Abstract
Introduction
The cognitive effects of nicotine in humans remain a topic of great interest, due to the continued prevalence of cigarette smoking in society as well as the hypothesis that cognitively impaired populations such as schizophrenia patients use nicotine as a means of self-medicating against deficits of sensory gating. However, chronic smoking can predispose individuals to robust monoamine oxidase (MAO) inhibition, and thus far, the effect of MAO inhibition on human sensory gating is unknown.
Methods
In this study, we investigated the effects of both nicotine (6-mg gum) and pharmacologically induced MAO-A inhibition via moclobemide (75 mg) on P50 event-related potential-indexed sensory gating in a sample of 24 healthy non-smoking males.
Results
Ratio score (rP50) measured gating revealed significant improvement in auditory stimulus suppression after combined nicotine and MAO-A inhibition compared to placebo and to the nicotine-alone condition. This nicotine + MAO-A inhibition-induced efficient gating was consistent regardless of participants’ baseline (placebo) gating efficiency, despite the observation that nicotine in the absence of MAO-A inhibition exhibited a detrimental effect on gating in participants with high baseline suppression ratios.
Conclusion
Nicotine and monoamine oxidase-inhibiting agents in tobacco smoke appear to exert a synergistic effect on sensory gating, which may contribute to the elevated dependence rates seen in populations with cognitive deficits such as schizophrenia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
While a large volume of research has focused on nicotine’s effects on cognition in schizophrenia (Hashimoto et al. 2005), evidence suggests that the neuropsychopharmacological effects of tobacco smoke are not a result of nicotine’s actions alone. A number of studies have demonstrated an inhibition of the enzyme monoamine oxidase (MAO) via tobacco smoke (Berlin et al. 1995a, b; Fowler et al. 2003; Oreland et al. 1981), and moreover, this inhibition is likely not a result of nicotine (Castagnoli and Murugesan 2004). MAO activity has been negatively correlated with smoking behavior, and low baseline MAO significantly predicted the intensity of withdrawal symptoms after smoking cessation (Rose et al. 2001). It is thus probable that MAO inhibition plays a significant role in the reinforcing effects of smoking behavior. Interestingly, pharmacologically inhibited MAO has been shown to antagonize the cognitive deficits associated with cholinergic blockade (Wesnes et al. 1988). As such, an understanding of the relationship between cognition, MAO activity, and nicotine is a necessary step on the path to understanding smoking behavior as well as achieving practical treatment of low-cognition, high-smoking populations.
Smoking rates among individuals with mental illness (40.1 %) are double the rate reported in individuals with no psychiatric diagnosis (21.3 %) (Lawrence et al. 2009). Schizophrenia patients, in particular, exhibit the highest rates of smoking, estimated to be as high as 80 % (Dalack et al. 1999). This elevated smoking rate, combined with observed deficits in nicotinic receptors (nAChRs) in patients (Dalack et al. 1998), has led to the hypothesis that schizophrenia patients utilize smoking as a form of self-medication against cognitive deficits that characterize the disease (Kumari and Postma 2005). Specifically, smoking has been shown to normalize auditory event-related potential (P50)-indexed sensory gating deficits in schizophrenia and first-degree relatives (Adler et al. 1992, 1993). However, the extent to which this effect results from nicotine, MAO inhibition, or the combination thereof is not known.
Two isoforms of MAO exist in humans: MAO-A, which preferentially metabolizes serotonin and norepinephrine and is preferentially inhibited by clorgyline and moclobemide, and MAO-B, which catabolizes phenylethylamine and benzylamine and is preferentially inhibited by l-deprenyl (selegiline). Dopamine, tyramine, and tryptamine are metabolized by both MAO-A and MAO-B (Weyler et al. 1976; Johnston 1968; Lewis et al. 2007; Yamada and Yasuhara 2004). It has been suggested that MAO may act to maintain a low concentration of monoamine neurotransmitters within the neuron, thus facilitating the uptake of neurotransmitters from the synaptic cleft. MAO may also protect the neuron from accidental stimulation by extraneous amines (Saura et al. 1996), though it has been shown that the MAO-A inhibitor clorgyline inhibits serotonin degradation (Blier et al. 1986; Twist et al. 1990), suggesting MAO-A may oxidize serotonin exterior to the neuron (Shih et al. 1999).
In clinical settings, pharmacological MAO inhibition is typically used as treatment for depression, though it has also proven effective in Parkinson’s and Alzheimer’s diseases (Youdim et al. 2006). The potentially lethal side effects of early irreversible MAO inhibitors earned these drugs a dangerous reputation, only to be used as a last resort (Youdim and Bakhle 2006). The development of reversible MAO inhibitors, such as moclobemide, allowed for safe and effective clinical use of these medications, aided in part by the observation that selective inhibition of either MAO-A or B increases dopamine release in striatum (Haefely et al. 1992). Moclobemide has been proposed as an effective aid for smoking cessation, possibly by counteracting the state of dopamine depletion experienced by ex-smokers as a result of normalizing MAO activity 3–4 weeks after quitting (Berlin et al. 1995a, b; Watkins et al. 2000).
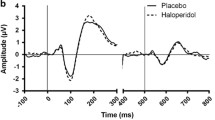
To our knowledge, the contribution of MAO inhibition to the cognitive effects of cigarette smoking, and specifically sensory gating, has not been studied. However, there is evidence that both dopaminergic and cholinergic mechanisms are simultaneously at play. Gating, typically measured electroencephalographically by comparing the P50 amplitude difference (dP50) or ratio (rP50) of two identical auditory stimuli (“clicks”) presented 500 ms apart, was differentially improved by nicotine depending on dopamine transporter 1 (Millar et al. 2011) and D2 receptor (Knott et al. 2010a, b) gene polymorphisms in healthy controls. Moreover, nicotine was shown to improve gating in subjects with both low baseline gating and catechol-O-methyltransferase (COMT) polymorphisms associated with reduced synaptic dopamine and reduced gating in individuals with high baseline gating and COMT polymorphisms associated with higher synaptic dopamine (de la Salle et al. 2013). Dextroamphetamine reduced gating in healthy subjects (Light et al. 1999). The dopamine D2 receptor antagonist haloperidol also increases gating in individuals exhibiting low baseline gating and similarly disrupts gating in subjects with normal baseline gating (Csomor et al. 2008), and this same “inverted U” pattern of effect is observed with nicotine administration in the absence of other drugs (Knott et al. 2013).
A number of studies have found evidence that the modulation of serotonin and noradrenaline also affect P50 gating in healthy individuals. Mann et al. (2007) observed a disruption of P50 gating after simultaneously depleting serotonin and dopamine, but not after selective depletion of either serotonin or dopamine individually. Interestingly, selective reuptake inhibition of serotonin via a 10-mg escitalopram had no effect on gating (Jensen et al. 2008) while a dose of 15-mg escitalopram significantly reduced gating (Oranje et al. 2011). Imipramine, which has anticholinergic properties at muscarinic receptors and which inhibits reuptake of serotonin, noradrenaline, and, to a much lesser extent, dopamine, was found to decrease P50 suppression (Hammer et al. 2007). Ayahuasca, an herbal concoction which combines the psychedelic N,N-dimethyltryptamine (DMT) as well as MAO inhibiting agents, was shown to disrupt P50 gating in a dose-dependant manner (Riba et al. 2002). Increased noradrenergic transmission via yohimbine reduced gating, albeit in a small sample (Adler et al. 1994). In schizophrenia, selective antagonism of serotonin at the 5-HT3 receptor improved P50 gating in medicated patients (Adler et al. 2005), and increased noradrenaline via clonidine normalized gating in schizophrenia except at a high dose (Oranje and Glenthøj 2014). While few of these studies are directly comparable, overall it appears that P50 gating can be modulated differentially depending on the affected combination of monoamines as well as the degree (dose) to which these monoamines are increased or decreased.
We hypothesized that inhibition of MAO-A via moclobemide would yield similar effects to the above described monoaminergic modulation in a sample of healthy individuals, i.e., the disruption of P50 gating in individuals with normal baseline gating and improvement of P50 gating in individuals with low baseline gating. Animal models have associated gating ability with the presence and function of hippocampal low-affinity nicotinic acetylcholine receptors (α7 nAChRs) (Luntz-Leybman et al. 1992; Stevens et al. 1996). In a computational model of hippocampal P50 gating, it was shown that dopamine may modulate the synchrony of gating response in nicotinic-dependant GABAergic microcircuits in an inverted U fashion, wherein optimal levels of dopamine yielded the most efficient gating and too much or too little dopamine resulted in disrupted gating via reduction in neuronal signal-to-noise ratio (Moxon et al. 2003). We thus further hypothesized that the combined nicotinic stimulation of inhibitory GABAergic interneurons and moclobemide-enhanced dopaminergic release would further improve P50 gating in healthy individuals exhibiting low baseline gating. In individuals with normal baseline gating, we hypothesized that this combination would rescue gating deficiencies seen with separate administration of moclobemide or nicotine, by returning hippocampal microcircuit signal-to-noise ratios to normal.
Materials and methods
Subjects
This study was approved by and carried out in compliance with the Research Ethics Board of the Royal Ottawa Health Care Group as well as the University of Ottawa Research Ethics Board. Twenty-four healthy male volunteers were recruited by local advertisement. In order to avoid potential gender differences in gating (Hetrick et al. 1996), as well as possible menstrual cycle-related variation in serotonin levels (Hindberg and Naesh 1992), only male participants were included. All participants were non-smokers, defined as having smoked less than 100 total lifetime cigarettes and none in the past year, as well as exhibiting expired carbon monoxide (CO) levels less than 3 ppm. Prior to the first test session, participants underwent a medical evaluation as well as psychiatric interview using the structured clinical interview for DSM-IV-R Non-Patient Edition (SCID-NP) (First et al. 1995) and the Family Interview for Genetic Studies (FIGS) (Maxwell 1992). Volunteers were screened via self-report for current/past personal or family psychiatric (including alcohol/drug abuse/dependence) or neurologic (including seizures, head trauma with loss of consciousness <1 h within the past 2 years) disorder, current use of medication (including over the counter medications and herbal medications), excessive caffeine use (>4 cups of coffee/day or equivalent), body mass index (BMI) 20–30 kg/m2, and audiometrically assessed normal hearing.
Experimental design
Participants attended the laboratory on four test days (separated by a minimum of 48 h) in a randomized, double-blind, placebo-controlled crossover design, where counterbalanced drug combinations included placebo/placebo (PP), moclobemide/placebo (MP), placebo/nicotine (PNic), or moclobemide/nicotine (MNic).
Moclobemide administration
Moclobemide 75 mg (Manerix®, Hoffman-La Roche) was used to pharmacologically inhibit MAO-A. Moclobemide, having a mean Tmax of 49 min and elimination half-life of 1.5 h, decreases plasma 3,5-dihydroxyphenylglycine (DHPG) by ~55 % at 120 min (Hoffman-La Roche Ltd 2009). As such, this study used a single dose of 75 mg in order to achieve ~30–40 % plasma DHPG reductions. To maintain a double-blind, the dose of moclobemide and the placebo (cellulose) were each placed in opaque capsules.
Nicotine administration
Nicotine was administered in the form of two pieces (4 mg + 2 mg) of cinnamon-flavored Nicorette® gum (Johnson & Johnson Inc., Markham, Ontario, Canada). The total (6 mg) dose was used to achieve a similar blood nicotine level to that of an average smoker after smoking a single cigarette of average nicotine yield, i.e., 15–30 ng/ml (Hukkanen et al. 2005). Peak blood nicotine levels using this method and dose arise at approximately 30 min following the start of chewing. The elimination half-life of nicotine is ~120 min. Gum was chewed in accordance with manufacturer’s guidelines, i.e., a chewing time of 25 min, biting twice every minute (as cued by audio recording), and “parking” gum between the teeth and cheeks between bites. Placebo gum was similar in size, color, texture, and taste. In addition, participants wore nose plugs throughout the chewing process in order to reduce any sensory differences between the nicotine gum and placebo.
A physical symptom checklist (Harkrider and Hedrick 2005) was used to measure the severity of nicotine-related adverse symptoms as reported by each participant on each session. Symptoms (such as heart pounding, headache, dizziness, and nausea) were quantified on a five-point scale where 1 = “no symptoms,” 2 = “mild symptoms,” 3 = moderate symptoms,” 4 = “strong symptoms,” and 5 = “extreme symptoms.”
Procedure
Prior to any testing session, participants were interviewed by the study psychiatrist to screen for any contraindications associated with the use of moclobemide. Participants attended four test sessions after 8 h of abstinence from food, medicines, alcohol, and caffeine. Upon arrival, CO levels were assessed in order to ensure CO levels below 3 ppm. Participants were then given a capsule containing either 75-mg moclobemide or placebo, after which they engaged in light reading during a 90-min rest period in order to ensure Tmax activity during recording. Electrodes were attached after this rest period, while the participant was given either nicotine or placebo gum. After hookup/gum chewing, the P50 paradigm was administered.
P50 ERP acquisition
During the P50 paradigm, participants sat in a dimly lit, sound attenuated chamber and were instructed to keep their eyes open as they watched a silent nature movie and to ignore the auditory stimuli presented binaurally through headphones. Sixty-four 85-dB (SPL) stimulus (click) pairs (S1–S2) were presented, all with 1-ms stimulus durations and inter-stimulus intervals (between S1 and S2) of 500 ms and inter-pair intervals (between S2 and S1) of 10 s. EEG was recorded from eight scalp sites (F Z, F 3, F 4, C Z, C 3, C 4, P Z, O Z) using a nose reference and a ground electrode positioned between FPz and Fz sites. Vertical (VEOG) and horizontal (HEOG) electro-oculographic activity was measured using additional electrodes above and below the right eye as well as on the external canthus of both eyes, respectively. Electrode impedances were maintained below 5 kΩ, and electrical activity was recorded using a Brain Vision V-8 Amplifier® (Brain Products, Germany) with bandpass filters set at 0.1–120 Hz, digitized continuously at 500 Hz by Brain Vision Recorder Software (Brain Products, Germany).
P50 ERP processing
Offline analysis was performed using Brain Vision Analyzer® (Brain Products, Germany). Data was filtered (10–50 Hz) and segmented into 250-ms (50-ms pre-stim) epochs. Epochs were then corrected for eye movement and blink activity (Gratton et al. 1983), and artifacts (voltages exceeding ±75 μV) were excluded from the analysis. When either an S1 or S2 segment was rejected, the corresponding, paired segment (S1 or S2) was also excluded from analysis. Remaining epochs were baseline corrected (to 50-ms pre-stim) and averaged separately for S1 and S2.
Peak amplitudes for S1 and S2 were measured at the Cz site, with the stipulation that a P50 must be identifiable in at least one additional central site (i.e., C3/C4). Semi-automatic identification of P50 proceeded as described by Boutros et al. (2004). P50 was chosen as the second of two positive peaks, appearing as the largest positivity between 40 and 80 ms relative to pre-stimulus baseline and following an earlier positive peak (Pa) at 15–40 ms. The peak for S1 was used to guide the identification of the relative onset of S2. In addition to peak amplitude and latency, both the ratio index (S2 P50 amplitude divided by S1 P50 amplitude) and difference score (S1 P50 amplitude minus S2 P50 amplitude) were derived as measures of sensory gating.
Statistical analysis
Data was analyzed using IBM SPSS software. Amplitudes, latencies, and gating measures (rP50/dP50) were subjected to separate repeated measures analyses of variance (ANOVA) with drug and stimulus (S1/S2) as within-group factors. Significant effects and a priori hypotheses were followed up with pairwise comparisons. To test whether drug conditions differentially affected subjects with high (HG) or low (LG) baseline P50 gating as measured by the placebo (PP) condition, subjects were grouped via median split into low (N = 12) and high (N = 12) gaters, as has been employed by previous studies (Csomor et al. 2008; Knott et al. 2010a, b; de la Salle et al. 2013). In order to maintain consistency with the literature in using both rP50 and dP50 measures, separate repeated measures ANOVAs were performed after grouping subjects by placebo rP50 (rHG vs. rLG) and after grouping subjects by placebo dP50 measures (dHG vs. dLG), with drug conditions as within-subject factors and gating group (HG vs. LG) as between-subject factors. Groups created using rP50 baselines differed from groups created using dP50 baselines by two participants. The Shapiro-Wilk test of normality was used for all datasets prior to analysis. Datasets that were not normally distributed were compared using the Wilcoxon signed-rank test; all other data were compared with paired sample t tests.
Results
Tests of normality
For all subjects (N = 24), it was found that amplitude data for both S1 and S2 were not normally distributed, with the exception of S1 amplitude in the MP group. While dP50 scores were normally distributed, rP50 scores in the MP, PNic, and MNic conditions were not normally distributed. After segregating data into groups based on baseline rP50 scores, rLG amplitudes for S1 and S2 were not normally distributed with the exception of S1 amplitude in the MP group. rLG rP50 scores were not normally distributed in the PP and MP groups. rHG S1 amplitudes in the PP and MP groups as well as rHG S2 amplitude in the MNic group were not normally distributed. rHG rP50 data was not normally distributed in the MNic group.
After segregating data into groups based on baseline dP50 scores, dLG S1 and S2 amplitudes were normally distributed while dHG S1 amplitudes were not normally distributed with the exception of the MP group, and dHG S2 amplitudes were not normally distributed in all groups. Both dLG and dHG dP50 scores were normally distributed. Amplitudes, latencies, and gating measures are summarized in Table 1.
P50 amplitudes
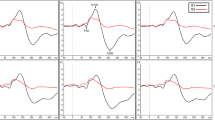
Grand-averaged waveforms for S1 vs. S2 in each drug condition are shown in Fig. 1. Analysis of P50 amplitudes resulted in a significant main effect of stimulus, F(1,23) = 61.275 p < 0.000, due to larger overall amplitudes of S1 (M = 4.556 μV, SE = 0.67) compared to S2 (M = 2.450 μV, SE = 0.63), t(23) = 7.83. There was no significant stimulus by drug interaction. Follow-up comparisons confirmed there were no significant differences between drug conditions for either S1 or S2 amplitudes.
After segregation of low and high baseline gating based on rP50, no significant stimulus × group, drug × group, or stimulus × group × drug interactions were observed. However, planned comparisons revealed larger rLG S2 amplitudes in the PP condition (M = 4.093, SE = 1.54) compared to the MNic condition (M = 2.995, SE = 1.00) Z = 1.96, p = 0.05.
Segregating groups based on dP50 revealed a significant drug × stimulus × group interaction F(3,66) = 3.143, p = 0.045, due to larger dHG S1 amplitudes in the PP condition (M = 6.359 μV, SE = 1.88) compared to both the PNic condition (M = 5.160 μV, SE = 1.92) Z = −2.35, p = 0.019. The low gating group showed lower dLG S1 amplitudes in the PP condition (M = 3.085 μV, SE = 0.35) compared to the MP condition (M = 4.038 μV, SE = 0.52) t(11) = 2.285, p = 0.043, as well as compared to the PNic condition (M = 4.212 μV, SE = 1.44) t(11) = 2.084, p = 0.061 and to the MNic condition (M = 4.134 μV, SE = 0.49) t(11) = 3.106, p = 0.010.
P50 latencies
Analysis of P50 latencies showed a significant main effect of stimulus, F(1,23) = 6.080, p = 0.022, due to longer overall latencies for S1 (M = 61.417 ms, SE = 2.01) compared to S2 (M = 57.083 ms, SE = 1.45), t(23) = 2.47. Pairwise comparisons revealed that only the PNic condition yielded significant differences in latency between S1 (M = 60.417 ms, SE = 1.99) and S2 (M = 55.083 ms, SE = 1.67) t(23) = 2.43. There was no significant stimulus by drug interaction. Follow-up analysis confirmed there were no significant differences between drug conditions for either S1 or S2 latencies.
After segregation of low and high baseline rP50 gating, no significant stimulus × group, drug × group, or stimulus × group × drug interactions were observed. Segregating groups based on dP50 revealed a significant stimulus × group interaction, F(1,22) = 5.738, p = 0.026, due to longer dHG S1 latencies (M = 62.917 ms, SE = 2.87) compared to S2 latencies (M = 54.750 ms, SE = 1.97) t(11) = 3.61, p = 0.002.
P50 gating measures
Overall analysis of rP50 and dP50 gating measures yielded no significant main effects. Planned comparisons revealed significantly lower rP50 scores in the MNic session (M = 0.405, SE = 0.08) compared to the PP session (M = 0.574, SE = 0.06) Z = 2.34, p = 0.019 (Fig. 2). The MNic group also exhibited significantly lower rP50 scores compared to the PNic session (M = 0.684, SE = 0.10) Z = 2.00, p = 0.046.
After grouping participants based on low and high baseline rP50 gating, no significant drug × group interactions were found. Planned comparisons revealed a significant difference between rLG rP50 scores in the PP condition (M = 0.817, SE = 0.07) and rLG rP50 scores in the MNic condition (M = 0.537, SE = 0.07) Z = 2.35, p = 0.019 as well as significantly reduced rHG rP50 gating in the PNic condition (M = 0.734, SE = 0.14) compared to both the PP condition (M = 0.331, SE = 0.05) t(11) = 2.99, p = 0.012 and the MNic condition (M = 0.274, SE = 0.13) Z = 2.43, p = 0.006 (Fig. 3).
After grouping participants based on low and high baseline dP50 gating, there was a significant group × drug interaction F(1,22) = 3.143, p = 0.045, due to significantly lower dLG dP50 scores in the PP condition (M = 0.775 μV, SE = 0.20) compared to the MNic condition (M = 2.144 μV, SE = 0.52) t(11) = 2.73, p = 0.020 as well as significantly reduced dHG dP50 scores in the PNic condition (M = 1.644 μV, SE = 0.53) compared to the PP condition (M = 3.214 μV, SE = 0.42) t(11) = 2.79, p = 0.018.
Adverse events
There was a significant effect of drug F(1,23) = 1.643, p = 0.033, due to higher severity ratings for symptoms in the PNic session (M = 1.33, SE = 0.00) compared to the PP session (M = 1.00, SE = 0.00) t(23) = 0.23, p = 0.029 as well as compared to the MNic session (M = 1.00, SE = 0.00) t(23) = 0.23, p = 0.029.
Discussion
The present study was designed to investigate the separate and combined effects of acute nicotine administration and MAO-A inhibition via moclobemide on gating of the P50 auditory event-related potential. Though there was no main effect overall, planned comparisons revealed significantly reduced rP50 gating ratios after the combination of moclobemide and nicotine compared to placebo and to nicotine alone. Importantly, while nicotine generally improves rP50-measured gating in low baseline gating individuals (Knott et al. 2013), improvement by nicotine in our low baseline gating sample did not reach significance. The combination of moclobemide and nicotine did significantly improve gating in low baseline gating individuals, suggesting that the interaction of nicotine and monoamine oxidase A inhibition yields a more robust effect on the neural systems underlying gating than does nicotine alone.
Moreover, our high baseline gating sample exhibited results similar to those seen in previous studies (Knott et al. 2010a, b, 2013) with nicotine significantly attenuating gating in these individuals. Interestingly, the combination of moclobemide and nicotine did not attenuate gating in the high baseline gating group; participants in this condition exhibited gating measures similar to baseline. It seems possible that the previously observed “inverted U” relationship between cognitive function and nicotine (Newhouse et al. 2004), with nicotine ameliorating cognition in low-functioning individuals but inhibiting performance in optimally performing individuals, may be overridden by enhanced monoamine availability achieved through MAO-A inhibition, though whether this effect extends beyond P50 gating remains to be seen.
While dP50 did not show a significant overall (un-segregated) effect, the general direction across drug conditions was similar to our rP50 results, with the lack of dP50 significance possibly due to this measures’ higher sensitivity to S1P50 amplitude (Fuerst et al. 2007; Lu et al. 2007). This same phenomenon might also have contributed to our finding no interaction between drug, baseline group, and amplitude using rP50 baseline segregation, compared to dP50 segregation where the interaction was significant, and larger baseline S1P50 amplitudes were observed in the high gating group compared to the nicotine and moclobemide condition. However, the finding that rP50 segregation elucidated larger placebo S2P50 amplitudes in the low gating group compared to the nicotine and moclobemide condition suggests that these results are not simply a consequence of S1P50 modulation alone. This supports the interpretation that these are indeed sensory gating effects, as opposed to a modulation of S1-dependant sensory registration. The differences in S1P50 vs. S2P50 latencies were also specific to dP50 segregation and were significant only in the high baseline gating group, a finding not reported in previous studies and which may be specific to our sample.
Moclobemide in the absence of nicotine did not affect gating overall or after segregation compared to both placebo or to the moclobemide-with-nicotine condition. However, the direction of our results suggests that moclobemide-induced monoamine oxidase inhibition trended in a direction similar to nicotine’s effects, in that mean gating values were improved, albeit non-significantly, compared to baseline in the low baseline group and diminished in the high baseline group. It is possible that either a higher dose or a larger sample size may have yielded significant differences between moclobemide and placebo gating scores, similar to previous studies that have shown baseline-dependant differences following monoaminergic modulation via haloperidol (Csomor et al. 2008) and sertindole (Holstein et al. 2011).
Inconsistent with previous studies, nicotine in the absence of moclobemide did not significantly improve gating in the low-baseline group. Although similar to moclobemide, mean ratios trended in a direction of improvement compared to placebo. It is possible that this trend did not reach significance due to the fact that no “mid range” gating group was stratified in the current study due to a smaller sample size than was used in Knott et al. (2013), which would eliminate the possibility of relatively high gating individuals being stratified into the low group after median split. Another possibility is the gene-specific differential effects of nicotine observed by de la Salle et al. (2013), in that nicotine’s improvement in low baseline suppressors is more evident in carriers of the homozygous valine (Val/Val) variant of the COMT polymorphism compared to that of homozygous methionine (Met/Met) variant carriers. A disproportionate number of Met/Met allele carriers in the current low group could have prevented nicotine-driven improvements from reaching significance. Future studies may benefit from grouping subject based on genotype in addition to baseline gating.
As in Moxon et al. (2003)’s simulation, the most robust improvement of gating in this experiment occurred with the simultaneous promotion of monoaminergic release and nicotinic activation. Our results support findings where atypical antipsychotic drugs differentially improve gating depending on their ability to target multiple neurotransmitter systems (e.g., cholinergic, serotonergic, dopaminergic) simultaneously (Adler et al. 2004). In healthy individuals, it has been shown that normal gating is only diminished following the simultaneous depletion of dopamine and serotonin, but not when either monoamine is depleted individually (Mann et al. 2007). Thus, it would seem that optimal availability of dopamine and serotonin are necessary for efficient gating and that cholinergic activation contributes to the normalization of this availability, as was seen in our high baseline gating group in the MNic condition.
This study is limited to event-related potential data, and as such, we can only assume that the monoamine-modulating properties of moclobemide are responsible for the reported effects. Although subjects were asked to abstain from food prior to each test session, we did not control for day-to-day consumption of dietary choline or for foods with monoamine oxidase inhibitory properties. Although subjects reported greater adverse symptoms during the PNic condition compared to the PP and MNic condition, mean symptoms were very low, with the PNic group exhibiting a mean score of 1.33 where a score of 1 indicates no adverse symptoms at all. Thus it is not likely that physical symptoms contributed to event-related potential (ERP) results, though they cannot be ruled out entirely.
Care should be taken when interpreting the high vs. low baseline (placebo) comparisons in this study, as the use of the median split has been shown to decrease effect size and may produce misleading results (MacCallum et al. 2002), though we deemed this method appropriate for the current study due to the previously observed differential effects of nicotine in high vs. low gating individuals (Knott et al. 2010a, b) as well as the importance of utilizing our low gating group to serve as a model of gating deficits in schizophrenia. In our low group, mean ratio scores were 0.82, comparable to Patterson et al. (2008)’s meta-analysis which found mean schizophrenia ratio scores to be 0.80. Although we did control for family history of psychosis in our healthy control sample, we cannot determine if deficient gating in our low gating group was due to common mechanisms. One possibility is that our low-gaters share common nicotinic receptor polymorphisms (Houy et al. 2004); however, we lack the genetic data necessary to confirm this hypothesis. Finally, due to the relatively low number of electrodes (eight scalp sites), we cannot reliably report differences in brain region activation. Follow-up experiments are necessary to investigate the effects of MAO-B inhibition as well as combined MAO-A and MAO-B inhibition on gating with and without nicotine. A sample of non-smoking schizophrenia patients will also be necessary to confirm whether the gating improvements in our low gating group translate to the patient population, though the effects of treatment/medication would have to be taken into account.
Conclusion
This study supports the hypothesis that the ratio index of P50-measured sensory gating can be improved under conditions of acute nicotine and MAO-A inhibition in healthy individuals and, specifically, in individuals with low baseline gating. The improvement in P50 ratio in the current sample seems to be a result of true gating and not simply auditory registration. As this effect was seen in individuals with low baseline gating, a group that has been used as a healthy control model of schizophrenia (Light and Braff 2003; Csomor et al. 2008), the current study provides corroborating evidence that the theorized self-medicating smoking behavior of neuropsychologically impaired populations (e.g., schizophrenia) is not solely driven by activation of nicotinic receptors and instead may be due to a more complex MAO/nicotine interaction. Furthermore, MAO inhibition eliminates the detrimental effects of nicotine on high baseline gating individuals. Future studies on smoking and cognition should take into account the neuromodulating properties of non-nicotinic agents in tobacco in order to more accurately model smoking in laboratory paradigms. Clinicians may benefit from considering the smoking status of patients when determining treatment, particularly for heavy smokers who may exhibit robust MAO inhibition, due to the potential interaction of smoking with monoaminergic- or cholinergic-based medication.
References
Adler LE, Hoffer LJ, Griffith J, Waldo MC, Freedman R (1992) Normalization by nicotine of deficient auditory sensory gating in the relatives of schizophrenics. Biol Psychiatry 32:607–616
Adler LE, Hoffer LD, Wiser A, Freedman R (1993) Normalization of auditory physiology by cigarette smoking in schizophrenic patients. Am J Psychiatry 150:1856–1861
Adler LE, Hoffer L, Nagamoto HT, Waldo MC, Kisley MA, Giffith JM (1994) Yohimbine impairs P50 auditory sensory gating in normal subjects. Neuropsychopharmacology 10:249–257
Adler LE, Olincy A, Cawthra EM, McRae KA, Harris JG, Nagamoto HT et al (2004) Varied effects of atypical neuroleptics on P50 auditory gating in schizophrenia patients. Am J Psychiatry 161:1822–1828
Adler LE, Cawthra EM, Donovan KA, Harris JG, Nagamoto HT, Olincy A, Waldo MC (2005) Improved p50 auditory gating with ondansetron in medicated schizophrenia patients. Am J Psychiatry 162:386–388
Berlin I, Said S, Spreux-Varoquaux O, Olivares R, Launay JM, Puech AJ (1995a) Monoamine oxidase A and B activities in heavy smokers. Biol Psychiatry 38:756–761
Berlin I, Saïd S, Spreux-Varoquaux O, Launay JM, Olivares R, Millet V et al (1995b) A reversible monoamine oxidase A inhibitor (moclobemide) facilitates smoking cessation and abstinence in heavy, dependent smokers. Clin Pharmacol Ther 58:444–452
Blier P, De Montigny C, Azzaro AJ (1986) Modification of serotonergic and noradrenergic neurotransmissions by repeated administration of monoamine oxidase inhibitors: electrophysiological studies in the rat central nervous system. J Pharmacol Exp Ther 237:987–994
Boutros NN, Korzyukov O, Jansen B, Feingold A, Bell M (2004) Sensory gating deficits during the mid-latency phase of information processing in medicated schizophrenia patients. Psychiatry Res 126:203–215
Castagnoli K, Murugesan T (2004) Tobacco leaf, smoke and smoking, MAO inhibitors, Parkinson’s disease and neuroprotection; are there links? NeuroToxicology 25:279–291
Csomor PA, Stadler RR, Feldon J, Yee BK, Geyer MA, Vollenweider FX (2008) Haloperidol differentially modulates prepulse inhibition and p50 suppression in healthy humans stratified for low and high gating levels. Neuropsychopharmacology 33:497–512
Dalack GW, Healy DJ, Meador-Woodruff JH (1998) Nicotine dependence in schizophrenia: clinical phenomena and laboratory findings. Am J Psychiatry 155:1490–1501
Dalack GW, Becks L, Hill E, Pomerleau OF, Meador-Woodruff JH (1999) Nicotine withdrawal and psychiatric symptoms in cigarette smokers with schizophrenia. Neuropsychopharmacology 21:195–202
de la Salle S, Smith D, Choueiry J, Impey D, Philippe T, Dort H, Knott V (2013) Effects of COMT genotype on sensory gating and its modulation by nicotine: differences in low and high P50 suppressors. Neuroscience 241:147–156
First M, Spitzer R, Williams J, Gibbon M (1995) Structured Clinical Interview for DSM-IV: non-patient Version. American Psychiatric, Washington, DC
Fowler JS, Logan J, Wang GJ, Volkow ND, Telang F, Zhu W et al (2003) Low monoamine oxidase B in peripheral organs in smokers. Proc Natl Acad Sci U S A 100:11600–11605
Fuerst DR, Gallinat J, Boutros NN (2007) Range of sensory gating values and test–retest reliability in normal subjects. Psychophysiology 44:620–626
Gratton G, Coles MG, Donchin E (1983) A new method for off-line removal of ocular artifact. Electroencephalogr Clin Neurophysiol 55:468–484
Haefely W, Burkard WP, Cesura AM, Kettler R, Lorez HP, Martin JR et al (1992) Biochemistry and pharmacology of moclobemide, a prototype RIMA. Psychopharmacol (Berl) 106:S6–S14
Hammer TB, Oranje B, Glenthoj BY (2007) The effects of imipramine on P50 suppression, prepulse inhibition and habituation of the startle response in humans. Int J Neuropsychopharmacol 10:787–795
Harkrider AW, Hedrick MS (2005) Acute effect of nicotine on auditory gating in smokers and non-smokers. Hear Res 202:114–128
Hashimoto K, Koike K, Shimizu E, Iyo M (2005) α7 Nicotinic receptor agonists as potential therapeutic drugs for schizophrenia. Curr Med Chem Cent Nerv Sys 5:171–184
Hetrick WP, Sandman CA, Bunney WE Jr, Jin Y, Potkin SG, White MH (1996) Gender differences in gating of the auditory evoked potential in normal subjects. Biol Psychiatry 39:51–58
Hindberg I, Naesh O (1992) Serotonin concentrations in plasma and variations during the menstrual cycle. Clin Chem 38:2087–2089
Hoffman-La Roche Ltd. (2009) Manerix product monograph. www.rochecanada.com
Holstein DH, Csomor PA, Geyer MA, Huber T, Brugger N, Studerus E et al (2011) The effects of sertindole on sensory gating, sensorimotor gating, and cognition in healthy volunteers. J Psychopharmacol 25:1600–1613
Houy E, Raux G, Thibaut F, Belmont A, Demily C, Allio G et al (2004) The promoter−194 C polymorphism of the nicotinic alpha 7 receptor gene has a protective effect against the P50 sensory gating deficit. Mol Psychiatry 9:320–322
Hukkanen J, Jacob P, Benowitz NL (2005) Metabolism and disposition kinetics of nicotine. Pharmacol Rev 57:79–115
Jensen KS, Oranje B, Wienberg M, Glenthøj BY (2008) The effects of increased serotonergic activity on human sensory gating and its neural generators. Psychopharmacol (Berl) 196:631–641
Johnston J (1968) Some observations upon a new inhibitor of monoamine oxidase in brain tissue. Biochem Pharmacol 17:1285–1292
Knott VJ, Fisher DJ, Millar AM (2010a) Differential effects of nicotine on P50 amplitude, its gating, and their neural sources in low and high suppressors. Neuroscience 170:816–826
Knott V, Millar A, Fisher D, Albert P (2010b) Effects of nicotine on the amplitude and gating of the auditory P50 and its influence by dopamine D2 receptor gene polymorphism. Neuroscience 166:145–156
Knott V, de la Salle S, Smith D, Phillipe T, Dort H, Choueiry J et al (2013) Baseline dependency of nicotine’s sensory gating actions: similarities and differences in low, medium and high P50 suppressors. J Psychopharmacol 27:790–800
Kumari V, Postma P (2005) Nicotine use in schizophrenia: the self medication hypotheses. Neurosci Biobehav Rev 29:1021–1034
Lawrence D, Mitrou F, Zubrick SR (2009) Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health 9:285
Lewis A, Miller JH, Lea RA (2007) Monoamine oxidase and tobacco dependence. Neurotoxicology 28:182–195
Light GA, Braff DL (2003) Sensory gating deficits in schizophrenia: can we parse the effects of medication, nicotine use, and changes in clinical status? Clin Neur Res 3:47–54
Light GA, Malaspina D, Geyer MA, Luber BM, Coleman EA, Sackeim HA et al (1999) Amphetamine disrupts P50 suppression in normal subjects. Biol Psychiatry 46:990–996
Lu BY, Edgar JC, Jones AP, Smith AK, Huang MX, Miller GA et al (2007) Improved test–retest reliability of 50 ms paired click auditory gating using magnetoencephalography source modeling. Psychophysiology 44:86–90
Luntz-Leybman V, Bickford PC, Freedman R (1992) Cholinergic gating of response to auditory stimuli in rat hippocampus. Brain Res 587:130–136
MacCallum RC, Zhang S, Preacher KJ, Rucker DD (2002) On the practice of dichotomization of quantitative variables. Psychol Methods 7:19
Mann C, Croft RJ, Scholes KE, Dunne A, O’Neill BV, Leung S et al (2007) Differential effects of acute serotonin and dopamine depletion on prepulse inhibition and P50 suppression measures of sensorimotor and sensory gating in humans. Neuropsychopharmacology 33:1653–1666
Maxwell ME (1992) Family Interview for Genetic Studies (FIGS): a manual for FIGS. Clinical Neurogenetics Branch, Intramural Research Program, National Institute of Mental Health, Bethesda
Millar A, Smith D, Choueiry J, Fisher D, Albert P, Knott V (2011) The moderating role of the dopamine transporter 1 gene on P50 sensory gating and its modulation by nicotine. Neuroscience 180:148–156
Moxon KA, Gerhardt GA, Adler LE (2003) Dopaminergic modulation of the P50 auditory-evoked potential in a computer model of the CA3 region of the hippocampus: its relationship to sensory gating in schizophrenia. Biol Cybern 88:265–275
Newhouse PA, Potter A, Singh A (2004) Effects of nicotinic stimulation on cognitive performance. Curr Opin Pharmacol 4:36–46
Oranje B, Glenthøj BY (2014) Clonidine normalizes levels of P50 gating in patients with schizophrenia on stable medication. Schizophr Bull 40:1022–1029
Oranje B, Wienberg M, Glenthoj BY (2011) A single high dose of escitalopram disrupts sensory gating and habituation, but not sensorimotor gating in healthy volunteers. Psychiatry Res 186:431–436
Oreland L, Fowler CJ, Schalling D (1981) Low platelet monoamine oxidase activity in cigarette smokers. Life Sci 29:2511–2518
Patterson JV, Hetrick WP, Boutros NN, Jin Y, Sandman C, Stern H et al (2008) P50 sensory gating ratios in schizophrenics and controls: a review and data analysis. Psychiatry Res 158:226–247
Riba J, Rodríguez-Fornells A, Barbanoj MJ (2002) Effects of ayahuasca on sensory and sensorimotor gating in humans as measured by P50 suppression and prepulse inhibition of the startle reflex, respectively. Psychopharmacol (Berl) 165:18–28
Rose JE, Behm FM, Ramsey C, Ritchie JC Jr (2001) Platelet monoamine oxidase, smoking cessation, and tobacco withdrawal symptoms. Nicotine Tob Res 3:383–390
Saura J, Bleuel Z, Ulrich J, Mendelowitsch A, Chen K, Shih JC et al (1996) Molecular neuroanatomy of human monoamine oxidases A and B revealed by quantitative enzyme radioautography and in situ hybridization histochemistry. Neuroscience 70:755–774
Shih JC, Chen K, Ridd MJ (1999) Monoamine oxidase: from genes to behavior. Annu Rev Neurosci 22:197–217
Stevens KE, Freedman R, Collins AC, Hall M, Leonard S, Marks MJ et al (1996) Genetic correlation of inhibitory gating of hippocampal auditory evoked response and α-bungarotoxin-binding nicotinic cholinergic receptors in inbred mouse strains. Neuropsychopharmacology 15:152–162
Twist EC, Brammer MJ, Stephenson JD, Corn TH, Campbell IC (1990) The effect of chronic ritanserin and clorgyline administration on 5-HT2 receptor linked inositol phospholipid hydrolysis. Biochem Pharmacol 40:2111–2116
Watkins SS, Koob GF, Markou A (2000) Neural mechanisms underlying nicotine addiction: acute positive reinforcement and withdrawal. Nicotine Tob Res 2:19–37
Wesnes KA, Simpson PM, Christmas L, Anand R, McClelland GR (1988) The effects of moclobemide on cognition. J Neural Transm Suppl 28:91–102
Weyler W, Hsu Y, Breakefield X (1976) Biochemistry and genetics of monoamine oxidase. Pharmacol Ther 54:137–141
Yamada M, Yasuhara H (2004) Clinical pharmacology of MAO inhibitors: safety and future. NeuroToxicology 25:215–221
Youdim MB, Bakhle YS (2006) Monoamine oxidase: isoforms and inhibitors in Parkinson’s disease and depressive illness. Br J Pharmacol 147:S287–S296
Youdim MB, Edmondson D, Tipton KF (2006) The therapeutic potential of monoamine oxidase inhibitors. Nat Rev Neurosci 7:295–309
Funding and disclosure
The authors declare no conflict of interest. Contributions from all authors were carried out with funding by the University of Ottawa Medical Research Fund and by a grant from the Natural Sciences and Engineering Research Council of Canada (NSERC) awarded to Dr. Verner Knott.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Smith, D.M., Fisher, D., Blier, P. et al. The separate and combined effects of monoamine oxidase inhibition and nicotine on P50 sensory gating. Psychopharmacology 232, 1911–1920 (2015). https://doi.org/10.1007/s00213-014-3823-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-014-3823-8