Abstract
Rationale and objectives
Stress increases drug intake. This depends on the stressor, drug, and aspect of drug seeking assessed. The objectives of these experiments done in adolescent and adult male rats were to (1) examine social defeat effects on acquisition of nicotine self-administration (SA) and the reinforcing efficacy of nicotine and (2) determine the effects of acute exposure to intermittent footshock (FS) or yohimbine on the reinforcing efficacy of nicotine.
Methods
In experiment 1, rats received four defeat exposures prior to nicotine SA acquisition and progressive ratio (PR) SA sessions (30 μg/kg nicotine/infusion). Exposure to an olfactory cue previously paired with defeat was also tested on responding maintained by nicotine on the PR schedule. In experiments 2 and 3, the effects of FS (5 and 10 min) or yohimbine (0.625 and 1.25 mg/kg, i.p.) on PR responding for nicotine (15, 30, or 60 μg/kg/infusion) were assessed. Adolescents were aged PD34-36 and adults PD81-85 at the beginning of nicotine SA training.
Results
Defeat did not affect nicotine SA acquisition. Prior exposure to defeat or a defeat-paired olfactory cue did not affect PR responding for nicotine. FS modestly decreased PR responding in adolescents at the middle nicotine infusion dose. Yohimbine increased PR responding independent of nicotine infusion dose and age.
Conclusions
Together with previous work with other drugs, our data indicate that the effects of stress on the reinforcing efficacy of nicotine are stressor- and drug-dependent. This suggests that there is heterogeneity among stressors on how they affect neuronal systems underlying drug intake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Studies in humans show that stressful life events are associated with increased use of, and relapse to, nicotine or other drugs of abuse (Brown et al. 1995; Pomerleau and Pomerleau 1991). The effects of stress on the initiation, maintenance, and reinstatement of drug seeking have been studied extensively using animal models. Using the reinstatement procedure, the effects of stress on relapse have been shown to be reliable and consistent across different laboratories and drug classes. As will be discussed below, there is heterogeneity among stressors in their effects on reinstatement, and these effects can depend on the drug examined (Le and Shaham 2002; Shalev et al. 2010). Despite the fact that stress clearly increases smoking in humans, to our knowledge, there are no studies examining the effects of stress on nicotine self-administration (SA) in laboratory animals.
Footshock stress (FS) is one of the most commonly used laboratory stressors. The effects of FS on SA vary as a function of drug class, dose, reinforcement schedule, level of dependence, and interactions among these variables. Although FS has been used extensively to examine the effects of stress on alcohol SA, these studies have produced inconsistent results. The effects of FS may depend on the conditions under which alcohol SA was examined. For example, FS has been shown to enhance alcohol SA under alcohol deprivation conditions (Funk et al. 2004; Vengeliene et al. 2003) but to have weak or inconsistent effects under non-deprivation conditions (Logrip and Zorrilla 2012). In contrast, non-contingent exposure to FS is facilitatory on cocaine SA (Goeders and Guerin 1994; Mantsch and Katz 2007). Similarly, FS increases the oral intake of fentanyl solution under higher demand FR (FR4) and progressive ratio (PR) schedules of reinforcement (Shaham et al. 1993). FS also increased heroin SA under a PR schedule (Shaham and Stewart 1994).
Two stressors, FS and yohimbine, an alpha-2 adrenoceptor antagonist, reliably reinstate the seeking of nicotine and other drugs (Anker and Carroll 2010; Buczek et al. 1999; Feltenstein and See 2006; Le et al. 2005; Leao et al. 2009; Shaham et al. 2000; Shepard et al. 2004; Yamada and Bruijnzeel 2011; Zislis et al. 2007). In contrast to the variable effects of FS, we and others have shown that yohimbine also increases alcohol SA (Ayanwuyi et al. 2013; Bertholomey et al. 2013; Le et al. 2005), and we recently reported that it increases nicotine SA in adolescent rats (Li et al. 2012). The effects of yohimbine on the SA of other drugs are not known.
Another stressor, social defeat, has a unique pattern of effects on drug-seeking behavior. It produces the most reliable effects on the initiation of drug SA, and importantly, exposure to this stressor can have long-lasting effects on drug SA (Bardo et al. 2013; Miczek et al. 2008). These effects have been systematically studied in cocaine-trained animals. Exposure to social defeat prior to initiation of cocaine SA training increases the rate of acquisition of cocaine SA and increases cocaine intake under FR and PR schedules of reinforcement (Covington et al. 2005; Covington and Miczek 2001a; Tidey and Miczek 1997). In contrast, acute exposure to this stressor may decrease drug intake, possibly due to fear responses such as freezing (Chung et al. 2000). For example, acute exposure to defeat decreases alcohol SA (Funk et al. 2005; van Erp and Miczek 2001). No work has been done on the effects of defeat on any aspect of nicotine seeking.
Adolescence is a vulnerable period in the initiation of drug intake (SAMHSA 2011). Stressful events are significantly correlated with smoking and intentions to smoke in adolescents (Booker et al. 2004, 2007, 2008), and adolescents report that stress is a salient precipitant of smoking (DiFranza et al. 2004; Weiss et al. 2008). Stress also enhances the rate of smoking initiation in adolescents (Booker et al. 2007, 2008; Byrne et al. 1995; Byrne and Mazanov 2003). Two possible reasons for this are that adolescence is a stressful developmental period and that adolescents may be more sensitive to the effects of stress than adults (Choi and Kellogg 1996; Novak et al. 2007; Slawecki 2005; Vazquez 1998). In support of these findings, FS was shown to facilitate the development of conditioned place preference (CPP) to nicotine in adolescent rats, suggesting that stress enhances the rewarding effects of nicotine (Brielmaier et al. 2012). Work with other drugs has demonstrated age-dependent effects of stress on drug seeking. Yohimbine-induced reinstatement of cocaine seeking was shown to be of a higher magnitude in adolescents (Anker and Carroll 2010). Despite these data, no work has been done examining the possibility that there are age differences in sensitivity to the effects of stressors on the reinforcing efficacy of nicotine or whether such differences in stress sensitivity may affect initiation of nicotine SA.
The purpose of the present investigation is to examine the effects of three different stressors on nicotine SA and its reinforcing efficacy. In light of the findings of the Miczek laboratory (Covington and Miczek 2001a), the first experiment investigated the effects of exposure to social defeat on acquisition of nicotine SA and then on the reinforcing efficacy of nicotine using a PR schedule of reinforcement, in both adolescent and adult rats. In the second and third experiments, the effects of acute exposure to FS and yohimbine, two stressors that reliably reinstate nicotine seeking, on the reinforcing efficacy of nicotine were determined in adolescent and adult rats previously trained to SA nicotine.
Materials and methods
Subjects
Forty-eight pregnant Long Evans dams (n = 16 per experiment; Charles River Laboratories, Quebec, Canada) were used as a source of juvenile rats run in the experiments and were housed singly in plastic cages (51 × 41 × 20 cm). Adult male Long Evans rats were purchased from Charles River and were singly housed in plastic cages. On the day of weaning (post-natal day (PD) 21), 92 male pups were group housed by litter. After surgery, all rats were singly housed and fed 20–22 g of rat chow per day. The rats were maintained on a 12/12 h light/dark cycle (lights on at 1900) in a humidity- and temperature-regulated vivarium. The experimental procedures followed the NIH publication “Principles of laboratory animal care” (Eighth edition, 2011) and were approved by animal care and use committee of the Centre for Addiction and Mental Health.
Apparatus
Nicotine SA was performed in 24 chambers equipped with one active lever and one inactive lever. Appropriate responding on the active lever activated the infusion pump that delivered the intravenous (i.v.) nicotine followed by a 40-s timeout. Each infusion was accompanied by a compound light-tone cue (stimulus light illumination for 6 s and a 2,800-Hz tone for 1 s). Responding on the inactive lever had no programmed consequences but was recorded. Sucrose pellet SA (prior to nicotine SA) was conducted in a separate set of 16 similar operant chambers equipped with pellet dispensers. No cues were present during sucrose pellet training.
Surgery
Rats (adolescents: PD26; adults: PD73-75) were anesthetized using ketamine/xylazine (75 mg/kg ketamine/10 mg/kg xylazine (Shram et al. 2008)). Incision sites were treated with a local anesthetic (0.1 ml bupivacaine, 0.125 %, s.c.). Penicillin (30,000 U, i.m.) was administered as an antibiotic prior to surgery and buprenorphine (0.01 mg/kg, s.c.) as an analgesic after surgery. Catheters were implanted into the right jugular vein as previously described (Corrigall and Coen 1989) and exited between the scapulae and were attached to the modified 22-gauge cannula connected to the fluid swivel system. After recovery, catheters were flushed daily with 0.1 ml of a sterile heparin–saline solution (50 U/ml). Catheter patency was tested after PR testing was completed by i.v. injections of sodium methohexital (0.05 mg/kg). The data from animals that did not show rapid anesthesia following methohexital injection were excluded from analysis.
Drugs
Solutions of nicotine (Sigma-Aldrich, Oakville, Ontario, Canada) of pH 6.8 to 7.2 were prepared fresh daily. The unit doses for the i.v. nicotine SA were 30 μg/kg/infusion in experiment 1 and 15, 30, or 60 μg/kg/infusion in experiments 2 and 3. Nicotine infusions were made in a volume of 10 μl nicotine solution/100 g body weight over 0.5–1.5 s. Yohimbine solutions (Sigma-Aldrich, Oakville, Ontario, Canada) were prepared fresh daily in a distilled water vehicle and were injected at doses of 0.625 and 1.25 mg/kg i.p., in a volume of 1 ml/kg. Drug doses are expressed as base.
Procedures
Figure 1 shows the timeline of each of the experiments.
Sucrose pellet SA
Prior to catheterization surgery, the juvenile (P22) and adult (PD68-70) rats underwent operant training for 45 mg sucrose pellets (Bioserv, Frenchtown, NJ, USA) over 2 days in overnight sessions under an FR1 reinforcement schedule (Li et al. 2012; Shram et al. 2008). Animals spontaneously acquired SA of the sucrose pellets. During these sessions, water was freely available but only the sucrose pellets were available as a source of calories.
Nicotine SA
Fixed ratio
After sucrose pellet training, surgery, and recovery, rats initiated nicotine SA in 1-h daily sessions at FR1 and then FR2.
Progressive ratio
After the final FR2 session, the daily 2-h PR sessions were conducted. The PR sequence was determined using the exponential formula (5 × EXP(0.2 × infusion number) − 5) (Donny et al. 1999). The number of infusions was recorded, and the session was terminated when no presses were made on the active lever for 20 min.
Stressors
Social defeat
The social defeat procedure is based on previous studies done on adolescent and adult rats (Burke et al. 2010, 2011; Funk et al. 2005; van Erp and Miczek 2001; van Erp et al. 2001). Animals receiving social defeat (intruders) were introduced into the home cages of larger, dominant male rats (n = 12). These “resident” (aggressive) rats were Long Evans males (400–450 g) that had been housed with female rats (n = 12) for 10 days to enhance their territoriality and aggression and were selected based on their display of stable patterns of aggressive behavior (e.g., short latency to induce attacks, threatening postures) towards intruders. After the defeat of the intruders, defined as demonstration of supine posture that typically occurred following one or two attacks by the resident males, a wire screen was inserted into the cage to separate the intruder from the resident for 30 min. This prevented further attacks, but allowed the defeated rat to be exposed to the olfactory, visual, and auditory stimuli of the attacker. To insure consistently robust defeat induction, intruders were exposed to a different resident rat on each of the four defeat episodes. Five minutes prior to and during the defeat sessions, animals were exposed to an olfactory cue (peppermint essence, 1 ml, McCormick, London, Ontario, Canada) on gauze pads in culture dishes placed above the wire mesh of the cages. Control animals not receiving defeat were placed in cages similar to those used for defeat and received exposure to the odor but were not subject to defeat.
FS
Intermittent FS (5 and 10 min) was administered just prior to the start of the 2-h PR sessions. The shock delivery parameters were as follows: 0.5 s ON, a mean OFF period of 40 s, and a range of 10–70 s between each shock delivery (Le et al. 1998, 2011; Shaham and Stewart 1995). The intensity of FS required to induce vocalization in the adolescents and adults was determined to be 0.6 mA for adolescents and 0.8 mA for adults in a pilot study (data not shown); these intensity values were used for the administration of FS in the present studies.
Yohimbine
Yohimbine or its vehicle (water) was injected at doses of 0.625 and 1.25 mg/kg (i.p.) 30 min prior to the 2-h PR sessions. The yohimbine doses selected are based on previous work (Le et al. 2011; Li et al. 2012; Marinelli et al. 2007).
Statistics and data presentation
The dependent measures for SA under FR were the number of infusions and active and inactive lever presses during the 1-h sessions. For the PR sessions, they were the number of infusions and inactive lever presses made before cessation of responding for 20 min. These measures were analyzed separately using ANOVAs or ANCOVAs. Significant interactions (p values < 0.05) determined in the omnibus analyses were followed by post-hoc tests where appropriate using the Newman–Keuls method (Tybout et al. 2001). The numbers of active lever presses made during the PR sessions are presented but were not analyzed statistically.
Experiment 1: effects of social defeat on acquisition of nicotine SA and reinforcing efficacy of nicotine
Figure 1a shows the timeline of experiment 1. After catheter surgery and 2–3 days of recovery, rats received four daily defeat episodes, each paired with a mint olfactory cue, with a 1-day break between the second and third episodes beginning on PD31 for the adolescents (n = 11) and PD 80 (n = 11) for the adults. Non-defeated controls (n = 11 adolescents; n = 11 adults) received exposure to the olfactory cue, but no defeat. The day after the last defeat episode, rats initiated SA of nicotine at 30 μg/kg/infusion at FR1 for 4 days and FR2 for 3 days and then received PR sessions for 5 days (beginning on PD43 for adolescent and PD91 for adults). On the fifth day under the PR schedule, all rats received a test of the effects of the mint olfactory cue.
Experiment 2: acute effects of FS on the reinforcing efficacy of nicotine
Figure 1b shows the timeline of experiment 2. Adolescent (PD34; n = 34) and adult (PD81; n = 29) rats initiated SA of nicotine at 30 μg/kg/infusion at FR1 for 4 days and then at FR2 for 3 days. Rats were then assigned to one of three nicotine infusion dose groups (15, 30, or 60 μg/kg/infusion; N = 11–12 for adolescents, N = 9–10 for adults), matched on their mean nicotine intake over the three sessions at FR2. Rats responded for nicotine at these doses under an FR2 reinforcement schedule for a 1-h session.
Rats underwent daily PR SA sessions for 7 days (beginning on PD42 for adolescents and PD89 for adults) at one of the three nicotine doses. Rats received 5 min of intermittent FS on the fifth day of PR (adolescents: PD46; adults: PD93) and 10 min of FS on the seventh day (PD48 and PD95), immediately prior to the start of the PR sessions. Responding on the fourth day of the PR was used as the baseline.
Experiment 3: acute effects of yohimbine on the reinforcing efficacy of nicotine
Figure 1c shows the timeline of experiment 3. Adolescent (n = 36) and adult (n = 30) rats were trained to self-administer nicotine (FR1 and FR2 for 4 and 3 days, respectively) and were assigned to the three nicotine infusion dose groups (15, 30, or 60 μg/kg/infusion; N = 12/group for adolescents, N = 10/group for adults) as in experiment 2. They received PR sessions and stressor exposure according to the same schedule and at the same ages as the rats in experiment 2. They were injected with yohimbine vehicle (water, “0” dose) on the fourth day of PR, 1.25 mg/kg yohimbine on the fifth day of PR and with 0.625 mg/kg on the seventh day, 30 min prior to the start of the PR sessions. The half-life of yohimbine following i.p. injection in rodents was estimated to be 3 h in the brain (Ho et al. 1971). The inter-injection interval we used (48 h) is therefore sufficient for drug washout.
Results
Experiment 1: social defeat
Effect of prior defeat on acquisition of nicotine SA
Figure 2 shows the mean ± standard error of the mean (sem) number of infusions (a) and the active (b) and inactive (c) lever presses during acquisition of nicotine SA of animals previously exposed to social defeat or the control condition. There was no significant effect of social defeat or interaction of social defeat with any other factor on these measures (p's > 0.05). The numbers of infusions received decreased across days at FR1 (F(3,36) = 5.89, p < 0.05). Post-hoc tests showed that days 2, 3, and 4 were significantly lower than day 1 in all groups (p's < 0.05) except in the adult rats that did not receive defeat. Overall, infusions increased across days at FR2 (F(2,40) = 5.91, p < 0.05), but post-hoc tests did not show any differences within groups across the days at FR2. Adults received greater numbers of nicotine infusions than did adolescents at FR1 and FR2, reflected in significant effects of age (FR1: (F(1,36) = 8.56, p < 0.05); FR2: (F(1,40) = 43.3, p < 0.05)). As was the case for the infusion data, active lever responding decreased across days at FR1 (F(1,36) = 15.18, p < 0.05). At FR2, active responding increased across days (F(2,40) = 3.16, p < 0.05) and adults pressed more than adolescents (F(1,40) = 25.73, p < 0.05). There were no significant effects in the analysis of the inactive lever data.
Mean numbers (±sem) of nicotine infusions (a) and active (b) and inactive (c) lever presses during acquisition of nicotine SA (30 μg/kg/infusion) at FR1 and FR2 shown by adolescent and adult rats that had previously experienced social defeat or no defeat. n = 11 per age/defeat group. Open symbols, no defeat; closed symbols, defeat; triangles, adolescents; circles, adults; asterisk, significantly lower than day 1 in the adolescent-no defeat, adolescent-defeat, and adult-defeat groups
Effect of prior defeat on the reinforcing efficacy of nicotine
Figure 3 shows the mean ± sem number of infusions (a) and the active (b) and inactive (c) lever presses of the animals averaged over the first 4 PR sessions. In the analyses done on infusions and inactive lever presses, there was no significant effect of social defeat (p's > 0.05). Irrespective of defeat condition, adults received a greater number of nicotine infusions than did adolescents (F(1,40) = 18.22, p < 0.05). Adults also pressed slightly but significantly more than adolescents on the inactive lever (F(1,40) = 5.03, p < 0.05).
Mean numbers (±sem) of nicotine infusions (a) and active (b) and inactive (c) lever presses averaged over the 4 days of a PR schedule of reinforcement shown by adolescent and adult rats that had previously experienced four daily episodes of social defeat or no defeat. n = 11 per age/defeat group. Open bars, adolescents; shaded bars, adults; asterisks, significantly different from adolescents
Effect of an odor cue associated with defeat on the reinforcing efficacy of nicotine
Figure 4 shows the mean ± sem number of infusions (a) and the active (b) and inactive (c) lever presses in response to an odor cue previously paired or not paired with social defeat. In the analyses done on infusions and inactive lever pressing, there were no significant effects of the odor cue (p's > 0.05). Compared to adolescents, adults received significantly greater numbers of nicotine infusions (F(1,38) = 11.34, p < 0.05). There were no significant effects in the analysis of the inactive lever data.
Mean numbers (±sem) of nicotine infusions (a) and active (b) and inactive (c) lever presses on a PR schedule in response to an olfactory cue previously unpaired (left panels) or paired (right panels) with social defeat in adolescent and adult rats. n = 10–11 per age/defeat group. Open bars, adolescents; shaded bars, adults; asterisk, significantly different from adolescents
Experiments 2 and 3: effects of acute administration of FS and yohimbine stressors on PR responding maintained by nicotine
Effect of age on the reinforcing efficacy of different doses of nicotine
Figure 5 shows the mean ± sem number of infusions (a) and the active (b) and inactive (c) lever presses of the animals in experiments 2 and 3 responding for 15, 30, or 60 μg/kg infusion doses of nicotine averaged over the first 4 PR sessions. Numbers of infusions (F(2,128) = 16.5, p < 0.05) significantly increased as a function of nicotine dose. Overall, adults received greater numbers of infusions (F(1,128) = 38.6, p < 0.05). There was a significant Age × Nicotine dose interaction (F(2,128) = 6.6, p < 0.05), as adults received greater numbers of nicotine infusions than adolescents at the 15 and 30 μg/kg infusion doses (p's < 0.05), but there was no difference at the 60 μg/kg infusion dose. There were slight but significant nicotine dose-dependent increases in inactive lever responding (F(2,128) = 9.27, p < 0.05), and adults overall pressed more on the inactive lever (F(1,128) = 12.95, p < 0.05).
Mean numbers (±sem) of nicotine infusions (a) and active (b) and inactive (c) lever presses shown by adolescent and adult rats in experiments 2 and 3 averaged over 4 days on a PR schedule of reinforcement at nicotine doses of 15, 30, or 60 μg/kg/infusion, prior to testing with stressors. n = 19–24 per age/dose group. Open bars, adolescents; shaded bars, adults; asterisk, significantly different from adolescents
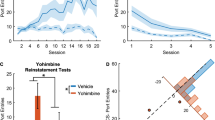
Experiment 2: acute effect of FS on the reinforcing efficacy of nicotine
Figure 6 presents the mean ± sem number of infusions (a) and the active (b) and inactive (c) lever presses for the FS duration–response curve. As there were significant main effects and interaction on inactive lever presses (see below), ANCOVA with inactive lever responding as a covariate was used to analyze the infusion data. Analysis of nicotine infusions showed a significant FS duration × Age × Nicotine dose interaction (F(4,96) = 2.56, p < 0.05). Adult rats received significantly more infusions at the 15 and 30 μg/kg doses (p's < 0.05), but there were no age differences at the 60 μg/kg dose. Two-way ANOVAs done at each nicotine infusion dose revealed a significant Age × FS duration interaction for the 30-μg dose (F(2,32) = 4.38, p < 0.05). One-way ANOVAs done for each age group at this dose showed a significant effect of FS duration in the adolescents (F(2,16) = 8.16, p < 0.05) but not adults (p > 0.05), and post-hoc analysis showed that 10 min of FS significantly reduced responding in adolescents (p < 0.05). ANOVA done on inactive lever presses revealed significant effects of FS duration (F(2,102) = 5.02, p < 0.05), age (F(1,51) = 8.47, p < 0.05), nicotine dose (F(2,51) = 3.46, p < 0.05), and a significant FS duration × Age × Nicotine dose interaction (F(4,102) = 3.092, p < 0.05). Two-way ANOVAs done on numbers of inactive lever presses at each nicotine infusion dose revealed a significant Age × FS duration interaction for the 15-μg dose (F(2,17) = 4.04, p < 0.05), but the follow-up one-way ANOVAs done on each age group at this dose with the repeated factor of FS duration did not show any significant effects (p's > 0.05).
Effects of intermittent FS (0, 5, and 10 min) on mean numbers (±sem) of nicotine infusions (top) and active (middle) and inactive lever presses (bottom) shown by adolescent and adult rats responding for nicotine on a PR schedule at doses of 15 (a), 30 (b), and 60 (c) μg/kg nicotine/infusion. n = 9–11 per age/dose group. Open bars, adolescents; shaded bars, adults; asterisks, significantly different from adolescents; plus sign, significantly different from no shock condition
Experiment 3: acute effect of yohimbine on the reinforcing efficacy of nicotine
Figure 7 shows the mean ± sem number of infusions (a) and the active (b) and inactive (c) lever presses for the yohimbine dose–response curve. Since there was a significant effect of yohimbine dose (F(2,120) = 15.56, p < 0.05) in the analysis of inactive lever pressing, ANCOVA with the covariate of inactive lever presses was used to analyze the infusion data. Yohimbine significantly increased numbers of nicotine infusions received under the PR schedule (F(2,114) = 55, p < 0.05). Adults overall received more nicotine infusions than adolescents (F(1,57) = 24.48, p < 0.05). There was significant Age × Nicotine dose interaction (F(2.57) = 6.25, p < 0.05), and post-hoc analysis of this interaction revealed that adult rats received more infusions than adolescents at the 15- and 30-μg doses (p's < 0.05) but did not differ at the 60-μg dose.
Effects of yohimbine (vehicle (0), 0.625, 1.25 mg/kg) on mean number (±sem) of nicotine infusions (top) and active (middle) and inactive (bottom) lever presses shown by adolescent and adult rats responding for nicotine on a PR schedule at doses of 15 (a), 30 (b), and 60 (c) μg/kg nicotine/infusion. n = 10–12 per age/dose group. Open bars, adolescents; shaded bars, adults; asterisk, significantly different from adolescents; plus sign, significantly different from yohimbine vehicle (0 dose) condition
Discussion
We found that prior exposure to social defeat did not affect acquisition of nicotine SA or the reinforcing efficacy of nicotine under a PR schedule in either adolescent or adult rats, nor did an odor cue previously paired with social defeat affect the reinforcing efficacy of nicotine. Acute intermittent FS had slight, suppressive effects on the reinforcing efficacy of nicotine that were expressed in an age- and nicotine infusion dose-dependent manner. In contrast, we found that acute administration of the alpha-2 antagonist yohimbine strongly increased the reinforcing efficacy of nicotine; this effect was independent of age or infusion dose of nicotine. We also found that across the three experiments, adults self-administered more nicotine under both FR and PR schedules than adolescents.
Effects of social defeat on nicotine SA
Social defeat is an ethologically relevant stressor that produces similar behavioral and physiological effects to more routinely used stressors such as FS and can have long-lasting effects on behavior and biochemistry (Berton et al. 1999; Burke et al. 2013). While the effects of stressors such as FS on drug SA are mixed or small in magnitude (Brunell and Spear 2005; Chester et al. 2008; Dayas et al. 2004; Logrip and Zorrilla 2012), social defeat has been shown to have more reliable and long-lasting effects (Covington et al. 2005; Cruz et al. 2011).
We found that prior exposure to social defeat did not affect the acquisition of nicotine SA or influence the reinforcing efficacy of nicotine as indexed by responding on a PR schedule. These results are at odds with previous work showing that social defeat enhances acquisition of cocaine self-administration and responding maintained by cocaine on FR and PR schedules (Covington et al. 2005; Covington and Miczek 2001b, 2005; Cruz et al. 2011; Kabbaj et al. 2001; Miczek et al. 2004). The reasons for the lack of effect are not clear. One possibility is that the effects of defeat are drug-specific and enhancing effects are only expressed with cocaine. In support of this, exposure to defeat did not affect responding for heroin (Cruz et al. 2011) and decreased responding maintained by alcohol (Funk et al. 2005; van Erp and Miczek 2001). Further studies are needed to evaluate this issue.
In the present study, we did not find that an odor cue previously paired with defeat affected nicotine SA in adolescents or adults. This contrasts with our previous report that such a cue significantly reduced alcohol SA on an FR schedule (Funk et al. 2005). This may again suggest a specific effect of such cues on alcohol seeking, although this is difficult to evaluate as the effects of defeat-paired cues on the SA of other drugs are not known.
Few studies have examined the effects of social defeat in adolescents. Burke et al. showed that exposure to repeated defeat during adolescence led to enhanced development of CPP to amphetamine and hyperactivity in adulthood (Burke et al. 2010, 2011, 2013). In these studies, however, the effects of defeat were not specifically compared between adolescents and adults.
A potential concern is that the degree of stress experienced by the defeated adults differed from that of the defeated adolescents. In our study, to ensure that defeat would be reliably and efficiently induced, the resident male rats (aggressors) were previously housed with females to increase their territoriality and were selected on the basis of aggression towards intruders. The defeated animals were also exposed to a different aggressor in each defeat episode to avoid habituation. Despite this, we did note that the adolescents took longer to be attacked by the resident and defeated (display of supine posture), suggesting reduced aggression. We did not, however, observe any differences between adolescents and adults in the effects of defeat on any aspect of nicotine SA, suggesting that this increased defeat latency did not impact the results. Nevertheless, in the absence of a biological measure of stress, such as circulating corticosterone, the possibility that there were age differences in induced levels of stress by the defeat cannot be ruled out.
Effects of FS on nicotine SA
Although intermittent FS induces relapse to nicotine seeking in rodents (Bilkei-Gorzo et al. 2008; Buczek et al. 1999; Yamada and Bruijnzeel 2011; Zislis et al. 2007), its effects on nicotine SA are not known. We found that FS had modest suppressive effects on the reinforcing efficacy of nicotine in both adolescent and adult rats. Although the relevance of these small effects of FS can be called into question, our results, taken with previous research, indicate differences in the effects of FS on nicotine taking and seeking. FS suppresses intake mildly but robustly induces reinstatement of nicotine seeking (Buczek et al. 1999; Zislis et al. 2007). These results are different from those previously reported for the effects of FS on responding maintained by heroin on a PR schedule. FS increased the reinforcing efficacy of heroin, particularly at high infusion doses. It is possible that the failure to observe such effects in adult rats in the present study is due to the flattened nicotine infusion dose curve under the PR schedule. This, however, is an unlikely explanation as a dose–response relationship for nicotine SA was observed in the adolescent rats, and as discussed below, yohimbine can enhance SA in both adult and adolescent rats. Therefore, a potential future experiment would be to test the effects of FS on higher nicotine infusion doses than used in the present experiment to determine whether there is a similar dose dependency for the effects of FS on the reinforcing efficacy of nicotine.
Exposure to FS has been shown to enhance the development of CPP to nicotine in adolescent rats, suggesting that this stressor may affect the rewarding properties of nicotine (Brielmaier et al. 2012). This contrasts with our findings of slight suppression of the reinforcing efficacy of nicotine measured on a PR schedule. In the Brielmaier et al. study, FS was given 24 h prior to any pairing or exposure to nicotine, whereas in our study, it was administered immediately prior to the PR SA sessions in rats that were trained to self-administer nicotine. Whether this difference in timing can account for the different patterns of results observed between the two studies is not known. Another possible factor is that while FS might enhance the rewarding effect of nicotine as assessed by CPP, such an enhancement might not affect its reinforcing efficacy as measured on a PR in an operant paradigm. In our previous work, we have found age differences in the development of CPP to nicotine, with adolescent but not adult rats displaying CPP across different doses of nicotine (Shram et al. 2006). On a PR schedule, however, adolescents appear to be less motivated to self-administer nicotine than adults as shown in the present and previous studies (Shram et al. 2008).
Effects of yohimbine on nicotine SA
We and others have found that yohimbine reliably reinstates the seeking of alcohol, psychostimulants, heroin, and food (Anker and Carroll 2010; Feltenstein et al. 2012; Ghitza et al. 2006; Le et al. 2005; Nair et al. 2009; Shepard et al. 2004; Zhou et al. 2013). Yohimbine is a prototypical alpha-2 adrenoceptor antagonist that induces stress-like states in both humans and non-human primates (Bremner et al. 1996a, b; Holmberg and Gershon 1961; Lang and Gershon 1963). Yohimbine is unique as a stressor because it increases nicotine and alcohol SA (Li et al. 2012; Marinelli et al. 2007), whereas acute exposure to other stressors, including FS, does not do so reliably (Brunell and Spear 2005; Darnaudery et al. 2007). With the exception of our recent study (Li et al. 2012), there is no work on the effects of yohimbine on the reinforcing efficacy of nicotine.
We found in the present study that yohimbine strongly increased the reinforcing efficacy of nicotine on a PR schedule in both adolescents and adults at all infusion doses of nicotine employed. This is in agreement with our recent findings of significant yohimbine-induced increases in the reinforcing efficacy of nicotine in male and female adolescent rats (Li et al. 2012). The size of the effects of yohimbine on intake was not markedly influenced by age. This indicates that adolescents are not more sensitive to the effects of this stressor on the reinforcing efficacy of nicotine.
We noted that the effects of yohimbine on nicotine's reinforcing efficacy were not dose-dependent. Yohimbine produced significant increases in responding maintained by nicotine on the PR schedule at both of the doses tested. This lack of dose dependency is consistent with our past work on yohimbine-induced reinstatement of alcohol seeking (Le et al. 2005). In addition, we noted a lack of dose dependency of yohimbine administered at a lower dose range (0.3–0.6 mg/kg) than in the present study on the reinforcing efficacy of a 30 μg/kg infusion dose of nicotine (Li et al. 2012).
Age differences in nicotine self-administration
In the present study, we found that adults self-administered significantly more nicotine under the PR schedule than did adolescents at 15 and 30 μg, but not at the 60-μg infusion dose. Consistent with this, in a previous study, we observed that adults responded more for nicotine on a PR at a 30-μg infusion dose than did adolescents (Shram et al. 2008). Our present findings extend this in showing that such age differences also occur at 15 μg, but not at a higher infusion dose of 60 μg. These findings with PR suggest that adolescents find nicotine less reinforcing than adults. This contrasts with our other work using conditioned place preference, discussed above, showing that adolescents find nicotine more rewarding (Shram et al. 2006). Taken together with our previous findings with place preference, our present data suggest that although adolescents may find nicotine more rewarding, they find it less reinforcing.
We observed that, although statistically significant, the effect of nicotine infusion dose on the numbers of infusions received on the PR was relatively small. This is consistent with previous work on nicotine SA in rats on a PR. For example, the number of infusions received on a PR at nicotine infusion doses of 20, 30, and 60 μg/kg was about 6, 7, and 10 infusions/4 h session, respectively (Donny et al. 1999), values in line with our present findings. The reasons for this relatively flat nicotine dose response are not known. Despite this shallow dose response, we believe that nicotine was self-administered due to its reinforcing effects. Overall, animals pressed reliably and at high rates during FR training, and their responding increased when they were shifted to the PR.
Conclusions
The three stressors we examined each had distinct effects on nicotine SA. Prior exposure to defeat had no effects, FS had very small, suppressive effects, and yohimbine strongly increased nicotine SA. We did not observe the effects of these stressors to be markedly influenced by age.
The neurobiological mechanisms underlying the differences in the effects of these stressors are not known. The foci of our previous work were to characterize these three stressors in their effects on relapse using the reinstatement procedure and to determine the brain mechanisms underlying these effects. We found that these three stressors affected relapse, with FS and yohimbine reliably inducing reinstatement of nicotine and alcohol seeking, while social defeat had slight suppressive effects on reinstatement of alcohol seeking (Buczek et al. 1999; Funk et al. 2005; Le et al. 1998, 2005). We also reported that all three of these stressors activated the extrahypothalamic corticotropin-releasing factor (Funk et al. 2006), which is consistent with previous work on their effects on HPA axis activation (Berton et al. 1999; Dazzi et al. 2001; Marinelli et al. 2007). Taken together with this work, our present data suggest that activation of extrahypothalamic CRF pathways alone may not be sufficient to affect SA. CRF may, however, have an important role under other conditions, for example, with enhanced intake. Blockade of CRF R1 with antalarmin does not affect basal alcohol intake but does reduce the increased intake produced by withdrawal in alcohol-dependent animals (Funk et al. 2007) or the increased intake seen with yohimbine (Marinelli et al. 2007).
Yohimbine had the most salient effects on the reinforcing efficacy of nicotine, producing marked increases in responding. Taking these results together with previous work on yohimbine, it can be argued that yohimbine is quite unique among the stressors or other stimuli that have been assessed on drug taking and seeking. Yohimbine administration (Charney et al. 1983; Davis et al. 1979) and withdrawal from alcohol (Gilpin 2012; Slawecki and Roth 2004; Valdez et al. 2002) or nicotine (Kenny and Markou 2001) are all associated with increased anxiety. With these results in mind, it is interesting to note that both yohimbine (Le et al. 2011; Li et al. 2012) and withdrawal from ethanol (Walker 2012) or nicotine (George et al. 2007) can enhance alcohol or nicotine SA.
The reasons why yohimbine has this unique constellation of behavioral effects are not known. One possibility is that it has widespread actions on brain pathways that underlie drug seeking and taking. In support of this, in addition to its alpha-2 antagonist properties, yohimbine acts as a dopamine D2 antagonist and as a 5-hydroxytryptamine (5-HT) 1a receptor agonist (Millan et al. 2000). Combined actions at these receptor classes may contribute to the potent effects of yohimbine on both drug SA and relapse. Consistent with the idea that this lack of specificity may be tied to its potency is that in a recent fMRI study, yohimbine produced widespread activation of extrahypothalamic stress systems implicated in drug seeking (Gozzi et al. 2013).
To summarize our findings, in nicotine SA studies, we found that prior exposure to social defeat stress did not affect the acquisition of nicotine SA or the rewarding efficacy of nicotine. Intermittent FS caused small, infusion dose-dependent decreases in the rewarding efficacy of nicotine that was also influenced by age. Yohimbine strongly increased the rewarding efficacy of nicotine, an effect that depended on nicotine infusion dose, but was not related to age. Consistent with our previous work, we also found that adults self-administered more nicotine than adolescents under a PR schedule, indicating that adults find intravenous nicotine more reinforcing than adolescents. Our data indicate that the effects of stress on the reinforcing efficacy of nicotine are highly dependent on the stressor. This suggests heterogeneity in the effects of stressors on the neuronal systems that underlie nicotine intake and the rewarding efficacy of nicotine.
References
Anker JJ, Carroll ME (2010) Reinstatement of cocaine seeking induced by drugs, cues, and stress in adolescent and adult rats. Psychopharmacology (Berl) 208:211–222
Ayanwuyi LO, Carvajal F, Lerma-Cabrera JM, Domi E, Bjork K, Ubaldi M, Heilig M, Roberto M, Ciccocioppo R, Cippitelli A (2013) Role of a genetic polymorphism in the corticotropin-releasing factor receptor 1 gene in alcohol drinking and seeking behaviors of Marchigian Sardinian alcohol-preferring rats. Front Psychiatry 4:23
Bardo MT, Neisewander JL, Kelly TH (2013) Individual differences and social influences on the neurobehavioral pharmacology of abused drugs. Pharmacol Rev 65:255–290
Bertholomey ML, Verplaetse TL, Czachowski CL (2013) Alterations in ethanol seeking and self-administration following yohimbine in selectively bred alcohol-preferring (P) and high alcohol drinking (HAD-2) rats. Behav Brain Res 238:252–258
Berton O, Durand M, Aguerre S, Mormede P, Chaouloff F (1999) Behavioral, neuroendocrine and serotonergic consequences of single social defeat and repeated fluoxetine pretreatment in the Lewis rat strain. Neuroscience 92:327–341
Bilkei-Gorzo A, Racz I, Michel K, Darvas M, Maldonado R, Zimmer A (2008) A common genetic predisposition to stress sensitivity and stress-induced nicotine craving. Biol Psychiatry 63:164–171
Booker CL, Gallaher P, Unger JB, Ritt-Olson A, Johnson CA (2004) Stressful life events, smoking behavior, and intentions to smoke among and multiethnic sample of sixth graders. Ethn Health 9:369–397
Booker CL, Unger JB, Azen SP, Baezconde-Garbanati L, Lickel B, Johnson CA (2007) Stressful life events and smoking behaviors in Chinese adolescents: a longitudinal analysis. Nicotine Tob Res 9:1085–1094
Booker CL, Unger JB, Azen SP, Baezconde-Garbanati L, Lickel B, Johnson CA (2008) A longitudinal analysis of stressful life events, smoking behaviors, and gender differences in a multicultural sample of adolescents. Subst Use Misuse 43:1521–1543
Bremner JD, Krystal JH, Southwick SM, Charney DS (1996a) Noradrenergic mechanisms in stress and anxiety: I. preclinical studies. Synapse 23:28–38
Bremner JD, Krystal JH, Southwick SM, Charney DS (1996b) Noradrenergic mechanisms in stress and anxiety: II.clinical studies. Synapse 23:39–51
Brielmaier J, McDonald CG, Smith RF (2012) Effects of acute stress on acquisition of nicotine conditioned place preference in adolescent rats: a role for corticotropin-releasing factor 1 receptors. Psychopharmacology (Berl) 219:73–82
Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA (1995) Stress, vulnerability and adult alcohol relapse. J Stud Alcohol 56:538–545
Brunell SC, Spear LP (2005) Effect of stress on the voluntary intake of a sweetened ethanol solution in pair-housed adolescent and adult rats. Alcohol Clin Exp Res 29:1641–1653
Buczek Y, Le AD, Stewart J, Shaham Y (1999) Stress reinstates nicotine seeking but not sucrose solution seeking in rats. Psychopharmacology (Berl) 144:183–188
Burke AR, Renner KJ, Forster GL, Watt MJ (2010) Adolescent social defeat alters neural, endocrine and behavioral responses to amphetamine in adult male rats. Brain Res 1352:147–156
Burke AR, Watt MJ, Forster GL (2011) Adolescent social defeat increases adult amphetamine conditioned place preference and alters D2 dopamine receptor expression. Neuroscience 197:269–279
Burke AR, Forster GL, Novick AM, Roberts CL, Watt MJ (2013) Effects of adolescent social defeat on adult amphetamine-induced locomotion and corticoaccumbal dopamine release in male rats. Neuropharmacology 67:359–369
Byrne DG, Mazanov J (2003) Adolescent stress and future smoking behaviour: a prospective investigation. J Psychosom Res 54:313–321
Byrne DG, Byrne AE, Reinhart MI (1995) Personality, stress and the decision to commence cigarette smoking in adolescence. J Psychosom Res 39:53–62
Charney DS, Heninger GR, Redmond DE Jr (1983) Yohimbine induced anxiety and increased noradrenergic function in humans: effects of diazepam and clonidine. Life Sci 33:19–29
Chester JA, Barrenha GD, Hughes ML, Keuneke KJ (2008) Age- and sex-dependent effects of footshock stress on subsequent alcohol drinking and acoustic startle behavior in mice selectively bred for high-alcohol preference. Alcohol Clin Exp Res 32:1782–1794
Choi S, Kellogg CK (1996) Adolescent development influences functional responsiveness of noradrenergic projections to the hypothalamus in male rats. Brain Res Dev Brain Res 94:144–151
Chung KK, Martinez M, Herbert J (2000) c-fos expression, behavioural, endocrine and autonomic responses to acute social stress in male rats after chronic restraint: modulation by serotonin. Neuroscience 95:453–463
Corrigall WA, Coen KM (1989) Nicotine maintains robust self-administration in rats on a limited-access schedule. Psychopharmacology (Berl) 99:473–478
Covington HE 3rd, Miczek KA (2001a) Repeated social-defeat stress, cocaine or morphine. Effects on behavioral sensitization and intravenous cocaine self-administration “binges”. Psychopharmacology (Berl) 158:388–398
Covington HE 3rd, Miczek KA (2001b) Repeated social-defeat stress, cocaine or morphine. Effects on behavioral sensitization and intravenous cocaine self-administration “binges”. Psychopharmacology 158:388–398
Covington HE 3rd, Miczek KA (2005) Intense cocaine self-administration after episodic social defeat stress, but not after aggressive behavior: dissociation from corticosterone activation. Psychopharmacology (Berl) 183:331–340
Covington HE 3rd, Kikusui T, Goodhue J, Nikulina EM, Hammer RP Jr, Miczek KA (2005) Brief social defeat stress: long lasting effects on cocaine taking during a binge and zif268 mRNA expression in the amygdala and prefrontal cortex. Neuropsychopharmacology 30:310–321
Cruz FC, Quadros IM, Hogenelst K, Planeta CS, Miczek KA (2011) Social defeat stress in rats: escalation of cocaine and “speedball” binge self-administration, but not heroin. Psychopharmacology (Berl) 215:165–175
Darnaudery M, Louvart H, Defrance L, Leonhardt M, Morley-Fletcher S, Gruber SH, Galietta G, Mathe AA, Maccari S (2007) Impact of an intense stress on ethanol consumption in female rats characterized by their pre-stress preference: modulation by prenatal stress. Brain Res 1131:181–186
Davis M, Redmond DE Jr, Baraban JM (1979) Noradrenergic agonists and antagonists: effects on conditioned fear as measured by the potentiated startle paradigm. Psychopharmacology (Berl) 65:111–118
Dayas CV, Martin-Fardon R, Thorsell A, Weiss F (2004) Chronic footshock, but not a physiological stressor, suppresses the alcohol deprivation effect in dependent rats. Alcohol Alcohol 39:190–196
Dazzi L, Serra M, Spiga F, Pisu MG, Jentsch JD, Biggio G (2001) Prevention of the stress-induced increase in frontal cortical dopamine efflux of freely moving rats by long-term treatment with antidepressant drugs. Eur Neuropsychopharmacol 11:343–349
DiFranza JR, Savageau JA, Rigotti NA, Ockene JK, McNeill AD, Coleman M, Wood C (2004) Trait anxiety and nicotine dependence in adolescents: a report from the DANDY study. Addict Behav 29:911–919
Donny EC, Caggiula AR, Mielke MM, Booth S, Gharib MA, Hoffman A, Maldovan V, Shupenko C, McCallum SE (1999) Nicotine self-administration in rats on a progressive ratio schedule of reinforcement. Psychopharmacology (Berl) 147:135–142
Feltenstein MW, See RE (2006) Potentiation of cue-induced reinstatement of cocaine-seeking in rats by the anxiogenic drug yohimbine. Behav Brain Res 174:1–8
Feltenstein MW, Ghee SM, See RE (2012) Nicotine self-administration and reinstatement of nicotine-seeking in male and female rats. Drug Alcohol Depend 121:240–246
Funk D, Vohra S, Le AD (2004) Influence of stressors on the rewarding effects of alcohol in Wistar rats: studies with alcohol deprivation and place conditioning. Psychopharmacology (Berl) 176:82–87
Funk D, Harding S, Juzytsch W, Le AD (2005) Effects of unconditioned and conditioned social defeat on alcohol self-administration and reinstatement of alcohol seeking in rats. Psychopharmacology (Berl) 183:341–349
Funk D, Li Z, Le AD (2006) Effects of environmental and pharmacological stressors on c-fos and corticotropin-releasing factor mRNA in rat brain: relationship to the reinstatement of alcohol seeking. Neuroscience 138:235–243
Funk CK, Zorrilla EP, Lee MJ, Rice KC, Koob GF (2007) Corticotropin-releasing factor 1 antagonists selectively reduce ethanol self-administration in ethanol-dependent rats. Biol Psychiatry 61:78–86
George O, Ghozland S, Azar MR, Cottone P, Zorrilla EP, Parsons LH, O’Dell LE, Richardson HN, Koob GF (2007) CRF-CRF1 system activation mediates withdrawal-induced increases in nicotine self-administration in nicotine-dependent rats. Proc Natl Acad Sci U S A 104:17198–17203
Ghitza UE, Gray SM, Epstein DH, Rice KC, Shaham Y (2006) The anxiogenic drug yohimbine reinstates palatable food seeking in a rat relapse model: a role of CRF1 receptors. Neuropsychopharmacology 31:2188–2196
Gilpin NW (2012) Corticotropin-releasing factor (CRF) and neuropeptide Y (NPY): effects on inhibitory transmission in central amygdala, and anxiety- & alcohol-related behaviors. Alcohol 46:329–337
Goeders NE, Guerin GF (1994) Non-contingent electric footshock facilitates the acquisition of intravenous cocaine self-administration in rats. Psychopharmacology (Berl) 114:63–70
Gozzi A, Lepore S, Vicentini E, Merlo-Pich E, Bifone A (2013) Differential effect of orexin-1 and CRF-1 antagonism on stress circuits: a fMRI study in the rat with the pharmacological stressor yohimbine. Neuropsychopharmacology 38:2120–2130
Ho AK, Hoffman DB, Gershon S, Loh HH (1971) Distribution and metabolism of tritiated yohimbine in mice. Arch Int Pharmacodyn Ther 194:304–315
Holmberg G, Gershon S (1961) Autonomic and psychic effects of yohimbine hydrochloride. Psychopharmacologia 2:93–106
Kabbaj M, Norton CS, Kollack-Walker S, Watson SJ, Robinson TE, Akil H (2001) Social defeat alters the acquisition of cocaine self-administration in rats: role of individual differences in cocaine-taking behavior. Psychopharmacology (Berl) 158:382–387
Kenny PJ, Markou A (2001) Neurobiology of the nicotine withdrawal syndrome. Pharmacol Biochem Behav 70:531–549
Lang WJ, Gershon S (1963) Effects of psychoactive drugs on yohimbine induced responses in conscious dogs. A proposed screening procedure for anti-anxiety agents. Arch Int Pharmacodyn Ther 142:457–472
Le A, Shaham Y (2002) Neurobiology of relapse to alcohol in rats. Pharmacol Ther 94:137–156
Le AD, Quan B, Juzystch W, Fletcher PJ, Joharchi N, Shaham Y (1998) Reinstatement of alcohol-seeking by priming injections of alcohol and exposure to stress in rats. Psychopharmacology 135:169–174
Le AD, Harding S, Juzytsch W, Funk D, Shaham Y (2005) Role of alpha-2 adrenoceptors in stress-induced reinstatement of alcohol seeking and alcohol self-administration in rats. Psychopharmacology (Berl) 179:366–373
Le AD, Funk D, Juzytsch W, Coen K, Navarre BM, Cifani C, Shaham Y (2011) Effect of prazosin and guanfacine on stress-induced reinstatement of alcohol and food seeking in rats. Psychopharmacology (Berl) 218:89–99
Leao RM, Cruz FC, Planeta CS (2009) Exposure to acute restraint stress reinstates nicotine-induced place preference in rats. Behav Pharmacol 20:109–113
Li S, Zou S, Coen K, Funk D, Shram MJ, Le AD (2012) Sex differences in yohimbine-induced increases in the reinforcing efficacy of nicotine in adolescent rats. Addict Biol. doi:10.1111/j.1369-1600.2012.00473.x
Logrip ML, Zorrilla EP (2012) Stress history increases alcohol intake in relapse: relation to phosphodiesterase 10A. Addict Biol 17:920–933
Mantsch JR, Katz ES (2007) Elevation of glucocorticoids is necessary but not sufficient for the escalation of cocaine self-administration by chronic electric footshock stress in rats. Neuropsychopharmacology 32:367–376
Marinelli PW, Funk D, Juzytsch W, Harding S, Rice KC, Shaham Y, Le AD (2007) The CRF1 receptor antagonist antalarmin attenuates yohimbine-induced increases in operant alcohol self-administration and reinstatement of alcohol seeking in rats. Psychopharmacology (Berl) 195:345–355
Miczek KA, Covington HE 3rd, Nikulina EM Jr, Hammer RP (2004) Aggression and defeat: persistent effects on cocaine self-administration and gene expression in peptidergic and aminergic mesocorticolimbic circuits. Neurosci Biobehav Rev 27:787–802
Miczek KA, Yap JJ, Covington HE 3rd (2008) Social stress, therapeutics and drug abuse: preclinical models of escalated and depressed intake. Pharmacol Ther 120:102–128
Millan MJ, Newman-Tancredi A, Audinot V, Cussac D, Lejeune F, Nicolas JP, Coge F, Galizzi JP, Boutin JA, Rivet JM, Dekeyne A, Gobert A (2000) Agonist and antagonist actions of yohimbine as compared to fluparoxan at alpha(2)-adrenergic receptors (AR)s, serotonin (5-HT)(1A), 5-HT(1B), 5-HT(1D) and dopamine D(2) and D(3) receptors. Significance for the modulation of frontocortical monoaminergic transmission and depressive states. Synapse 35:79–95
Nair SG, Adams-Deutsch T, Epstein DH, Shaham Y (2009) The neuropharmacology of relapse to food seeking: methodology, main findings, and comparison with relapse to drug seeking. Prog Neurobiol 89:18–45
Novak CM, Parfitt DB, Sisk CL, Smale L (2007) Associations between behavior, hormones, and Fos responses to novelty differ in pre- and post-pubertal grass rats. Physiol Behav 90:125–132
Pomerleau OF, Pomerleau CS (1991) Research on stress and smoking: progress and problems. Br J Addict 86:599–603
SAMHSA (2011) Results from the 2011 National Survey on Drug Use and Health: summary of national findings. Substance Abuse and Mental Health Services Administration, Rockville
Shaham Y, Stewart J (1994) Exposure to mild stress enhances the reinforcing efficacy of intravenous heroin self-administration in rats. Psychopharmacology (Berl) 114:523–527
Shaham Y, Stewart J (1995) Stress reinstates heroin self-administration behavior in drug-free animals: an effect mimicking heroin, not withdrawal. Psychopharmacology 119:334–341
Shaham Y, Klein LC, Alvares K, Grunberg NE (1993) Effect of stress on oral fentanyl consumption in rats in an operant self-administration paradigm. Pharmacol Biochem Behav 46:315–322
Shaham Y, Erb S, Stewart J (2000) Stress-induced relapse to heroin and cocaine seeking in rats: a review. Brain Res Brain Res Rev 33:13–33
Shalev U, Erb S, Shaham Y (2010) Role of CRF and other neuropeptides in stress-induced reinstatement of drug seeking. Brain Res 1314:15–28
Shepard JD, Bossert JM, Liu SY, Shaham Y (2004) The anxiogenic drug yohimbine reinstates methamphetamine seeking in a rat model of drug relapse. Biol Psychiatry 55:1082–1089
Shram MJ, Funk D, Li Z, Le AD (2006) Periadolescent and adult rats respond differently in tests measuring the rewarding and aversive effects of nicotine. Psychopharmacology (Berl) 186:201–208
Shram MJ, Funk D, Li Z, Le AD (2008) Nicotine self-administration, extinction responding and reinstatement in adolescent and adult male rats: evidence against a biological vulnerability to nicotine addiction during adolescence. Neuropsychopharmacology 33:739–748
Slawecki CJ (2005) Comparison of anxiety-like behavior in adolescent and adult Sprague–Dawley rats. Behav Neurosci 119:1477–1483
Slawecki CJ, Roth J (2004) Comparison of the onset of hypoactivity and anxiety-like behavior during alcohol withdrawal in adolescent and adult rats. Alcohol Clin Exp Res 28:598–607
Tidey JW, Miczek KA (1997) Acquisition of cocaine self-administration after social stress: role of accumbens dopamine. Psychopharmacology 130:203–212
Tybout A, Sternthal B, Keppel G, Verducci J, Meyers-Levy J, Barnes J, Maxwell S, Allenby G, Gupta S, Steenkamp J (2001) Analysis of variance. J Consum Psychol 10:5–35
Valdez GR, Roberts AJ, Chan K, Davis H, Brennan M, Zorrilla EP, Koob GF (2002) Increased ethanol self-administration and anxiety-like behavior during acute ethanol withdrawal and protracted abstinence: regulation by corticotropin-releasing factor. Alcohol Clin Exp Res 26:1494–1501
van Erp AM, Miczek KA (2001) Persistent suppression of ethanol self-administration by brief social stress in rats and increased startle response as index of withdrawal. Physiol Behav 73:301–311
van Erp AM, Tachi N, Miczek KA (2001) Short or continuous social stress: suppression of continuously available ethanol intake in subordinate rats. Behav Pharmacol 12:335–342
Vazquez DM (1998) Stress and the developing limbic-hypothalamic-pituitary-adrenal axis. Psychoneuroendocrinology 23:663–700
Vengeliene V, Siegmund S, Singer MV, Sinclair JD, Li TK, Spanagel R (2003) A comparative study on alcohol-preferring rat lines: effects of deprivation and stress phases on voluntary alcohol intake. Alcohol Clin Exp Res 27:1048–1054
Walker BM (2012) Conceptualizing withdrawal-induced escalation of alcohol self-administration as a learned, plasticity-dependent process. Alcohol 46:339–348
Weiss JW, Palmer PH, Chou CP, Mouttapa M, Johnson CA (2008) Association between psychological factors and adolescent smoking in seven cities in China. Int J Behav Med 15:149–156
Yamada H, Bruijnzeel AW (2011) Stimulation of alpha2-adrenergic receptors in the central nucleus of the amygdala attenuates stress-induced reinstatement of nicotine seeking in rats. Neuropharmacology 60:303–311
Zhou Y, Leri F, Grella SL, Aldrich JV, Kreek MJ (2013) Involvement of dynorphin and kappa opioid receptor in yohimbine-induced reinstatement of heroin seeking in rats. Synapse 67:358–361
Zislis G, Desai TV, Prado M, Shah HP, Bruijnzeel AW (2007) Effects of the CRF receptor antagonist d-Phe CRF((12–41)) and the alpha2-adrenergic receptor agonist clonidine on stress-induced reinstatement of nicotine-seeking behavior in rats. Neuropharmacology 53:958–966
Acknowledgments
This work was supported by a grant from the Canadian Psychiatric Research Foundation to ADL. We would like to thank Dr. Yavin Shaham of the National Institute on Drug Abuse for his valuable comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zou, S., Funk, D., Shram, M.J. et al. Effects of stressors on the reinforcing efficacy of nicotine in adolescent and adult rats. Psychopharmacology 231, 1601–1614 (2014). https://doi.org/10.1007/s00213-013-3314-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-013-3314-3