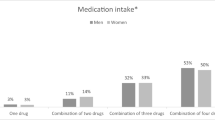
Overall, 124 (57.4%) patients used statins for 3 years or more following admission (study group). Most (n = 86; 69.4%) used moderate intensity statins on hospital discharge, and the rest used low-intensity statins (n = 25; 20.2%) or high-intensity statins (n = 13; 10.5%). Compared with patients who did not use statins (control group), statin users were younger and had a higher prevalence of ischemic heart disease, congestive heart failure, diabetes mellitus, chronic renal failure, and peripheral vascular disease. Patients who used statins also had lower total cholesterol serum levels. Patients who did not use statins had a higher prevalence of dementia (Table 1).
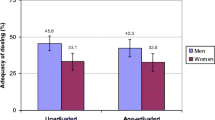
Among the 124 statin users 66 (53.2%) were women and 58 (46.8%) were men (Fig. 1), 37 (56.1%) women used statins as part of primary cardiovascular prevention and 29 (43.9%) women used statins as part of secondary cardiovascular prevention. Most (n = 49; 83.1%) men used statins as part of secondary cardiovascular prevention. Compared with women who did not use statins, women who used statins had a higher prevalence of hypertension and lower prevalence of dementia. Compared with men who did not use statins, men who used statins had a higher prevalence of ischemic heart disease, congestive heart failure, diabetes mellitus, and peripheral vascular disease. Compared with patients who did not use statins, statin users both women and men, were younger and had lower total cholesterol serum levels (Table 1).
Overall, 48 (39.3%) women and 48 (51.1%) men died within 3 years of hospital admission. The all-cause 3‑year mortality rates were significantly lower in women who had used statins compared with women who had not used statins (16 vs. 32 patients; 24.2% vs. 57.1%; relative risk RR 0.2; 95% confidence interval CI 0.1–0.5; p < 0.0001) but not in men who used statins compared with men who had not used statins (31 vs. 17 patients; 53.4% vs. 47.2%; RR 1.2; 95% CI 0.5–2.9; p = 0.672).
The 3‑year cumulative survival rates were significantly higher in women who had used statins compared with women who had not used statins (Fig. 2b) but not in men (Fig. 2a). Following propensity score matching, there were no significant differences in mean age, prevalence of chronic comorbidities, and mean albumin serum levels between 21 men who had used statins compared with 21 men who had not used statins (p > 0.2), as well as in 31 women who had used statins compared with 31 women who had not used statins (p > 0.12). Men who had used statins had a higher risk for mortality compared with men who had not used statins (hazard ratio HR 2.8; 95% CI 0.9–8.6; Fig. 2c), and women who had used statins had a lower risk for mortality compared with women who had not used statins (HR 0.2; 95% CI 0.1–0.8; Fig. 2d). Compared with women who had not used statins, the 3‑year cumulative survival rates were also significantly higher in women who had used statins as part of primary cardiovascular prevention as well as secondary cardiovascular prevention (Fig. 3).
Compared with survivals, deceased women had a higher prevalence of cancer, higher prevalence of peripheral vascular disease, lower mean albumin serum levels, and they used statins less frequently (Table 2). A Cox regression analysis showed that statin therapy was associated with low 3‑year cumulative mortality rates in women (HR = 0.3; 95% CI = 0.1–0.6; p = 0.001) independent of cancer, peripheral vascular disease, and albumin serum levels (Table 3).
Discussion
In the current cohort, more than 50% of the older adults aged 80 years or more used statins and most statin users were women. Considering the lack of evidence regarding the usefulness of statin therapy in this age group and in older adult women in terms of mortality reduction [3,4,5,6,7,8,9,10], these rates are significant. Accordingly, the purpose of this study was to evaluate the association between statin therapy and 3‑year mortality/survival rates in men and in women aged 80 years or more, with a special emphasis on well-nourished patients with high albumin serum levels, since some physicians believe that it is reasonable to prescribe statins in very old patients only if they are well-nourished. The present findings show that in the general population of well-nourished older adults aged 80 years or more, statin therapy is associated with high 3‑year survival rates only in women and not in men. Following propensity score matching, statin therapy might even be associated with a higher risk for mortality in men. These gender differences in mortality among older adults aged 80 years or more have been demonstrated for the first time.
Most men in the current cohort used statins as part of secondary cardiovascular prevention, and the lack of a survival benefit in older adult men who used statins as part of secondary cardiovascular prevention is consistent with the findings in one RCT [13] of older adults aged 60 years or more with systolic heart failure, most of them men with cardiovascular diseases. Survival benefits in older adult women using statins as part of secondary cardiovascular prevention are already known, but it has remained uncertain if statin therapy is efficacious also in primary cardiovascular prevention in this population [14]. Statin therapy as part of primary cardiovascular prevention has been associated with reduced all-cause 4‑year mortality rates in older adult women (and men) in only one RCT but these women were younger (aged 70 years or more) than the women in the present study [10]. To the best of our knowledge, a survival benefit from the use of statins in well-nourished older adult women aged 80 years or more, who used statins as part of primary as well as secondary cardiovascular prevention, has never been demonstrated until now. These findings mainly have research implications rather than clinical implications. It is too early to prescribe statins to all well-nourished older adult women aged 80 years or more with high cholesterol serum levels based on the findings of one observational study, but there is still a place to prospectively study the survival benefits of statin therapy in this population.
In the current analysis, women who used statins did not have a higher prevalence of cardiovascular diseases, while men who used statins had a higher prevalence of ischemic heart disease, congestive heart failure, diabetes mellitus, and peripheral vascular disease. In other words, it may be claimed that statin therapy is associated with higher survival rates only in women and not in men because women were healthier than men. In order to address this argument, a subgroup analysis included only women with cardiovascular diseases; however, the 3‑year cumulative survival rates were also higher in women who used statins as part of secondary cardiovascular prevention compared with women who had not used statins. We believe these findings may be explained by the life expectancy of women being higher than the life expectancy of men, even in older adults and even in older adults with cardiovascular diseases [15].
The current analysis does not resemble previous observational studies which have demonstrated a survival benefit of statin therapy in older adults aged 75–80 years or more [3,4,5,6,7]. Strandberg et al. [5] and Allen Maycock et al. [6] have shown that statin therapy is associated with reduced all-cause 6‑year and 3‑year mortality rates in patients aged 75 and 80 years or more but no gender differences in mortality rates have been studied. Jacobs et al. [7] have shown that statin therapy is associated with reduced all-cause mortality rates 5 years following the age of 78 and 5 years following the age of 85 in the general population; but again, no gender differences in mortality rates have been studied. Eaton et al. [3] and Gränsbo et al. [4] studied gender differences in mortality rates among statin users aged 75 and 80 years or more, but all of their patients had cardiovascular diseases and the follow-up was shorter. The current analysis is unique in several aspects: the age of the cohort (80 years or more), the heterogeneity of the cohort (the general population), the nature of the cohort (well-nourished older adults), the outcome studied (gender differences in mortality/survival rates) and the duration of the follow-up (3 years).
The main limitation of the study, apart from its small size and its observational nature, is a selection bias: only patients with at least another admission or an outpatient clinic visit within 3 years following the index admission were included in the analysis in order to confirm compliance to statin therapy; accordingly, healthier patients without hospitalization during the study period were not included in the analysis. Moreover, data concerning the type of statins and the dose during the follow-up years was incomplete. Another limitation is the lack of data concerning high-density lipoprotein (HDL), low-density lipoprotein (LDL), lipoprotein(a), and triglyceride serum levels before and during statin therapy. Additional limitation is that that only a single “hard” outcome, namely all-cause mortality, has been evaluated instead of other outcomes such as cardiovascular mortality, major adverse cardiac events (MACE), and statin-associated adverse events. Another limitation is that patients who started using statins and patients who stopped using statins during their hospitalization were very few, and accordingly, the all-cause mortality rates could not be studied separately. Finally, the use of albumin serum levels as a marker of a nutritional state is probably insufficient [16]; nevertheless, many physicians adhere to it in the clinical practice, and therefore, we have used it in order to reflect real life. In the future, large RCTs in older adults aged 80 years or more should prospectively address these limitations.
Conclusion
In the general population of well-nourished older adults aged 80 years or more, statin therapy is associated with high 3‑year cumulative survival rates only in women who are using statins as part of primary as well as secondary cardiovascular prevention. Future large RCTs should address these findings.
References
Naci H, Brugts JJ, Fleurence R, Tsoi B, Toor H, Ades AE (2013) Comparative benefits of statins in the primary and secondary prevention of major coronary events and all-cause mortality: a network meta-analysis of placebo-controlled and active-comparator trials. Eur J Prev Cardiol 20(4):641–657
Depp CA, Jeste DV (2006) Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry 14:6–20
Eaton CB, Lapane KL, Murphy JB, Hume AL (2002) Effect of statin (HMG-Co-A-Reductase Inhibitor) use on 1‑year mortality and hospitalization rates in older patients with cardiovascular disease living in nursing homes. J Am Geriatr Soc 50:1389–1395
Gränsbo K, Melander O, Wallentin L, Lindbäck J, Stenestrand U, Carlsson J, Nilsson J (2010) Cardiovascular and cancer mortality in very elderly post-myocardial infarction patients receiving statin treatment. J Am Coll Cardiol 55:1362–1369
Strandberg TE, Pitkala KH, Tilvis RS (2008) Statin treatment is associated with clearly reduced mortality risk of cardiovascular patients aged 75 years and older. J Gerontol A Biol Sci Med Sci 63:213–214
Allen Maycock CA, Muhlestein JB, Horne BD, Carlquist JF, Bair TL, Pearson RR, Li Q, Anderson JL, Intermountain Heart Collaborative Study (2002) Statin therapy is associated with reduced mortality across all age groups of individuals with significant coronary disease, including very elderly patients. J Am Coll Cardiol 40:1777–1785
Jacobs JM, Cohen A, Ein-Mor E, Stessman J (2013) Cholesterol, statins, and longevity from age 70 to 90 years. J Am Med Dir Assoc 14:883–888
Rothschild DP, Novak E, Rich MW (2016) Effect of statin therapy on mortality in older adults hospitalized with coronary artery disease: a propensity-adjusted analysis. J Am Geriatr Soc 64:1475–1479
Lloyd SM, Stott DJ, de Craen AJ, Kearney PM, Sattar N, Perry I, Packard CJ, Briggs A, Marchbank L, Comber H, Jukema JW, Westendorp RG, Trompet S, Buckley BM, Ford I (2013) Long-term effects of statin treatment in elderly people: extended follow-up of the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER). PLOS ONE 8:e72642
Glynn RJ, Koenig W, Nordestgaard BG, Shepherd J, Ridker PM (2010) Rosuvastatin for primary prevention in older persons with elevated C‑reactive protein and low to average low-density lipoprotein cholesterol levels: exploratory analysis of a randomized trial. Ann Intern Med 152:488–496
Farahani P (2014) Sex/gender disparities in randomized controlled trials of statins: the impact of awareness efforts. Clin Invest Med 37:E163
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC Jr, Watson K, Wilson PW (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 63(25 Pt B):2889–2934
Kjekshus J, Apetrei E, Barrios V, Böhm M, Cleland JG, Cornel JH, Dunselman P, Fonseca C, Goudev A, Grande P, Gullestad L, Hjalmarson A, Hradec J, Jánosi A, Kamenský G, Komajda M, Korewicki J, Kuusi T, Mach F, Mareev V, McMurray JJ, Ranjith N, Schaufelberger M, Vanhaecke J, van Veldhuisen DJ, Waagstein F, Wedel H, Wikstrand J, CORONA Group (2007) Rosuvastatin in older patients with systolic heart failure. N Engl J Med 357:2248–2261
Allen M, Canadian Academic Detailing Collaboration (2006) Statins in primary prevention: uncertainty in women, elderly. Am Fam Physician 73:973–974
Owen A (2006) Life expectancy of elderly and very elderly patients with chronic heart failure. Am Heart J 151:1322.e1–1322.e4
Kuzuya M, Izawa S, Enoki H, Okada K, Iguchi A (2007) Is serum albumin a good marker for malnutrition in the physically impaired elderly? Clin Nutr 26:84–90
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
D. Justo, M. Tchernichovsky, A. Kremer, E. Joffe, S. Sherman, M. Ioffe and H. Mayan declare that they have no competing interests.
This contribution depicts a historical prospective study which does not interfere with therapy.
Rights and permissions
About this article
Cite this article
Justo, D., Tchernichovsky, M., Kremer, A. et al. Gender differences in mortality among statin users aged 80 years or more. Z Gerontol Geriat 51, 882–888 (2018). https://doi.org/10.1007/s00391-017-1335-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00391-017-1335-y