Abstract
This study aimed to investigate the effects of recombinant human bone morphogenetic protein (rhBMP-7) on human cancellous bone grafts (BGs) while differentiating between anabolic and catabolic events. Human BGs alone or supplemented with rhBMP-7 were harvested 14 weeks after subcutaneous implantation into NOD/Scid mice, and studied via micro-CT, histomorphometry, immunohistochemistry and flow cytometry. Immunohistochemical staining for human-specific proteins made it possible to differentiate between grafted human bone and newly formed murine bone. Only BGs implanted with rhBMP-7 formed an ossicle containing a functional hematopoietic compartment. The total ossicle volume in the BMP+ group was higher than in the BMP− group (835 mm3 vs. 365 mm3, respectively, p < 0.001). The BMP+ group showed larger BM spaces (0.47 mm vs. 0.28 mm, p = 0.002) and lower bone volume-to-total volume ratio (31% vs. 47%, p = 0.002). Immunohistochemical staining for human-specific proteins confirmed a higher ratio of newly formed bone area (murine) to total area (0.12 vs. 0.001, p < 0.001) in the BMP+ group, while the ratio of grafted bone (human) area to total area was smaller (0.14 vs. 0.34, p = 0.004). The results demonstrate that rhBMP-7 induces BG resorption at a higher rate than new bone formation while creating a haematopoietic niche. Clinicians therefore need to consider the net catabolic effect when rhBMP-7 is used with BGs. Overall, this model indicates its promising application to further decipher BMPs action on BGs and its potential in complex bone tissue regeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ever since 1965, when Urist described the biological foundation for bone morphogenesis, the regenerative capacity of human bone has been a field of extensive research [1]. His work ultimately led to the isolation of bone morphogenetic proteins (BMPs) from mammalian demineralised bone [2] and the later characterisation of recombinant human BMP (rhBMP) [3].
BMPs are a subclass of growth factors in the transforming growth factor beta superfamily exhibiting major osteoinductive properties while facilitating intramembranous and endochondral bone formation [3, 4]. The pleiotropism of BMPs and their crucial role in cell differentiation, bone development and fracture healing has been well characterised [5, 6].
Despite ongoing debate about their side effects [7, 8], rhBMPs are still widely used in procedures like non-union surgeries, spinal fusion and fracture healing with a rising interest in fields such as implant device stabilisation, critical size-defect reconstruction, treatment of femoral head necrosis or bone impaction grafting [9,10,11].
For the treatment of large bone defects, allogenic bone grafting is widely used [12, 13] as autologous grafting can be associated with limited availability and significant donor site morbidity [14]. However, the use of allogenic bone has inherent disadvantages and side effects such as the potential transmission of infectious diseases [15, 16] and relatively high costs [17]. Moreover, allogenic bone grafts (BGs) only act as an osteoconductive scaffold with more or less absent osteoinductive properties [18]. To transfer osteoinductive properties to an osteoconductive scaffold, BGs can be combined with rhBMPs in order to improve graft remodelling and eventually clinical outcome [19, 20].
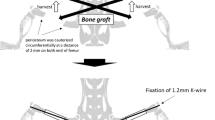
However, it is well known that BMPs not only induce new bone formation but at the same time stimulate osteoclastogenesis [21, 22], indicating its role in both anabolic and catabolic pathways (Fig. 1). Within this context, Magnus Tagil and co-workers have long shown that adding rhBMP to BGs accelerates their resorption rate, suggesting the application of anti-resorptive drugs to contain this effect [23]. These syngeneic transplantation studies provided the surgical community with insights into how rhBMPs affect BG remodelling and how this process could be further manipulated by anti-resorptive drugs. Yet, these models did not allow to clearly determine the individual rates of new bone formation and BG resorption under the influence of rhBMP, as syngeneic transplantation studies impede clear differentiation and hence quantification of newly formed bone versus grafted bone.
Schematic of anabolic and catabolic events induced by rhBMP-7: osteoblast differentiation results in new bone formation from monomers such as amino acids, calcium and phosphates. At the same time the haematopoietic cell expansion induces recruitment of osteoclasts, eventually triggering the reverse process
The present study was designed to uncover the effects of rhBMP-7 on BGs remodelling, osteoclastogenesis and haematopoiesis in vivo. To decipher and quantify the remodelling process, we employed a mouse xenograft model, providing the unique ability to differentiate between the fate of the transplanted human bone graft and the rate of new murine bone formation. The subcutaneous transplantation site was chosen to prevent any effects of biomechanical loading on the BG remodelling process and therefore to analyse the impact of rhBMP-7 on BGs alone.
Material and Methods
Cancellous bone chips were harvested during elective hip arthroplasty from an otherwise healthy male patient (76 years) without comorbidities or documented medication. During the reaming process of the acetabulum, only chips gained from the last of ascending reamer sizes were used in order to ensure a homogenous dispersal of the graft fragments without any cartilage remnants.
The harvested cancellous fragments were washed several times with phosphate buffer saline (PBS, Life Technologies, Australia) to remove any human bone marrow components and then packed into a cylindrical plastic mould with a volume of 0.5 cm3 while adding 60 µL Fibrin Glue (TISSEEL Fibrin Sealant, Baxter Healthcare International, USA) with or without 20 µL rhBMP-7 (1 µg/µL, Olympus Biotech Corporation, USA).
12 male non-obese diabetic-severe combined immunodeficient mice (NOD/scid; strain name: NOD.CB17-Prkdc scid/J) were ordered from the Animal Resource Centre (Canning Vale, Western Australia) and housed in a temperature-controlled and pathogen-free environment according to The University of Queensland animal-housing standards.
Bone grafts were subcutaneously implanted into both flanks of the mice (each mouse received 2 transplants), whereas one group (n = 6 mice × 2 implantation sites) received BGs with Fibrin Glue only (BMP−) while in the other group (n = 6 × 2) the BGs were supplemented with Fibrin Glue and rhBMP-7 (BMP+; Fig. 2). To ensure postsurgical animal welfare, subcutaneous injections of Temgesic® (0.1 mg/kg body weight; Buprenorphine 0.3 mg/mL) were conducted.
14 weeks post-implantation, mice were sacrificed via CO2 asphyxiation. Transplants were harvested and analysed via visual inspection, micro-computed tomography (µCT), histology, histomorphometry and flow cytometry (Fig. 2). Samples were fixed in 4% paraformaldehyde (PFA) for 24 h hours before transfer into 70% methyl carbinol.
µCT Analysis
After fixation, specimens were scanned via high-resolution µCT (μCT 40, Scanco Medical AG, Switzerland) and evaluated according to guidelines described by Bouxsein et al. [24] (six transplants per group).
Flow Cytometry
Flow cytometry analysis was performed as previously reported using BD LSRFortessa X-20 cytometer (BD Biosciences, USA) [25, 26]. In brief, bone transplants were harvested and gently crushed with a pestle and mortar in PBS (4 °C) containing 2% fetal calf serum (FCS, Life Technologies, Australia). To collect the femoral bone marrow, mice femora were flushed with PBS with subsequent centrifuging at 400×g for 5 min at 4 °C. A cell strainer (40 µm, FALCON, USA) was used to make a single-cell suspension. Single-cell suspensions were stained with mouse CD11b-PECY7, B220-APCCY7, CD3ɛ-FITC, F4/80Alexa647, CD45-Pacific Blue, Ly6G-PE (BioLegend, Australia) to determine the mouse hematopoietic lineage. Dead cells were excluded by staining for 7-amino actinomycin D (Life Technologies, Australia). Data were analysed using FlowJo software (Tree Star Inc., San Carlos, CA).
Histological Analysis and Immunohistochemistry
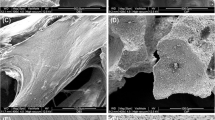
Standardised protocols optimised for paraffin sections were followed. In order to differentiate between human bone (BG) and mouse bone (newly formed bone, NB), IHC was performed for human-specific Collagen 1 (hsCol-1) (Abcam, Australia).
Histomorphometry/Osteomeasure
Osteomeasure (Osteometrics, Atlanta, GA, USA) was used on three representative tissue sections, each 20 sections apart from each other (in six transplants of every group), to quantify total bone tissue area, area of intertrabecular spaces and the number of osteoclasts per total area. Hs-Col1 staining made it possible to quantify the area of grafted bone (human) and the area of newly formed bone (murine), respectively. Tartrate-resistant acid phosphatase (TRAP) staining revealed the number of osteoclasts per area. Four independent sections of each biological replicate were analysed.
Statistical Analysis
SigmaPlot 13.0 (Systat Software Inc., CA, USA) was used for statistical analyses and graph design. Data were tested for normal distribution using the Shapiro–Wilk test and then further analysed with the student’s t test or Mann–Whitney U test to determine differences between groups. The level of significance was set at p ≤ 0.05.
Source of Funding
Baxter Healthcare Australia kindly provided Fibrin Glue (TISSEEL Fibrin Sealant). The following funding existed during conduction of this study: National Health and Medical Research Council of Australia (Project Grant 1082313 to BMH and DWH), German Research Foundation (DFG HO 5068/1-1 to BMH) and Australian Research Council (IC160100026).
Results
rhBMP-7 Induces BG Remodelling and the Development of a Morphologically Intact Organ Bone
Gross macroscopic examination revealed neoangiogenesis in both groups with and without rhBMP-7 (Fig. 3, macroscopic). The BMP+ group appeared with a purple-like outer structure indicating a highly vascularised bone organ, while the BMP− group showed a sallow-rubble like outer appearance. Surface morphology of the BMP+ group appeared smooth in 3D-reconstructed µCT images, while looking rough in the BMP− group (Fig. 3, µCT). BG implanted together with rhBMP-7 resulted in a remodelled bone resembling a physiological organ bone that featured a bone marrow (BM) compartment, while omitting rhBMP-7 resulted in loose fibrous tissue (FT) expanding between the trabeculae (Fig. 3, H&E). Histological examination of the samples further revealed a cortex-like outer structure (Fig. 3, H&E) as well as an inner trabecular network for the group receiving rhBMP-7. Without the influence of rhBMP-7, however, trabeculae appeared unorganised and larger with smaller intertrabecular spaces occupied by loose connective tissue (Fig. 3, H&E). On higher magnifications H&E staining revealed empty lacunae, while the addition of rhBMP-7 showed empty lacunae of the BG coexisting with osteoblasts residing in lacunae of the newly formed bone (Fig. 3, H&E).
rhBMP-7 induces new bone formation as well as the creation of a haematopoietic niche. Results of BMP+ versus BMP− groups; macroscopic (1st column), µCT(2nd column); Hematoxylin & Eosin staining (low and high power views) showing intertrabecular spaces filled with fibrous tissue (FT) or bone marrow (BM)—black arrow heads demonstrate the presence of a cortical shell (3rd column); bone transplanted without rhBMP-7 exhibited empty lacunae (red arrow heads), whereas rhBMP-7 resulted in the formation of vital new bone with osteoblasts residing within lacunae (green arrow heads) (column 4 & 5)
rhBMP-7 Exerts Osteo-Catabolic Effects on BGs That Outweigh Its Osteo-Anabolic Capacity
Volumetric and histomorphometric analyses showed that the total volume of the ossicles was significantly higher in the BMP+ group compared to the BMP− group (835.5 mm3 ± 88.3 vs. 365 mm3 ± 101.6, respectively, p ≤ .001). Moreover, the level of bone volume (258.7 mm3 ± 39.4 vs. 162.4 mm3 ± 35.7, p = .001) and the BM spaces (0.47 mm ± 0.09 vs. 0.28 mm ± 0.06, p ≤ .002) in the BMP+ group was significantly higher than in the BMP− group (Table 1). While the total ossicle volume was 2.3 times higher in the BMP+ group, the bone volume only increased by 1.6 compared to the BMP− control.
Immunostaining using hsCOL-1 confirmed the presence of human-grafted bone and revealed the presence of newly formed murine bone in the BMP+ group, while in the absence of rhBMP-7 almost no new bone formation was observed (Fig. 4). Histomorphometric analysis revealed that the ratio of BG to total bone organ area (TA) was significantly lower in the BMP+ group compared to the BMP− control (n = 6 biological replicates; p ≤ 0.001). After 14 weeks in vivo, only 14% of the TA was occupied by the implanted human BGs in the BMP+ group while omitting rhBMP-7 resulted in 34% BG/TA. NB apposition was also higher in the BMP+ group compared to the BMP− group (p = 0.002). 12% of the TA was occupied by new bone in the group receiving BMP+ while the BMP− group barely showed any new bone formation (0.1%). Causing a 12% higher new bone formation rate and 20% higher BG resorption rate, the application of rhBMP-7 exerted a significant osteo-catabolic effect on the BG, that overall outweighed its anabolic effects.
The newly formed BM as seen in the BMP+ group only, created a local niche for osteoclasts, as depicted by TRAP staining (Fig. 5). In accordance with the volumetric evidence for bone graft resorption, quantification of osteoclasts (N.Oc/mm2) demonstrated significantly higher numbers in the group receiving rhBMP-7 (p = 0.002), indicating the involvement of osteoclasts in the remodelling process of the ossicles (Fig. 5). Without the presence of a local BM niche (BMP− group), no relevant osteoclast activity was seen (Fig. 5).
rhBMP-7 Induces the Development of a Physiological Bone Marrow Compartment via Haematopoiesis
In contrast to the BMP− group, flow cytometry of the BMP+ ossicles showed similar patterns (Ly6G, CD11b, B220 and Sca-1) compared to the control NOD/Scid mouse femur (Fig. 6), resembling features of a remodelled bone marrow niche. Though, the ratio of bone volume to total volume was significantly higher (47% vs. 31%, p = 0.002) without the influence of rhBMP-7, the concomitant lack of a physiological remodelling process caused no BM niche formation.
Immunohistochemical staining for murine B-Cells (B220) and T-Cells (CD3) demonstrated a similar pattern when comparing the BMP+ group to the mouse femur (Fig. 7). Ly6G and F4/80 staining uncovered cells of the myeloid linage with again high histomorphological similarity to the mouse femur, suggesting the formation of a haematopoietic niche. Also, TRAP staining revealed the presence of osteoclasts in the BMP+ group, mirroring what was found in the mouse femur control. Without the influence of rhBMP-7 a local infiltrate of macrophages appeared within the ossicles (Fig. 7—F4/80 staining). Yet, IHC staining did not reveal an active remodelling process mediated via osteoclastic activity (Fig. 7—TRAP staining). Altogether, only the BMP+ group established an ectopic hematopoietic niche within the ossicles, similar to what can be found in the mouse femur.
Discussion
To date, various in vivo models have employed rhBMPs to investigate bone regeneration and disease [27,28,29], including its effects on bone marrow expansion of tissue-engineered bone implants [25, 30,31,32,33,34,35,36,37,38,39,40]. Using a well-established ectopic humanised xenograft mouse model this study untangles the remodelling process induced by rhBMP-7 and demonstrates its anabolic and catabolic effects on the transplanted tissue (BG). Ultimately, we demonstrate the unique feature of this model unmasking the faith of the implanted BG and show individual rates of BG resorption and new bone apposition, with and without the influence of rhBMP-7.
Due to BMPs osteoinductive properties, its application in combination with BG to treat bone defects became increasingly popular. Pioneers in the field have investigated the remodelling response of transplanted BG’s after supplementation with rhBMPs, with and without the coadministration of common bone resorption inhibitors such as zoledronate [41] and denosumab [42]. Until now the isolated effect of BMPs on the BG and on new bone formation has not been separately demonstrated due to the syngeneic nature of current models. However, a detailed understanding of BMP’s effects on bone metabolism is of crucial clinical relevance as shown in a study of patients who underwent acetabular and femoral revision surgery [43]. Karrholm et al. compared patients receiving either allograft only or a combination of allograft and osteogenic protein-1 (OP-1, BMP-7) [43]. After 2-year follow-up, an increase in posterior stem tilt in the patients receiving rhBMP-7 was observed with subsequent need for surgical revision [43]. This could have been the result of local bone resorption due to rhBMP-7 application. In contrast, another study has shown an increased bone formation rate and bone density when combining BGs with rhBMP-7 and zoledronate [41]. Though bisphosphonates such as zoledronate seem to counteract the catabolic process triggered by BMPs [41], it cannot be concluded whether drugs like zoledronate only affect the newly formed bone or also the grafted tissue itself. Experimentally, a clear differentiation between newly formed bone and the fate of the grafted bone has not been shown yet and therefore the detailed effects of rhBMP-7 on BG remodelling remain largely speculative.
Consequently, we chose to perform our experiments in a xenograft model allowing us to individually analyse the rate of bone graft resorption and new bone apposition mediated by rhBMP-7. Our results showed that the rate of BG resorption was significantly higher when the bone graft was supplemented with rhBMP-7. Also, demonstrating individual rates for BG resorption and new bone formation revealed the net osteo-catabolic effect of rhBMP-7. In accordance with that, the increase in total volume in the BMP+ group was higher than the increase in actual ossicle volume. Both phenomena are the results of the remodelling process induced by rhBMP-7, creating a physiological BM compartment while locally inducing osteoclastogenesis and recruiting hematopoietic cells of the murine host.
In this context it was demonstrated that the addition of rhBMP-7 to the BGs induces the development of a morphologically intact bone organ including a functional BM compartment, with cellular composition comparable to the native adult mouse femur. This development of a highly vascularised physiological BM compartment with all its myeloid and lymphoid cellular components might be considered as beneficial in the clinical setting for contaminated or avascular tissue defects.
However, while the remodelling process induced by rhBMP-7 filled the intertrabecular spaces with haematopoietic cells, it also caused a decrease in bone volume-to-total volume ratio. The result is a lower volumetric density of the grafted mass in the BMP+ group as BMPs not only stimulate new bone formation but also promote osteoclastogenesis and thereby graft resorption.
Due to the lack of mature T- and B-cells in NOD/scid mice, this model does not allow to study BMPs role of regulating T-cell development [44] nor the involvement of the adaptive immune system on bone graft resorption. However, a remaining macrophage population within these mice have been shown to be involved in the resorption process (Fig. 7; F4/80). Here, the capacity of BMP-7 to polarise macrophages towards M2 macrophage subpopulation [45, 46] further indicates its importance in tissue repair and the remodelling process.
Overall, bone homeostasis is a fine balance between anabolic and catabolic events influenced by systemic hormones and local secretion of cytokines and growth factors such as BMPs. As this and other studies have shown, BMPs stimulate both anabolic and catabolic processes. This seems self-evident as BMPs induce osteoblastic differentiation and maturation which in turn increases RANK ligand (RANKL) and osteoprotegerin (OPG) expression, the balance of which regulates osteoclast differentiation and activation [47]. In general, BMPs, depending on their subtype and dosage, appear to have different impacts on complex regulatory pathways such as RANKL/OPG or WNT signalling pathways, both of which play a crucial role regulating bone haemostasis [48]. BMP-5 and BMP-6, for example, show a biphasic dose-dependent curve stimulating osteoclastogenesis with an increased osteoclast activity only in a defined dose range [49]. While both BMP-5 and 6 display an overall lower osteoclast activity compared to BMP-2, BMP-5 exhibits a higher osteoblast stimulation compared to BMP-2, initiating mesenchymal stem cell differentiation towards the osteoblast lineage [49]. Drugs that can modulate these regulatory pathways which are initially stimulated by BMP can thus be of utmost interest to improve bone regeneration. In a murine critical size femoral defect model, BMP-2 in combination with systemic OPG application has been shown to induce increased bone volume and a lower rate of osteoclast response, compared to a BMP-2-only control [42]. This, in accordance with studies using bisphosphonates to prevent bone resorption, clearly indicates how controlling osteoclast activity could improve bone healing responses.
Eventually, the model described here could be used to identify the effects of substances like bisphosphonates, OPG or BMP antagonist such as Noggin [50], more meticulously and measure their specific influence on bone remodelling, osteoclastogenesis and ultimately bone graft resorption. The chosen design of this study successfully revealed several effects of rhBMP-7 devoid of external stimuli and most importantly allowed differentiation between catabolic and anabolic events. Excluding load as a relatively inconstant variable can be beneficial in an experimental setting. On the other hand, the implantation at an orthotopic/load bearing site could bring additional valuable insights for the clinic as this setting more closely represents a clinical scenario where external forces influence the process of bone remodelling. Additional biomechanical and molecular analysis could further reveal the impact of BMP and coadministered drugs on biomechanical stability and enhance the knowledge on its multitude of effects on osteoclast homeostasis.
Ultimately, we will use this model to test and find new medications that will favour an anabolic response and attenuate the concomitant catabolic process initiated by BMPs, to decrease bone graft resorption and improve patient outcome. It appears that even 50 years after Urist’s findings on bone morphogenesis, we are still only at the beginning of comprehending the potential of an osteogenic protein with high hopes for complex bone tissue regeneration.
References
Urist MR (1965) Bone: formation by autoinduction. Science 150(3698):893–899
Ripamonti U, Reddi AH (1997) Tissue engineering, morphogenesis, and regeneration of the periodontal tissues by bone morphogenetic proteins. Crit Rev Oral Biol Med 8(2):154–163
Wang EA, Rosen V, D’Alessandro JS, Bauduy M, Cordes P, Harada T et al (1990) Recombinant human bone morphogenetic protein induces bone formation. Proc Natl Acad Sci USA 87(6):2220–2224
Wozney JM, Rosen V (1998) Bone morphogenetic protein and bone morphogenetic protein gene family in bone formation and repair. Clin Orthop Relat Res 346:26–37
Scarfi S (2016) Use of bone morphogenetic proteins in mesenchymal stem cell stimulation of cartilage and bone repair. World J Stem Cells 8(1):1–12
Mi M, Jin H, Wang B, Yukata K, Sheu TJ, Ke QH et al (2013) Chondrocyte BMP2 signaling plays an essential role in bone fracture healing. Gene 512(2):211–218
James AW, LaChaud G, Shen J, Asatrian G, Nguyen V, Zhang X et al (2016) A review of the clinical side effects of bone morphogenetic protein-2. Tissue Eng Part B Rev 22(4):284–297
Tannoury CA, An HS (2014) Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J 14(3):552–559
Schmidmaier G, Capanna R, Wildemann B, Beque T, Lowenberg D (2009) Bone morphogenetic proteins in critical-size bone defects: what are the options? Injury 40(Suppl 3):S39–S43
Giannoudis PV, Tzioupis C (2005) Clinical applications of BMP-7: the UK perspective. Injury 36(Suppl 3):S47–S50
Aspenberg P, Linder L (2001) Impaction grafting. Acta Orthop Scand 72(2):198–199
Wang W, Yeung KWK (2017) Bone grafts and biomaterials substitutes for bone defect repair: a review. Bioact Mater 2(4):224–247
Capanna R, Campanacci DA, Caldora P, De Biase P (2005) Healing of large bone defects with allogenic bone grafts enriched with autologous bone marrow buffy coat and platelet-rich plasma. Orthop Proc 87-B(SUPP_I):59
Sen MK, Miclau T (2007) Autologous iliac crest bone graft: should it still be the gold standard for treating nonunions? Injury 38(Suppl 1):S75–S80
Ng VY (2012) Risk of disease transmission with bone allograft. Orthopedics. 35(8):679–681
Rudert M, Holzapfel BM, von Rottkay E, Holzapfel DE, Noeth U (2015) Impaction bone grafting for the reconstruction of large bone defects in revision knee arthroplasty. Oper Orthop Traumatol 27(1):35–46
Doppelt SH, Tomford WW, Lucas AD, Mankin HJ (1981) Operational and financial aspects of a hospital bone bank. J Bone Joint Surg Am 63(9):1472–1481
Jr. De Long WG, Einhorn TA, Koval K, McKee M, Smith W, Sanders R et al (2007) Bone grafts and bone graft substitutes in orthopaedic trauma surgery. A critical analysis. J Bone Joint Surg Am 89(3):649–658
Faundez A, Tournier C, Garcia M, Aunoble S, Le Huec JC (2016) Bone morphogenetic protein use in spine surgery-complications and outcomes: a systematic review. Int Orthop 40(6):1309–1319
Papanagiotou M, Dailiana ZH, Karachalios T, Varitimidis S, Vlychou M, Hantes M et al (2015) RhBMP-7 for the treatment of nonunion of fractures of long bones. Bone Joint J 97-b(7):997–1003
Granholm S, Henning P, Lindholm C, Lerner UH (2013) Osteoclast progenitor cells present in significant amounts in mouse calvarial osteoblast isolations and osteoclastogenesis increased by BMP-2. Bone. 52(1):83–92
Zheng Y, Wang L, Zhang X, Zhang X, Gu Z, Wu G (2012) BMP2/7 heterodimer can modulate all cellular events of the in vitro RANKL-mediated osteoclastogenesis, respectively, in different dose patterns. Tissue Eng Part A 18(5–6):621–630
Mathavan N, Bosemark P, Isaksson H, Tagil M (2013) Investigating the synergistic efficacy of BMP-7 and zoledronate on bone allografts using an open rat osteotomy model. Bone 56(2):440–448
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Muller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25(7):1468–1486
Holzapfel BM, Hutmacher DW, Nowlan B, Barbier V, Thibaudeau L, Theodoropoulos C et al (2015) Tissue engineered humanized bone supports human hematopoiesis in vivo. Biomaterials 61:103–114
Shahtalebi MA, Asghari GR, Rahmani F, Shafiee F, Jahanian-Najafabadi A (2018) Formulation of herbal gel of antirrhinum majus extract and evaluation of its anti-propionibacterium acne effects. Adv Biomed Res 7:53
Shafiee A, McGovern JA, Lahr CA, Meinert C, Moi D, Wagner F et al (2018) Immune system augmentation via humanization using stem/progenitor cells and bioengineering in a breast cancer model study. Int J Cancer 143:1470–1482
Thibaudeau L, Quent VM, Holzapfel BM, Taubenberger AV, Straub M, Hutmacher DW (2014) Mimicking breast cancer-induced bone metastasis in vivo: current transplantation models and advanced humanized strategies. Cancer Metastasis Rev 33(2–3):721–735
Wagner F, Holzapfel BM, Martine LC, McGovern J, Lahr CA, Boxberg M et al (2019) A humanized bone microenvironment uncovers HIF2 alpha as a latent marker for osteosarcoma. Acta Biomater 89:372–381
Hesami P, Holzapfel BM, Taubenberger A, Roudier M, Fazli L, Sieh S et al (2014) A humanized tissue-engineered in vivo model to dissect interactions between human prostate cancer cells and human bone. Clin Exp Metastasis 31(4):435–446
Holzapfel BM, Wagner F, Loessner D, Holzapfel NP, Thibaudeau L, Crawford R et al (2014) Species-specific homing mechanisms of human prostate cancer metastasis in tissue engineered bone. Biomaterials 35(13):4108–4115
Holzapfel BM, Wagner F, Thibaudeau L, Levesque JP, Hutmacher DW (2015) Concise review: humanized models of tumor immunology in the 21st century: convergence of cancer research and tissue engineering. Stem Cells 33(6):1696–1704
Hutmacher DW, Holzapfel BM, De-Juan-Pardo EM, Pereira BA, Ellem SJ, Loessner D et al (2015) Convergence of regenerative medicine and synthetic biology to develop standardized and validated models of human diseases with clinical relevance. Curr Opin Biotechnol 35:127–132
Thibaudeau L, Holzapfel BM, Hutmacher DW (2015) Humanized mice models for primary bone tumor and bone metastasis research. Cell Cycle 14(14):2191–2192
Seib FP, Berry JE, Shiozawa Y, Taichman RS, Kaplan DL (2015) Tissue engineering a surrogate niche for metastatic cancer cells. Biomaterials 51:313–319
Zhang J, Niu C, Ye L, Huang H, He X, Tong WG et al (2003) Identification of the haematopoietic stem cell niche and control of the niche size. Nature 425(6960):836–841
Su YH, Cai HB, Ye ZY, Tan WS (2015) BMP-7 improved proliferation and hematopoietic reconstitution potential of ex vivo expanded cord blood-derived CD34(+) cells. Hum Cell 28(1):14–21
Sacchetti B, Funari A, Michienzi S, Di Cesare S, Piersanti S, Saggio I et al (2007) Self-renewing osteoprogenitors in bone marrow sinusoids can organize a hematopoietic microenvironment. Cell. 131(2):324–336
Larsson J, Karlsson S (2005) The role of Smad signaling in hematopoiesis. Oncogene 24(37):5676–5692
Wagner F, Holzapfel BM, McGovern JA, Shafiee A, Baldwin JG, Martine LC et al (2018) Humanization of bone and bone marrow in an orthotopic site reveals new potential therapeutic targets in osteosarcoma. Biomaterials 171:230–246
Belfrage O, Flivik G, Sundberg M, Kesteris U, Tagil M (2011) Local treatment of cancellous bone grafts with BMP-7 and zoledronate increases both the bone formation rate and bone density: a bone chamber study in rats. Acta Orthop 82(2):228–233
Bougioukli S, Jain A, Sugiyama O, Tinsley BA, Tang AH, Tan MH et al (2016) Combination therapy with BMP-2 and a systemic RANKL inhibitor enhances bone healing in a mouse critical-sized femoral defect. Bone 84:93–103
Karrholm J, Hourigan P, Timperley J, Razaznejad R (2006) Mixing bone graft with OP-1 does not improve cup or stem fixation in revision surgery of the hip: 5-year follow-up of 10 acetabular and 11 femoral study cases and 40 control cases. Acta Orthop 77(1):39–48
Yoshioka Y, Ono M, Osaki M, Konishi I, Sakaguchi S (2012) Differential effects of inhibition of bone morphogenic protein (BMP) signalling on T-cell activation and differentiation. Eur J Immunol 42(3):749–759
Rocher C, Singla R, Singal PK, Parthasarathy S, Singla DK (2012) Bone morphogenetic protein 7 polarizes THP-1 cells into M2 macrophages. Can J Physiol Pharmacol 90(7):947–951
Singla DK, Singla R, Wang J (2016) BMP-7 treatment increases M2 macrophage differentiation and reduces inflammation and plaque formation in Apo E−/− mice. PLoS ONE 11(1):e0147897
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T et al (1998) Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93(2):165–176
Kamiya N, Mishina Y (2011) New insights on the roles of BMP signaling in bone-A review of recent mouse genetic studies. BioFactors (Oxford, England). 37(2):75–82
Wutzl A, Brozek W, Lernbass I, Rauner M, Hofbauer G, Schopper C et al (2006) Bone morphogenetic proteins 5 and 6 stimulate osteoclast generation. J Biomed Mater Res A 77(1):75–83
Zhu W, Kim J, Cheng C, Rawlins BA, Boachie-Adjei O, Crystal RG et al (2006) Noggin regulation of bone morphogenetic protein (BMP) 2/7 heterodimer activity in vitro. Bone 39(1):61–71
Acknowledgements
Baxter Healthcare Australia kindly provided Fibrin Glue (TISSEEL Fibrin Sealant). The following funding existed during conduction of this study: National Health and Medical Research Council of Australia (Project Grant 1082313 to BMH and DWH), German Research Foundation (DFG HO 5068/1-1 to BMH) and Australian Research Council (IC160100026).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Christoph A. Lahr, Ferdinand Wagner, Abbas Shafiee, Maximilian Rudert, Dietmar W. Hutmacher and Boris Michael Holzapfel declare that there is no conflict of interest.
Human and Animal Rights and Informed Consent
This study was approved by the University Animal Ethics Committee (Approval No. 130/025). All animal experiments were executed in conformity with the national animal care guidelines.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lahr, C.A., Wagner, F., Shafiee, A. et al. Recombinant Human Bone Morphogenetic Protein 7 Exerts Osteo-Catabolic Effects on Bone Grafts That Outweigh Its Osteo-Anabolic Capacity. Calcif Tissue Int 105, 331–340 (2019). https://doi.org/10.1007/s00223-019-00574-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-019-00574-5