Abstract
Rationale
Tobacco use is linked to cerebral atrophy and reduced cognitive performance in later life. However, smoking-related long-term effects on brain function remain largely uncertain. Previous studies suggest that nicotine affects serotonergic signaling, and the intensity dependence (alias loudness dependence) of the auditory evoked N1-P2 potential has been proposed as a marker of serotonergic neurotransmission.
Objective
In the present study, we assesed the effects of chronic smoking on amplitude and intensity dependence of the auditory evoked N1-P2 potential.
Methods
Subjects underwent a 15-min intensity dependence of auditory evoked potentials (IAEP) paradigm. From N = 1739 eligible subjects (40–79 years), we systematically matched current smokers, ex-smokers, and never-smokers by sex, age, alcohol and caffeine consumption, and socioeconomic status. Between-group differences and potential dose-dependencies were evaluated.
Results
Analyses revealed higher N1-P2 amplitudes and intensity dependencies in never-smokers relative to ex- and current smokers, with ex-smokers exhibiting intermediate intensity dependencies. Moreover, we observed pack years and number of cigarettes consumed per day to be inversely correlated with amplitudes in current smokers.
Conclusions
According to the IAEP serotonin hypothesis, our results suggest serotonin activity to be highest in current smokers, intermediate in ex-smokers, and lowest in never-smokers. To our knowledge, the present study is the first providing evidence for a dose-dependent reduction in N1-P2 amplitudes. Further, we extend prior research by showing reduced amplitudes and intensity dependencies in ex-smokers even 25 years, on average, after cessation. While we can rule out several smoking-related confounders to bias observed associations, causal inferences remain to be established by future longitudinal studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tobacco use is linked to numerous preventable diseases, resulting in considerable public health expenditures and about 100,000 deaths per annum in the UK alone (Allender et al. 2009). Beyond negative vascular and respiratory health outcomes, smokers show poorer cognitive performance in later life and exhibit an increased risk for dementia (Chang et al. 2014, Mons et al. 2013). Nevertheless, discrete effects of chronic smoking on physiological brain function remain largely uncertain.
Prior imaging studies point to a link between chronic smoking and reduced cortical volume, density, and thickness, aside from higher atrophy rates in widespread brain regions (Almeida et al. 2008, Durazzo et al. 2012, Fritz et al. 2014, Karama et al. 2015). Functional approaches suggest that smokers exhibit a reduced default mode and executive control network connectivity (Weiland et al. 2015) and a lower cerebral perfusion (i.e., blood flow) in the orbitofrontal cortex, inferior parietal lobules, superior temporal gyri, and cingulate gyrus (Durazzo et al. 2015). Due to their dependence on hemodynamics, a large proportion of currently applied techniques are rather restricted in rendering rapid information processing visible. Recordings of electroencephalic activity, on the other hand, enable direct assessment of neural mechanisms with high temporal resolution. While acute effects of smoking on various electrophysiological potentials have been described (Pritchard et al. 2004), evidence for long-term effects is scarce.
The intensity dependence (also referred to as loudness dependence) of the auditory evoked N1-P2 component has been suggested as an indicator of central serotonergic neurotransmission, with weaker intensity dependencies hypothesized to reflect higher serotonin activity (Hegerl et al. 2001, Hegerl and Juckel 1993). This hypothesis was validated in experimental animal studies (Juckel et al. 1997, Juckel et al. 1999, Manjarrez et al. 2005, Wutzler et al. 2008), while several studies on patients with putative serotonergic dysfunction provided further indirect evidence. For instance, an enhanced N1-P2 intensity dependence was reported in ecstasy users (Daumann et al. 2006, Tuchtenhagen et al. 2000) and in patients with migraine (Siniatchkin et al. 2000). A reduced N1-P2 intensity dependence, on the other hand, was shown in schizophrenia (see Juckel 2015). Further, intensity dependencies were utilized to predict responses on drugs that influence the serotonin system, such as lithium and selective serotonin reuptake inhibitors (Gallinat et al. 2000, Juckel et al. 2004, Juckel et al. 2007, Lee et al. 2005, Linka et al. 2004, Linka et al. 2005, Mulert et al. 2007). By analogy to intensity dependencies, an elevated serotonergic function has also been linked to weaker auditory evoked amplitudes (Ehlers et al. 1991, O’Connor et al. 1992, Rowan et al. 1988).
Notably, the N1 and P2’s intracerebral origins, i.e., the superior temporal gyri (Crowley and Colrain 2004), have been associated with smoking-related morphological and functional alterations (Durazzo et al. 2015, Karama et al. 2015). In addition, nicotine was found to impact serotonergic signaling (Benwell et al. 1990, Hernandez-Lopez et al. 2013, Malone et al. 2003, Seth et al. 2002). Consequently, two studies previously reported a lower N1-P2 intensity dependence among current smokers relative to non-smokers (Gallinat et al. 2005, Min et al. 2012). However, both studies did not provide information about absolute N1-P2 amplitudes, nor they systematically controlled for confounders beyond sex and age. Further, non-smokers were not consistently subdivided into ex- and never-smokers, and sample sizes might have been too small to detect potential dose-dependent relationships.
On this basis, we sought to investigate the effects of smoking status on brain function by means of amplitude and intensity dependence of the cortical auditory evoked N1-P2 component in a sample providing enhanced power and the opportunity to systematically control for several major smoking-related confounders. Beyond this, we aimed to investigate potential dose-dependent relationships.
Methods and materials
Sample
The sample was drawn from the LIFE-Adult study (Loeffler et al. 2015), a population-based cohort study which aims to examine prevalences, genetic predispositions, and lifestyle factors of civilization diseases. The LIFE-Adult cohort comprises 10,000 randomly selected inhabitants of Leipzig, Germany (main age range 40–79 years). Of those, 2,718 subjects completed an EEG assessment and provided sufficient data to evaluate tobacco use, socioeconomic status, alcohol and caffeine consumption, and hearing threshold level. In the context of the present investigation, we did not include subjects with any current psychiatric disorder (according to a structured clinical interview for DSM-IV axis I disorders), any current intake of psychotropic medication, or any history of a major neurological disorder (leaving 1,974 subjects). Further, we did not include cigar, cigarillo, stogie and pipe smokers, or subjects with a hearing loss exceeding a moderate degree (>55 dB SPL). Never-smokers reported no 6-month history of five or more cigarettes a week. Ex- and current smokers reported a regular tobacco intake of at least one cigarette a day over a 1-year period. Current smokers were allowed to smoke ad libitum. Ex-smokers quit smoking at least 12 months ago. A resulting number of N = 1739 eligible subjects (40–79 years, 873 female) passed these criteria and subsequent EEG data quality checks (described below).
However, current, ex-, and never-smokers differed substantially concerning various potential confounders (see supplementary Table S1). To improve group comparability, we performed nearest neighbor matching using R-based SPSS extension bundle psmatching 3.04 (Thoemmes 2012). Propensity scores were calculated from a generalized additive model with relaxed assumptions. Age on assessment date, socioeconomic status, average amount of alcohol consumed daily during the past 12 months, and the amount of caffeine consumed prior to EEG served as covariates. Ex- and current smokers were additionally matched by age of smoking onset and number of cigarettes consumed daily. Exact matching was carried out for sex. Units out of common support were discarded. To avoid incomplete matches, a caliper (0.05 in size) was only used for 1:1 matching. First, we identified n = 544 never-smokers and n = 272 ex-smokers, respectively, matching n = 136 current smokers. Due to a substantial loss of power in detecting statistically relevant differences between never- and ex-smokers, we identified n = 468 never-smokers matching n = 468 ex-smokers in a second step. Table 1 provides detailed group characteristics of subsample 1 (never- and ex-smokers matched to current smokers) and the overlapping subsample 2 (never-smokers matched to ex-smokers; 57.5 % of subsample 2 subjects were also included in subsample 1 analyses).
Questionnaires and assessment of arousal
The assessment of tobacco use contained questions on ever- and current smoking, age of onset, duration and cessation, and the amount of intake of different tobacco products. Socioeconomic status was calculated from self-reported education, occupational status, and household income as described elsewhere (Lampert et al. 2013). Average amount of alcohol consumed daily during the past 12 months was calculated from self-reported amount and frequency of intake of different alcoholic beverages. If the amount was not reported but the associated frequency, or vice versa (2.2 %), the missing value was substituted by the median item response derived from responses of all other subjects with a congruent value in the associated item. Amount of caffeine consumed prior to EEG assessment was calculated from the self-reported amount of intake of different caffeinated beverages. Further, prior research suggests smoking to impact arousal (Evatt and Kassel 2010) and arousal to impact evoked potentials (Colrain and Campbell 2007). Therefore, arousal was assessed in advance using the German version of the Karolinska Sleepiness Scale (Åkerstedt and Gillberg 1990) and by applying a recently developed EEG- and EOG-based computer algorithm, i.e., the Vigilance Algorithm Leipzig (VIGALL) 2.0 (Hegerl and Hensch 2014, Sander et al. 2016), to preceding resting EEG recordings. Detailed information about procedure and parameters of the latter assessment are described elsewhere (Huang et al. 2015, Jawinski et al. 2015).
Physiological data collection and reduction
All procedures were carried out according to the Declaration of Helsinki and approved by the Ethics Committee of the University of Leipzig (263-2009-14122009). Subjects gave written informed consent and received an expense allowance. Subjects were seated in a chair in a sound-attenuated booth. Instructions and paradigm stimuli were presented binaurally via E-A-RTONE 3A Audiometric Insert Earphones (Aearo Company, Indianapolis, IN, USA) using Presentation software (Neurobehavioral Systems Inc., Albany, USA). Subjects were asked to avoid body movements, to relax, and to direct their gaze towards a self-chosen point in front of them. No attention instruction was given. The 15-min eyes-opened intensity dependence of auditory evoked potentials (IAEP) paradigm consisted of 450 pseudo-randomized 1000 Hz sinus tones (30 ms duration, 10 ms rise and fall) of five calibrated intensities (72, 78, 84, 90, 96 dB SPL). The interstimulus interval varied between 1600 and 2100 ms. Simultaneity of trigger and sound was verified according to Neurobehavioral Systems’ guidelines. EEGs were recorded against common average reference by 31 Ag/AgCl electrodes from standardized scalp sites (extended 10–20 systems) with an additional nose-tip electrode and AFz ground. Electroencephalic activity was amplified using a QuickAmp amplifier (Brain Products GmbH, Gilching, Germany) and sampled at 1000 Hz with a low-pass filter at 280 Hz. Impedances were kept below 10 kΩ. In addition, vertical and horizontal electrooculogram (EOG) was recorded for Gratton and Coles offline correction of eye movement artifacts.
Offline processing was performed using Brain Vision Analyzer 2.0 (Brain Products GmbH, Gilching, Germany). Recordings were filtered (30 Hz low-pass, 0.1 Hz high-pass) and re-referenced against the nose tip. Based on tone intensity markers, EEGs were segmented into epochs of 600 ms length including a pre-stimulus baseline interval of 200 ms. Epochs with a voltage exceeding ±50 μV at Cz were excluded. At least 30 artifact-free epochs in each tone intensity condition were required for averaging. The median number of averaged epochs was 81 (at 90 dB SPL) or 82 (at 72, 78, 84, 96 dB SPL), respectively. Following automatic detection of baseline-to-peak amplitudes for N1 (55–160 ms) and P2 (110–260 ms) at Cz, N1-P2 peak-to-peak amplitudes were calculated. Individual intensity dependence was calculated as linear slope of N1-P2 amplitudes across all tone intensities and, additionally, as median slope of N1-P2 amplitudes derived from all possible pairs of amplitudes across the five tone intensity conditions (Hensch et al. 2006, Hensch et al. 2008, Strobel et al. 2003). Subjects with amplitudes falling three interquartile range units below the first or above the third quartile of the ascending group distributions were defined as outliers (0.2 %) and excluded.
Statistical analyses
All analyses were conducted using SPSS Statistics 20 (2012; IBM corp.; Armonk, New York). Physiological data reliability was determined by means of split-half method within our large unmatched sample. To this end, N1-P2 amplitudes and slope parameters were derived from odd and even trials, respectively, and Spearman-Brown corrected rank correlations were calculated. Further, available data from a small supplementary sample enabled estimation of test-retest reliabilities (n = 15; age range at T1 66–74 years; 9 males; test-retest interval 1–3 years).
Group comparisons were conducted within both subsamples comprising matched subjects. We performed repeated-measures ANCOVAs with tone intensity as within- and smoking status as between-subjects factor. Sex and age were entered as covariates. Covariates were centered in advance (according to Van Breukelen and Van Dijk 2007). Additionally, we conducted univariate ANCOVAs with smoking status as independent and linear and median slopes, respectively, as dependent variable. Again, sex and age served as covariates. Within subsample 1, we performed contrast analyses. All analyses were repeated without covariates, and results are reported in case of decisively altered effects. Greenhouse-Geisser corrected degrees of freedom are reported where appropriate.
To determine potential dose-dependent relationships, we conducted partial Spearman correlations linking the number of cigarettes consumed per day and pack years, respectively, to N1-P2 amplitudes and slopes. Separate analyses were performed for current and ex-smokers. Effects of sex, age, average amount of alcohol consumed daily during the past 12 months, and the amount of caffeine consumed prior to EEG were partialled out. Analyses were repeated partialling out effects of sex and age only.
Results
Physiological data reliability
Spearman-Brown-corrected rank correlations revealed high odd-even reliabilities of N1-P2 amplitudes (0.88–0.98) and moderate odd-even reliabilities of linear (0.77) and median slope (0.75). Furthermore, we observed moderate to high test-retest reliabilities for N1-P2 amplitudes (0.80–0.95) and moderate to low test-retest reliabilities of linear (0.54) and median slope (0.36) after an interval of 1 to 3 years. Detailed results are shown in Table 2.
Group comparisons
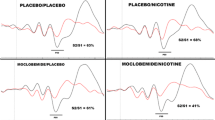
Within subsample 1 (never- and ex-smokers matched to current smokers), repeated-measures ANCOVAs revealed a significant main effect of tone intensity (F 2.4,2311.4 = 775.485, p = 2E-300, η p 2 = 0.450), with higher tone intensities eliciting larger N1-P2 amplitudes (see Fig. 1 for grand averages). Further, we observed a significant main effect of sex (F 1,947 = 119.095, p = 3E-26, η p 2 = 0.112) and a sex × tone intensity interaction (F 2.4,2311.4 = 10.373, p = 7E-6, η p 2 = 0.011), with women showing higher N1-P2 amplitudes and steeper slopes. Moreover, younger subjects exhibited higher N1-P2 amplitudes and steeper slopes, underpinned by a significant main effect of age (F 1,947 = 5.014, p = 0.025, η p 2 = 0.005) and an age × tone intensity interaction (F 2.4,2129.1 = 31.246, p = 1E-16, η p 2 = 0.032).
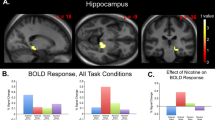
Further, analyses revealed a significant main effect of smoking status, with never-smokers displaying highest N1-P2 amplitudes followed by ex- and current smokers (F 2,947 = 4.679, p = 0.010, η p 2 = 0.010). Contrast analyses showed a significant difference between never- and current smokers (p = 0.012) and never- and ex-smokers (p = 0.019) in N1-P2 amplitudes, whereas ex- and current smokers did not significantly differ (p = 0.534). Moreover, analyses provided evidence for a smoking status × tone intensity interaction (F 4.9,2311.4 = 5.913, p = 2E-5, η p 2 = 0.012), suggesting differential intensity dependencies among current, ex-, and never-smokers. Figure 2a indicates the steepest increase of N1-P2 amplitudes among never-smokers, with ex-smokers showing an intermediate phenotype and current smokers showing the shallowest increase.
Estimated marginal means (covariates: sex, age) and standard errors of N1-P2 peak-to-peak amplitudes at Cz (nose reference) across five tone intensities stratified by smoking status and subsample. a Subsample 1—544 never-smokers and 272 ex-smokers were matched to 136 current smokers. b Subsample 2—468 never-smokers were matched to 468 ex-smokers
Statistical differences in intensity dependencies were further analyzed using slope parameters. In this respect, univariate ANCOVAs revealed significant covariate effects on linear slope (sex F 1,947 = 15.852, p = 7E-5, η p 2 = 0.016; age F 1,947 = 51.757, p = 1E-12, η p 2 = 0.052) and median slope (sex F 1,947 = 17.524, p = 3E-5, η p 2 = 0.018; age F 1,947 = 47.784, p = 9E-12, η p 2 = 0.048), with women and younger subjects exhibiting steeper slopes. In line with repeated-measures analyses, we observed a significant effect of smoking status on linear (F 2,947 = 9.234, p = 1E-4, η p 2 = 0.019) and median slope (F 2,947 = 8.606, p = 2E-4, η p 2 = 0.018), with never-smokers exhibiting the steepest slopes followed by ex- and never-smokers in approximately equally sized successive intervals. Contrast analyses revealed a significant difference between never- and current smokers (linear slope p = 4E-5; median slope p = 9E-5) and never- and ex-smokers (linear slope p = 0.027; median slope p = 0.021), whereas the difference between ex- and current smokers only partly surpassed the threshold of significance (linear slope p = 0.027; median slope p = 0.051). Repeating analyses without covariates did not decisively alter association results, except for contrasts between never- and ex-smokers, suggesting no differential intensity dependencies (linear slope p = 0.091; median slope p = 0.071).
Differences between never- and ex-smokers were elucidated with enhanced power in subsample 2 (never-smokers matched to ex-smokers). Repeated-measures analyses revealed a significant main effect of smoking status (F 1,932 = 11.693, p = 0.001, η p 2 = 0.012), with never-smokers exhibiting higher N1-P2 amplitudes (see Fig. 2b). Moreover, never-smokers showed a steeper increase of N1-P2 amplitudes across tone intensities, underpinned by a significant smoking status × tone intensity interaction (F 2.5,2347.7 = 6.669, p = 4E-4, η p 2 = 0.007). Additional supportive evidence for differential intensity dependencies was provided by univariate ANCOVAs, showing significantly steeper slopes for never-smokers (linear slope F 1,932 = 9.531, p = 0.002, η p 2 = 0.010; median slope F 1,932 = 9.850, p = 0.002, η p 2 = 0.010).
Dose-dependent relationships
Results of correlation analyses are presented in Table 2. In current smokers, the partial Spearman correlations provided evidence for cigarettes consumed per day and pack years to be associated with reduced N1-P2 amplitudes at 72, 78, 84, and 90 dB SPL and when averaging N1-P2 amplitudes across all tone intensities (all p ≤ 0.024). In ex-smokers, we found a trend correlation between cigarettes consumed per day and reduced amplitudes at 96 dB SPL (p = 0.054). Although currently consumed cigarettes per day or pack years did not appear to be associated with slope parameters (all p ≥ 0.587), analyses showed a significant link between formerly consumed cigarettes per day and reduced slopes (all p ≤ 0.035). Association results did not decisively change by partialling out effects of sex and age only.
Discussion
The aim of the present study was to further elucidate the effects of chronic smoking on brain function by comparing systematically matched groups of current, ex-, and never-smokers in amplitude and intensity dependence of the auditory evoked N1-P2 component. Analyses revealed higher N1-P2 amplitudes and intensity dependencies in never-smokers compared to ex- and current smokers. Ex-smokers showed intermediate intensity dependencies concerning linear slope analyses. Notably, we observed pack years and cigarettes consumed per day, respectively, to be inversely correlated with N1-P2 amplitudes in current smokers with some indications in ex-smokers. Inconsistent evidence was found for a potential link between dose and N1-P2 intensity dependencies.
Keeping abreast of the methodological progress in group matching, we took into account several major confounders obscuring comparisons of naturally occurring, non-randomized groups of smokers and non-smokers. Differences in alcohol and caffeine consumption, socioeconomic status, or even sex and age have previously often been neglected or inadequately dealt with, e.g., by entering confounding variables as covariates in ANCOVAs with intent to control for evident between-group imbalances (Miller and Chapman 2001). In contrast, we identified statistical siblings, who differed in smoking status but were similar in the abovementioned characteristics. Beyond this, we systematically ensured comparability of current and ex-smokers concerning age of onset and cigarettes consumed per day. Groups were also comparable regarding arousal prior to assessment and hearing threshold level. Consequently, a number of major confounders can be ruled out to bias observed associations.
Regarding group comparisons, our findings partly contradict the results of Gallinat et al. (2005), who reported statistically equal intensity dependencies in never- and ex-smokers. Here, we demonstrated reduced amplitudes and intensity dependencies in ex-smokers who quit smoking, on average, about 25 years ago. This disagreement might be traced back to the higher power of the present study. Furthermore, our ex-smokers had their smoking cessation about 10 years later in life, indicating a prolonged use of tobacco, which in turn might have led to cerebral alterations more clearly differentiating from those of never-smokers. Interestingly, Karama et al. (2015) analyzed structural MRI data from a sample of ex-smokers with an average number of 30 pack years and revealed an estimated complete recovery from smoking-related cortical thinning 25 years after smoking cessation. Although our ex-smokers consumed not even half of this amount of cigarettes, alterations of the N1-P2 component were still evident. In sum, while our findings on differential N1-P2 amplitudes and intensity dependencies in never- vs. current smokers correspond to previous findings, novel evidence arises from comparisons of never- and ex-smokers, suggesting differences in brain function measurable even decades after cessation.
Present correlation analyses not only provide further support for an association of chronic smoking and reduced N1-P2 amplitudes but also suggest amplitudes to be dose-dependent. By analogy, based on a total number of 4,150 subjects, a recent systematic review suggests reduced P3 amplitudes in chronic smokers with possibly underlying dose dependencies (Hedges and Bennett 2014). Intuitively, an amplitude reduction of cortical potentials is well in agreement with atrophic cortices and impaired cognitive function reported in elderly smokers (Karama et al. 2015, Mons et al. 2013). In this respect, Edgar et al. (2012) observed positive correlations between cortical thickness, cognitive function, and strength of M1, i.e., the magnetic equivalent to N1. In line with these prior findings, correlations between amount of cigarettes consumed and N1-P2 amplitudes appear to add one further piece to the puzzle of broad and potentially interlinked brain alterations in chronic smokers.
Although correlation analyses revealed convincing results regarding potentially dose-dependent amplitudes, we obtained inconsistent evidence for a link between dose and intensity dependencies: Intensity dependencies were inversely linked to cigarettes consumed per day in former smokers without any indications in current smokers. Moreover, this association was not supported concerning pack years. Assuming the observed correlation in ex-smokers for cigarettes consumed per day to be true in current smokers with rho = −0.1, the lack of evidence among current smokers presumably relies on the analysis’ power scarcely exceeding 20 %. Beyond this, current smokers were allowed to smoke ad libitum and acute smoking effects may counteract or even cancel out effects of chronic smoking. In fact, some previous studies reported acute smoking to enhance N1-P2 amplitudes (Pritchard et al. 2004), and these opposing effects might have especially obscured amplitude correlations at 96 dB among our current smokers. Since amplitudes at 96 dB particularly determine calculated intensity dependencies (with rho ≥ 0.71) relative to amplitudes at lower tone intensities (0.16 ≤ rho ≤ 0.59), the lack of correlation between dose and intensity dependence in current smokers might be a consequence of acute smoking effects. However, subjects were abstinent for at least 60 to 90 min prior to the IAEP paradigm. Therefore, rather sub-acute smoking effects or even emerging effects of withdrawal might have obscured associations. Due to its inconsistency, the link between cigarettes consumed per day and intensity dependence should be interpreted with caution.
In light of studies investigating the N1-P2 intensity dependence as a marker of central serotonergic signaling (Hegerl et al. 2001, Hegerl and Juckel 1993, Juckel et al. 1997), our results suggest central serotonin activity to be highest in current smokers, intermediate in ex-smokers, and lowest in never-smokers. This finding is well in agreement with reported effects of smoking on serotonergic signaling (Benwell et al. 1990, Hernandez-Lopez et al. 2013, Malone et al. 2003, Seth et al. 2002). Consequently, smoking should be taken into account in clinical studies comparing N1-P2 intensity dependencies among psychiatric patients and healthy controls (e.g., Park et al. 2015, Wyss et al. 2013), with psychiatric patients exhibiting considerably higher prevalence rates of smoking (Smith et al. 2014). In the same vein, smoking as a confounder should be considered when investigating personality traits such as sensation seeking or hypomanic personality, which have similarly been associated with both N1-P2 intensity dependence and smoking (Hensch et al. 2007, Oreland et al. 2002).
Up to this point, it remains unclear whether effects of chronic smoking on the N1-P2 component arise from alterations in N1, P2, or both components. In view of grand averages (see Fig. 1), both components might be involved. Supplementary Tables S2 and S3 summarize reliabilities and effects of smoking status and dose on separate baseline-to-peak components. Effects appeared more consistent for the N1 relative to the P2 component. In general, presented data suggest lower reliabilities and effect consistencies of separate relative to peak-to-peak amplitudes. On this basis, we suppose that the N1-P2 component is the better-suited marker for detecting effects of chronic smoking. Differential component sensitivities towards smoking effects might be addressed by future studies.
Although we observed smoking status to impact the N1-P2 component with low type I error rates, effect sizes appeared generally small. In particular, variance explained by smoking status ranged between 0.7 and 1.9 %, while the overlap of variance in pack years and variance in N1-P2 amplitude approximated 5.8 % in current smokers. Several reasons may account for rather small effect sizes. First, with an average number of ten cigarettes consumed per day, current and ex-smokers were no excessive smokers. Second, the selection of healthy elderly smokers might have induced some bias towards those surviving smokers with the slightest smoking-related morbidities. Third, smoking history data were self-reported and recall errors likely caused some noise especially in ex-smokers, half of which had their smoking cessation more than 25 years ago. Fourth, non-invasive assessments of cortical potentials are generally overlaid with some noise, because recorded voltages depend on individual skull and scalp thickness (Chauveau et al. 2004). Taken together, potentially underestimated effect sizes should be considered in view of the abovementioned sample characteristics and due to some degree of inaccuracy in both self-report and physiological measures. Notably, observed effect sizes of smoking status on the N1-P2 component are still comparable to previous reports (e.g., η p 2 = 0.040; calculated from F 2,172 = 3.556; Gallinat et al. 2005).
One additional considerable limitation of the present study is the cross-sectional study design, which does not enable causal inferences. For instance, previous investigations found a reduction in P3 at age 17 to predict the occurrence of substance use disorders at age 20 (Iacono et al. 2002). To clarify the causal nature of the present results, either longitudinal or preferably randomized controlled trials (e.g., within the framework of smoking cessation therapies) are needed.
Conclusion
We extend current evidence on brain function in chronic smokers by demonstrating smoking-related reductions in amplitude and intensity dependence of the cortical auditory evoked N1-P2 component. According to the IAEP serotonin hypothesis, our results suggest serotonin activity to be highest in current smokers, intermediate in ex-smokers, and lowest in never-smokers. For the first time, the present study provides evidence for a potentially dose-dependent reduction in N1-P2 amplitudes. Moreover, we observed reduced amplitudes and intensity dependencies in ex-smokers relative to never-smokers even 25 years, on average, after cessation. While we can rule out several smoking-related confounders to bias observed associations, causal inferences remain to be established by future longitudinal studies.
Supplementary materials are available at the Psychopharmacology (Berl.) website.
References
Åkerstedt T, Gillberg M (1990) Subjective and objective sleepiness in the active individual. Int J Neurosci 52(1-2):29–37. doi:10.3109/00207459008994241
Allender S, Balakrishnan R, Scarborough P, Webster P, Rayner M (2009) The burden of smoking-related ill health in the UK. Tob Control 18(4):262–267. doi:10.1136/tc.2008.026294
Almeida OP, Garrido GJ, Lautenschlager NT, Hulse GK, Jamrozik K, Flicker L (2008) Smoking is associated with reduced cortical regional gray matter density in brain regions associated with incipient Alzheimer disease. Am J Geriatr Psychiatry 16(1):92–98. doi:10.1097/JGP.0b013e318157cad2
Benwell ME, Balfour DJ, Anderson JM (1990) Smoking-associated changes in the serotonergic systems of discrete regions of human brain. Psychopharmacology (Berl) 102(1):68–72
Chang RC, Ho Y, Wong S, Gentleman SM, Ng H (2014) Neuropathology of cigarette smoking. Acta Neuropathol 127(1):53–69. doi:10.1007/s00401-013-1210-x
Chauveau N, Franceries X, Doyon B, Rigaud B, Morucci JP, Celsis P (2004) Effects of skull thickness, anisotropy, and inhomogeneity on forward EEG/ERP computations using a spherical three-dimensional resistor mesh model. Hum Brain Mapp 21(2):86–97. doi:10.1002/hbm.10152
Colrain IM, Campbell KB (2007) The use of evoked potentials in sleep research. Sleep Med Rev 11(4):277–293. doi:10.1016/j.smrv.2007.05.001
Crowley KE, Colrain IM (2004) A review of the evidence for P2 being an independent component process: age, sleep and modality. Clin Neurophysiol 115(4):732–744. doi:10.1016/j.clinph.2003.11.021
Daumann J, Till B, Fischermann T, Rezk M, Gouzoulis-Mayfrank E (2006) Intensity dependence of auditory evoked dipole source activity in polydrug ecstasy users: evidence from an 18 months longitudinal study. J Psychopharmacol (Oxford) 20(2):236–244. doi:10.1177/0269881106059733
Durazzo TC, Insel PS, Weiner MW (2012) Greater regional brain atrophy rate in healthy elderly subjects with a history of cigarette smoking. Alzheimers Dement 8(6):513–519. doi:10.1016/j.jalz.2011.10.006
Durazzo TC, Meyerhoff DJ, Murray DE (2015) Comparison of regional brain perfusion levels in chronically smoking and non-smoking adults. Int J Environ Res Public Health 12(7):8198–8213. doi:10.3390/ijerph120708198
Edgar JC, Hunter MA, Huang M, Smith AK, Chen Y, Sadek J, Lu BY, Miller GA, Cañive JM (2012) Temporal and frontal cortical thickness associations with M100 auditory activity and attention in healthy controls and individuals with schizophrenia. Schizophr Res 140(1-3):250–257. doi:10.1016/j.schres.2012.06.009
Ehlers CL, Wall TL, Chaplin RI (1991) Long latency event-related potentials in rats: effects of dopaminergic and serotonergic depletions. Pharmacol Biochem Behav 38(4):789–793
Evatt DP, Kassel JD (2010) Smoking, arousal, and affect: the role of anxiety sensitivity. J Anxiety Disord 24(1):114–123. doi:10.1016/j.janxdis.2009.09.006
Fritz H, Wittfeld K, Schmidt CO, Domin M, Grabe HJ, Hegenscheid K, Hosten N, Lotze M (2014) Current smoking and reduced gray matter volume—a voxel-based morphometry study. Neuropsychopharmacology 39(11):2594–2600. doi:10.1038/npp.2014.112
Gallinat J, Bottlender R, Juckel G, Munke-Puchner A, Stotz G, Kuss HJ, Mavrogiorgou P, Hegerl U (2000) The loudness dependency of the auditory evoked N1/P2-component as a predictor of the acute SSRI response in depression. Psychopharmacology (Berl) 148(4):404–411
Gallinat J, Kunz D, Lang UE, Kalus P, Juckel G, Eggers J, Mahlberg R, Staedtgen M, Wernicke C, Rommelspacher H, Smolka MN (2005) Serotonergic effects of smoking are independent from the human serotonin transporter gene promoter polymorphism: evidence from auditory cortical stimulus processing. Pharmacopsychiatry 38(4):158–160. doi:10.1055/s-2005-871237
Hedges D, Bennett DP (2014) Cigarette smoking and p300 amplitude in adults: a systematic review. Nicotine Tob Res 16(9):1157–1166. doi:10.1093/ntr/ntu083
Hegerl U, Gallinat J, Juckel G (2001) Event-related potentials: do they reflect central serotonergic neurotransmission and do they predict clinical response to serotonin agonists? J Affect Disord 62(1-2):93–100
Hegerl U, Hensch T (2014) The vigilance regulation model of affective disorders and ADHD. Neurosci Biobehav Rev 44:45–57. doi:10.1016/j.neubiorev.2012.10.008
Hegerl U, Juckel G (1993) Intensity dependence of auditory evoked potentials as an indicator of central serotonergic neurotransmission: a new hypothesis. Biol Psychiatry 33(3):173–187. doi:10.1016/0006-3223(93)90137-3
Hensch T, Herold U, Brocke B (2007) An electrophysiological endophenotype of hypomanic and hyperthymic personality. J Affect Disord 101(1-3):13–26. doi:10.1016/j.jad.2006.11.018
Hensch T, Herold U, Diers K, Armbruster D, Brocke B (2008) Reliability of intensity dependence of auditory-evoked potentials. Clin Neurophysiol 119(1):224–236. doi:10.1016/j.clinph.2007.09.127
Hensch T, Wargelius H, Herold U, Lesch K, Oreland L, Brocke B (2006) Further evidence for an association of 5-HTTLPR with intensity dependence of auditory-evoked potentials. Neuropsychopharmacology 31(9):2047–2054. doi:10.1038/sj.npp.1301020
Hernandez-Lopez S, Garduño J, Mihailescu S (2013) Nicotinic modulation of serotonergic activity in the dorsal raphe nucleus. Rev Neurosci 24(5):455–469. doi:10.1515/revneuro-2013-0012
Huang J, Sander C, Jawinski P, Ulke C, Spada J, Hegerl U, Hensch T (2015) Test-retest reliability of brain arousal regulation as assessed with VIGALL 2.0. Neuropsychiatr Electrophysiol 1(1):263. doi:10.1186/s40810-015-0013-9
Iacono WG, Carlson SR, Malone SM, McGue M (2002) P3 event-related potential amplitude and the risk for disinhibitory disorders in adolescent boys. Arch Gen Psychiatry 59(8):750–757
Jawinski P, Sander C, Mauche N, Spada J, Huang J, Schmidt A, Häntzsch M, Burkhardt R, Scholz M, Hegerl U, Hensch T (2015) Brain arousal regulation in carriers of bipolar disorder risk alleles. Neuropsychobiology 72(2):65–73. doi:10.1159/000437438
Juckel G (2015) Serotonin: from sensory processing to schizophrenia using an electrophysiological method. Behav Brain Res 277:121–124. doi:10.1016/j.bbr.2014.05.042
Juckel G, Hegerl U, Molnár M, Csépe V, Karmos G (1999) Auditory evoked potentials reflect serotonergic neuronal activity—a study in behaving cats administered drugs acting on 5-HT1A autoreceptors in the dorsal raphe nucleus. Neuropsychopharmacology 21(6):710–716. doi:10.1016/S0893-133X(99)00074-3
Juckel G, Mavrogiorgou P, Bredemeier S, Gallinat J, Frodl T, Schulz C, Möller H, Hegerl U (2004) Loudness dependence of primary auditory-cortex-evoked activity as predictor of therapeutic outcome to prophylactic lithium treatment in affective disorders—a retrospective study. Pharmacopsychiatry 37(2):46–51. doi:10.1055/s-2004-815524
Juckel G, Molnár M, Hegerl U, Csépe V, Karmos G (1997) Auditory-evoked potentials as indicator of brain serotonergic activity—first evidence in behaving cats. Biol Psychiatry 41(12):1181–1195
Juckel G, Pogarell O, Augustin H, Mulert C, Müller-Siecheneder F, Frodl T, Mavrogiorgou P, Hegerl U (2007) Differential prediction of first clinical response to serotonergic and noradrenergic antidepressants using the loudness dependence of auditory evoked potentials in patients with major depressive disorder. J Clin Psychiatry 68(8):1206–1212
Karama S, Ducharme S, Corley J, Chouinard-Decorte F, Starr JM, Wardlaw JM, Bastin ME, Deary IJ (2015) Cigarette smoking and thinning of the brain’s cortex. Mol Psychiatry 20(6):778–785. doi:10.1038/mp.2014.187
Lampert T, Kroll L, Müters S, Stolzenberg H (2013) Measurement of socioeconomic status in the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 56(5-6):631–636. doi:10.1007/s00103-012-1663-4
Lee TW, Yu YW, Chen TJ, Tsai SJ (2005) Loudness dependence of the auditory evoked potential and response to antidepressants in Chinese patients with major depression. J Psychiatry Neurosci 30(3):202–205
Linka T, Müller BW, Bender S, Sartory G (2004) The intensity dependence of the auditory evoked N1 component as a predictor of response to citalopram treatment in patients with major depression. Neurosci Lett 367(3):375–378. doi:10.1016/j.neulet.2004.06.038
Linka T, Müller BW, Bender S, Sartory G, Gastpar M (2005) The intensity dependence of auditory evoked ERP components predicts responsiveness to reboxetine treatment in major depression. Pharmacopsychiatry 38(3):139–143. doi:10.1055/s-2005-864126
Loeffler M, Engel C, Ahnert P, Alfermann D, Arelin K, Baber R, Beutner F, Binder H, Brähler E, Burkhardt R, Ceglarek U, Enzenbach C, Fuchs M, Glaesmer H, Girlich F, Hagendorff A, Häntzsch M, Hegerl U, Henger S, Hensch T, Hinz A, Holzendorf V, Husser D, Kersting A, Kiel A, Kirsten T, Kratzsch J, Krohn K, Luck T, Melzer S, Netto J, Nüchter M, Raschpichler M, Rauscher FG, Riedel-Heller SG, Sander C, Scholz M, Schönknecht P, Schroeter ML, Simon J, Speer R, Stäker J, Stein R, Stöbel-Richter Y, Stumvoll M, Tarnok A, Teren A, Teupser D, Then FS, Tönjes A, Treudler R, Villringer A, Weissgerber A, Wiedemann P, Zachariae S, Wirkner K, Thiery J (2015) The LIFE-Adult-Study: objectives and design of a population-based cohort study with 10,000 deeply phenotyped adults in Germany. BMC Public Health 15(1):691. doi:10.1186/s12889-015-1983-z
Malone KM, Waternaux C, Haas GL, Cooper TB, Li S, Mann JJ (2003) Cigarette smoking, suicidal behavior, and serotonin function in major psychiatric disorders. Am J Psychiatry 160(4):773–779
Manjarrez G, Hernandez E, Robles A, Hernandez J (2005) N1/P2 component of auditory evoked potential reflect changes of the brain serotonin biosynthesis in rats. Nutr Neurosci 8(4):213–218. doi:10.1080/10284150500170971
Miller GA, Chapman JP (2001) Misunderstanding analysis of covariance. J Abnorm Psychol 110(1):40–48
Min J, Lee S, Lee S, Chae J, Lee C, Park Y, Bae S (2012) Clinical characteristics associated with different strengths of loudness dependence of auditory evoked potentials (LDAEP) in major depressive disorder. Psychiatry Res 200(2-3):374–381. doi:10.1016/j.psychres.2012.06.038
Mons U, Schöttker B, Müller H, Kliegel M, Brenner H (2013) History of lifetime smoking, smoking cessation and cognitive function in the elderly population. Eur J Epidemiol 28(10):823–831. doi:10.1007/s10654-013-9840-9
Mulert C, Juckel G, Brunnmeier M, Karch S, Leicht G, Mergl R, Möller H, Hegerl U, Pogarell O (2007) Prediction of treatment response in major depression: integration of concepts. J Affect Disord 98(3):215–225. doi:10.1016/j.jad.2006.07.021
O’Connor JJ, Rowan MJ, Anwyl R (1992) Serotoninergic depression of auditory evoked responses recorded in the rat hippocampus: effect of repeated buspirone treatment. Brain Res 573(2):190–196
Oreland L, Damberg M, Hallman J, Garpenstrand H (2002) Smoking only explains part of the associations between platelet monoamine oxidase activity and personality. J Neural Transm 109(5-6):963–975. doi:10.1007/s007020200079
Park Y, Jung E, Kim HS, Hahn SW, Lee S (2015) Differences in central serotoninergic transmission among patients with recent onset, sub-chronic, and chronic schizophrenia as assessed by the loudness dependence of auditory evoked potentials. Schizophr Res 168(1-2):180–184. doi:10.1016/j.schres.2015.07.036
Pritchard W, Sokhadze E, Houlihan M (2004) Effects of nicotine and smoking on event‐related potentials: a review. Nicotine Tob Res 6(6):961–984. doi:10.1080/14622200412331324848
Rowan MJ, O’Connor JJ, Anwyl R (1988) Changes in auditory evoked responses and in the inhibitory action of 5-hydroxytryptophan following chronic treatment with imipramine in the rat. Psychopharmacology (Berl) 96(3):408–413
Sander C, Hensch T, Wittekind DA, Böttger D, Hegerl U (2016) Assessment of wakefulness and brain arousal regulation in psychiatric research. Neuropsychobiology:195–205. doi: 10.1159/000439384
Seth P, Cheeta S, Tucci S, File SE (2002) Nicotinic—serotonergic interactions in brain and behaviour. Pharmacol Biochem Behav 71(4):795–805
Siniatchkin M, Kropp P, Neumann M, Gerber W, Stephani U (2000) Intensity dependence of auditory evoked cortical potentials in migraine families. Pain 85(1-2):247–254
Smith PH, Mazure CM, McKee SA (2014) Smoking and mental illness in the U.S. population. Tob Control 23(e2):e147–53. doi:10.1136/tobaccocontrol-2013-051466
Strobel A, Debener S, Schmidt D, Hünnerkopf R, Lesch K, Brocke B (2003) Allelic variation in serotonin transporter function associated with the intensity dependence of the auditory evoked potential. Am J Med Genet B Neuropsychiatr Genet 118B(1):41–47. doi:10.1002/ajmg.b.10019
Thoemmes F (2012) Propensity score matching in SPSS. Retrieved December 2, 2015, from http://arxiv.org/ftp/arxiv/papers/1201/1201.6385.pdf
Tuchtenhagen F, Daumann J, Norra C, Gobbelé R, Becker S, Pelz S, Sass H, Buchner H, Gouzoulis-Mayfrank E (2000) High intensity dependence of auditory evoked dipole source activity indicates decreased serotonergic activity in abstinent ecstasy (MDMA) users. Neuropsychopharmacology 22(6):608–617. doi:10.1016/S0893-133X(99)00140-2
Van Breukelen GJP, Van Dijk KRA (2007) Use of covariates in randomized controlled trials. J Int Neuropsychol Soc 13(5):903–904
Weiland BJ, Sabbineni A, Calhoun VD, Welsh RC, Hutchison KE (2015) Reduced executive and default network functional connectivity in cigarette smokers. Hum Brain Mapp 36(3):872–882. doi:10.1002/hbm.22672
Wutzler A, Winter C, Kitzrow W, Uhl I, Wolf RJ, Heinz A, Juckel G (2008) Loudness dependence of auditory evoked potentials as indicator of central serotonergic neurotransmission: simultaneous electrophysiological recordings and in vivo microdialysis in the rat primary auditory cortex. Neuropsychopharmacology 33(13):3176–3181. doi:10.1038/npp.2008.42
Wyss C, Hitz K, Hengartner MP, Theodoridou A, Obermann C, Uhl I, Roser P, Grünblatt E, Seifritz E, Juckel G, Kawohl W (2013) The loudness dependence of auditory evoked potentials (LDAEP) as an indicator of serotonergic dysfunction in patients with predominant schizophrenic negative symptoms. PLoS One 8(7):e68650. doi:10.1371/journal.pone.0068650
Acknowledgments
We thank Mandy Schmidt, Alexander Heinzig, and Ulrike Gessendorfer for their assistance with the data collection and data management and Anne Gärtner, who assisted with the proofreading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were carried out according to the Declaration of Helsinki and approved by the Ethics Committee of the University of Leipzig (263-2009-14122009). Subjects gave written informed consent and received an expense allowance.
Conflict of interest
Within the last 3 years, Prof. Hegerl was an advisory board member for Lilly, Lundbeck, Takeda Pharmaceuticals, Servier, and Otsuka Pharma and a speaker for Bristol-Myers Squibb, Medice Arzneimittel, Novartis, and Roche Pharma. The other authors have no financial or competing interests to declare.
Role of the funding source
This publication was supported by LIFE – Leipzig Research Center for Civilization Diseases, University of Leipzig. This project was funded by means of the European Social Fund and the Free State of Saxony. The funding sources were not involved in the design of the study and writing of the paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 477 kb)
Rights and permissions
About this article
Cite this article
Jawinski, P., Mauche, N., Ulke, C. et al. Tobacco use is associated with reduced amplitude and intensity dependence of the cortical auditory evoked N1-P2 component. Psychopharmacology 233, 2173–2183 (2016). https://doi.org/10.1007/s00213-016-4268-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-016-4268-z