Abstract
Rationale
Over the past decade, adolescent cigarette smoking has been declining. However, adolescent nicotine consumption via electronic cigarettes is rapidly gaining popularity. Earlier onset nicotine use is associated with increased risk of dependence. A bidirectional relationship between nicotine and stress exists; perceived stress is a predictor for nicotine use, and stress reduction is a commonly reported reason for using nicotine.
Objectives
We assessed the prolonged impact of adolescent high-dose nicotine and/or footshock exposure on adult nicotine self-administration, anxiety-like behaviour, and hormonal responsivity.
Methods
During adolescence (postnatal day [P]28-56) male Sprague-Dawley rats were assigned to one of five groups: saline (SALPRE: 1 ml/kg, SC, every day), nicotine (NICPRE: 1 mg/kg, SC, alternating daily with saline; 14 total nicotine injections), footshock (SHOCKPRE: 8 of 0.5 s, 0.8 mA alternating sessions; saline every day), or combination nicotine and footshock (NIC+SHOCK: concurrent and alternating daily with saline, or NIC–SHOCK: alternating with saline on shock sessions). On P70, one cohort underwent spontaneous intravenous nicotine self-administration (0.03 mg/kg/infusion); another cohort was assessed for open-field behaviour (P71), then corticosterone (CORT) response to nicotine or footshock in adulthood (P72-73).
Results
Intermittent adolescent nicotine or footshock alone (NICPRE and SHOCKPRE) did not potentiate adult spontaneous nicotine intake compared to SALPRE. However, both combination groups (NIC+SHOCK, NIC–SHOCK) showed increased adult nicotine consumption without associated differences in baseline anxiety-like behaviour or CORT response.
Conclusions
Adolescent nicotine and footshock stressors have a synergistic effect on adult nicotine consumption, enhancing nicotine intake. Avenues toward reducing stress in adolescent nicotine users may provide opportunities to reduce vulnerability to adult nicotine consumption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The last decade has seen a steady decline in tobacco use among adolescence. However, use of the primary reinforcer found in tobacco, nicotine, has become extremely popular among the current generation of adolescents via the use of electronic cigarettes (Miech et al. 2019). The newer generation pod devices, including the brand name product JUUL, contain high nicotine content e-liquids, which when inhaled, produce similar or higher plasma levels of nicotine compared to a traditional cigarette (Goniewicz et al. 2019; Reilly et al. 2019), and can even produce blood serum nicotine levels in rats that are about threefold higher than a traditional cigarette or previous generation e-cigarettes after a 20-min exposure (Rao et al. 2020).
E-cigarette use in youth is common among individuals that have never smoked cigarettes, and is associated with increased intentions to smoke cigarettes, and initiation and establishment of cigarette smoking (Bunnell et al. 2015; Loukas et al. 2018; Primack et al. 2018; Chaffee et al. 2018). In humans, early initiation of nicotine consumption is associated with increased consumption and lower probability of quitting (Chen and Millar 1998), and in rodents when nicotine self-administration begins in adolescence, there is greater nicotine consumed compared to rats with adult-onset self-administration (Levin et al. 2003, 2007). Due to the rising popularity of nicotine use via e-cigarettes in adolescents, it is important to investigate the long-lasting effects of this high-dose nicotine exposure (Goniewicz et al. 2019; Reilly et al. 2019; Miech et al. 2019; Rao et al. 2020).
In rodents, adolescents are more sensitive to the reinforcing, rewarding, and analgesic effects of nicotine (Shram et al. 2006; Kota et al. 2007; Ahsan et al. 2014; Frie et al. 2020), and less sensitive to its aversive effects (Le Foll and Goldberg 2005; Shram et al. 2008), and show fewer withdrawal symptoms than adults (O’Dell et al. 2007). Adolescent nicotine use is also associated with increased anxiety-like (Slawecki et al. 2003; Smith et al. 2006), and depressive-like behaviour (Iñiguez et al. 2009), and decreased sensitivity to a natural sucrose reward (Iñiguez et al. 2009)—all risk factors for nicotine use disorder (Laje et al. 2001; Morisette et al. 2007). Adolescent nicotine preexposure can also reduce the aversive effects of nicotine in adulthood at a dose that is aversive to drug-naïve rats (Torres et al. 2008)—indicating that adolescent nicotine exposure can alter future perception of the stimulus effects of nicotine in a way that may encourage consumption. Higher levels of intravenous (IV) (Levin et al. 2003, 2007) and oral (Nesil et al. 2011) nicotine self-administration is also observed in male (Levin et al. 2007) and female (Levin et al. 2003) adolescent-onset rats compared to adult-onset rats. Adolescent nicotine preexposure has also been shown to increase subsequent adult oral (Cole et al. 2019) and IV nicotine consumption (Adriani et al. 2003; Natividad et al. 2013).
Furthermore, there are interactions between nicotine use and stress experience. An online survey by the American Psychological Association found that adolescents reported their stress levels were higher than what they believed to be healthy, and higher than stress levels reported by adults (Anderson et al. 2014). Whether teens experience more stress or just perceive more stress may not matter, as perceived stress is also a predictor of future nicotine consumption, including vaping (Leventhal et al. 2017). Indeed, a bidirectional relationship exists between nicotine and stress; stress and perceived stress are predictors of nicotine use (Leventhal et al. 2017), and nicotine use relieves stress (Gilbert et al. 1989). In rats, footshock stress 24 h before place conditioning enhanced nicotine reward (Brielmaier et al. 2011), and the pharmacological stressor yohimbine immediately enhanced nicotine reinforcement and motivation to self-administer IV nicotine in male and female rats (Li et al. 2014). Nicotine can also function as a stressor, as it dose-dependently increases corticosterone (CORT) levels (Porcu et al. 2003), a glucocorticoid released as part of the stress response. Thus, it is important to investigate the long-lasting effects of individual and combined adolescent high-dose nicotine and stress exposure. While one study found that adolescent nicotine and the combination of restraint stress and social instability stress in mice resulted in a blunted stress response to restraint stress in adulthood, the abstinence period was only 5 days (Holliday et al. 2019). To date, no studies have assessed the long-lasting effects of adolescent systemic high-dose nicotine and stressor exposure followed by a period of prolonged abstinence. As well as capturing any lingering impact of these exposures, this may also serve as a model for adolescent experimentation with e-cigarettes that provide high nicotine serum levels, followed by a period of cessation before re-initiation in adulthood. Therefore, the present study assessed the long-lasting effect of adolescent nicotine and/or shock experience on adult nicotine IV self-administration, anxiety-like behaviour in a drug-free state, and CORT response to adult nicotine and footshock.
Methods
Subjects
Male Sprague-Dawley rats (Charles River Lab, St. Constant, Quebec, Canada) arrived at the facility on P22 and were pair housed in opaque standard plastic cages. Unless otherwise specified, rats were maintained at ~ 90% of free-feeding body weight (Envigo, Madison, Wisconsin, Rodent Diet, 18% protein) according to the standardized growth chart for this strain provided by Charles River Lab (Envigo, Madison, Wisconsin, Rodent Diet, 18% protein). Water was available ad libitum throughout the experiment. The colony was on a 12:12 light-dark cycle (lights on at 8 a.m.) and maintained at 21 °C. All animal procedures were approved by the Animal Care Committee of the University of Guelph and adhere to the guidelines set forth by the Canadian Council of Animal Care.
Drug preparation
For adolescent preexposure and adult acute testing, nicotine ditartrate dihydrate (Fisher Scientific, Ottawa, ON, CAN) was dissolved in 0.9% saline at a concentration of 1 mg base/ml for subcutaneous SC injections (1 ml/kg) during adolescence (P28-56) (Matta et al. 2007). For adult IV self-administration, the nicotine concentration was 0.03 mg base/kg per 0.04 ml/s IV infusion across the average rat weights (Charntikov et al. 2020). Precision infusion pumps automatically adjusted the duration of the infusion for each rat’s individual weight on a given day to keep dosage consistent. All nicotine used was adjusted to a pH of 7.0–7.2 using NaOH and was prepared fresh weekly.
Surgery
Following adolescent preexposure procedures, a subset of adult rats (P60) was administered carprofen (5 mg/kg), anaesthetized using isoflurane, and implanted with a jugular catheter. The silastic catheter (RJVR-40; SAI, Lake Villa, IL, USA) was secured into the right jugular vein; the other end was threaded subcutaneously over the shoulder and attached to a back-mount cannula (313-000BM-20-5up/spc; PlasticsOne, Anjou, QC, Canada) exiting between the shoulder blades. Tethers in the operant boxes were attached to the rat via the cannula. Rats recovered for 7 days and receive carprofen (5 mg/kg) for 3 days during recovery. Rats were flushed daily with 0.1 ml of flushing solution [heparin (30 U/ml)/baytril (5 mg/ml)/saline (0.9% sterile)] and were single housed from surgery onward. Catheter patency was confirmed by infusing 0.05 ml of a 10% dilution of ketamine/xylazine at the end of the experiment (85:15). Only rats with patent catheters at the end of the experiment were included in the analyses. All surgical drugs were provided by the Ontario Veterinary College.
Apparatus
Adolescent preexposure
For adolescent nicotine and shock preexposure, rats were tested in 8 standard conditioning chambers (Coulbourn Intruments, Allentown, Pennsylvania, USA) enclosed in sound- and light-attenuating cubicles fitted with ventilation fans to reduce external noise. The chamber’s (30.5 × 25.4 × 33 cm; l × w × h) two side walls and ceiling were made of aluminum and the front and back were constructed from clear polycarbonate. An electrified grid floor was programmed to deliver 8 random presentations of 0.5 s 0.8 mA footshock. No other chamber-specific stimuli were present during these sessions.
Adult IV nicotine self-administration
For adult nicotine self-administration, rats were tested in 10 standard conditioning chambers (Med-Associates, Georgia, VT, USA) enclosed in sound- and light-attenuating cubicles fitted with ventilation fans to reduce external noise. The chamber’s (30.5 × 24.1 × 21 cm; l × w × h) two side walls were made of aluminum and the front, back, and ceiling were constructed from clear polycarbonate. Located centrally on the right wall was a recessed liquid dipper with retractable levers on either side, and a house light was located at the top of the opposite aluminum wall. Levers were set such that 147 nN of force was required for a successful lever press to be recorded. A white cue light (2.54 cm dia; 28 V, 100 mA) was centered 7 cm above each lever. Outside of each cubicle, a motor-driven syringe pump set to a rate of 0.04 ml/s (adjusted for weight) and fitted with a syringe infused nicotine via PE50 Tygon tubing attached to a liquid swivel and strung through a metal tether that could be connected to the catheter.
Open-field test
Anxiety-like behaviour was assessed using a novel open field test (OFT) in a drug-free state using two black opaque open-top chambers (100 × 100 × 30 cm; l × w × h). The floor of the maze was subdivided into 16 equivalent squares. The inner 4 squares constituted the center of the maze, and the external 12 the periphery. Total distance travelled (cm) was recorded along with the percent time spent in the center of the OFT, calculated as follows: (time spent in center/time spent in periphery)*100. Behaviour was automatically recorded using Ethovision (Noldus, Netherlands).
Procedure
Adolescent preexposure
Rats received an injection 5 min prior to onset of each daily 20 min session in their assigned conditioning chamber from P28-P56. Saline control rats (SALPRE) received 1 ml/kg saline, SC, every day (28 total injections) with no in-session stimuli. Nicotine-preexposed (NICPRE) rats received alternating injections of 1 mg/kg nicotine or saline, SC (14 nicotine and 14 saline injections), and no in-session stimuli. Footshock stressor–preexposed rats (SHOCKPRE) received saline every day and 8 random presentations of footshock (0.8 mA; 0.5 s) in the operant chamber every other session (14 total sessions with shock). Two groups experienced the combination of both nicotine and shock. Concurrent nicotine and shock rats (NIC+SHOCK) received their nicotine injections and shock exposure co-occurring in the same sessions; intermixed sessions involved saline injections and no in-session stimuli. Thus, this group received a stressor every other day throughout adolescence. Non-concurrent nicotine and shock rats (NIC–SHOCK) received the same number of nicotine injections and shock exposures in the chamber, but on alternating days; these stimuli were never experienced together to assess the effects of the same amount of nicotine and shock as the NIC+SHOCK group, but never at the same time. Thus, this group received a stressor every day throughout adolescence.
IV self-administration
A subset of rats began intravenous self-administration (IVSA) on P70 (SALPRE: n=6; SHOCKPRE: n=7; NICPRE: n=7; NIC+SHOCK: n=8; NIC–SHOCK: n=9). Active and inactive levers were counterbalanced across chambers and group assignment, and there was no lever pretraining. The first phase of self-administration was fixed ratio 1 (FR1). On this schedule, a single press of the active lever resulted in a 0.03 mg/kg infusion of nicotine, and initiated a 20-s time out during which both levers were retracted, the cue light above the active lever was illuminated, and the house light was turned off (Caggiula et al. 2002). Inactive lever presses were not reinforced but were recorded. After 16 1-h sessions on FR1, the schedule was shifted to fixed interval 1 min (FI1). On this schedule, a single active lever press was only reinforced at the termination of a 1-min interval. Infusion and time-out stimuli were identical to FR1. This schedule was selected to remove the constraint of a fixed number of presses per reinforcement in order to allow for more behavioural variability (McClure et al. 2014). After 16 1-h sessions on FI1, the schedule was shifted to progressive ratio (PR) with a gradual increase in the number of presses necessary to deliver each successive infusion (i.e., 1, 2, 3, 4, etc.) for 4 sessions. Finally, rats underwent extinction training with no drug or light stimulus presentations for 6 sessions. The active and inactive levers retracted according to the FR1 schedule.
Open-field test
On P71, a second subset of rats (n=18 per group) was placed on the outer edge of one of two black opaque mazes in a drug-free state and allowed to freely move around the apparatus for 10 min to assess behavioural reactivity to a novel OFT. Maze assignment was counterbalanced across groups.
Blood collection and immunoassay
Stress reactivity was assessed the day after the novel OFT. Blood samples (300 μl) were collected in microvette tubes (Clotting activator, VWR, Radnor, PA) from the saphenous vein immediately before and 15 min after stressor presentation (1.0 mg/kg nicotine, SC, or 4 presentations of 0.8 mA; 0.5 s, footshock in 2 min). Samples (n=9 per adolescent treatment group) were centrifuged (10,000g × 5 min) 1 h after collection, and serum was collected and stored at – 80 °C until processing. A Corticosterone Paramater Enzyme Assay Kit was used (KGE009; R&D Systems; Minneapolis, MN) in duplicate to quantify concentrations of CORT. The concentration of CORT was calculated corresponding to the mean absorbance from the standard curve. Optical density was determined at 450 nm after 10 min using the EL800 Universal Microplate Reader and KC Junior software package (BioTek, Winooski, VT). Intra-assay CV values were below 10% (average was 7.81), and the inter-assay CV was below 15% (13.80 for standard 1 and 7; 14.23 for all standards together).
Statistical analysis
IV self-administration
A mixed-model repeated-measures analysis of variance (ANOVA) was performed for each schedule of reinforcement and assessed the between-subjects factor of Group (5 levels of adolescent preexposure) by the within-subjects factor of session (16; 16; 4; 6 sessions) and included the following concurrently collected within-subjects measures: Total Infusions, Active Lever Presses, Inactive Lever Presses. Lever discrimination within each group was assessed using a repeated-measures ANOVA that compared lever type (2 levels) across session (16; 16; 4; 6 sessions) for each group at each schedule of reinforcement. Significant interactions were followed by post hoc Fisher’s LSD comparisons.
Open-field test
A one-way ANOVA comparing the between subjects effect of Group (5 levels of adolescent preexposure) on total distance travelled (cm) and on percent time spent in the center was used.
Corticosterone
Hormone reactivity measured via CORT levels was assessed using a three-way mixed-factor repeated-measures ANOVA comparing the within-subjects factor Timepoint (Pre- vs. Post-stressor) across the between subjects’ factors of Group (5 levels of adolescent preexposure), and Stressor (Nicotine vs. Shock). Significant interactions were followed by planned post hoc Fisher’s LSD comparisons.
Results
Total infusions
Fixed ratio 1
For the FR1 phase, all rats increased the number of Total Infusions across Sessions, regardless of Group, with NIC+SHOCK rats earning more infusions compared to NICPRE, SHOCKPRE, and SALPRE and no difference between NIC+SHOCK and NIC–SHOCK (Fig. 1A). There was a significant main effect of Session (F15,480=8.876, p<.001, ηp2=.217), a main effect of Group (F4,32=3.345, p=.021, ηp2=.295), and no significant Session by Group interaction (F60,480=44.704, p=.065, ηp2=.141). Post hoc analyses of the main effect of Group revealed that NIC+SHOCK took significantly more infusions compared to NICPRE, SHOCKPRE, and SALPRE. NIC–SHOCK took significantly more total infusions compared to NICPRE and SHOCKPRE, but the difference from SALPRE did not quite reach statistical significance (p=.056). NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Effect of adolescent preexposure on (A) Total infusions (mean ± SEM), (B) Active lever presses (mean ± SEM), and (C) Inactive lever presses (mean ± SEM) during adult nicotine self-administration on FR1, FI1, PR, and EXT schedules of reinforcement. $ indicates a main effect of Group (p<.05), representing a significant difference between one of the combination groups (NIC+SHOCK, NIC–SHOCK) and at least one or all of the control groups (NICPRE, SHOCKPRE, SALPRE). SALPRE n=6; SHOCKPRE n=7; NICPRE n=7; NIC+SHOCK n=8; NIC–SHOCK n=9. Significant between-group post hoc comparisons can be found detailed in the “Inactive lever presses” section
Fixed interval 1
For the FI1 phase, all rats increased Total Infusions across Sessions, regardless of Group (Fig. 1A). There was a significant main effect of Session (F15,480=11.932, p<.001, ηp2=.272), but no main effect of Group (F4,32=2.564, p=.057, ηp2=.243), and no significant Session by Group interaction (F60,480=1.066, p=.352, ηp2=.118).
Progressive ratio
For the PR phase, NIC+SHOCK and NIC–SHOCK rats had a higher breakpoint than NICPRE and SHOCKPRE but not SALPRE (Fig. 1A). There was no main effect of Session (F3,96=0.746, p=.527, ηp2=.023), but there was a main effect of Group (F4,32=3.899, p=.011, ηp2=.328), though no significant Session by Group interaction (F12,96=0.770, p=.680, ηp2=.088). Post hoc analyses of the main effect of Group revealed that NIC+SHOCK rats had a significantly higher breakpoint compared to NICPRE and SHOCKPRE, but not SALPRE. NIC–SHOCK had a significantly higher breakpoint than NICPRE and SHOCKPRE, but not SALPRE. NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Extinction
For the extinction phase, though total infusions decreased across Sessions regardless of Group, NIC+SHOCK rats earned more potential infusions than NICPRE and NIC–SHOCK earned more than both NICPRE and SHOCKPRE, but not SALPRE (Fig. 1A). There was a main effect of Session (F5,160=15.396, p<.001, ηp2=.325), a main effect of Group (F4,32=2.895, p=.038, ηp2=.266), and no Session by Group interaction (F20,160=0.758, p=.760, ηp2=.087). Post hoc analyses of the main effect of Group revealed that NIC+SHOCK maintained higher infusions than NICPRE. NIC–SHOCK was higher than NICPRE and SHOCKPRE, but not SALPRE. NICPRE, SHOCKPRE but not SALPRE controls did not differ from one another.
Summary
During acquisition (FR1), rats with a history of simultaneous combination adolescent nicotine and footshock preexposure (NIC+SHOCK) showed enhanced nicotine consumption compared to nicotine, shock, and saline controls. On FI1 there were no between-group differences. On PR both of the combination nicotine and shock groups showed enhanced nicotine consumption compared to shock or nicotine control rats, but not saline control rats. During extinction, NIC–SHOCK rats earned more potential infusions compared to nicotine, shock, and saline controls.
Active lever presses
Fixed ratio 1
For the FR1 phase, rats increased the number of active lever presses across Session regardless of Group, and NIC+SHOCK rats made more drug-seeking responses compared to NICPRE, SHOCKPRE, and SALPRE (Fig. 1B). There was a significant main effect of Session for Active Lever Presses (F15,480=8.341, p<.001, ηp2=.207), a main effect of Group (F4,32=3.113, p=.028, ηp2=.280), but no significant Session by Group interaction (F60,480=1.301, p=.073, ηp2=.140). Post hoc analyses of the main effect of Group revealed that NIC+SHOCK made significantly more active lever presses than NICPRE, SHOCKPRE, and SALPRE. NIC–SHOCK also had significantly more active lever presses than NICPRE and SHOCKPRE, and the difference from SALPRE did not quite reach statistical significance (p=.053). NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Fixed interval 1
For the FI1 phase, all rats increased active lever presses across Sessions regardless of Group (Fig. 1B). There was a significant main effect of Session (F15,480=6.285, p<.001, ηp2=.164), but no main effect of Group (F4,32=1.529, p=.217, ηp2=.160), and no significant Session by Group interaction (F60,480=1.108, p=.278, ηp2=.122).
Progressive ratio
For the PR phase, NIC+SHOCK and NIC–SHOCK rats made more active lever presses than NICPRE and SHOCKPRE but not SALPRE (Fig. 1B). There was no main effect of Session (F3,96=0.717, p=.544, ηp2=.022), a main effect of Group (F4,32=3.303, p=.023, ηp2=.292), and no significant Session by Group interaction (F12,96=0.806, p=.643, ηp2=.092). Post hoc analyses revealed that NIC+SHOCK made significantly more active lever presses compared to NICPRE and SHOCKPRE but not SALPRE. NIC–SHOCK made more active lever presses compared to NICPRE and SHOCKPRE but not SALPRE. NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Extinction
During the extinction phase, active lever pressing decreased regardless of Group, and NIC–SHOCK rats engaged in more drug-seeking compared to NICPRE, SHOCKPRE, and SALPRE (Fig. 1B). There was a main effect of Session (F5,160=10.548, p<.001, ηp2=.248), a main effect of Group (F4,32=2.872, p=.039, ηp2=.264), and no Session by Group effect (F20,160=1.438, p=.112, ηp2=.152). Post hoc analyses of the main effect of Group revealed NIC–SHOCK rats made significantly more active lever presses compared to NICPRE, SHOCKPRE, and SALPRE. NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Summary
During acquisition (FR1), rats with a history of simultaneous combination adolescent nicotine and footshock preexposure (NIC+SHOCK) had enhanced nicotine-seeking behaviour compared to nicotine, shock, and saline controls. On FI1 there were no between-group differences. On PR, both of the combination nicotine and shock groups showed enhanced nicotine consumption compared to shock or nicotine control rats, but not saline control rats. During extinction, NIC–SHOCK rats made more nicotine-seeking responses compared to nicotine, shock, and saline controls.
Inactive lever presses
Fixed ratio 1
During the FR1 phase, NIC–SHOCK rats made more inactive lever presses compared to all other groups (Fig. 1C). There was a significant main effect of Session for Inactive Lever Presses (F15,480=1.716, p=.045, ηp2=.051), a main effect of Group (F4,32=4.572, p=.005, ηp2=.364), and no significant Session by Group interaction (F60,480=0.772, p=.892, ηp2=.088). Post hoc analyses of the main effect of Group revealed that NIC–SHOCK made significantly more inactive lever presses compared to all other groups (NIC+SHOCK, NICPRE, SHOCKPRE, SALPRE). NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Fixed interval 1
During the FI1 phase, all rats increased inactive lever pressing across Sessions regardless of Group (Fig. 1c). There was a significant main effect of Session (F15,480=1.723, p=.043, ηp2=.051), no main effect of Group (F4,32=0.573, p=.684, ηp2=.067), and no significant Session by Group interaction (F60,480=0.594, p=.993, ηp2=.069).
Progressive ratio
During the PR phase, inactive lever presses did not differ (Fig. 1C). There was no main effect of Session (F3,96=0.062, p=.979, ηp2=.002), no main effect of Group (F4,32=1.560, p=.209, ηp2=.163), and no significant Session by Group interaction (F3,96=0.926, p=.525, ηp2=.104).
Extinction
During the extinction phase, though inactive lever pressing decreased across Sessions regardless of Group, NIC+SHOCK and NIC–SHOCK rats continued making more inactive lever presses compared to NICPRE, SHOCKPRE, and SALPRE (Fig. 1C). There was a main effect of Session (F5,160=3.099, p=.011, ηp2=.088), a main effect of Group (F4,32=2.733, p=.046, ηp2=.255), and no Session by Group effect (F20,160=0.518, p=.956, ηp2=.061). Post hoc analyses of the main effect of Group revealed that NIC+SHOCK and NIC–SHOCK rats made more inactive lever presses compared to NICPRE, SHOCKPRE, and SALPRE controls. NICPRE, SHOCKPRE, and SALPRE controls did not differ from one another.
Summary
During acquisition (FR1), rats with a history of alternating adolescent nicotine and footshock preexposure (NIC–SHOCK) had increased non-reinforced responses compared to all other groups. There were no group differences on FI1 or on PR. During extinction sessions, both adolescent combination nicotine and shock groups showed increased non-reinforced responses compared to nicotine, shock, and saline controls.
Lever discrimination
SALPRE active vs. inactive
SALPRE rats learned to discriminate between active and inactive levers, maintained discrimination across every schedule of reinforcement, and extinguished drug-seeking behaviour when nicotine became unavailable (Fig. 2A). During FR1, there was a main effect of Session (F15,150=4.235, p<.001, ηp2=.298), a main effect of Lever (F1,10= 5.070, p=.048, ηp2=.336), and a significant Session by Lever type interaction (F15,150= 1.785, p=.042, ηp2=.151). Post hoc analyses on the interaction revealed significantly more active lever presses compared to inactive on sessions 7, 9, and 11–16. On FI1, rats continued to discriminate between active and inactive levers. There was a main effect of Session (F15,150= 3.299, p<.001, ηp2=.248), a main effect of Lever (F1,10= 8.186, p=.017, ηp2=.450), but no significant Session by Lever type interaction (F15,150=1.551, p=.094, ηp2=.134). Post hoc analyses of the main effect of Lever revealed significantly more active lever presses compared to inactive. On PR, rats continued to press more on the active than inactive lever. There was no effect of Session (F3,30=0.432, p=.732, ηp2=.041), there was a main effect of Lever type (F1,10=5.063, p=.048, ηp2=.336), but no Session by Lever type interaction (F3,30=0.612, p=.613, ηp2=.058). During extinction, rats gradually decreased active lever pressing to the level of inactive lever pressing. There was a main effect of Session (F5,50=6.745, p<.001, ηp2=.403), no main effect of Lever type (F1,10=4.717, p=.055, ηp2=.321), and a significant Session by Lever type interaction (F5,50=2.891, p=.023, ηp2=.224). Post hoc analyses on the interaction revealed that active lever presses were significantly higher than inactive lever presses on the first 2 extinction sessions.
Lever discrimination, active vs. inactive lever presses (mean ± SEM), across groups and schedules of reinforcement. (A) SALPRE, (B) SHOCKPRE, (C) NICPRE, (D) NIC+SHOCK, (E) NIC–SHOCK. $ indicates a main effect of Lever type (p<.05). * indicates significant difference between active and inactive lever on a particular session (p<.05). SALPRE n=6; SHOCKPRE n=7; NICPRE n=7; NIC+SHOCK n=8; NIC–SHOCK n=9. Significant between-group post hoc comparisons can be found detailed in the “Lever discrimination” section
SHOCKPRE active vs. inactive
SHOCKPRE rats did not significantly discriminate between active and inactive levers across training except on the first 2 extinction sessions when drug became unavailable (Fig. 2B). During FR1, there was no effect of Session (F15,180=0.980, p=.478, ηp2=.076), no effect of Lever (F1,12=1.838, p=.200, ηp2=.133), and no Session by Lever interaction (F15,180=0.938, p=.524, ηp2=.072). On FI1, rats increased pressing regardless of lever. There was a main effect of Session (F15,180= 1.296, p=.208, ηp2=.098), but no effect of Lever (F1,12=4.374, p=.058, ηp2=.267), or significant Session by Lever interaction (F15,180=0.510, p=.933, ηp2=.041). Similarly, on PR, rats increased responding over sessions regardless of lever. There was a main effect of Session (F3,36= 3.895, p=.017, ηp2=.245), but no effect of Lever (F1,12=4.689, p=.051, ηp2=.281), or Session by Group interaction (F3,36=2.368, p=.087, ηp2=.165). During extinction, rats demonstrated an ability to discriminate between levers that declined across sessions. There was a main effect of Session (F5,60=3.190, p=.013, ηp2=.210), a main effect of Lever type (F1,12=6.338, p=.027, ηp2=.346), and a significant Session by Lever type interaction (F5,60=2.960, p=.019, ηp2=.198). Post hoc analyses on the interaction revealed that active lever presses were significantly higher than inactive on the first 2 sessions.
NICPRE active vs. inactive
NICPRE rats learned to discriminate between active and inactive levers, maintained discrimination when an interval schedule was implemented, did not show enhanced motivation to obtain nicotine on PR, and did not extinguish drug-seeking when drug was made unavailable (Fig. 2C). During FR1, there was a main effect of Session (F15,180=5.451, p<.001, ηp2=.312), no main effect of Lever (F1,12=2.574, p=.135, ηp2=.177), and a significant Session by Lever interaction (F15,180= 1.843, p=.032, ηp2=.133). Post hoc analyses on the interaction revealed significantly greater active vs. inactive lever presses on sessions 11 and 13–16. During FI1, there was a main effect of Session (F15,180=2.419, p=.003, ηp2=.168), no main effect of Lever (F1,12= 4.263, p=.061, ηp2=.262), and a significant Session by Lever type interaction (F15,180= 2.078, p=.013, ηp2=.148). Post hoc analyses on the interaction revealed that active lever presses were significantly higher than inactive on all sessions. During PR, rats did not significantly discriminate between active and inactive levers. There was no main effect of Session (F3,36=.873, p=.464, ηp2=.068), no main effect of Lever (F1,12=3.032, p=.107, ηp2=.202), and no significant Session by Lever interaction (F3,36= 0.790, p=.507, ηp2=.062). During extinction, rats made significantly more active lever presses than inactive. There was no effect of Session (F5,60=1.339, p=.260, ηp2=.100), a main effect of Lever (F1,12=5.614, p=.035, ηp2=.319), and no significant Session by Lever interaction (F5,60=0.633, p=.675, ηp2=.050).
NIC+SHOCK active vs. inactive
NIC+SHOCK rats learned to discriminate on the very first session, maintained a significant discrimination for the entirety of the experiment, and did not extinguish drug-seeking when nicotine was made unavailable (Fig. 2D). During FR1, there was a main effect of Session (F15,210=2.543, p=.002, ηp2=.154), a main effect of Lever (F1,14=12.220, p=.004, ηp2=.466), and no significant Session by Lever interaction (F15,210=1.577, p=.082, ηp2=.101). Active lever presses were significantly higher than inactive lever presses. During FI1, rats maintained a significant discrimination between active and inactive levers. There was a main effect of Session (F15,210=1.570, p=.084, ηp2=.101), a main effect of Lever (F1,14= 41.273, p<.001, ηp2=.747), and no significant Session by Lever interaction (F15,210= 1.284, p=.214, ηp2=.084). Active lever pressing was significantly higher than inactive lever pressing. During PR, rats again maintained higher active than inactive lever pressing. There was no main effect of Session (F3,42=1.254, p=.302, ηp2=.082), a main effect of Lever type (F1,14=29.923, p<.001, ηp2=.681), and no significant Session by Lever type interaction (F3,42=0.296, p=.828, ηp2=.021). Active lever presses are significantly higher than inactive. During extinction, rats significantly discriminated between active and inactive levers and did not extinguish this drug-seeking behaviour. There was a main effect of Session (F5,70=4.085, p=.003, ηp2=.226), a main effect of Lever (F1,14=10.753, p=.005, ηp2=.434), and no significant Session by Lever interaction (F5,70=1.619, p=166, ηp2=.104).
NIC–SHOCK active vs. inactive
NIC–SHOCK rats did not learn to significantly discriminate between active and inactive levers during FR1, significantly discriminated when the interval schedule was implemented (FI1) and during PR, and successfully extinguished drug-seeking when nicotine became unavailable (Fig. 2E). During FR1, rats did not significantly discriminate between active and inactive levers. There was no effect of Session (F15,240=1.378, p=.158, ηp2=.079), Lever (F1,16=0.787, p=.388, ηp2=.047), or Session by Lever interaction (F15,240=0.764, p=.716, ηp2=.046). On FI1, rats significantly discriminated between active and inactive levers and increased responding over sessions. There was a main effect of Session (F15, 240= 2.652, p=.001, ηp2=.142), Lever (F1,16= 7.042, p=.017, ηp2=.306), and a significant Session by Lever interaction (F15,240=2.595, p=.001, ηp2=.140). Post hoc analyses on the interaction revealed that active lever pressing was significantly higher than inactive on all sessions. On PR, rats significantly discriminated between active and inactive levers. There was no effect of Session (F3,48=0.451, p=.718, ηp2=.027), a main effect of Lever (F1,16=9.257, p=.008, ηp2=.367), and no significant Session by Lever interaction (F3,48=0.353, p=.787, ηp2=.022). During extinction, rats gradually decreased active lever pressing to the level of inactive across sessions. There was a main effect of Session (F5,80=5.895, p<.001, ηp2=.269), Lever (F1,16=8.072, p=.012, ηp2=.335), and a significant Session by Lever interaction (F5,80=3.858, p=.003, ηp2=.194). Post hoc analyses on the interaction revealed that active lever presses were significantly higher than inactive on the first 2 sessions.
Summary
During acquisition (FR1), all groups learned to significantly discriminate between active and inactive levers except for SHOCKPRE and NIC–SHOCK. During FI1, all groups maintain significant discrimination between active and inactive levers, except SHOCKPRE. All groups also maintain discrimination on PR except SHOCKPRE. All groups learn to extinguish their drug-seeking responses across 7 sessions, except NICPRE and NIC+SHOCK rats that persisted in drug-seeking to a degree that still produced significant differences between active and inactive levers. SHOCKPRE rats significantly discriminated on the first two extinction sessions for the first time.
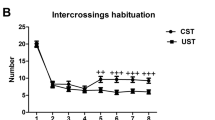
Open-field test
Total distance travelled
Adolescent exposure groups did not differ on novelty-induced locomotion in a drug-free state in adulthood (Fig. 3A). There were no significant differences in total distance travelled (cm) (F4,91=2.315, p=.064, ηp2=.096).
Baseline anxiety-like behaviour measured by (A) distance travelled (cm) (mean ± SEM), and (B) percent time spent in the center (mean ± SEM) of a novel OFT in adulthood, and (C) baseline CORT levels (mean ± SEM). There were no differences across for groups for any of these measures. SALPRE n=18; SHOCKPRE n=20; NICPRE n=18; NIC+SHOCK n=18; NIC–SHOCK n=18
Percent time spent in center
Adolescent exposure groups did not differ on baseline anxiety-like behaviour in a drug-free state (Fig. 3B). There were no significant differences in the percent time spent in the center of the OFT (F4,91=0.289, p=.884, ηp2=.013).
Summary
There were no differences among adolescent preexposure groups in anxiety-like behaviour.
Corticosterone quantification
Baseline CORT
Adolescent nicotine, shock, or the combination of nicotine and shock exposure did not alter baseline CORT levels in adulthood (Fig. 3C). All rats in the experiment did not differ on baseline CORT levels across adolescent exposure group (F9,82=0.978, p=.465, ηp2=.097). Further, rats that received nicotine as their stressor in adulthood did not differ from rats that received shock as their stressor in adulthood on their baseline CORT levels (F1,90=0.523, p=.471, ηp2=.006).
CORT levels in response to adult nicotine and shock across groups
There was no effect of adolescent preexposure (Group) on stress response to nicotine or shock; however, nicotine increased CORT release significantly more than shock (Fig. 4). There was a main effect of Timepoint (F1,82=272.491, p<.001, ηp2=.769), and a main effect of Stressor (F1,82=22.995, p<.001, ηp2=.219), but no main effect of Group (F4,82=1.024, p=.400, ηp2= .048). There was a significant Timepoint by Stressor interaction (F1,82 =93.524, p<.001, ηp2= .533), but no significant Timepoint by Group interaction (F4,82=1.074, p=.375, ηp2=.050). Post hoc analyses reveal that though both nicotine and footshock enhanced CORT levels, nicotine increased CORT levels significantly more than footshock.
Adult pre- and post-stressor CORT response (mean ± SEM) to nicotine or footshock stress for each adolescent preexposure group. $ indicates a significant effect of Timepoint (p<.05). # indicates a main effect of Stressor type (p<.05). SALPRE(NIC) n=9; SALPRE(SHOCK) n=9; SHOCKPRE(NIC) n=10; SHOCKPRE(SHOCK) n=10; NICPRE(NIC) n=9; NICPRE(SHOCK) n=9; NIC+SHOCK(NIC) n=9; NIC+SHOCK(SHOCK) n=9; NIC–SHOCK(NIC) n=9; NIC–SHOCK(SHOCK) n=8
Summary
Adult rats preexposed to adolescent nicotine and/or footshock exposure did not differ on baseline CORT levels or the magnitude of CORT response to nicotine or footshock stress. Both nicotine (1 mg/kg/SC) and footshock (2 min session; 4 × 0.5 s;0.8 mA) significantly increased CORT levels in all groups 15 min following stress exposure, though nicotine increased CORT levels significantly more than footshock stress.
Discussion
The synergistic effects of adolescent nicotine and footshock exposure enhanced acquisition of spontaneous adult nicotine IVSA and drug-seeking relative to either of these adolescent experiences independently. This effect occurred without a concomitant enhancement of adult anxiety-like behaviour in a drug-free state or altered CORT responsivity to nicotine or footshock exposure. Receiving alternating sessions of exposure to high-dose nicotine or footshock alone throughout adolescence did not significantly alter adult nicotine IVSA, anxiety-like behaviour, or CORT responsivity.
To summarize our discrimination findings, during FR1, saline-preexposed (SALPRE) and nicotine-preexposed (NICPRE) control rats learned over time to discriminate between active and inactive levers. In the first sessions, active and inactive lever pressing did not differ for these rats, but as the FR1 sessions progressed, they learned to make significantly more active than inactive lever presses. Rats receiving concurrent nicotine and shock (NIC+SHOCK) also significantly discriminated between active and inactive levers; however, this discrimination was present from the very first session. This could be due to an increased perceptibility of nicotine in these rats, or enhanced learning for this task. Though rats with alternating nicotine and shock sessions (NIC–SHOCK) took more infusions during FR1 compared to shock and nicotine controls, they did not significantly discriminate between the two levers. This could be due to overall increased non-specific behavioural excitability evidenced by enhanced non-reinforced inactive lever pressing compared to all groups, which has been previously reported with nicotine IVSA (Cole et al. 2019; Renda et al. 2020). The pharmacological stressor yohimbine has also been shown to similarly enhance the reinforcing properties of nicotine while also increasing inactive lever pressing (Li et al. 2014); thus, it is also possible that the increase in inactive lever pressing seen in NIC–SHOCK rats during FR1 was stress-induced. Finally, the shock-preexposed (SHOCKPRE) control group did not learn to significantly discriminate between active and inactive levers. When a 1-min delay was implemented during FI1, all rats successfully learned to discriminate between active and inactive levers except for SHOCKPRE rats again. When the schedule was shifted to PR, which requires more responses for each successive infusion, SHOCKPRE (and NICPRE) rats still failed to discriminate levers. Finally, when nicotine was made unavailable during extinction, SHOCKPRE rats do significantly discriminate on the first two sessions and then successfully extinguish their drug-seeking behaviour—evidence that SHOCKPRE rats may have learned the contingency throughout self-administration and that non-reinforcement caused an extinction burst (Pushparaj et al. 2012). It may be that the SHOCKPRE rats had increased sensitivity to the reinforcing effects of nicotine and thus required less nicotine to achieve optimal nicotine titration, resulting in the lack of difference between active and inactive lever pressing. It is also possible that these rats had increased sensitivity to the aversive effects of nicotine and were therefore less likely to self-administer; however, our enthusiasm for that explanation is diminished by their increased seeking response during extinction, showing they were motivated for the drug. SALPRE and NIC–SHOCK rats also show a similar pattern of extinction; they discriminate on the first two sessions, and then extinguish their drug-seeking. Interestingly, both NICPRE and NIC+SHOCK rats did not technically extinguish this drug-seeking. In contrast to the other three groups, these rats continued to make significantly more active than inactive lever presses throughout all extinction sessions, meaning that more extinction training would have been required to eventually reduce their active lever pressing.
During adult spontaneous acquisition of nicotine IVSA on an FR1 schedule of reinforcement, rats exposed to concurrent nicotine and shock every other day (NIC+SHOCK) showed enhanced adult nicotine IVSA and increased inactive lever pressing during extinction compared to shock-preexposed (SHOCKPRE), nicotine-preexposed (NICPRE), and saline control rats (SALPRE). Interestingly, rats with the same amount of nicotine and footshock in adolescence, but never simultaneously (NIC–SHOCK), also showed this enhancement of nicotine self-administration and inactive lever pressing during extinction compared to shock and nicotine controls—evidence that these two experiences did not have to occur simultaneously in order to exert their synergistic effects.
Rats that received nicotine and footshock never co-occurring (NIC–SHOCK), and thus received a stressor every day throughout adolescence, also showed increased inactive lever pressing during acquisition (FR1) compared to all groups and enhanced drug-seeking during extinction when nicotine became unavailable compared to NICPRE, SHOCKPRE, and SALPRE controls. As mentioned earlier, this increase in inactive lever pressing during FR1 and extinction may be indicative of non-specific behavioural activation or impaired impulse control (Cole et al. 2019; Renda et al. 2020). Similarly, male and female adolescent (P33) rats showed an increase in inactive lever pressing on a PR schedule when the pharmacological stressor yohimbine was administered (0, 0.3, 0.6 mg/kg yohimbine, IP) (Li et al. 2014); thus, these increases in inactive lever pressing observed when nicotine became unavailable during extinction may be stress-induced. This non-specific behavioural activation was specific to the IVSA environment where drug and drug-paired cues were present but was not evident in the novel OFT where drug and drug-paired cues were never encountered.
The key difference between the two experimental groups is that NIC+SHOCK rats received a stressor every other day, whereas NIC–SHOCK rats experienced a stressor daily—these differences in stressor exposure patterns may underlie the greater behavioural activation and persistent drug-seeking during extinction seen in the NIC–SHOCK compared to NIC+SHOCK rats. Alternatively, nicotine has been shown to have antinociceptive properties (Tripathi et al. 1982), and stressors have been shown to potentiate the rewarding effects of nicotine in adolescence (Pentkowski et al. 2011; Li et al. 2014; Zou et al. 2014). Taken together, it is possible that for the NIC+SHOCK group, concurrent nicotine and shock exposure resulted in nicotine exerting an antinociceptive effect on the shock stressor, while the shock stressor is simultaneously enhancing the rewarding value of the nicotine. This unique experience in adolescence resulted in increased acquisition of nicotine self-administration, increased motivation to obtain nicotine compared to individual nicotine or shock preexposure, without the additional increase in inactive lever presses seen from NIC–SHOCK rats during FR1 or drug-seeking during extinction.
Across FR1 training, responding in control rats approached levels of the combined nicotine and shock–preexposed rats, and there were no group differences once the 1-min delay was implemented between each possible nicotine infusion (FI1). All groups continued to increase nicotine consumption across those sessions. Importantly, this finding indicates that nicotine and footshock stress exposure in adolescence may predispose individuals to acquire self-administration faster, but not necessarily to take more nicotine in the long-term. However, during PR, both of the nicotine and shock combination groups worked harder to obtain nicotine compared to nicotine- or shock-preexposed rats, and when drug availability stopped during extinction, combination alternating adolescent nicotine and shock–preexposed rats (NIC–SHOCK) persisted in drug-seek to a greater extent than nicotine, shock, and saline controls, indicating greater motivation for the drug despite having similar intake levels during the previous phase. Furthermore, both combination adolescent nicotine and shock groups also showed greater inactive lever pressing compared to controls during extinction, and this could also be evidence of extinction-evoked increases in response variability, and indicative of greater levels of extinction-induced frustration (Amsel 1958; Dudley and Papini 1997; Neuringer et al. 2001; Pushparaj et al. 2012).
Of note, none of the three control groups, nicotine preexposure (NICPRE), shock preexposure (SHOCKPRE), or no-nicotine/no-shock (SALPRE) ever differed from each other on any of the dependent measures assessed herein. This finding contrasts with some existing literature showing that adolescent nicotine exposure increases adult nicotine self-administration (Adriani et al. 2003; Cole et al. 2019; Natividad et al. 2013). However, species (e.g., Cole et al. 2019) and strain (e.g., Natividad et al. 2013), as well as procedural differences in studies, may account for differences in findings. Rats in the current study received 1 mg/kg SC nicotine or shock every other day throughout adolescence, whereas studies that found increased nicotine IVSA used 0.4 mg/kg, IP, once per day for 10 days from P34-43 (Adriani et al. 2003); 4.7 mg/kg/day for 14 days via mini osmotic pump beginning on P32-34 (Natividad et al. 2013); and 3 mg/kg/day for 2 weeks (P33-35) or 6.3 mg/kg/day (P61-63) for 2 weeks via osmotic minipumps (Cole et al. 2019). Therefore, the differences are a higher bolus dosage periodically throughout development in our study that may be more reflective of human teenage nicotine consumption compared to previous literature. Furthermore, a recent study from our lab exposed rats starting at the same age to the same number of injections, same route of administration, and same dose as this current study but for 14 consecutive days during early adolescence (P28-41), instead of every other day, and found a significant increase in spontaneous adult nicotine IVSA under a FI1 schedule of reinforcement at 0.02 mg/kg/infusion instead of the current 0.03 mg/kg/infusion (Renda et al. 2020). Those training conditions were such that the saline-preexposed rats did not develop reliable self-administration. It is possible that daily nicotine exposure, as opposed to intermittent or alternating exposure, may have more profound of an effect during a critical developmental stage. Such a finding also coincides with the osmotic minipump literature described previously. The age differences in adolescent nicotine exposure in the current study compared to our previous work may also contribute to the differential findings. In stark contrast however, one study reported a reduction in adult nicotine self-administration following adolescent nicotine exposure of 3.2 mg/kg/day nicotine from P28-34 compared to drug-naïve rats (de la Peña et al. 2014); however, this was the only study that lever trained rats for pellets prior to IVSA, and the reinforcer switch may have been more disruptive to the nicotine-preexposed rats. Given that control rats in the current study (SALPRE) can demonstrate spontaneous adult nicotine IVSA at 0.03 mg/kg/infusion without pretraining, it may be preferential to avoid any confounding effects of training and non-drug reward. The present study also only assessed the long-lasting impact of one dose of nicotine in adolescence; thus, it cannot be determined whether these behavioural effects observed were due to shifts in the dose response, or a shift in the maximum response. Similarly, the present study also only assessed the effect of short (0.5-s duration) footshock presentations of a particular mA (0.8 mA). Assessing the effect of multiple nicotine doses as well as footshock magnitudes would help further clarify factors driving these behavioural responses in our particular species and strain of investigation.
Interestingly, our study found that while rats with nicotine and shock experience in adolescence show greater nicotine self-administration as adults, they did not show greater anxiety-like behaviour in the open field. This finding is in contrast to some previous studies using the OFT. Decreased time spent in the center of a novel OFT has been shown 1 month after adolescent (P28-42) nicotine exposure (2 mg/kg/day via osmotic minipump for 15 days) (Smith et al. 2006). Decreased exploratory activity in novel OFT has also been shown 2–3 weeks after adolescent (P31-36) nicotine exposure (5 days of 5.0 mg/kg/day via Nicoderm CQ patches) (Slawecki 2003). Additionally, increased novelty-induced locomotion in a place conditioning chamber is observed 5 weeks after adolescent (P34-43) nicotine exposure (0.4 mg/kg, IP, 10 days daily) (Adriani et al. 2006). Similar to how nicotine or shock preexposure alone in the present study was not able to enhance adult nicotine IVSA, we observed no change in anxiety-like behaviour in adulthood. However, those previous studies utilized nicotine preexposure methods that resulted in consistent nicotine exposure for days at a time, whereas the present study administered nicotine in a high-dose bolus once every other day, a pattern that may be more likely to be experienced by human adolescents. It is conceivable that this difference in preexposure patterns may underlie differences in adult novelty-induced locomotion and anxiety-like behaviour.
The synergistic effects of experiencing nicotine and footshock exposure in adolescence also altered adult IVSA behaviour in nicotine intake and seeking without altering adult stress responsivity to nicotine or footshock. CORT concentrations across adolescent preexposure groups did not differ for nicotine or shock exposure in adulthood, though both evoked increased CORT post-stressor. The interaction between adolescent stress (restraint stress and social instability stress) and nicotine exposure has been shown to blunt adult CORT response to restraint stress in adulthood (Holliday et al. 2019); however, this is a social stressor in combination with a high consistent dose of nicotine—these differences in exposure type may underlie differences in long-term effects. Evidence for cross-sensitization to shock or nicotine following the opposite preexposure exists (Cam et al. 1984); however, their preexposure period was twice as long with a different dose of nicotine.
We show here that intermittent adolescent nicotine and footshock stress exposure function synergistically to enhance vulnerability to adult nicotine consumption and nicotine-seeking during unavailability without altering baseline anxiety or stress responsivity. Such a finding is relevant for understanding the long-term impact of such adolescent experiences. The current rates of teenage nicotine vaping are extremely high and continue to rise yearly with each set of updated statistics. In 2019, about 12% of 12th graders self-reported vaping nicotine daily, with approximately a quarter of them reporting use in the last month (Miech et al. 2019). Nicotine vaping in 8th graders in 2019 was almost as high as the prevalence of nicotine vaping in 12th graders in 2017 (Miech et al. 2019). The increase in nicotine vaping from 2017 to 2018 was the largest 1-year jump ever tracked in the 45-year history of the ‘Monitoring the Future’ survey for any substance in 8th, 10th, and 12th graders (Miech et al. 2019). The brand name product JUUL is currently the most popular nicotine vaping device in adolescents (Krishnan-Sarin et al. 2019), produces high plasma nicotine content—almost threefold the levels of a cigarette (P. Rao, Liu, & Springer, 2020)—and is associated with higher socioeconomic status (Krishnan-Sarin et al. 2019) compared to low socioeconomic status previously associated with increased prevalence of tobacco use (Hiscock et al. 2012). Furthermore, adolescents will inevitably face stress or perceived stress. Given that adolescent nicotine and stress exposure in the current study was able to increase adult nicotine reinforcement more than either of these experiences alone, and there are high rates of adolescent vaping and adolescent stress (Leventhal et al. 2017), it is possible that there will be a surge in adult nicotine use in the next decade if smoking cessation therapies and prevention methods do not adapt to novel smoking patterns and exposure types. It is well known that adolescent initiation of nicotine use does increase the risk of adult use and dependence (Chen and Millar 1998; Cullen et al. 2018; Sharapova et al. 2018); however, the range and number of adolescents that are using these products today differ from what is known about the demographic of cigarette smoking. An emphasis on improving prevention methods, understanding the interaction between nicotine and stress in adolescence, and advancing smoking cessation therapies, perhaps by incorporating explicit stress-reduction techniques, may help avoid a new rise in adult nicotine use and the negative health outcomes that accompany this use.
References
Adriani W, Spijker S, Deroche-Gamonet V, Laviola G, le Moal M, Smit AB, Piazza PV (2003) Evidence for enhanced neurobehavioral vulnerability to nicotine during periadolescence in rats. J Neurosci 23:4712–4716. https://doi.org/10.1523/jneurosci.23-11-04712.2003
Adriani W, Deroche-Gamonet V, Le Moal M et al (2006) Preexposure during or following adolescence differently affects nicotine-rewarding properties in adult rats. Psychopharmacology 184:382–390. https://doi.org/10.1007/s00213-005-0125-1
Ahsan HM, Chrislean Jun Botanas HJK, de la Peña JBI , et al. (2014) Conditioned place preference and self-administration induced by nicotine in adolescent and adult rats. doi:https://doi.org/10.4062/biomolther.2014.056
Amsel A (1958) The role of frustrative nonreward in noncontinuous reward situations. Psychol Bull 55:102–119. https://doi.org/10.1037/h0043125
Anderson NB, Belar CD, Breckler SJ, et al (2014) Stress in America: are teens adopting adults’ stress habits ?
Brielmaier J, Mcdonald CG, Smith RF (2011) Effects of acute stress on acquisition of nicotine conditioned place preference in adolescent rats: a role for corticotropin-releasing factor 1 receptors. Psychopharmacology 219:73–82. https://doi.org/10.1007/s00213-011-2378-1
Bunnell RE, Agaku IT, Arrazola RA, Apelberg BJ, Caraballo RS, Corey CG, Coleman BN, Dube SR, King BA (2015) Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011-2013. Nicotine Tob Res 17:228–235. https://doi.org/10.1093/ntr/ntu166
Caggiula AR, Donny EC, White AR, Chaudhri N, Booth S, Gharib M, Hoffman A, Perkins K, Sved A (2002) Environmental stimuli promote the acquisition of nicotine self-administration in rats. Psychopharmacology 163:230–237. https://doi.org/10.1007/s00213-002-1156-5
Cam GR, Basseti JR, Bassett JR (1984) Effect of prolonged exposure to nicotine and stress on the pituitary-adrenocortical response; the possibility of cross-adaptation
Chaffee BW, Watkins SL, Glantz SA (2018) Electronic cigarette use and progression from experimentation to established smoking. Pediatrics 141:e20173594. https://doi.org/10.1542/peds.2017-3594
Charntikov S, Pittenger ST, Swalve N, Barrett ST, Bevins RA (2020) Conditioned enhancement of the nicotine reinforcer. Exp Clin Psychopharmacol. https://doi.org/10.1037/pha0000370
Chen J, Millar WJ (1998) Age of smoking initiation: implications for quitting. Health Rep 9:39
Cole RD, Wolsh C, Zimmerman M, Harrington E, Gould TJ, Parikh V (2019) Adolescent and adult nicotine exposure differentially impacts oral nicotine and oral saccharin self-administration in mice. Behav Brain Res 359:836–844. https://doi.org/10.1016/j.bbr.2018.07.019
Cullen KA, Ambrose BK, Gentzke AS, et al (2018) Morbidity and mortality weekly report notes from the field use of electronic cigarettes and any tobacco product among middle and high school students-United States, 2011-2018. https://doi.org/10.15585/mmwr.mm6722a3
de la Peña JB, Ahsan HM, Botanas CJ, Sohn A, Yu GY, Cheong JH (2014) Adolescent nicotine or cigarette smoke exposure changes subsequent response to nicotine conditioned place preference and self-administration. Behav Brain Res 272:156–164. https://doi.org/10.1016/j.bbr.2014.06.044
Dudley RT, Papini MR (1997) Amsel’s frustration effect: a Pavlovian replication with control for frequency and distribution of rewards. Physiol Behav 61:627–629. https://doi.org/10.1016/S0031-9384(96)00498-2
Frie JA, Underhill J, Zhao B, et al (2020) OpenVape: an open-source e-cigarette vapour exposure device for rodents. eneuro ENEURO.0279-20.2020. doi:https://doi.org/10.1523/ENEURO.0279-20.2020
Gilbert DG, Robinson JH, Chamberlin CL, Spielberger CD (1989) Effects of smoking/nicotine on anxiety, heart rate, and lateralization of EEG during a stressful movie. Psychophysiology 26:311–320. https://doi.org/10.1111/j.1469-8986.1989.tb01924.x
Goniewicz ML, Boykan R, Messina CR, Eliscu A, Tolentino J (2019) High exposure to nicotine among adolescents who use Juul and other vape pod systems (pods’). Tob Control 28:676–677
Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M (2012) Socioeconomic status and smoking: a review. Ann N Y Acad Sci 1248:107–123. https://doi.org/10.1111/j.1749-6632.2011.06202.x
Holliday ED, Logue SF, Oliver C, Bangasser DA, Gould TJ (2019) Stress and nicotine during adolescence disrupts adult hippocampal-dependent learning and alters stress reactivity. Addict Biol 25:e12769. https://doi.org/10.1111/adb.12769
Iñiguez SD, Warren BL, Parise EM, Alcantara LF, Schuh B, Maffeo ML, Manojlovic Z, Bolaños-Guzmán CA (2009) Nicotine exposure during adolescence induces a depression-like state in adulthood. Neuropsychopharmacology 34:1609–1624. https://doi.org/10.1038/npp.2008.220
Kota D, Martin BR, Robinson SE, Damaj MI (2007) Nicotine dependence and reward differ between adolescent and adult male mice. J Pharmacol Exp Ther 322:399–407. https://doi.org/10.1124/jpet.107.121616
Krishnan-Sarin S, Jackson A, Morean M, Kong G, Bold KW, Camenga DR, Cavallo DA, Simon P, Wu R (2019) E-cigarette devices used by high-school youth. Drug Alcohol Depend 194:395–400. https://doi.org/10.1016/j.drugalcdep.2018.10.022
Laje RP, Berman JA, Glassman AH (2001) Depression and nicotine: preclinical and clinical evidence for common mechanisms. Curr Psychiatry Rep 3:470–474
Le Foll B, Goldberg SR (2005) Nicotine induces conditioned place preferences over a large range of doses in rats. Psychopharmacology 178:481–492. https://doi.org/10.1007/s00213-004-2021-5
Leventhal AM, Urman R, Barrington-Trimis JL, Goldenson NI, Gallegos K, Chou CP, Wang K, Berhane K, Cruz TB, Pentz MA, Unger J, McConnell RS (2017) Perceived stress and poly-tobacco product use across adolescence: Patterns of association and gender differences. J Psychiatr Res 94:172–179. https://doi.org/10.1016/j.jpsychires.2017.07.010
Levin ED, Rezvani AH, Montoya D, Rose JE, Swartzwelder HS (2003) Adolescent-onset nicotine self-administration modeled in female rats. Psychopharmacology 169:141–149. https://doi.org/10.1007/s00213-003-1486-y
Levin ED, Lawrence SS, Petro A, Horton K, Rezvani AH, Seidler FJ, Slotkin TA (2007) Adolescent vs. adult-onset nicotine self-administration in male rats: Duration of effect and differential nicotinic receptor correlates. Neurotoxicol Teratol 29:458–465. https://doi.org/10.1016/J.NTT.2007.02.002
Li S, Zou S, Coen K, Funk D, Shram MJ, Lê AD (2014) Sex differences in yohimbine-induced increases in the reinforcing efficacy of nicotine in adolescent rats. Addict Biol 19:156–164. https://doi.org/10.1111/j.1369-1600.2012.00473.x
Loukas A, Marti CN, Cooper M, Pasch KE, Perry CL (2018) Exclusive e-cigarette use predicts cigarette initiation among college students. Addict Behav 76:343–347. https://doi.org/10.1016/J.ADDBEH.2017.08.023
Matta SG, Balfour DJ, Benowitz NL, Boyd RT, Buccafusco JJ, Caggiula AR, Craig CR, Collins AC, Damaj MI, Donny EC, Gardiner PS, Grady SR, Heberlein U, Leonard SS, Levin ED, Lukas RJ, Markou A, Marks MJ, McCallum SE, Parameswaran N, Perkins KA, Picciotto MR, Quik M, Rose JE, Rothenfluh A, Schafer WR, Stolerman IP, Tyndale RF, Wehner JM, Zirger JM (2007) Guidelines on nicotine dose selection for in vivo research. Psychopharmacology 190:269–319. https://doi.org/10.1007/s00213-006-0441-0
McClure J, Podos J, Richardson HN (2014) Isolating the delay component of impulsive choice in adolescent rats. Front Integr Neurosci 8:3. https://doi.org/10.3389/fnint.2014.00003
Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME (2019) Trends in adolescent vaping, 2017–2019. N Engl J Med 381:1490–1491. https://doi.org/10.1056/NEJMc1910739
Morisette SB, Tull MT, Bulliver SB et al (2007) Anxiety, anxiety disorders, tobacco use, and nicotine: a critical review of interrelationships. Psychol Bull 133:245–272
Natividad LA, Torres OV, Friedman TC, O’Dell LE (2013) Adolescence is a period of development characterized by short- and long-term vulnerability to the rewarding effects of nicotine and reduced sensitivity to the anorectic effects of this drug. Behav Brain Res 257:275–285. https://doi.org/10.1016/j.bbr.2013.10.003
Nesil T, Kanit L, Collins AC, Pogun S (2011) Individual differences in oral nicotine intake in rats. Neuropharmacology 61:189–201. https://doi.org/10.1016/j.neuropharm.2011.03.027
Neuringer A, Kornell N, Olufs M (2001) Stability and variability in extinction. J Exp Psychol Anim Behav Process 27:79–94. https://doi.org/10.1037/0097-7403.27.1.79
O’Dell LE, Torres OV, Natividad LA, Tejeda HA (2007) Adolescent nicotine exposure produces less affective measures of withdrawal relative to adult nicotine exposure in male rats. Neurotoxicol Teratol 29:17–22. https://doi.org/10.1016/J.NTT.2006.11.003
Pentkowski NS, Painter MR, Thiel KJ, Peartree NA, Cheung THC, Deviche P, Adams M, Alba J, Neisewander JL (2011) Nicotine-induced plasma corticosterone is attenuated by social interactions in male and female adolescent rats. Pharmacol Biochem Behav 100:1–7. https://doi.org/10.1016/j.pbb.2011.07.005
Porcu P, Sogliano C, Cinus M, Purdy RH, Biggio G, Concas A (2003) Nicotine-induced changes in cerebrocortical neuroactive steroids and plasma corticosterone concentrations in the rat. Pharmacol Biochem Behav 74:683–690. https://doi.org/10.1016/S0091-3057(02)01065-1
Primack BA, Shensa A, Sidani JE et al (2018) Initiation of traditional cigarette smoking after electronic cigarette use among tobacco-naïve US young adults. Am J Med 131:443.e1–443.e9. https://doi.org/10.1016/J.AMJMED.2017.11.005
Pushparaj A, Pryslawsky Y, Forget B, Yan Y, le Foll B (2012) Extinction bursts in rats trained to self-administer nicotine or food in 1-h daily sessions. Am J Transl Res 4:422–431
Rao P, Liu J, Springer ML (2020) JUUL and combusted cigarettes comparably impair endothelial function. Tob Regul Sci 6:30–37. https://doi.org/10.18001/TRS.6.1.4
Reilly SM, Bitzer ZT, Goel R, Trushin N, Richie JP Jr (2019) Free radical, carbonyl, and nicotine levels produced by Juul electronic cigarettes. Nicotine Tob Res 21:1274–1278. https://doi.org/10.1093/NTR/NTY221
Renda B, Andrade AK, Frie JA, Sgarbossa CL, Murray JE, Khokhar JY (2020) High-dose adolescent nicotine exposure permits spontaneous nicotine self-administration in adult male rats. Drug Alcohol Depend 215:108215. https://doi.org/10.1016/J.DRUGALCDEP.2020.108215
Sharapova S, Reyes-Guzman C, Singh T, et al (2018) Age of tobacco use initiation and association with current use and nicotine dependence among US middle and high school students, 2014–2016. Tob Control tobaccocontrol-2018-054593. doi:https://doi.org/10.1136/TOBACCOCONTROL-2018-054593
Shram MJ, Funk D, Li Z, Lê AD (2006) Periadolescent and adult rats respond differently in tests measuring the rewarding and aversive effects of nicotine. Psychopharmacology 186:201–208. https://doi.org/10.1007/s00213-006-0373-8
Shram MJ, Funk D, Li Z, Lê AD (2008) Nicotine self-administration, extinction responding and reinstatement in adolescent and adult male rats: evidence against a biological vulnerability to nicotine addiction during adolescence. Neuropsychopharmacology 33:739–748. https://doi.org/10.1038/sj.npp.1301454
Slawecki C (2003) Increased anxiety-like behavior in adult rats exposed to nicotine as adolescents. Pharmacol Biochem Behav 75:355–361. https://doi.org/10.1016/S0091-3057(03)00093-5
Slawecki CJ, Gilder A, Roth J, Ehlers CL (2003) Increased anxiety-like behavior in adult rats exposed to nicotine as adolescents. Pharmacol Biochem Behav 75:355–361. https://doi.org/10.1016/S0091-3057(03)00093-5
Smith LN, McDonald CG, Bergstrom HC et al (2006) Long-term changes in fear conditioning and anxiety-like behavior following nicotine exposure in adult versus adolescent rats. Pharmacol Biochem Behav 85:91–97. https://doi.org/10.1016/J.PBB.2006.07.014
Torres OV, Tejeda HA, Natividad LA, O’Dell LE (2008) Enhanced vulnerability to the rewarding effects of nicotine during the adolescent period of development. Pharmacol Biochem Behav 90:658–663. https://doi.org/10.1016/J.PBB.2008.05.009
Tripathi HL, Martin BR, Aceto MD (1982) Nicotine-induced antinociception in rats and mice: correlation with nicotine brain levels1
Zou S, Funk D, Shram MJ, Lê AD (2014) Effects of stressors on the reinforcing efficacy of nicotine in adolescent and adult rats. Psychopharmacology 231:1601–1614. https://doi.org/10.1007/s00213-013-3314-3
Acknowledgements
We are grateful for the skilled technical support of Derek Jacklin of the Central Animal Facility.
Funding
Support for the research was provided in part by the US National Institute on Drug Abuse DA045740 and the Canadian Natural Sciences and Engineering Research Council #RGPIN-2019-05147 to JEM. The funding sources had no role in study design; data collection, analyses, or interpretation; writing; or decision to submit article for publication.
Author information
Authors and Affiliations
Contributions
BR and JEM designed the study; BR, AKA, APS, RE, and MS conducted the behaviour studies; MA optimized the ELISA procedures and trained BR to conduct and interpret the ELISA assays; JYK provided access to and training on shock and open field equipment; BR analyzed the data and wrote the first draft of the manuscript; JEM provided manuscript revisions; all authors have given feedback on the final manuscript and approved its submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Renda, B., Andrade, A.K., Stone, A.P.S. et al. Adolescent nicotine and footshock exposure augments adult nicotine self-administration and drug-seeking without affecting baseline anxiety-like behaviour or stress responsivity in male rats. Psychopharmacology 238, 1687–1701 (2021). https://doi.org/10.1007/s00213-021-05803-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-021-05803-0