Abstract
Bone metastasis is a complication that occurs in 80 % of women with advanced breast cancer. Despite the prevalence of bone metastatic disease, the avenues for its clinical management are still restricted to palliative treatment options. In fact, the underlying mechanisms of breast cancer osteotropism have not yet been fully elucidated due to a lack of suitable in vivo models that are able to recapitulate the human disease. In this work, we review the current transplantation-based models to investigate breast cancer-induced bone metastasis and delineate the strengths and limitations of the use of different grafting techniques, tissue sources, and hosts. We further show that humanized xenograft models incorporating human cells or tissue grafts at the primary tumor site or the metastatic site mimic more closely the human disease. Tissue-engineered constructs are emerging as a reproducible alternative to recapitulate functional humanized tissues in these murine models. The development of advanced humanized animal models may provide better platforms to investigate the mutual interactions between human cancer cells and their microenvironment and ultimately improve the translation of preclinical drug trials to the clinic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Breast cancer is the most commonly diagnosed cancer and one of the leading causes of cancer-related death among women in the western world [1]. At the first diagnosis, most women do not show any clinicopathological signs of overt secondary cancer lesions (metastases), meaning that they can achieve a state of complete clinical remission after surgical treatment in combination with individualized first-line treatment such as chemo-, radio-, and anti-hormonal therapy [2]. The propensity to develop metastases depends on several prognostic factors, including tumor size, histopathological grade, and lymph node status. Development of distant metastases usually occurs in 10–15 % of all breast cancer patients within 3 years of the detection of the primary tumor [3]. However, some breast cancers show a trend for late metastatic recurrence even 10 years or more after initial diagnosis [3]. The skeleton, liver, lung, and brain account for the most common sites affected by breast cancer cell colonization. Metastatic lesions are found at the highest frequency in bone (83 %) whereas liver and lung are usually affected to a lesser extent (27 %) [4]. The median survival after diagnosis of bone metastases is 24–40 months, which is relatively long compared to patients with liver metastasis (3 months) [2]. However, clinical symptoms associated with metastatic bone disease are highly debilitating. Tumor expansion and the associated bone degradation (Fig. 1) can lead to serious morbidity with symptoms such as severe bone pain, pathological fractures, spinal cord compression, bone marrow aplasia, and hypercalcemia [5].
Clinical case of a 42-year-old patient who presented with right-sided hip pain for the previous 3 months. The patient’s history revealed an ablatio mammae and anti-hormonal therapy due to breast cancer. She was diagnosed with a single bone metastasis of breast cancer. a Radiographic examination demonstrated an osteolytic lesion of her right proximal femur with cortex penetration (Lodwick grade III lesion). b Magnetic resonance imaging (coronal, T1-weighted) showed a heterogeneous low-signal intensity lesion with marrow infiltration indicative of a secondary bone tumor. c Postoperative radiographic imaging after proximal femoral resection and replacement of the defect with a tumor-prosthesis. d Histological analysis (H&E) demonstrated infiltrative strands of cancer cells progressively replacing the bone marrow compartment. e High-power view showed a typical phalanx of multinucleated cells (osteoclasts) in resorption pits advancing a front of infiltrative cancer cell clusters and resulting in the lysis of the bone matrix. White arrow head, metastasis. Black arrow head, osteoclast. B, bone. T, tumor
Metastasis to bone occurs via a multistep process initiated by the detachment of single cancer cells from the primary tumor, followed by their invasion into the circulation, their dissemination and implantation at a favorable distant site in bone, and finally the formation of a secondary tumor [6]. Overt bone metastases are classified according to their radiographic appearance as either osteolytic or osteoblastic. Both types of lesions result from an imbalance of the normal bone remodeling process. Osteolytic lesions show an increase in bone resorption caused by activated osteoclasts, while compensatory bone formation is impaired [5]. In contrast, osteoblastic lesions are characterized by disorganized new bone formation and insufficient bone resorption [5]. This classification represents two extremes, as patients can have mixed lesions containing both osteolytic and osteoblastic elements. The majority of breast cancer-related bone metastases are characterized as osteolytic, whereas approximately 15 % are of osteoblastic or mixed entity [5].
Current treatment options for cancer-related bone disease are rarely curative, and advanced pain management is often the major treatment avenue. Palliative treatment with anti-resorptive drugs, such as bisphosphonates and the anti-receptor activator of nuclear factor kappa-B ligand (RANKL) antibody Denosumab have been found to reduce the frequency of skeletal-related events [7, 8]. Additionally, complications associated with tumor-induced bone destruction such as pain and morbidity could be diminished, thus improving the patient’s quality of life but without prolonging survival [7]. However, the development of new curative treatment options is hampered by the fact that the pathophysiological cascade leading to skeletal metastasis is not yet fully deciphered as a consequence of the lack of appropriate model systems. In fact, in vitro models are suitable to answer specific biological questions, but certainly show limitations in mimicking the complex metastatic process. Furthermore, each step of the development of bone metastasis is intimately regulated by the microenvironment encountered by the metastatic cancer cells; thus, suitable animal models are necessary to closely mimic these interactions. This article reviews the current models to investigate breast cancer-induced bone metastases in vivo and delineates their strengths and limitations. The focus is placed on the recent advances provided by the development of humanized murine models and the translation of tissue engineering concepts into models for cancer research.
2 Syngeneic and xenograft transplantation models
Mice and rats are the most extensively utilized and well-characterized species for preclinical research and present obvious practical advantages due to their small size and short generation time. The most common strategies to induce breast cancer-related metastasis to bone in rodents are transplantation models, which can be divided broadly into two categories, namely, syngeneic models and xenografts.
Syngeneic (i.e., allograft) transplantation models refer to the inoculation of rodent cancer cell lines or tissues into an immunocompetent host of the same species and genetic background, allowing the assessment of species-compatible tumor-stroma interactions, endocrine signaling, and intact immune responses during tumor development [9]. Syngeneic models have a short latency for tumor growth and metastasis to bone and can provide useful insights into specific mechanisms of the disease. However, they have a limited potential for direct translation into clinical application due to species-related differences. For example, the clinically proven human monoclonal antibody Denosumab failed to suppress bone resorption in mouse or rat models due to the species specificity in RANKL antigen binding of this antibody [8]. Another limitation of syngeneic models pointed out in the literature is the use of grafts derived from homozygously inbred mice which may lack resemblance to clinical tumors in terms of histopathological and genetic complexity [9, 10]. Nevertheless, a clear heterogeneity in drug sensitivity [11], immunogenic character [12], and metastatic potential [13] has been observed within subpopulations of cancer cells obtained from a single mouse mammary tumor.
Several rodent cancer cell lines have been established either from spontaneous tumors that developed in a particular mouse/rat or from carcinogen-induced tumors and can be applied as syngeneic grafts. Due to recent advances in genetic engineering, an increasing number of new rodent cell lines expressing specific receptors, growth factors, or biomarkers have been derived [14, 15]. However, the use of genetically modified cell lines is not straightforward in syngeneic hosts, because an immune rejection of the exogenously expressed proteins may occur in certain cases [16].
Xenograft models refer to human cancer cells or tissues transplanted into immunocompromised hosts. Most of the mechanistic insights into the process of osteotropic metastasis as well as the identification of novel prognostic and therapeutic agents have been derived from xenograft studies. Xenografted human tumor tissue can retain the cell differentiation, morphology, and molecular signatures of original patient tumors following repeated in vivo passages in mice, making this model relevant for preclinical testing of new therapeutic agents and a potential platform for individualized therapy [17]. Cell line-derived xenografts, however, usually exhibit a lack of tissue organization and consist mostly of proliferating epithelial cells with little associated stroma [9, 17]. Due to prolonged culture in vitro, cell lines lose their cellular heterogeneity [17, 18]. To circumvent this problem, a common approach in bone metastasis research is the use of a panel of cell lines with different organ tropism, metastatic efficiency, and effect on bone (osteolytic and/or osteoblastic) in order to represent the cellular diversity of metastatic breast cancer. Nevertheless, an important limitation of xenograft models is the need for an immunocompromised host to prevent rejection of the grafted human cells. This has a major impact on the predictability for clinical translation as tumor-induced immune responses have been shown to mediate critical steps in the metastatic process [19].
For example, Bidwell et al. identified an Irf7-driven innate immune pathway intrinsic to breast cancer cells and demonstrated that its suppression in the primary tumor enables cells to escape from immunosurveillance and form overt metastases in the bone [20]. Consequently, due to their impaired immune system, xenograft models fail to take into account these escape mechanisms that cancer cells normally have to display in humans. Furthermore inter-species differences between tumor and the host organism have been shown to reduce the relevance and predictive power of the results obtained with xenografts [21].
3 Transplantation methods in models of bone metastasis
3.1 End organ bone colonization models: intra-osseous injections
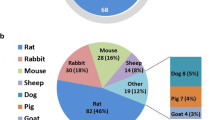
Depending on the stages of the disease that are being assessed, a number of different transplantation methods are utilized in syngeneic and xenograft transplantation models of breast cancer metastasis (Fig. 2). While early studies have shown that intramuscular injection of the Walker 256 rat mammary tumor cells into syngeneic rats generates local metastases to the adjacent bone, the tumors also spread to the kidney, liver, and lungs and proliferated considerably in those organs [22]. A common approach in modeling tumor invasion and growth in bone, i.e., bone colonization, is the intra-osseous injection of cancer cells into the host tibia or femur (Online Resource 1).
Transplantation models recapitulating the bone metastatic cascade. Bone colonization models using intra-osseous injection only mimic the final tumor-stroma interactions at the bone site, while experimental metastasis models include earlier steps of the metastatic process. After systemic injection, the cancer cells first circulate in the bloodstream and form aggregates with other blood cells before arresting and extravasating from distant capillaries into bone. Spontaneous metastasis models using orthotopic transplantation of cancer cells furthermore recapitulate the initial tumor-host interactions at the primary tumor site and the phenotypic changes such as the epithelial to mesenchymal transition (EMT) that cancer cells undergo before detachment and hematogenous dissemination (figure produced using the image bank at www.servier.com with permission from Servier Medical Art)
Direct intra-tibial or intra-femoral implantation of syngeneic rat mammary tumor cells into female rats resulted in reproducible localized osteolytic lesions in the bone, and this method has been utilized in a range of studies investigating bone pain associated with metastasis, the mechanical changes in tumor-harboring bones, and the efficacy of therapeutic agents to reduce tumor burden within the bone [23, 24]. Whereas studies looking at the structural or physiological consequences of tumor-induced bone degradation have been generally carried out in syngeneic rat models, more mechanistic studies can be conducted in mouse models due to the availability of a larger range of cell lines amenable to genetic manipulation. As an example, injection of an αvβ3 overexpressing mouse mammary epithelial cell line 66cl4 through the proximal tibial metaphysis of female Balb/c mice was used to demonstrate the effect of integrin αvβ3 expression in promoting osteoclast recruitment and bone resorption [15].
Similarly, several xenograft models have utilized the injection of a range of human breast cancer cell lines in the long bones of immunodeficient rodents to mimic breast cancer-induced bone colonization. The most common model is the estrogen-independent MDA-MB-231 human breast cancer cell line, which reproducibly generates osteolytic lesions upon intra-osseous inoculation [25, 26]. Depending on the characteristics of the cell line used, the injection of tumor cells into the mouse skeleton may result in osteolytic, osteoblastic, or mixed lesions. For example, the effect of vitamin D deficiency on tumor growth in both osteolytic and osteoblastic bone metastases was investigated by using intra-tibial injection of a variant of the MDA-MB-231 cells with enhanced affinity for bone [27] and the MCF-7 human breast cancer cell line, respectively [28, 29].
Although most bone colonization studies investigate tumor development in the long bones, clinically, the axial skeleton and particularly the spine are the most common target site for bone metastatic disease. Loss of mechanical stability in the vertebral column is associated with intractable local pain and life-threatening complications, including pathological fracture and spinal cord compression leading to paralysis and neurological deficits [30]. Therefore, specific approaches have been developed to reproduce spinal metastatic disease in both syngeneic [31] and xenograft models [32]. For example, subcutaneous tumors obtained by injection of a syngeneic rat breast adenocarcinoma cell line 13762 into the right hind limb of Fisher 344 rats were resected and used as solid tumor grafts for intra-osseous implantation into the thoraco-lumbar vertebra of the rats [31]. Consistent tumor growth in the vertebra as well as the replication of the natural course of metastatic spinal cord compression syndrome could be achieved by this approach.
A distinctive advantage of inoculating cancer cells directly into the bone is that tumor growth is localized at the site of injection; therefore, systemic spread to other organs and the associated morbidity are reduced. Nevertheless, intra-osseous injection models are still characterized by the appearance of paralysis, bone pain, and other debilitating complications that mimic the situation in patients but also limit the experimental time course. Nannuru et al. described an ectopic model of direct breast cancer-bone interactions based on the transplantation of the mouse mammary tumor cell lines 4T1, Cl66, and Cl66M2 mixed in growth-factor-reduced Matrigel directly onto the surface of the calvaria of female BALB/c mice [33]. This system allowed the investigation of the molecular mechanisms of breast cancer-induced osteolysis with no associated complications for up to 4 weeks postimplantation.
A general criticism against intra-osseous transplantation models is that they are a model of primary tumor growth in bone and do not replicate the dissemination process occurring in metastasis. Thus, they can only be applied to investigate the final stage of bone colonization by extravasated cancer cells. The direct injection of a bolus of cells into the bone does not replicate the clinical situation in which tumor cells colonize a distant organ as small aggregates with other cell types [6]. Moreover, the injection itself causes a local bone damage which may activate a nonspecific immune response and changes in the bone metabolism thus impacting the investigation of tumor development [34].
3.2 Experimental bone metastasis models: systemic injections
Experimental metastasis refers to the injection of tumor cells directly into the circulatory system of the host, thereby bypassing the early stages of the metastatic cascade (Online Resource 2). The intravenous injection of tumor cells in the rodent tail vein has been the most common inoculation method in experimental metastasis models, but usually generates predominantly pulmonary metastases [10, 13]. It has been reported that injection of the BO2 xenograft cell line in the tail vein of nude mice led to radiographically detectable osteolytic bone lesions within 18 days, with no associated lung metastases [35]. A study by Garcia et al. using whole-body bioluminescence live imaging demonstrated that B02 cells injected through the lateral tail vein were transiently detected in the lungs within the first 3 h after injection, but overt metastases developed only in bones [36]. Although micrometastases below the detection level of this imaging technique might still persist in the lungs, this observation indicates that there is a preferential development of breast cancer metastases in bone. Thus, the establishment of metastases does not rely solely on the mechanical trapping of cancer cells in the capillary network, which provides additional support for Paget’s seed and soil hypothesis [37].
Most studies on experimental bone metastasis have used alternative routes of inoculation to avoid the trapping of cells in the lung microvasculature, either via injection into the arteries or into the left ventricle of the heart. Early studies using the intra-arterial injection approach to obtain bone metastasis in syngeneic and xenograft models were based on the systemic delivery of the cancer cells, e.g., via the abdominal aorta [38]. This method gave rise to extensive osteolytic bone lesions and hypercalcemia in a high percentage of animals, and was also associated with dissemination to other peripheral organs which caused additional morbidity.
Neudert et al. developed a novel model in which localized tumor growth was achieved by injecting MDA-MB-231 human breast cancer cells into the femoral artery of athymic rats, followed by complete vascular ligation [34]. This approach resulted in a near 100 % take rate and the development of rapidly expanding osteolytic lesions restricted to the distal femur and proximal tibia, thus preventing systemic spread. The delivery of cancer cells via the femoral artery was also used in a syngeneic model of bone metastasis [39]. The artery was surgically exposed and threaded through a bone morphogenetic protein (BMP)-2-loaded hydroxyapatite scaffold which promoted the formation of a collagen-rich osteoid [39]. This study showed that the growth rate of a subsequently injected mammary tumor cell line was significantly enhanced in the presence of the tissue-engineered osteoid. Thus, intra-arterial injection can be utilized either to mimic systemic spread or achieve the development of targeted bone lesions. In the latter case, unlike in intra-osseous injection models, the tumor cells still need to display the ability to extravasate from the blood vessels to arrest in bone.
The intracardiac injection remains the most widely used and reliable method to induce bone metastasis in experimental models. In syngeneic hosts, a number of breast cancer cell lines have been shown to successfully generate osteolytic lesions in the skeleton after left ventricular injection and have been applied in preclinical studies of breast cancer-mediated bone metastasis [13, 40]. In xenograft models, intracardiac injection of MDA-MB-231 cells remains the most widely used system to generate experimental bone metastases from breast cancer [27, 41]. Osteolytic lesions occur in the limbs, vertebrae, pelvis, and maxilla 3 to 5 weeks after cancer cell inoculation and are often associated with typical bone metastatic disease-related symptoms such as hind limb paralysis [41]. However, only few breast cancer cell lines have been described to generate osteoblastic lesions after intracardiac injection. For instance, the MCF-7 human breast cancer cells cause predominantly osteoblastic bone metastases 20–25 weeks after inoculation into the left cardiac ventricle in female nude mice [42]. Yi et al. showed that overexpression of the Neu oncogene in MCF-7 cells resulted in a significantly shorter latency for the development of osteoblastic bone metastases (10–12 weeks) and the increased expression of human platelet-derived growth factor (hPDGF)-BB compared to the parental cells [42]. Inhibition of hPDGF-BB production in MCF-7/Neu cells significantly decreased osteoblastic bone metastases whereas introduction of hPDGF-BB cDNA in the osteolytic MDA-MB-231 cells induced osteoblastic lesions, therefore demonstrating the critical role of this growth factor in the aberrant bone-forming pattern of osteoblastic bone metastases.
Besides providing a system to study the mechanisms by which tumor cells colonize bones or test new treatment strategies, one of the important applications of the intracardiac injection model has been the isolation of breast cancer sublines with enhanced osteotropism and metastatic potential [27, 35]. The procedure involves repeated sequential passages in immunodeficient hosts through left ventricular injection, followed by the in vitro isolation of the metastatic cells from the explanted bone metastases. This method has been utilized by several groups to isolate clones of syngeneic or xenograft cell lines with enhanced bone affinity, and these bone-seeking cell lines have been applied in numerous studies (Online Resource 3).
3.3 Spontaneous bone metastasis models: orthotopic injections
Spontaneous models of metastasis provide a more physiologically relevant system to mimic bone metastasis as they involve the transplantation of cells into an orthotopic site to form a primary tumor, which may subsequently metastasize spontaneously to the skeleton (Online Resource 4). Although many orthotopic transplantation models display metastasis to distant organs such as the lungs, the number of examples which reproducibly generate bone metastases from the primary site is still very limited.
The 4T1 cells belong to a panel of syngeneic tumor lines which were originally isolated from a spontaneous carcinoma in a Balb/cfC3H mouse and displayed a spectrum of different metastatic phenotypes [13, 43]. While some populations metastasized only to the lungs (66cl4) or were nonmetastatic (67NR), the 4T1 cell line demonstrated dissemination to the lungs, liver, and bones after injection into the fourth mammary fat pad (MFP) [13]. Since then, two clonal variants, 4T1.2 and 4T1.13, have been shown to spread to several organs including bone following orthotopic inoculation [13, 43]. Mice bearing 4T1.2 and 4T1.13 tumors developed osteolytic lesions in the femur and spine as well as signs of partial paralysis of the hind limbs, hypercalcemia, and elevated parathyroid hormone-related protein (PTHrP) plasma levels. Thus, the 4T1 cell variants were the first preclinical animal models of spontaneous breast cancer metastasis which reliably metastasized to bone [13]. These syngeneic models of spontaneous bone metastasis provided an experimental system that replicated the entire metastatic process from the primary tumor to the secondary bone site. Moreover the use of genetically matched cell clones with different metastatic profiles allowed the investigation of molecular mechanisms underlying site-specific metastasis. In fact, induction of β3 integrin expression in the formerly nonosteotropic 66 cl4 cells was shown to induce metastasis to the long bones and the spine after MFP implantation, thus indicating the critical role of this integrin in promoting spontaneous metastasis to bone [15].
To date, there is no reproducible xenograft model of spontaneous metastasis to bone. Most human breast cancer cell lines commonly used in experimental metastasis assays either fail to reach or establish secondary growths in the bone from the orthotopic site. Some dissemination to lumbar vertebral bone but not to long bones was observed for the first time in an orthotopic model based on the MKL-4 cell line [44]. Recently, a study by Ghajar et al. demonstrated the presence of dormant disseminated tumor cells in bone 9 weeks after orthotopic injection of green fluorescent protein (GFP)-expressing MDA-MB-231 into the mammary gland of nonobese diabetic severe combined immunodeficient (NOD/SCID) mice [45]. The small GFP-positive and Ki67-negative cell clusters could be found residing directly on the microvascular endothelium of the bone marrow in the femur and tibia [45].
Some groups have investigated the use of fresh patient-derived tumor cells or tissue for orthotopic implantation, but with limited success in reproducing spontaneous metastasis to bone. As an example, one study described the isolation of a range of cell lines from primary or metastatic tumor samples from 49 different breast cancer patients [46]. After transplantation into the cleared MFPs of female NOD/SCID mice, only one primary cell line (HCI-007) developed spontaneous bone metastases in two animals [46].
The only report to date showing spontaneous bone metastasis of human breast cancer cells from the orthotopic site in nude mice that led to histologically detectable osteolytic changes in the bone was described by Hoffman et al. in a review article [47]. The group developed a surgical orthotopic implantation approach as an alternative to the injection of cell suspensions. MDA-MB-435 breast tumor cells, which do not normally metastasize spontaneously to bone upon injection into the MFP, were implanted subcutaneously in nude mice to form hybrid tumors consisting of human cancer cells and mouse stroma. Intact tumor fragments were then transplanted into the MFPs of female nude mice and resulted in tumors that spread to numerous organs and developed osteolytic skeletal metastases in 100 % of animals [47]. This technique may improve reproducibility and metastatic take rates for spontaneous bone metastasis models, and these results underline the importance of the surrounding stroma for tumor progression and the initiation of metastasis. However, to our knowledge, the original results have not yet been published elsewhere.
Besides manipulating the tumor cell characteristics or the implantation technique, another alternative to improve orthotopic models is the use of more permissive hosts. Using a highly immunodeficient double knockout mice model, Rag2−/−;Il2rg−/−, which lacks T, B, and natural killer cell activity, Nanni et al. showed that intra-mammary or subcutaneous injection of the human breast cancer cells MDA-MB-453 and BT-474 resulted in spontaneous multiorgan metastatic spread to all sites commonly affected in human patients, including the bones, over a period of 9–59 weeks [48].
In conclusion, spontaneous metastasis models may replicate a more natural course of metastatic disease compared to experimental models; however, their lower reproducibility and longer time frame still restricts their potential for high-throughput studies such as those needed to test new therapeutic drugs.
4 Humanized models of bone metastasis
An accurate recapitulation of the cancer cell-microenvironment interactions occurring during human cancer progression remains challenging with traditional xenograft models, as there exist species-related incompatibilities between the host and tumor. In particular, different groups have hypothesized that mechanisms governing the establishment of bone metastases could be species-specific [49–51], which may explain in part the rare occurrence of bone metastasis from the orthotopic site in these models. Consequently, recent efforts have been made to develop more advanced humanized xenograft models to overcome these shortcomings. The term “humanized” encompasses a range of different strategies to mimic more closely the human physiology in mouse models, including genetic manipulation to insert human genes into the mouse genome [8], reconstitution of a human immune system [51], and engraftment of human cells or functional human stromal tissues in immunodeficient hosts. In the following section, we will concentrate on the latter and describe how humanizing the primary tumor site and/or the target site for bone metastasis may improve xenograft models of breast cancer metastasis.
4.1 Humanized primary tumor site
The tumor microenvironment significantly influences the development and progression of carcinomas. Although orthotopic transplantation models generally replicate a more natural course of metastasis, there are important microenvironmental differences between the human and mouse mammary gland in terms of tissue composition or host responses that may prevent physiological cancer-stroma interactions and play a role in the low incidence of tumor take rate and metastasis to distant sites [52]. Several studies have directed their efforts toward humanizing the mouse mammary microenvironment to improve the engraftment of normal or malignant human epithelial cells in murine hosts [52, 53]. Partial humanization of the MFP by co-injecting human fibroblasts with xenografted cells orthotopically was shown to promote tumor development [53]. This approach also lead to the increased stromal expression of factors associated with invasiveness [53]. Interestingly, the use of carcinoma-associated fibroblasts extracted from human breast carcinomas has been shown to promote the growth of xenografted breast cancer tumors significantly more than normal mammary fibroblasts derived from the same patients [54].
The first fully humanized mammary gland system was developed by Kuperwasser et al. In this human-in-mouse (HIM) model, human epithelium was engrafted into a previously humanized stromal microenvironment obtained by injecting irradiated and nonirradiated immortalized human mammary fibroblasts into the cleared mammary glands of NOD/SCID mice [55, 56]. After introduction of human mammary epithelial cell organoids into the humanized stroma of the MFP, epithelial outgrowth with ductal, lobular, and acinar structures could be observed. The group was able to show that humanization of the MFP with fibroblasts genetically modified to overexpress hepatocyte growth factor or transforming growth factor β resulted in the outgrowth of lesions with different degrees of malignancy. Furthermore, by introducing genetically engineered human breast epithelial organoids to this system, the effect of specific oncogenes on the development of human breast cancer could be investigated [57]. Thus, modulating the humanized stromal environment allowed mimicking the progressive microenvironmental stages occurring during the early steps of tumor progression. The HIM model provided species-specific interactions and a physiologically relevant environment for the development of human malignant breast tissue, contrary to traditional orthotopic transplantation models.
The mammary stroma regulates tumor formation, malignancy, and invasiveness; therefore, this approach could potentially be applied to improve spontaneous metastasis models. Wang et al. developed the first humanized mouse model integrating orthotopic tumor development and metastasis [58]. In their breast tissue-derived orthotopic and metastatic (BOM) mouse model, normal human breast tissues were implanted subcutaneously in the right and left flank of SCID mice, and one side was inoculated with the human breast cancer cell line MDA-MB-231. Orthotopic tumor formation occurred in 100 % of injected human breast tissue, and metastasis to the contralateral breast tissues was seen in 72.7 % of animals. As a comparison, cells injected subcutaneously had a lower tumor take rate and metastasized preferentially to the mouse tissues. Thus, the BOM model mimicked the species-specific process of tumor progression in a normal human mammary microenvironment and demonstrated preferential metastasis to distant human tissues.
4.2 Humanized metastatic site
The first humanized xenograft models of bone metastatic disease were developed for lung and prostate cancer. Those utilized subcutaneous implants of human fetal or adult bone cores in immunodeficient mice as ectopic target sites for human cancer cell dissemination and growth [49, 50]. Since then, human bone cores have been implemented in different models of breast cancer-related bone metastasis using either a direct inoculation [59, 60], experimental metastasis [61], or spontaneous metastasis approach [62].
In one study, MDA-MB-231 cells or primary metastatic breast tumor tissues from patients were co-implanted with morcellized human bone in the flank of NOD/SCID mice and formed large osteolytic tumors [59, 63]. Metastasis from the initial site of implantation to a second cancer-free human bone implant was observed for the cell line and for four out of ten patient tumor samples. An increase in osteoclast number as well as resorption pits characteristic of osteolytic lesions could be observed. Metastatic lesions were also detected in several host soft tissues but not in femurs; thus, the bone tropism of the human breast tumors was considered to be species specific (other mouse bones were not analyzed). This represented the first mouse model to characterize the behavior and metastatic potential of primary breast cancer tissue from patients in a human bone microenvironment. However, these results contradict the findings of a different study in which MDA-MB-231 cells introduced into human bone implants formed visible tumors, but failed to metastasize to a second tumor-free human bone implant in the opposite flank [60]. These discrepancies could be related to experimental differences in timing for analysis, method of cancer cell injection, or the use of intact bone cores instead of morcellized bone tissue.
Serial transplantation of small fragments of the xenografted patient tumor tissues in morcellized human bone implants resulted in an increased tumor incidence, growth rate, and metastatic potential as well as the downregulation of insulin-like growth factor-binding protein 7 expression, a marker inversely correlated with disease progression in breast cancer [63, 64]. This indicates the isolation of a more aggressive bone metastatic cell subpopulation from the heterogeneous patient-derived breast tumor tissues after repeated in vivo selection in bone. Serial passaging of tumor cells through direct injection into the human bone core has also been applied to isolate the SUM1315-BP2 subline (Online Resource 3) [65]. Compared to the parental SUM1315 cells this “bone-educated” line displayed a unique gene expression signature enriched for genes known to promote metastasis.
The first in vivo model recapitulating the natural bone metastatic cascade of spontaneous human breast cancer metastasis from the orthotopic site to human bone implants was developed by Kuperwasser et al. [62]. They tested a panel of 12 breast cancer cell lines for their osteotropic potential, but only one cell line (SUM1315) gave rise to metastases in human bone and mouse lung in, respectively, 20 and 30 % of mice. Irradiation of the mice with a sublethal dose of radiation 4 weeks postimplantation lead to a significant increase in the number, size, and osteolytic phenotype of the human bone metastases. Whole body X-ray analysis did not detect any lesions to the mouse skeleton; thus, researchers concluded that the SUM1315 cells displayed a species-specific osteotropism from the orthotopic site. However, in a later study by the same group, the use of the more sensitive whole-body bioluminescent imaging technique revealed that both SUM1315 and MDA-MB-231 cells metastasized to human bone, mouse bone, and other organs after MFP injection [66].
Despite the advantages of this humanized model, sourcing and utilizing patient bone tissue is associated with practical issues (Table 1). In particular, assuring the quality and maintaining the functionality of the native bone tissue after implantation is challenging, as the implant may not be vascularized adequately and undergo necrotic or fibrous remodeling. We and others have observed the presence of empty bone lacunae and the frequent infiltration with fibrous tissue effectively replacing the bone marrow in this model (Fig. 3) [51, 62]. This indicates that subcutaneously implanted human bone cores do not replicate a viable bone tissue and thus do not allow studying clinically relevant interactions with tumor cells.
Application of the bone core model does not lead to a physiologically relevant bone implant. Bone cores obtained from the femur head neck of patients undergoing orthopedic surgery are implanted subcutaneously into immunodeficient mice. Following implantation, the trabecular structure and the mineralized bone matrix are preserved in the model. However, hematopoietic cells are missing in the marrow spaces, which are filled with fibrous and adipose tissue, and the absence of osteocytes in the bone lacunae indicates that the bone tissue is not viable. Black circle, empty bone lacunae. B, bone. FT, fibrous tissue. AT, adipose tissue
The formation of a bone marrow niche is critical in metastasis models, since it is well known from the recent literature that osteotropic cancer cells utilize hematopoietic stem cell homing pathways to reach the bone microenvironment [3]. To overcome the limitations of the human bone core model, we have developed a novel approach in which human bone from the reamed acetabular ground is implanted in NOD/SCID mice in combination with recombinant human (rh) BMP-7 (Fig. 4) [51]. This cancellous and therefore highly porous bone can easily be obtained from patients undergoing hip arthroplasty and provides a tissue rich in proliferative bone marrow. When combined with osteogenic growth factors, it leads to a more viable marrow-rich bone implant compared to the bone core model. Furthermore, we were able to show not only that the bone matrix is human-derived but also that some human hematopoietic and mesenchymal cells are retained in the implant (unpublished data) (Fig. 4).
Developing humanized bone microenvironments in murine hosts. a Human bone from the acetabular ground obtained from patients undergoing hip arthroplasty is implanted into immunodeficient hosts in combination with rhBMP-7. The model leads to a viable bone “organ” containing human-derived mineralized and organic bone tissue. Furthermore, residual human hematopoietic (CD34, CD45) and mesenchymal (CD146) stem cells can be detected in the bone marrow niche using human-specific antibodies (brown). b hTEBCs designed using primary human osteoblasts-seeded scaffolds in combination with rhBMP-7 are implanted into immunodeficient hosts. In addition to a high amount of mineralized tissue and large host-derived bone marrow spaces, the hTEBCs lead to a humanized microenvironment containing human-derived bone cells (positive for human nuclear mitotic apparatus protein, NuMA) and extracellular matrix proteins such as collagen I (Col I) and osteocalcin (OC), as shown by immunohistochemical analysis with human-specific antibodies (brown). White arrow head, human hematopoietic or mesenchymal cell. B, bone. BM, bone marrow. BV, blood vessel. NB, new bone
Incorporation of a bone-tissue engineering strategy has the potential to overcome some limitations associated with the use of patient-derived bone tissue and provide more reproducible, controllable, and functional models [67]. Our group has focused on the topic over the last 3 years and shown that new bone tissue formation can be obtained in an ectopic site in a reproducible manner by combining the appropriate living cells, biologically active molecules, and a scaffold in a tissue engineering construct [68, 69]. However, to date, only few tissue engineering models have been applied to the investigation of human diseases, such as bone metastasis [70, 71].
Moreau et al. described the first integration of engineered tissues in a model system of human breast cancer metastasis [70]. Silk scaffolds coupled with BMP-2 and seeded with human bone marrow stromal cells (hBMSCs) were maintained in culture for 1 day, 4, or 7 weeks under osteogenic conditions before subcutaneous implantation in NOD/SCID mice. Four weeks later, SUM1315 cells were injected orthotopically into the mouse MFP. Metastasis was observed by bioluminescent imaging within 3 months, but only to the 1-day scaffolds in two of six animals [70]. This study demonstrated for the first time that engineered microenvironments can be applied as homing sites for metastatic spread from the orthotopic site. However the 4-week and 7-week implants were negative for metastatic spread although more advanced bone formation was obtained in these groups [70]. In fact, the authors described that the 1-day implants conducive to breast cancer cell dissemination consisted mostly of stromal cells and fibroblasts actively remodeling the scaffold and depositing collagen, thus presenting an immature state of bone development [70]. To identify the elements of the engineered construct that contributed to metastatic spread, the use of scaffolds coupled with BMP-2, hBMSC, or BMP-2/hBMSC was compared. All scaffold treatments supported metastasis of SUM1315 but a higher take rate was observed in the BMP-2-only and hBMSC-only treatment groups (4/4 mice) as opposed to the BMP-2/hBMSC combination (1/6) [70]. Thus, metastasis did not occur preferentially to the hBMSC cell groups, which indicates the lack of species-specificity in this homing process.
Our group has developed a unique approach using human tissue-engineered bone constructs (hTEBCs) based on melt electrospun medical grade polycaprolactone scaffolds coated with calcium phosphate and seeded with primary human osteoblastic cells obtained from patients undergoing orthopedic surgery [72–74]. Seeded scaffolds were cultured in vitro under osteogenic conditions before subcutaneous implantation in combination with fibrin glue and rhBMP-7 into NOD/SCID mice. The hTEBCs lead to the formation of a morphologically intact and viable “organ” bone incorporating a high amount of mineralized matrix, human-derived osteoblasts, osteocytes, and bone matrix proteins as well as a host-derived bone marrow (Fig. 4). Importantly, we have shown that the hTEBCs provide a suitable microenvironment for the growth of human breast cancer cells injected directly into or implanted in close proximity to the constructs using a hydrogel carrier (unpublished data) (Fig. 5). We have also demonstrated that hTEBCs can serve as a target site for the dissemination of breast cancer cells injected intracardially [72] (Fig. 5). Using either of the above-mentioned experimental approaches, the osteolytic phenotype characteristic of breast cancer-induced bone metastases could be replicated reproducibly in the hTEBCs (Fig. 5).
Tissue-engineered models of breast cancer-related bone metastasis. a Injection of GFP-labeled breast cancer cells into the hTEBCs results in the colonization of the humanized bone implants detected by whole-body fluorescent imaging. The tumor cells invade the marrow spaces and induce extensive osteoclastic bone resorption as shown by tartrate-resistant acid phosphatase (TRAP) staining (red). b Luciferase-labeled breast cancer cells implanted next to the hTEBCs using hydrogel carriers mimic the invasion of the humanized bone by an extra-osseous tumor, as imaged by whole-body bioluminescent imaging. At the tumor-bone interface, osteolysis induced by TRAP-positive osteoclasts can be observed. c Breast cancer cells injected intracardially disseminate to several mouse organs including reproducibly to the hTEBCs, as detected by fluorescent imaging, and form osteolytic lesions in the new bone. Black arrow heads, osteoclasts. T, tumor. NB, new bone. Sc, scaffold. BM, bone marrow
4.3 Humanized primary and metastatic site
To date, there have been few attempts to combine the two approaches of a humanized orthotopic site and a humanized bone site in a xenograft model of metastasis. Kuperwasser et al. showed that co-injection of human breast cancer cell lines with hBMSCs in the MFP influenced tumor development and metastatic potential [65]. Whereas no increase in metastasis frequency was observed for SUM1315 cells, both SUM1315-BP2 and MDA-MB-231 cells exhibited a significant increase in skeletal metastasis to human bone grafts and mouse hind limbs when co-injected with hBMSCs [65]. These results suggest that humanization of the primary tumor site may influence tumor cell proliferation and metastasis to human bone.
This approach was also used by Xia et al. in their BOM model by incorporating both subcutaneous human bone cores and breast implants in SCID mice [60, 75]. MDA-MB-231 and MDA-231BO cells exhibited significantly higher tumorigenicity upon injection into human tissues (breast and bone) compared to mouse tissue (MFP), suggesting that species-specific microenvironmental factors promote human cancer cell proliferation; however, metastasis to bone was not observed [60]. Using the same model, SUM1315 cells were injected into the human breast implants and demonstrated species-specific homing to human bone cores in 7/10 mice after 9 weeks [75]. The use of human bone implants is associated with the above-mentioned issues, such as poor viability and functionality of the tissue (Fig. 3; Table 1). Nevertheless, this approach might be classified as the first humanized xenograft model of spontaneous breast cancer-induced bone metastasis involving a human-derived orthotopic site, metastatic site, and cancer cells in a murine host. Gene expression profiles of the cells isolated from the primary and metastatic tumors showed significant differences compared to the parental cells, suggesting that this novel humanized model is a useful tool for investigating the genetic requirements for human breast cancer bone metastasis [75].
5 Conclusion
In vivo models allow replicating the reciprocal interactions between tumor and stroma as well as the complexity of the metastatic process. They are essential research tools to dissect the mechanism involved in breast cancer metastasis and test new therapeutics. In general, transplantation models provide the best approach to mimic breast cancer metastasis and can be tailored using a wide range of surgical techniques, cell lines, and host animals. While syngeneic models are useful to investigate biomechanical changes in bone or specific molecular interactions between tumor cells and their species-compatible microenvironment, translation to human patients is more straightforward with xenograft models.
Current xenograft models still present major caveats. Firstly, most preclinical studies still employ immortalized human cell lines which do not represent the heterogeneity of breast cancer in terms of histological subtypes and hormone status. Furthermore, the surrounding stroma at the side of transplantation is normal and not “cancer associated,” which does not necessarily recapitulate all of the interactions occurring during tumor initiation and progression. Finally, the requirement for immunodeficient hosts prevents studies looking at the role of the immune system during metastasis.
Humanized xenograft models are a promising alternative to mimic more closely the human disease. Humanization of the host mammary gland via tissue engineering methods has been applied previously to replicate the progressive stromal and epithelial changes occurring at the primary site. Therefore, engineering of the tumor microenvironment may not only provide a humanized microenvironment but may also be applied to induce a more natural process of tumor formation. Humanization of the target bone site can improve metastatic take rates and provides more relevant species-specific tumor-bone interactions. Another important feature of the use of humanized bone constructs is the ability to recapitulate the hematopoietic niche and thus recreate a partial human immune system in an immunodeficient host. Finally, tissue engineering provides a reproducible approach to recreate functional human tissues in mice and may potentially be applied to develop fully humanized xenograft models to investigate the entire cascade of human breast cancer-induced metastasis to bone in a murine host.
However, future refinements of animal models of bone metastasis will not solely depend on the improvements in surgical techniques, gene technology, or tissue engineering science but also on the implementation with better means of data acquisition. Combining advanced animal models with emerging sensitive and noninvasive imaging techniques is crucial to allow more precise tracking of tumor cell behavior and enhance the benefit towards clinical translation obtained from these preclinical animal studies.
References
Siegel, R., Ma, J., Zou, Z., & Jemal, A. (2014). Cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 64(1), 9–29. doi:10.3322/caac.21208.
Coleman, R. E. (1997). Skeletal complications of malignancy. [Review]. Cancer, 80(8 Suppl), 1588–1594.
Psaila, B., Kaplan, R. N., Port, E. R., & Lyden, D. (2006). Priming the 'soil' for breast cancer metastasis: the pre-metastatic niche. [Research Support, N.I.H., Extramural. Research Support, Non-U.S. Gov't. Review]. Breast Disease, 26, 65–74.
Yoneda, T., & Hiraga, T. (2005). Crosstalk between cancer cells and bone microenvironment in bone metastasis. [Review]. Biochemical and Biophysical Research Communications, 328(3), 679–687. doi:10.1016/j.bbrc.2004.11.070.
Kozlow, W., & Guise, T. A. (2005). Breast cancer metastasis to bone: mechanisms of osteolysis and implications for therapy. Journal of Mammary Gland Biology and Neoplasia, 10(2), 169–180.
Buijs, J. T., & van der Pluijm, G. (2009). Osteotropic cancers: from primary tumor to bone. Cancer Letters, 273(2), 177–193. doi:10.1016/j.canlet.2008.05.044.
Brown, J. E., Neville-Webbe, H., & Coleman, R. E. (2004). The role of bisphosphonates in breast and prostate cancers. [Review]. Endocrine-Related Cancer, 11(2), 207–224.
Kostenuik, P. J., Nguyen, H. Q., McCabe, J., Warmington, K. S., Kurahara, C., Sun, N., et al. (2009). Denosumab, a fully human monoclonal antibody to RANKL, inhibits bone resorption and increases BMD in knock-in mice that express chimeric (murine/human) RANKL. Journal of Bone and Mineral Research, 24(2), 182–195. doi:10.1359/jbmr.081112.
Pearson, H., & Pouliot, N. (2012). Modeling Metastasis In Vivo. In: Madame Curie Bioscience Database [Internet]. Austin (TX): Landes Bioscience, Available from: http://www.ncbi.nlm.nih.gov/books/NBK100378/.
Khanna, C., & Hunter, K. (2005). Modeling metastasis in vivo. Carcinogenesis, 26(3), 513–523. doi:10.1093/carcin/bgh261.
Heppner, G. H., Dexter, D. L., DeNucci, T., Miller, F. R., & Calabresi, P. (1978). Heterogeneity in drug sensitivity among tumor cell subpopulations of a single mammary tumor. Cancer Research, 38(11 Part 1), 3758–3763.
Miller, F. R., & Heppner, G. H. (1979). Immunologic heterogeneity of tumor cell subpopulations from a single mouse mammary tumor. Journal of the National Cancer Institute, 63(6), 1457–1463. doi:10.1093/jnci/63.6.1457.
Lelekakis, M., Moseley, J. M., Martin, T. J., Hards, D., Williams, E., Ho, P., et al. (1999). A novel orthotopic model of breast cancer metastasis to bone. Clinical and Experimental Metastasis, 17(2), 163–170. doi:10.1023/a:1006689719505.
Bolin, C., Sutherland, C., Tawara, K., Moselhy, J., & Jorcyk, C. (2012). Novel mouse mammary cell lines for in vivo bioluminescence imaging (BLI) of bone metastasis. Biological Procedures Online, 14(1), 6.
Sloan, E., Pouliot, N., Stanley, K., Chia, J., Moseley, J., Hards, D., et al. (2006). Tumor-specific expression of alphavbeta3 integrin promotes spontaneous metastasis of breast cancer to bone. Breast Cancer Research, 8(2), R20.
Song, H., Shahverdi, K., Huso, D. L., Wang, Y., Fox, J. J., Hobbs, R. F., et al. (2008). An immunotolerant HER-2/neu transgenic mouse model of metastatic breast cancer. Clinical Cancer Research, 14(19), 6116–6124. doi:10.1158/1078-0432.ccr-07-4672.
Marangoni, E., Vincent-Salomon, A., Auger, N., Degeorges, A., Assayag, F., de Cremoux, P., et al. (2007). A New model of patient tumor-derived breast cancer xenografts for preclinical assays. Clinical Cancer Research, 13(13), 3989–3998. doi:10.1158/1078-0432.ccr-07-0078.
Keller, P. J., Lin, A. F., Arendt, L. M., Klebba, I., Jones, A. D., Rudnick, J. A., et al. (2010). Mapping the cellular and molecular heterogeneity of normal and malignant breast tissues and cultured cell lines. Breast Cancer Research, 12(5), 21.
DeNardo, D., Johansson, M., & Coussens, L. (2008). Immune cells as mediators of solid tumor metastasis. Cancer and Metastasis Reviews, 27(1), 11–18. doi:10.1007/s10555-007-9100-0.
Bidwell, B. N., Slaney, C. Y., Withana, N. P., Forster, S., Cao, Y., Loi, S., et al. (2012). Silencing of Irf7 pathways in breast cancer cells promotes bone metastasis through immune escape. Nat Med, 18(8), 1224-1231, doi:10.1038/nm.2830 http://www.nature.com/nm/journal/v18/n8/abs/nm.2830.html#supplementary-information.
Tolcher, A. W., Sugarman, S., Gelmon, K. A., Cohen, R., Saleh, M., Isaacs, C., et al. (1999). Randomized phase II study of BR96-doxorubicin conjugate in patients with metastatic breast cancer. Journal of Clinical Oncology, 17(2), 478–484.
Kostenuik, P., Singh, G., Suyama, K., & Orr, F. W. (1992). A quantitative model for spontaneous bone metastasis: evidence for a mitogenic effect of bone on Walker 256 cancer cells. Clinical & Experimental Metastasis, 10(6), 403–410. doi:10.1007/bf00133469.
Kurth, A. H. A., Wang, C., Hayes, W. C., & Shea, M. (2001). The evaluation of a rat model for the analysis of densitometric and biomechanical properties of tumor-induced osteolysis. Journal of Orthopaedic Research, 19(2), 200–205. doi:10.1016/s0736-0266(00)90014-7.
Medhurst, S. J., Walker, K., Bowes, M., Kidd, B. L., Glatt, M., Muller, M., et al. (2002). A rat model of bone cancer pain. Pain, 96(1–2), 129–140. doi:10.1016/s0304-3959(01)00437-7.
Buijs, J. T., Henriquez, N. V., van Overveld, P. G. M., van der Horst, G., Que, I., Schwaninger, R., et al. (2007). Bone morphogenetic protein 7 in the development and treatment of bone metastases from breast cancer. Cancer Research, 67(18), 8742–8751. doi:10.1158/0008-5472.can-06-2490.
Yang, R.-S., Tang, C.-H., Chuang, W.-J., Huang, T.-H., Peng, H.-C., Huang, T.-F., et al. (2005). Inhibition of tumor formation by snake venom disintegrin. Toxicon, 45(5), 661–669. doi:10.1016/j.toxicon.2005.01.013.
Yoneda, T., Williams, P. J., Hiraga, T., Niewolna, M., & Nishimura, R. (2001). A bone-seeking clone exhibits different biological properties from the MDA-MB-231 parental human breast cancer cells and a brain-seeking clone in vivo and in vitro. Journal of Bone and Mineral Research, 16(8), 1486–1495. doi:10.1359/jbmr.2001.16.8.1486.
Ooi, L. L., Zhou, H., Kalak, R., Zheng, Y., Conigrave, A. D., Seibel, M. J., et al. (2010). Vitamin D deficiency promotes human breast cancer growth in a murine model of bone metastasis. Cancer Research, 70(5), 1835–1844. doi:10.1158/0008-5472.can-09-3194.
Ooi, L. L., Zheng, Y., Zhou, H., Trivedi, T., Conigrave, A. D., Seibel, M. J., et al. (2010). Vitamin D deficiency promotes growth of MCF-7 human breast cancer in a rodent model of osteosclerotic bone metastasis. Bone, 47(4), 795–803. doi:10.1016/j.bone.2010.07.012.
Cossigny, D., & Quan, G. Y. (2012). In vivo animal models of spinal metastasis. Cancer and Metastasis Reviews, 31(1–2), 99–108. doi:10.1007/s10555-011-9332-x.
Zibly, Z., Schlaff, C. D., Gordon, I., Munasinghe, J., & Camphausen, K. A. (2012). A novel rodent model of spinal metastasis and spinal cord compression. BMC Neuroscience, 13(137), 1471–2202.
Liang, H., Ma, S. Y., Mohammad, K., Guise, T. A., Balian, G., & Shen, F. H. (1976). The reaction of bone to tumor growth from human breast cancer cells in a rat spine single metastasis model. Spine, 36(7), 497–504.
Nannuru, K., Futakuchi, M., Sadanandam, A., Wilson, T., Varney, M., Myers, K., et al. (2009). Enhanced expression and shedding of receptor activator of NF-κB ligand during tumor–bone interaction potentiates mammary tumor-induced osteolysis. Clinical & Experimental Metastasis, 26(7), 797–808. doi:10.1007/s10585-009-9279-2.
Neudert, M., Fischer, C., Krempien, B., Bauss, F., & Seibel, M. J. (2003). Site-specific human breast cancer (MDA-MB-231) metastases in nude rats: model characterisation and in vivo effects of ibandronate on tumour growth. International Journal of Cancer, 107(3), 468–477.
Peyruchaud, O., Winding, B., Pecheur, I., Serre, C. M., Delmas, P., & Clezardin, P. (2001). Early detection of bone metastases in a murine model using fluorescent human breast cancer cells: application to the use of the bisphosphonate zoledronic acid in the treatment of osteolytic lesions. Journal of Bone and Mineral Research, 16(11), 2027–2034.
Garcia, T., Jackson, A., Bachelier, R., Clément-Lacroix, P., Baron, R., Clézardin, P., et al. (2008). A convenient clinically relevant model of human breast cancer bone metastasis. Clinical & Experimental Metastasis, 25(1), 33–42. doi:10.1007/s10585-007-9099-1.
Paget, S. (1889). The distribution of secondary growths in cancer of the breast. The Lancet, 133(3421), 571–573.
Powles, T. J., Clark, S. A., Easty, D. M., Easty, G. C., & Neville, A. M. (1973). The inhibition by aspirin and indomethacin of Osteolytic tumour deposits and hypercalcaemia in rats with Walker tumour, and its possible application to human breast cancer. British Journal of Cancer, 28(4), 316–321.
Halpern, J., Lynch, C. C., Fleming, J., Hamming, D., Martin, M. D., Schwartz, H. S., et al. (2006). The application of a murine bone bioreactor as a model of tumor: bone interaction. [Article]. Clinical & Experimental Metastasis, 23(7–8), 345–356. doi:10.1007/s10585-006-9044-8.
Ono, K., Akatsu, T., Murakami, T., Kitamura, R., Yamamoto, M., Shinomiya, N., et al. (2002). Involvement of cyclo-oxygenase-2 in osteoclast formation and bone destruction in bone metastasis of mammary carcinoma cell lines. Journal of Bone and Mineral Research, 17(5), 774–781.
Sasaki, A., Boyce, B. F., Story, B., Wright, K. R., Chapman, M., Boyce, R., et al. (1995). Bisphosphonate risedronate reduces metastatic human breast cancer burden in bone in nude mice. Cancer Research, 55(16), 3551–3557.
Yi, B., Williams, P. J., Niewolna, M., Wang, Y., & Yoneda, T. (2002). Tumor-derived platelet-derived growth factor-BB plays a critical role in osteosclerotic bone metastasis in an animal model of human breast cancer. Cancer Research, 62(3), 917–923.
Eckhardt, B. L., Parker, B. S., van Laar, R. K., Restall, C. M., Natoli, A. L., Tavaria, M. D., et al. (2005). Genomic analysis of a spontaneous model of breast cancer metastasis to bone reveals a role for the extracellular matrix. Molecular Cancer Research, 3(1), 1–13.
Kurebayashi, J., Nukatsuka, M., Fujioka, A., Saito, H., Takeda, S., Unemi, N., et al. (1997). Postsurgical oral administration of uracil and tegafur inhibits progression of micrometastasis of human breast cancer cells in nude mice. Clinical Cancer Research, 3(5), 653–659.
Ghajar, C. M., Peinado, H., Mori, H., Matei, I. R., Evason, K. J., Brazier, H., et al. (2013). The perivascular niche regulates breast tumour dormancy. Nature Cell Biology, 15(7), 807–817.
DeRose, Y. S., Wang, G., Lin, Y.-C., Bernard, P. S., Buys, S. S., Ebbert, M. T. W., et al. (2011). Tumor grafts derived from women with breast cancer authentically reflect tumor pathology, growth, metastasis and disease outcomes. Nat Med, 17(11), 1514-1520, doi:10.1038/nm.2454 http://www.nature.com/nm/journal/v17/n11/abs/nm.2454.html#supplementary-information.
Hoffman, R. M. (1999). Orthotopic metastatic mouse models for anticancer drug discovery and evaluation: a bridge to the clinic. Investigational New Drugs, 17(4), 343–360. doi:10.1023/a:1006326203858.
Nanni, P., Nicoletti, G., Palladini, A., Croci, S., Murgo, A., Ianzano, M. L., et al. (2012). Multiorgan metastasis of human HER-2+ breast cancer in Rag2−/−;Il2rg−/− mice and treatment with PI3K inhibitor. PLoS ONE, 7(6), e39626. doi:10.1371/journal.pone.0039626.
Shtivelman, E., & Namikawa, R. (1995). Species-specific metastasis of human tumor cells in the severe combined immunodeficiency mouse engrafted with human tissue. Proceedings of the National Academy of Sciences, 92(10), 4661–4665.
Yonou, H., Yokose, T., Kamijo, T., Kanomata, N., Hasebe, T., Nagai, K., et al. (2001). Establishment of a novel species- and tissue-specific metastasis model of human prostate cancer in humanized Non-obese diabetic/severe combined immunodeficient mice engrafted with human adult lung and bone. Cancer Research, 61(5), 2177–2182.
Holzapfel, B. M., Thibaudeau, L., Hesami, P., Taubenberger, A., Holzapfel, N. P., Mayer-Wagner, S., et al. (2013). Humanised xenograft models of bone metastasis revisited: novel insights into species-specific mechanisms of cancer cell osteotropism. Cancer Metastasis Reviews. doi:10.1007/s10555-013-9437-5.
Parmar, H., & Cunha, G. R. (2004). Epithelial-stromal interactions in the mouse and human mammary gland in vivo. Endocrine-Related Cancer, 11(3), 437–458.
Olsen, C., Moreira, J., Lukanidin, E., & Ambartsumian, N. (2010). Human mammary fibroblasts stimulate invasion of breast cancer cells in a three-dimensional culture and increase stroma development in mouse xenografts. BMC Cancer, 10(1), 444.
Orimo, A., Gupta, P. B., Sgroi, D. C., Arenzana-Seisdedos, F., Delaunay, T., Naeem, R., et al. (2005). Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell, 121(3), 335–348. doi:10.1016/j.cell.2005.02.034.
Kuperwasser, C., Chavarria, T., Wu, M., Magrane, G., Gray, J. W., Carey, L., et al. (2004). Reconstruction of functionally normal and malignant human breast tissues in mice. Proceedings of the National Academy of Sciences of the United States of America, 101(14), 4966–4971. doi:10.1073/pnas.0401064101.
Proia, D. A., & Kuperwasser, C. (2006). Reconstruction of human mammary tissues in a mouse model. Nature Protocols, 1(1), 206–214. doi:10.1038/nprot.2006.31.
Wu, M., Jung, L., Cooper, A. B., Fleet, C., Chen, L., Breault, L., et al. (2009). Dissecting genetic requirements of human breast tumorigenesis in a tissue transgenic model of human breast cancer in mice. Proceedings of the National Academy of Sciences. doi:10.1073/pnas.0811785106.
Wang, J., Xia, T.-S., Liu, X.-A., Ding, Q. D., Qing, Yin, H., & Wang, S. (2010). A novel orthotopic and metastatic mouse model of breast cancer in human mammary microenvironment. Breast Cancer Research and Treatment, 120, 337–344.
Yang, W., Lam, P., Kitching, R., Kahn, H., Yee, A., Aubin, J. E., et al. (2007). Breast cancer metastasis in a human bone NOD/SCID mouse model. Cancer Biology & Therapy, 6(8), 1295–1300.
Xia, T. S., Wang, J., Yin, H., Ding, Q., Zhang, Y. F., Yang, H. W., et al. (2010). Human tissue-specific microenvironment: an essential requirement for mouse models of breast cancer. Oncology Reports, 24(1), 203–211.
Ling, L. J., Wang, S., Liu, X. A., Shen, E. C., Ding, Q., Lu, C., et al. (2008). A novel mouse model of human breast cancer stem-like cells with high CD44 + CD24-/lower phenotype metastasis to human bone. Chinese Medical Journal, 121(20), 1980–1986.
Kuperwasser, C., Dessain, S., Bierbaum, B. E., Garnet, D., Sperandio, K., Gauvin, G. P., et al. (2005). A mouse model of human breast cancer metastasis to human bone. Cancer Research, 65(14), 6130–6138. doi:10.1158/0008-5472.can-04-1408.
Lam, P., Yang, W., Amemiya, Y., Kahn, H., Yee, A., Holloway, C., et al. (2009). A human bone NOD/SCID mouse model to distinguish metastatic potential in primary breast cancers. Cancer Biology & Therapy, 8(11), 1010–1017.
Amemiya, Y., Yang, W., Benatar, T., Nofech-Mozes, S., Yee, A., Kahn, H., et al. (2011). Insulin like growth factor binding protein-7 reduces growth of human breast cancer cells and xenografted tumors. Breast Cancer Research and Treatment, 126(2), 373–384.
Goldstein, R. H., Reagan, M. R., Anderson, K., Kaplan, D. L., & Rosenblatt, M. (2010). Human bone marrow–derived MSCs can home to orthotopic breast cancer tumors and promote bone metastasis. Cancer Research, 70(24), 10044–10050. doi:10.1158/0008-5472.can-10-1254.
Liu, S., Goldstein, R. H., Scepansky, E. M., & Rosenblatt, M. (2009). Inhibition of Rho-associated kinase signaling prevents breast cancer metastasis to human bone. Cancer Research, 69(22), 8742–8751. doi:10.1158/0008-5472.can-09-1541.
Hutmacher, D. W. (2010). Biomaterials offer cancer research the third dimension. Nature Materials, 9(2), 90–93. doi:10.1038/nmat2619.
Vaquette, C., Ivanovski, S., Hamlet, S. M., & Hutmacher, D. W. (2013). Effect of culture conditions and calcium phosphate coating on ectopic bone formation. Biomaterials, 34(22), 5538–5551. doi:10.1016/j.biomaterials.2013.03.088.
Reichert, J. C., Quent, V. M., Noth, U., & Hutmacher, D. W. (2011). Ovine cortical osteoblasts outperform bone marrow cells in an ectopic bone assay. Journal of Tissue Engineering and Regenerative Medicine, 5(10), 831–844. doi:10.1002/term.392.
Moreau, J. E., Anderson, K., Mauney, J. R., Nguyen, T., Kaplan, D. L., & Rosenblatt, M. (2007). Tissue-engineered bone serves as a target for metastasis of human breast cancer in a mouse model. Cancer Research, 67(21), 10304–10308.
Schuster, J., Zhang, J., & Longo, M. (2006). A novel human osteoblast-derived severe combined immunodeficiency mouse model of bone metastasis. Journal of Neurosurgery. Spine, 4(5), 388–391.
Thibaudeau, L., Taubenberger, A. V., Holzapfel, B. M., Quent, V. M., Fuehrmann, T., Hesami, P., et al. (2014). A tissue-engineered humanized xenograft model of human breast cancer metastasis to bone. Disease Models & Mechanisms, 7(2), 299–309. doi:10.1242/dmm.014076.
Hesami, P., Holzapfel, B. M., Taubenberger, A., Roudier, M., Fazli, L., Sieh, S., et al. (2014). A humanized tissue-engineered in vivo model to dissect interactions between human prostate cancer cells and human bone. Clinical and Experimental Metastasis. doi:10.1007/s10585-014-9638-5.
Holzapfel, B. M., Wagner, F., Loessner, D., Holzapfel, N. P., Thibaudeau, L., Crawford, R., et al. (2014). Species-specific homing mechanisms of human prostate cancer metastasis in tissue engineered bone. Biomaterials. doi:10.1016/j.biomaterials.2014.01.062.
Xia, T.-S., Wang, G.-Z., Ding, Q., Liu, X.-A., Zhou, W.-B., Zhang, Y.-F., et al. (2011). Bone metastasis in a novel breast cancer mouse model containing human breast and human bone. Breast Cancer Research and Treatment, 1-16, doi:10.1007/s10549-011-1496-0
Acknowledgments
Some figures were produced using the image bank at www.servier.com with permission from Servier Medical Art. The work presented by the authors is supported by the Australian Research Council and the National Health and Medical Research Council. A.V.T. and B.M.H. are supported by the German Research Foundation (DFG HO 5068/1-1 to B.M.H.).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Thibaudeau, L., Quent, V.M., Holzapfel, B.M. et al. Mimicking breast cancer-induced bone metastasis in vivo: current transplantation models and advanced humanized strategies. Cancer Metastasis Rev 33, 721–735 (2014). https://doi.org/10.1007/s10555-014-9499-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-014-9499-z