Abstract
Purpose
Recent guidelines expand indications for statins. However, research on practical economic feasibility and cost-effectiveness in low-risk people is lacking. We aimed to describe the incidence of cardiovascular events (CVE), their total direct costs and the hypothetical effects of wide provision of statins on those rates and expenditures.
Methods
We conducted a population-based cohort study using administrative data among low risk individuals. Estimators of effects of statins were taken from Cholesterol Treatment trialist metaanalysis and from Heart Protection Study trial. Two statin prices were used for analyses: National Italian Health System (€ 0.36) and the International Drug Price Indicator (€ 0.021).
Results
Overall, 920,067 persons at low risk were identified and 14,849 CVE were registered (incidence rate 27.3 per 10,000 person-years). Direct costs for hospitalizations for CVE were 143 M €. Universal provision of statins would result in a significant decrease in CVE rates, from 27.3 to 17.5 per 10,000 person-years (PY) (95 % confidence interval (CI): 15.8–19.4). Universal prescription of simvastatin 20 mg would cost 802 M €. Otherwise, provision of simvastatin at International Drug Price Indicator’s prices would be both clinically effective and cost saving in men older than age 44 (observed expenditures 120 M €, expected 97.4 M €) but not in women (observed expenditures 22.7 M €, expected 36.5 M €).
Conclusions
Among a low-risk population, hypothetical universal provision of low-cost simvastatin to men over 44 years could be both clinically effective and a cost-saving strategy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Much controversy has arisen around appropriate use of statins in the context of primary prevention of cardiovascular events (CVE) with respect to the level of cardiovascular risk and time to initiate treatment. These debates range from positions stating that universal provision of statins after age 50 years—independent of cholesterol measurements—is an important public health strategy aimed at reducing the burden of death and disability from CVE, to those discouraging wide use of these agents based mostly on concerns about the balance between efficacy and safety [1, 2].
Recently, the American College of Cardiology-American Heart Association (ACC-AHA) Task Force released new practice guidelines for the treatment of high blood cholesterol [3]. These also are controversial, because the new recommendations have major impact on clinical, philosophical, and economic aspects of medical practice [4]. While recommendations based on thresholds for assessing risk may be practical and necessary in many circumstances, equally important is that every healthcare system considers their own resources, outcomes and medical/economic options in order to reflect their own priorities and opportunities. As has been noted elsewhere, public policy that only sets thresholds but fails to define process is destined to fail [5].
The burden of cardiovascular diseases constitutes a major health challenge around the world for both developing and developed countries [6]. Fighting this population-wide risk requires coordinated actions on multiple fronts, and societal-level approaches constitute a more strategic action than those based on the individual management of risk [7]. Population lifestyle approaches are generally considered fundamental strategies to reduce cardiovascular risk. Even so, only a small portion of the population adheres to ideal levels of these lifestyle strategies for cardiovascular health [8, 9]. On the other hand, access to safe and effective medicines, particularly statins, constitutes a milestone for the prevention of premature cardiovascular death and disability [10]. Statins have extensively demonstrated their clinical efficacy and safety in prevention settings, and recent evidence largely refutes major criticism about safety [11, 12]. Thus, a strategy based on wide prescription of statins using age as the sole eligibility criterion could theoretically impact the burden of cardiovascular disease. The current challenges to implementing such a strategy are financing this global recommendation and the reasonable philosophical viewpoint on life medicalization. While generic substitution has reduced the price of several strategic medicines, the challenges of generic substitutions still persist, and the availability of generic medicine at low price is not yet sufficiently guaranteed [13, 14]. In fact, research on the practical economic feasibility of extending statin prescriptions are lacking, particularly cost-effectiveness estimates of prescriptions in low-risk people [12]. In any case, these analyses must be part of the conceptual framework of this debate.
Using a large database of an Italian population with a low to very low cardiovascular risk, we described the incidence of major cardiovascular events (CVE), the total direct costs related to these events from the health system perspective, and the hypothetical effects of a wide provision of statins on the incidence rates and health system expenditures.
Materials and methods
We identified all persons living in one Italian region (Puglia) from 2002 to 2010 and qualified as having low to very low cardiovascular risk. For our purposes, we linked all databases that included detailed information on hospitalization, pharmacological treatments, and death/life status of a population of 4,040,990 people. Of these, people aged 40 to 65 years and considered at low to very low cardiovascular risk were selected for the present analysis (see below for cohort definition). According to the Italian law, no ethical approval is required to perform this type of analysis, so no committee was involved in this study.
Data sources
Hospital discharge records included information on primary diagnoses and up to 5 coexisting conditions, procedures, date of admission, discharge, and in-hospital death. All diagnoses were coded according to the International Classification of Disease, Ninth Revision [15].
The prescription database provided the community prescriptions reimbursed by the National Health System with drugs coded according to the Anatomical Therapeutic Chemical (ATC) Classification and qualified with respect to dosages, date of first prescription, and duration of exposure [16].
This strategy to produce epidemiological information has been validated [17, 18].
Cohort definition
The study cohort was people aged 40 to 65 years who had not been hospitalized for cardiovascular reasons within the 2 years prior to index date of January 1, 2004. Cardiovascular hospitalizations were defined as stroke, peripheral vascular disease (PVD), embolic episode, myocardial infarction (MI), chronic angina, unstable angina, heart failure (HF), or atrial fibrillation (AF). Additionally, the 24-month period preceding the index date was analyzed for chronic exposures to certain pharmacological treatments in order to exclude individuals with certain cardiovascular and non-cardiovascular conditions associated with increased risk: hypertension (beta blockers, calcium channel blockers, angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, or diuretics), congestive HF (the aforementioned plus digitalis, amiodarone, anticoagulation), coronary artery disease (nitrates or antiplatelet agents), or diabetes (insulin, sulfonylureas, biguanides, thiazolidinediones) as reported elsewhere [18]. Individuals with other non-cardiovascular conditions including malignancy, depression, and chronic obstructive pulmonary disease were also excluded using both hospitalization and prescription criteria.
Using these restrictions, a population aged 40 to 65 without previous history of cardiovascular hospitalizations and with no previous exposure to any cardiovascular treatment or antidiabetic agents was identified.
Outcomes definitions
All persons were followed up to 6 calendar years or until the occurrence of a major CVE. These events were defined as follows: Major CVE—time to the first occurrence of a hospitalization for MI, stable or unstable angina, or stroke. These events were identified based on the validated discharge diagnosis used in first position in the hospital record card. Cardiovascular death—all deaths that occurred within 180 days following a hospitalization for MI, stable or unstable angina, revascularization procedures, HF, or stroke. All deaths that occurred outside that timeframe were not considered cardiovascular death, and patients were censored at that time.
Statistical analysis
For all analyses, the study population was divided into four age categories (<45, 45 to ≤50, 50 to ≤55, and >55 years). For each category, outcome incidence rates were computed per 10,000 person-years (PY) of follow-up for both the overall cohort and the sex and age categories. Differences between genders were compared as rate differences, with their corresponding 95 % confidence intervals (95 % CI).
Observed expenditures (in €) were computed as the sum of hospital expenditures due to major CVE in the whole population and across each age-sex category.
To estimate the potential effects of statin therapy, we computed the expected risk reduction according to the expected reduction in LDL-cholesterol level. This was done by computing the expected risk ratios (RR) as the product of (log)RRs by the LDL-cholesterol (in mmol/L) reduction with simvastatin 20 mg/day, under the assumption that a log-linear relationship exists between LDL-cholesterol and risk without a lower boundary [19]. Observed incidence rates and expenditures were then multiplied by the expected RRs to obtain incidence rates and expenditures potentially to be observed under universal statin therapy. Computations of expected effects on outcomes and expenditures were conducted with the weighted estimator of LDL-cholesterol reduction as reported by Law et al., that is, for simvastatin 20 mg, the expected reduction in LDL-cholesterol is 1.54 mmol/l (95 % CI 1.46 to 1.63) [19]. Estimators of RRs were taken from reported effects by the Cholesterol Treatment Trialists for every mmol/L of reduction on major CVE in primary prevention, except for PVD whose estimator of expected effect was computed using RR for non-coronary revascularization as reported in Heart Protection Study trial [11, 20]. These RRs were as follows: 0.79 (95 % CI 0.77 to 0.81) for CVE, 0.76 (95 % CI 0.73 to 0.79) for MI, 0.85 (95 % CI 0.80 to 0.89) for stroke, 0.84 (95 % CI 0.74 to 0.95), 0.88 (95 % CI 0.84 to 0.91) for CV death, and 0.96 (95 % CI 0.92 to 1.01) for non-CV death.
Expected expenditures were computed as the product of observed expenditures among individuals experiencing an event by the expected RRs plus the cost of statin therapy (as daily cost of therapy until the event or last follow-up date whichever came first). Expected expenditures were estimated using two different simvastatin prices. The simvastatin 20-mg prices used in our calculations were the National Italian Health System price (€ 0.35786, daily) for the drug and the median buyer’s price taken from the International Drug Price Indicator (€ 0.021388, daily) [21].
Analyses on expenditures due to therapy assumed that all individuals would take the drug for the entire follow-up period. To further explore the relationship between observed and expected expenditures, we repeated the analyses using age deciles instead the four-age categories. We conducted sensitivity analyses to explore the effects of hypothetical changes in hospital and statin’s costs on the health system expenditures.
All analyses were conducted with SPSS 12.0 for Windows (SPSS Inc, Chicago, Ill, USA) and with R statistical package (R Foundation for Statistical Computing, Vienna, Austria).
Results
Low-risk population and outcomes
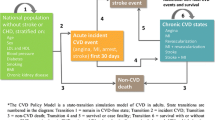
A total of 920,067 people considered at low cardiovascular risk were identified. The median age was 50.4 years (interquartile range, 44.8–56.7). Of these, 455,062 (49.4 %) were males and 465,005 (50.6 %) females (Fig. 1).
Overall, 14,849 CVE (1.6 %) occurred during a mean follow-up of 5.14 years, leading to an incidence rate 27.3 events/10,000 PY and an annual risk of 0.26 %. Events increased with age (from 0.7 % [incidence rate 12.4 events/10,000 PY, and an annual risk of 0.12 %] in those aged 40 to 45 years to 2.7 % [45.4 events/10,000 PY, with an annual risk of 0.45 %] in those aged >55 years) and were mostly concentrated in males (overall incidence rate difference (95 % CI) between males and females: 35.35 (34.45 − 36.24) for every 10,000 PY). Among this population, the highest risk category was males aged 55 to 65, who had a 4.3 % risk at 6 years (72.11 events/10,000 PY); in contrast, the lowest risk category was women aged 40 to 45 where the 10-year risk was less than 1 % (4.68 events/10,000 PY) (Table 1).
The most common CVEs were MI followed by stroke and PVD (Table 1).
Cardiovascular deaths were rare; overall, 488 deaths occurred during follow-up (0.1 % events annually or an incidence rate of 0.91 events/10.000 PY) (Table 1).
Cost of CVE
Direct costs for all CVE hospitalizations were nearly 143 M €. The majority of these costs, nearly 120 M €, were for the treatment of CVEs in males and the remaining nearly 23 M € was for females. Most of these expenditures were related to hospitalizations for MI (110 M €) followed by stroke (nearly 24 M €) and PVD (13 M €) (Table 2).
Analyses of potential effects of statins on CVE and mortality
We estimated that universal provision of simvastatin 20 mg/daily would have reduced LDL-cholesterol by 1.54 (1.46 − 1.63) mmol/L and that such effect would have resulted in a reduction of CVE leading to a HR of 0.64 (95 % CI 0.58 − 0.71), MI 0.59 (95 % CI 0.52 − 0.67), stroke 0.78 (95 % CI 0.71 − 0.84), PVD 0.77 (95 % CI 0.63 − 0.92), cardiovascular death 0.78 (95 % CI 0.67 − 0.92) and all cause death 0.87 (95 % CI 0.78 − 0.95).
These reductions would result in a significant difference in the observed rate of CVE from 27.28 events/10,000 PY to a predicted rate of 17.46 events (95 % CI 15.82 − 19.37), meaning an incidence rate reduction of 9.82 events/10,000 PY, mostly by reducing the occurrence of non-fatal MI among men (Table 3).
Observed and expected expenditures with a hypothetical universal provision of simvastatin 20 mg/day
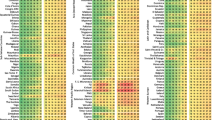
The Italian National Health System purchases simvastatin 20 mg at 10.02 € for 28 pills (daily price 0.35786 €), resulting in a 6-year cost for an individual of 783.71 €. Providing universal prescriptions of simvastatin 20 mg daily would result in total health expenditures of 802,356,962 €, far more expensive than the current expenditure of 142,895,869 € (Table 2). This overall unfavorable balance is present for both men (observed expenditures 120,157,950 € against estimated expenditures of 420,671,297 €) and women (observed expenditures 22,737,919 € against estimated expenditures of 381,685,665 €). No age group (either male or female) gains an equitable balance between observed and predicted costs with the universal provision of statins at current prices (Table 2 and Fig. 2a, b).
However, if simvastatin was available at the prices of the International Drug Price Indicator (the buyer median price of simvastatin 20 mg is 0.0213880 € per tablet or capsule), universal provision would be both clinically effective and economically attractive in men (observed expenditures 120,157,950 € against estimated expenditures of 97,447,164.4 €, with positive balance for men older than 45 years) but not in women (observed expenditures 22,737,919 € against estimated expenditures of 36,494,689.8 €) (Figs. 1d and 2c and Table 4).
Potential severe adverse effects
During follow-up, there were 10 hospitalizations with discharge diagnosis of rhabdomyolysis (0.21 cases/100.00 PY; 95 % CI 0.11 − 0.39), lower than reported with simvastatin 20–39 mg/day, and no case fatalities [22]. These events had a median cost of € 9347 (interquartile range € 5265 to € 14763).
Sensitivity analyses
Our overall findings were stable under hypothetical settings with different hospital and statin costs, including some unfavorable for statin strategy as the combined reduction in direct hospital costs and an increase in statin costs (Supplemental Table).
Discussion
This study found that in a large population considered to be at low to very low cardiovascular risk, the actual number of CVE and direct costs related to these were considerable. We also found that hypothetical universal provision of low-dose simvastatin would result in a reduction of CVE, yet direct costs could be reduced only among men >44 years of age only when simvastatin could be provided at the price suggested by International Drug Price Indicator. In other words, low-dose simvastatin results in cost savings only when generic prices become available.
This analysis identified a population with a low to very low risk of CVE who did not reach the threshold for recommendation of pharmacological prescription for primary prevention. The incidence rates of premature events in this otherwise “low risk” population indicates consideration of opportunities to implement safe and effective interventions to improve global health are warranted, although the most appropriate strategy to do so is not clear. Obviously, the first and only recommendation should be counseling the adoption of a healthy lifestyle [23]. A better lifestyle, including not smoking, 30 min or more of daily exercise, having a body mass index of 25 kg/m2 or less, following an ideal diet with no or modest alcohol consumption are all prudent recommendations. Still, few people effectively achieve these habits, and responsibility must not reside entirely with the single citizen [5, 8, 24, 25].
This burden of disease had another important consequence. The total hospital expenditures for the treatment of CVE totaled nearly 140 M € in a 6-year period in only one Italian region. This amount should be interpreted as a conservative estimate of total costs because it does not consider ambulatory treatments (drugs and visits), nor social and economic consequences from loss of productivity following events (indirect costs). Yet, the present analysis found that the (measured) economic benefits of providing statins (to men over 44 years but not to women) outweigh the (measured) economic costs, several limitations of these results should also be taken into account. As the analysis did not account for indirect costs that occur outside the hospital, the cost-offset may be underestimated. Additionally, since no clinical trial provide empirical evidence that treating persons at low risk effectively reduces all-cause mortality and morbidity, we cannot conclude that—if applied—this strategy would have a significant net effect on the desired outcomes. Furthermore, it would not be appropriate to conclude that the least expensive alternative (in this case simvastatin 20 mg at the International Drug Price Indicator’s prices) is the best alternative. Also, the duration of follow-up that could be considered short, notwithstanding that a clear cost saving effect was evident with International Drug Price Indicator’s simvastatin price. Finally, we have no data on non-severe adverse events, which could be relevant when considering a pharmacological prevention strategy at population level.
Recent NICE guidelines stress the absence of evidence of benefit of treatment for most population, the cost-effectiveness advantages of non-pharmacologic approaches for risk management, and the uncertainty of benefit/harm balance due to the possibility of higher than reported adverse effects incidence [26]. Considering the aforementioned uncertainties, our analyses should not be interpreted as evidence for recommendation of mass medication with statins, but only as a contribution to other existing data on this issue.
Although universal provision of low-dose statins to persons above 50 years has been proposed as an alternative or complement to (a failed) primary prevention [1], this strategy faces several challenges. The main being that universal provision without risk discrimination has not been demonstrated to be associated with any reduction of CVE. However, the lack of clinical trials does not necessarily mean that there are no data to support a benefit. It is hard to conceive that reducing LDL-cholesterol in a “healthy” population would not translate into a clinical benefit of a similar proportion of what has been observed in the context of secondary prevention. In fact, favorable risk factor levels in middle age are associated with a lower lifetime risk for cardiovascular mortality, increased survival, and improved quality of life [27]. Our analysis indicates a high total number of events in a low-risk population, and also that nearly 10 events would be avoided for each 10,000 PY (15 in men and 4 in women) with statin treatment. Assuming this effect, the second challenge with the universal provision strategy is related to cost. The present analysis confirms that universal provision of statins would be extremely expensive and certainly much more expensive than current spending as far as direct costs of treating the CVE that occur. However, the analysis also suggest that if the Italian government would decide to buy (or to produce) statins not at a market price but at the one suggested in the International Drug Price Indicator Guide, universal provision of generic statins would not only reduce CVE but also be a cost-saving strategy for all men above 44 years of age [21]. The analyses failed to demonstrate economic benefit in women up to 60 years, driven by the low number of CVE. Sensitivity analyses, showing stability of the cost-saving with statins even under the unfavorable relation of lower direct hospital costs and higher statin prices, extend our findings to other health settings with different costs. These analyses also suggest that in settings were mean direct hospital costs for CVE are higher, as is the case of US, savings associated with this strategy could potentially be higher [28].
The potential implications of these findings are medical and political. From a government policy perspective, support for prevention policies and the necessary appropriations that support prevention can be difficult to garner when resources are limited. Political decisions are usually made for clear and immediate gains, while long-term savings or savings that cannot be accurately measured are less persuasive [29]. For this reason, the mathematical models that have been published on this topic have not been terribly convincing to politicians [30, 31]. Our analysis does not make mathematical assumptions of cost but reports real ones, confirming and extending previous findings [30, 31].
In conclusion, our results suggest that universal provision of low dose simvastatin at generic prices would result in a reduction of CVE and their related direct costs men >44 years of age.
References
Ebrahim S, Casas JP (2012) Statins for all by the age of 50 years? Lancet 380:545–547
Ray KK, Seshasai SR, Erqou S, Jukema JW, Ford I, Sattar N (2010) Statins and all-cause mortality in high-risk primary prevention: a meta-analysis of 11 randomized controlled trials involving 65,229 participants. Arch Intern Med 170:1024–1031
Stone NJ, Robinson J, Lichtenstein AH, Bairey Merz CN, Lloyd-Jones DM, Blum CB, McBride P, Eckel RH, Schwartz JS, Goldberg AC, Shero ST, Gordon D, Smith SC Jr, Levy D, Watson K, Wilson PW (2013) 2013 ACC/AHA Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. doi:10.1016/j.jacc.2013.11.002
Ridker PM, Cook NR (2013) Statins: new American guidelines for prevention of cardiovascular disease. Lancet 382:1762–1765
Yancy CW (2011) Is ideal cardiovascular health attainable? Circulation 123:835–837
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O'Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380:2095–2128
Beaglehole R (2001) Global cardiovascular disease prevention: time to get serious. Lancet 358:661–663
Shay CM, Ning H, Daniels SR, Rooks CR, Gidding SS, Lloyd-Jones DM (2013) Status of cardiovascular health in US adolescents: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2005-2010. Circulation 127:1369–1376
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB, American Heart Association Statistics Committee and Stroke Statistics Subcommittee (2013) Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127:e6–e245
World Health Organization. WHO Model List of Essential Medicines. http://www.who.int/medicines/publications/essentialmedicines/en/index.html. Accessed 22 november 2013
Cholesterol Treatment Trialists’ (CTT) Collaborators, Mihaylova B, Emberson J, Blackwell L, Keech A, Simes J, Barnes EH, Voysey M, Gray A, Collins R, Baigent C (2012) The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: meta-analysis of individual data from 27 randomised trials. Lancet 380:581–590. doi:10.1016/S0140-6736(12)60367-5
Taylor FC, Huffman M, Ebrahim S (2013) Statin therapy for primary prevention of cardiovascular disease. JAMA 310:2451–2452
Haas JS, Phillips KA, Gerstenberger EP, Seger AC (2005) Potential savings from substituting generic drugs for brand-name drugs: medical expenditure panel survey, 1997-2000. Ann Intern Med 142:891–897
Cameron A, Ewen M, Ross-Degnan D, Ball D, Laing R (2009) Medicine prices, availability, and affordability in 36 developing and middle-income countries: a secondary analysis. Lancet 373:240–249
International Classification of diseases, 9th Revision Clinical Modification, 6th edition (2004) US Department of Health and Human Services, National Center for Health Statistics, Health Care Financing Administration. Washington: Public Health Service
WHO Collaborating Centre for Drug Statistics Methodology (2003) Guidelines for ATC classification and DDD assignment 2003. Oslo, Norway
Macchia A, Romero M, Comignani PD, Mariani J, D'Ettorre A, Prini N, Santopinto M, Tognoni G (2012) Previous prescription of β-blockers is associated with reduced mortality among patients hospitalized in intensive care units for sepsis. Crit Care Med 40:2768–2772
Macchia A, Romero M, D'Ettorre A, Mariani J, Tognoni G (2012) Temporal trends of the gaps in post-myocardial infarction secondary prevention strategies of co-morbid and elderly populations vs. younger counterparts: an analysis of three successive cohorts between 2003 and 2008. Eur Heart J 33:515–522
Law MR, Wald NJ, Rudnicka AR (2003) Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis. BMJ 326:1423
Heart Protection Study Collaborative Group (2002) MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360:7–22
Management Sciences for Health for World Health Organization (2012) International Drug Price Indicator Guide. Cambridge, MA, USA. Available at http://erc.msh.org/dmpguide/pdf/DrugPriceGuide_2012_en.pdf. Accessed 7 September 2014
Floyd JS, Heckbert SR, Weiss NS, Carrell DS, Psaty BM (2012) Use of administrative data to estimate the incidence of statin-related rhabdomyolysis. JAMA 307:1580–1582
Weintraub WS, Daniels SR, Burke LE, Franklin BA, Goff DC Jr, Hayman LL, Lloyd-Jones D, Pandey DK, Sanchez EJ, Schram AP, Whitsel LP, American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular Disease in the Young, Council on the Kidney in Cardiovascular Disease, Council on Epidemiology and Prevention, Council on Cardiovascular Nursing, Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Clinical Cardiology, and Stroke Council (2011) Value of primordial and primary prevention for cardiovascular disease: a policy statement from the American Heart Association. Circulation 124:967–990
Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE (2011) Low prevalence of “ideal cardiovascular health” in a community-based population: the Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study. Circulation 123:850–857
Fang J, Yang Q, Hong Y, Loustalot F (2012) Status of cardiovascular health among adult Americans in the 50 states and the district of Columbia, 2009. J Am Heart Assoc 1:e005371
Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. Available at https://www.nice.org.uk/guidance/cg181/resources/guidance-lipid-modification-cardiovascular-risk-assessment-and-the-modification-of-blood-lipids-for-the-primary-and-secondary-prevention-of-cardiovascular-disease-pdf (accessed December 1st 2014)
Lloyd-Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D (2006) Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation 113:791–798
O'Sullivan AK, Rubin J, Nyambose J, Kuznik A, Cohen DJ, Thompson D (2011) Cost estimation of cardiovascular disease events in the US. Pharmacoeconomics 29:693–704
Brownson RC, Royer C, Ewing R, McBride TD (2006) Researchers and policymakers: travelers in parallel universes. Am J Prev Med 30:164–172
Pletcher MJ, Lazar L, Bibbins-Domingo K, Moran A, Rodondi N, Coxson P, Lightwood J, Williams L, Goldman L (2009) Comparing impact and cost-effectiveness of primary prevention strategies for lipid-lowering. Ann Intern Med 150:243–254
Kang HY, Ko SK, Liew D (2009) Results of a Markov model analysis to assess the cost-effectiveness of statin therapy for the primary prevention of cardiovascular disease in Korea: the Korean Individual-Microsimulation Model for Cardiovascular Health Interventions. Clin Ther 31:2919–2930
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 26 kb)
Rights and permissions
About this article
Cite this article
Macchia, A., Mariani, J., Romero, M. et al. On the hypothetical universal use of statins in primary prevention: an observational analysis on low-risk patients and economic consequences of a potential wide prescription rate. Eur J Clin Pharmacol 71, 449–459 (2015). https://doi.org/10.1007/s00228-015-1808-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1808-0