Abstract
Stroke is the leading cause of death worldwide. Dipeptidyl peptidase-4 (DPP-4) inhibitors are a class of anti-diabetic drugs for treatment of type-2 diabetes mellitus. The aim of this study is to evaluate the possible neuroprotective effect of a dipeptidyl peptidase-4 inhibitor, vildagliptin, independent of its anti-diabetic properties in non-diabetic rats subjected to cerebral ischemia. Anesthetized Wistar rats were subjected to either left middle cerebral artery occlusion (MCAO) or sham operation followed by reperfusion after 30 min of MCAO. The other three groups were orally administered vildagliptin at 3 dose levels (2.5, 5, 10 mg/kg) for 3 successive weeks before subjected to left focal cerebral ischemia/reperfusion and till the end of the study. Neurological deficit scores and motor activity were assessed 24 h following reperfusion. Forty-eight hours following reperfusion, rats were euthanized and their left brain hemispheres were harvested and used in biochemical, histopathological, and immunohistochemical investigations. Vildagliptin pretreatment improved neurological deficit score, locomotor activity, and motor coordination in MCAO rats. Moreover, vildagliptin reduced malondialdehyde (MDA), elevated reduced glutathione (GSH), phosphotylinosital 3 kinase (PI3K), phosphoryated of protein kinase B (p-AKT), and mechanistic target of rapamycin (mTOR) brain contents in addition to reducing protein expression of caspase-3. Also, vildagliptin showed a dose-dependent attenuation in neuronal cell loss and histopathological alterations in MCAO rats. This study proves that vildagliptin exerted a neuroprotective effect in a dose-dependent manner as shown in the attenuation of the infarct area, neuronal cell loss, and histopathological damage in MCAO rats, which may be mediated by attenuating neuronal and motor deficits, its antioxidant property, activation of the PI3K/AKT/mTOR pathway, and its anti-apoptotic effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is the primary cause of long-term disability and is the fourth leading cause of death worldwide (Iadecola and Anrather 2011). According to the World Health Organization, 50% of stroke survivors suffer from some degree of physical or cognitive impairment, and about 20% of them require institutional care (Bustamante et al. 2016).
The vast majority of strokes are caused by a sudden occlusion of the intracranial or extracranial blood vessel by a thrombus or embolism, resulting in an almost immediate loss of oxygen and glucose to the cerebral tissue (Paulson 1971; Lakhan et al. 2009).
A critical therapeutic strategy is the rapid restoration of cerebral blood flow; however, aggravation of tissue injury commonly occurs during reperfusion, so-called ischemia and reperfusion (I/R) injury. Cerebral ischemia causes irreversible neuronal injury within minutes of the onset (Lakhan et al. 2009). I/R initiates a complex series of inflammatory events, which involve activation of microglia and astrocytes, influx of hematogenous cells recruited by adhesion molecules, cytokines, and chemokines across the activated blood vessel wall, and eventually leads to an increase in behavioral deficits and secondary brain damage (Jin et al. 2013; Wang et al. 2016). Furthermore, many studies have demonstrated that the severity of neuronal apoptosis is related to neuro-function, denoting that neuronal apoptosis plays a crucial role in the prognosis of ischemic stroke (Yu et al. 2016).
Despite the advances in understanding the pathophysiology of cerebral ischemia, therapeutic possibilities for acute ischemic stroke remain very limited. Thus, effective prevention and control of cerebral I/R injury is of great clinical importance (Donnan et al. 2008).
Vildagliptin is a selective inhibitor of dipeptidyl peptidase-4 (DPP-4), a membrane-associated peptidase that is widely distributed in body organs exerting different biological activities (Rohnert et al. 2012; Itou et al. 2013). In diabetes management, vildagliptin is relatively more effective than other DPP-4 inhibitors in increasing glucagon-like peptide (GLP)-1 concentration which in turn stimulates pancreatic β cell insulin secretion, decrease hepatic glucose output by the decreased glucagon secretion, decrease insulin resistance, and restore pancreatic β cell mass (Drucker and Nauck 2006; Ahren et al. 2011).
GLP-1 is not only produced in the gut and crosses the blood-brain barrier but is also expressed in the brain and acts on GLP-1R receptors. Vildagliptin ameliorated brain insulin sensitivity and cognitive deficit in insulin-resistant rats (Pipatpiboon et al. 2013; Sa-Nguanmoo et al. 2017). Independent of its anti-diabetic effect, vildagliptin has shown a neuroprotecive effect in an animal model of Parkinson’s disease through its antioxidant and anti-inflammatory activities (Abdelsalam and Safar 2015). It has been reported that gliptins may exert a neuroprotective effect against stroke, independent of GLP-1 receptors (Darsalia et al. 2016).
Besides its neuroprotective effect, vildagliptin has shown a protective effect against animal models of cardiac ischemic-reperfusion injury through reducing the infarct size, antioxidant and anti-apoptotic effects (Chinda et al. 2014; Pongkan et al. 2016; Sivasinprasasn et al. 2017). This raises the possibility that vildagliptin may exert a neuroprotective effect against an animal model of cerebral ischemia independent of its anti-diabetic effect. Thus, the aim of this study is to evaluate the potential neuroprotective effect of vildagliptin in non-diabetic rats with cerebral ischemia and further to explore the role of oxidative stress, inflammation, and brain apoptosis in this protective effect.
Material and methods
Drugs, kits, and chemicals
Vildagliptin was obtained from Novartis Pharma, Basel, Switzerland. Phosphotylinosital 3 kinase (PI3K) enzyme-linked immunosorbant assay (ELISA) kit was purchased from CUSABIO® Biotech Co., Ltd., USA. ELISA Kit for the determination of phosphoryated protein kinase B (pAKT) was obtained from DRG® International, Inc., USA. Rat mechanistic target of rapamycin (mTOR) ELISA Kit was obtained from LifeSpan BioSciences, Inc., USA. All the reagents used during the study were of a high analytical reagent grade.
Animals
A total number of 50 male Wistar rats weighing 150–180 g, 5 months of age were obtained from the Animal House Colony at the National Research Centre (NRC), Egypt. All animal procedures were performed in accordance with ARRIVE guidelines, the Ethics Committee of the National Research Centre, Egypt (registration number 17/097) and the Institutional Animal Care and Use Committee (IACUC), Cairo University (CU-II-F-9-18).
The experimental endpoint was set when the scientific aims and objectives have been reached. During the experimental study, we ensured that pain and distress were minimized. At the end of the study, euthanasia of rats was done by means that induce rapid unconsciousness and death without pain or distress.
Rats were kept at a constant temperature of 25 ± 1 °C, with a 12-h light/dark cycle with food and water ad libitum throughout the experimental period. After acclimatization for 1 week, rats were randomly allocated into five groups. The first group was sham-operated and assigned as the normal group. The second group was subjected to focal cerebral ischemia/reperfusion (I/R) and assigned as the ischemic control group. The third, fourth, and fifth groups were administered vildagliptin by oral gavage (100% w/v) in doses of 2.5, 5, and 10 mg/kg for 3 successive weeks before subjected to left brain I/R and till the end of the study. The dose of vildagliptin was selected according to a prior study by El Batsh et al. (2015).
Surgical procedures of transient focal cerebral ischemia/reperfusion
Overnight fasted rats were anesthetized with 10% chloral hydrate (40 mg/kg, ip) and subjected to either middle cerebral artery occlusion (MCAO) or sham operation. The left middle cerebral artery (MCA) was occluded as described previously with slight modifications (Longa et al. 1989). Briefly, the left carotid region was exposed through a midline cervical incision; the external carotid artery (ECA) and the common carotid artery (CCA) were exposed. A non-traumatic micro-vascular clip was introduced 5 mm caudally from the carotid bifurcation into the internal carotid artery; the clip remained in place and was not removed to ensure the occlusion of the origin of the MCA. The body temperature of rats was maintained at 36.5–37.5 °C throughout the surgery using a heating lamp. After 30 min of occlusion, recirculation was established by gentle withdrawal of the clips. For the rats in the sham group, the left carotid region was only exposed. Finally, the incision was sutured; the animal was allowed to recover from anesthesia. Surgery and neurological deficit scores and analyses were performed by experimenters blinded to the experimental groups. Fifty rats (10 per group) were assessed for neurological deficit score, locomotor activity, and motor coordination then 2 rats were excluded from each group due to high variation in behavioral activity (standard error values exceeds 20% of mean values). Six rats were randomly used for blood pressure recording, determination of blood glucose levels.
Neurological deficit
Neurological deficit scores were evaluated 24 h following reperfusion, using the modified Bederson’s method (Bederson et al. 1986; Yang et al. 1994). The five-point scoring system was used as follows: 0, normal walk, no observable neurological deficit; 1, failure to extend left forepaw; 2, circulating to the left; 3, falling to the left; and 4, no walk with loss of consciousness. Only rats scoring 1–3 points were used to assure successful model establishment.
Behavioral assessment
Assessment of locomotor activity using activity cage
Spontaneous locomotor activity of the rats was measured by using a grid floor activity cage (Model No. 7430, Ugo-Basile, Comerio, Italy) to detect the rat’s movements. Movements by the rat that interrupted infrared beams were automatically detected, and the beam-interruption information was processed by the activity cage software to provide counts of horizontal movements.
Before starting administration with the test drugs, rats were acclimated to the test room for 1 h. Then, each rat was placed individually into the activity cage for a 5-min session and the basal activity counts were recorded. At the end of the session, each rat was gently removed from the activity cage, and then returned to their home cage. The arena was wiped out with a 70% (v/v) alcohol solution in distilled water between sessions to prevent olfactory cues. Twenty-four hours after the last administration of the test drugs, each rat was then re-exposed to the activity apparatus for a 5-min test session and the final activity counts were recorded (Pavic et al. 2007; Yassin et al. 2013).
Assessment of motor coordination using rotarod
Motor coordination of rats was assessed using an accelerating rotarod (Model No. 7750; Ugo Basile), according to the procedure described before (Vijitruth et al. 2006). Rats were given three training sessions on three successive days. All rats were trained on the rotarod apparatus at fixed speed of 4 rotations per minute (rpm) in order to reach a stable performance, before starting treatment with the test drugs. On the fourth day, the rats were placed on the testing rod and the speed of the rotarod started at 4 rpm and then increased gradually to reach 40 rpm over 300 s. The basal falling time for each rat was recorded using a cut off limit of 300 s.
Twenty-four hours after the last administration of the test drugs, each rat was then re-placed on an accelerating rotarod for 300 s test session and the final falling time was recorded.
Body weight changes measurement
The initial body weight of each rat was recorded at the beginning of the experiment and the final body weight was recorded after 24 h following the last treatment. The percent change in body weight was calculated as follows:
% change in body weight = (final body weight -initial body weight/initial body weight) × 100.
Blood pressure recording
Systolic, diastolic blood pressure (BP) and pulse rate of conscious rats were measured at the start and at the end of the experiment. An average of three readings was recorded for each parameter. Animals were restrained in the restrainers for 10–20 min/day for 5 days prior to recording BP in the tail-cuff technique; animals were warmed for 30 min at 29 °C in a thermostatically controlled heating cabinet (Ugo Basile, Italy); for better detection of tail artery pulse, the tail was passed through a cuff and a tail-cuff sensor that was connected to an amplifier (ML 125 NIBP, AD Instruments, Australia). The amplified pulse was recorded during automatic inflation and deflation of the cuff.
Determination of blood glucose levels
Blood glucose levels were measured at a fixed time of the day (from 11 to 12 a.m.) after feeding using a glucometer (Accu-Chek, Roche Diabetes Care, Inc., USA) before the experiment and 24 h following the last treatment. Blood samples were withdrawn from the rats through the orbital plexus, and a drop of blood was placed on the glucometer strip loaded in the apparatus for blood glucose determination.
Euthanasia and brain tissue samplings
After 24 h of the last treatment, all animals were euthanized under decapitation and their brains were removed. Some brain samples were kept on 10% neutral-buffered formalin for further histopathological and immunohistochemical investigations and neuronal cell count. Whereas, other brain samples were cut and the left brain hemispheres were kept at − 80 °C for estimation of malondialdehyde (MDA), reduced gluthathione (GSH), PI3K, pAKT, and mTOR content in brain tissue homogenate.
Biochemical analyses in brain homogenates
Five left brains were homogenized (MPW-120; Medical Instruments, Poland) in 10% (w/v) ice-cold phosphate buffer. Then, the homogenate was centrifuged using a cooling centrifuge (2 k15; Sigma/Laborzentrifugen, Germany) at 4000 rpm for 10 min at − 4 °C and the resulting supernatant was used for determining biochemical parameters.
Determination of MDA brain content
Brain MDA content was determined according to the method described previously (Ruiz-Larrea et al. 1994). In brief, 0.5 ml of the homogenate supernatant were mixed with 4.5 ml of TCA-TBA reagent (20% TCA, and 0.8% TBA, 3:1) and heated for 20 min in a boiling water bath. After cooling, the mixture was then centrifuged at 3000 rpm for 10 min. The supernatant was collected, and the absorbance was read against blank (distilled water instead of sample), at 535 nm. The amount of MDA produced is calculated, using a molar absorption coefficient of 1.56 × 105 M−1 cm−1 and expressed as nanomole/gram tissue.
Determination of GSH brain content
Brain GSH content was determined according to the prior methods (Ellman 1959; Bulaj et al. 1998). In brief, 0.5 ml of the homogenate supernatant was added to 0.5 ml of trichloro-acetic acid 10%. The mixture was vortex-mixed and centrifuged at 4000 rpm/5 min at 4 °C. In a clean test tube; 1.8 ml of phosphate buffer pH 8.0 was added to 0.1 ml of the supernatant and 0.1 ml of Ellman reagent. The absorbance was read at wave length 412 nm after exactly 5 min against blank (distilled water instead of sample). Reduced glutathione levels were calculated using the extinction coefficient of 1.36 × 104 M−1 cm−1. The results were expressed in micromoles GSH/gram tissue.
Determination of PI3K brain content
The quantitative determination of rat PI3K concentrations in brain homogenate was done using commercial ELISA kits and according to the manufacturer instructions.
Determination of pAKT brain content
The concentration of pAKT in brain homogenate was done using commercial ELISA kits and according to the manufacturer instructions.
Determination of mTOR brain content
The brain content of mTOR was measured using commercial ELISA kits and according to the manufacturer instructions.
Histopathological examination
Five brain tissues were collected from each experimental group and were then fixed in 10% neutral-buffered formalin. Afterward, brain samples were processed to get 3–4 μm paraffin-embedded sections and were stained with hematoxylin and eosin (H&E) (Bancroft and Gamble 2008). The infarct size areas were calculated in histopathologically stained sections by an observer blinded to treatment. The infarct area in each animal in the different experimental groups was photographed and the percentage of ischemic lesion areas was represented as the ratio of infarct area to the whole field area under magnification power (× 200) by using Lieca Qwin 500 Image Analyzer (Leica, Cambridge, England).
Neuronal cell count
Brain tissue sections from each experimental group were stained by cresyl violet stain following the methods described before (Park et al. 2012). The brain cortex was examined by an observer blinded to the experimental design in five random fields/section under high magnification power (× 400), and the number of intact neuronal cells and the total number of the neuronal cells were counted using Lieca Qwin 500 Image Analyzer (Leica, Cambridge, England).
Immunohistochemical analysis of caspase-3 in the brain tissues
The immunohistochemical analysis was performed by an investigator blinded to treatments as described before Morgan et al. (2017). In brief, deparaffinization and rehydration were performed to the brain sections. The antigen retrieval was performed by preheating with 10 mM citrate buffer, pH 6.0 for 10 min in microwave. The primary antibody rabbit anti-caspase-3 polyclonal antibody (ab13847; Abcam, Cambridge, UK) at 1:50 dilution was added to the tissue sections for 2 h in a humidified chamber. The tissue sections were incubated with goat anti- rabbit IgG H&L (HRP) (ab205718; Abcam, Cambridge, UK); then, the slides were incubated with 3,3′-diaminobenzidine tetrahydrochloride (DAB, Sigma) for 10 min. Finally, the tissue sections were counterstained with hematoxylin and mounted. The image analyses of the stained sections were performed by Lieca Qwin 500 Image Analyzer (Leica, Cambridge, England). The absolute numbers for the immunopositive cells and total cell number were counted in random 10 microscopic fields/slide under high-power field (× 400) microscope.
Statistical analysis
Data concerning the neurological deficit, locomotor activity and rotarod tests, and biochemical analysis are presented as the mean ± SEM for eight rats per group in the behavioral tests and five rats per group in the biochemical tests. Comparisons between more than two groups regarding the body weight, blood glucose levels, systolic and diastolic blood pressure, pulse rate, and behavioral tests (locomotor activity and rotarod tests) were carried out using two-way analysis of variance (ANOVA) followed by Tukey’s multiple comparisons test, except for neurological deficit score comparison between more than two groups was carried out by one-way ANOVA followed by Newman-Keuls multiple comparison test. Comparisons between more than two groups in biochemical analyses were carried out using one-way ANOVA followed by Tukey’s multiple comparisons test; neuronal cell count comparison was carried out by two-way ANOVA followed by Newman-Keuls multiple comparison test. Immunohistochemical analyses were carried out by one-way ANOVA followed by Newman-Keuls multiple comparison test.
All analyses utilized the GraphPad Prism 6.0 statistical package for Windows (GraphPad, San Diego, CA). Statistical significance was set at p < 0.05.
Results
Effect of vildagliptin on body weight and physiological function of rats before and after ischemia
Tables 1 and 2 reveals that no change in physiological function of rats regarding body weight, blood glucose, systolic and diastolic blood pressure, and pulse rate pre- and post-ischemia in the normal, MCAO, and vildagliptin-treated rats.
Effect of vildagliptin on neurological deficit scores in middle cerebral artery occluded rats
Neurological deficit score was evaluated after 24 h reperfusion following 30 min MCAO (Fig. 1). Sham-operated rats showed no neurological deficit; however, MCAO rats significantly increased neurological deficit score (2.25 ± 0.25) when compared to sham-operated rats (p < 0.05). Vildagliptin pretreatment at doses of 2.5 mg/kg (0.5 ± 0.19), 5 mg/kg (0.25 ± 0.16), and 10 mg/kg (0.38 ± 0.26) significantly reduced neurological deficit score when compared to MCAO rats.
Effect of vildagliptin on neurological deficit score after cerebral I/R injury. Results are expressed as mean ± SEM (n = 8). Statistical analysis was carried out by one-way ANOVA followed by the Newman-Keuls multiple comparison test.*Significant difference from the normal group at p < 0.05. #Significant difference from the control (I/R) group at p < 0.05
Effect of vildagliptin on spontaneous locomotor activity
Table 3 illustrates that all rats showed a significant decrease in their final locomotor activity as compared to their correspondent basal activity. MCAO rats showed a significant decrease in final locomotor activity approximately by 3.95-folds as compared to sham rats, 20.25 counts whereas sham rats was 80.00 counts (p < 0.05). Pretreatment with vildagliptin in doses of 2.5, 5, and 10 mg/kg showed a significant increase in final locomotor activity as compared to MCAO rats, 32.50, 56.88, and 26.25 counts, respectively.
Effect of vildagliptin on motor coordination
As shown in Table 4, no significant change was detected in the basal falling latency time among the different group of rats. Cerebral ischemia induced by MCAO resulted in significant reduction in the final falling latency time, 2.09 min whereas sham rats 4.34 min (p < 0.05). Prior treatment with vildagliptin significantly prolonged the final falling latency time to 3.63, 3.64, and 3.66 min of MCAO rats, respectively.
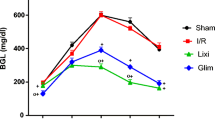
Effect of vildagliptin on biochemical parameters in brain tissue
Induction of cerebral I/R by MCAO resulted in significant elevation in MDA brain content to 277.88 nmol/mg tissue whereas in the sham rats, 205.77 nmol/mg tissue (p < 0.05). Vildagliptin pretreatment in doses of 2.5, 5, and 10 mg/kg had significantly decreased MDA brain contents in MCAO rats to 193.70, 228.53, and 225.48 nmol/mg tissue, respectively (Table 5).
Regarding GSH brain contents as demonstrated in Table 5, MCAO rats significantly reduced GSH brain content to 2.41 μmol/g tissue whereas sham-operated rats 5.46 μmol/g tissue (p < 0.05). Oral pretreatment with vildagliptin significantly elevated brain GSH in MCAO rats to 4.73, 5.02, and 4.88 μmol/g tissue, respectively.
Table 5 depicts that the brain contents of PI3K, p-AKT, and mTOR were significantly reduced following MCAO approximately by 5.14-, 5.68-, and 7.12-folds as compared to sham-operated rats, respectively, 2.50 pg/g, 1.8 U/g, and 0.76 n/g tissue, respectively (p < 0.05).
Interestingly, oral administration of vildagliptin (2.5, 5, 10 mg/kg) to MCAO rats resulted in a significant increase in the brain content of PI3K, p-AKT, and mTOR in a dose-dependent manner. Accordingly, oral administration of vildagliptin in doses of 2.5, 5, and 10 mg/kg to MCAO rats significantly increased PI3K content to 4.83, 6.53, and 8.20 pg/g tissue, respectively. Significant increase in p-AKT contents was assessed after pretreatment of vildagliptin (2.5, 5, 10 mg/kg, p.o.) in MCAO rats to 4.07, 6.17, and 8.4 U/g, respectively. Significant increase in mTOR contents after pretreatment of vildagliptin in doses of 2.5, 5, and 10 mg/kg to MCAO rats was measured to be 2.51, 3.23, and 4.33 n/g, respectively.
Histopathology of the brain
The brain tissue obtained from the normal (sham-operated) group showed no tissue alterations in the cerebral cortex (Fig. 2a), striatum, and hippocampus (Fig. 2f). The cerebral cortex gray matter of the MCAO rats showed multiple eosinophilic neurons with shrunken darkly stained nucleus, shrunken deeply basophilic neurons with pyknotic or lysed nuclei associated with satelitosis, multiple focal areas of gliosis (Fig. 2b), astrogliosis, activation of microglia cell, and swelling of endothelial cells lining blood vessels with perivascular edema. Some cases revealed focal areas of coagulative necrosis with inflammatory cell infiltration. The white matter of the cerebral cortex showed demyelination and axonal fragmentation. The hippocampus showed marked neuronal degeneration of the pyramidal cells with neurophagia (Fig. 2g). The groups treated with different doses of vildagliptin (2.5, 5. 10 mg/kg) showed marked reduction of all previous mentioned brain lesions in a dose-dependent manner as shown in Fig. 2c–j. The percentage of the infarct area in different groups was summarized in Fig. 3. The treated groups with vildagliptin (2.5, 5. 10 mg/kg) showed marked decline in the size of infarct areas when compared with the ischemic brain model (p < 0.05).
The histopathological examination of cerebral cortex and hippocampus in the different groups (H&E × 400). a–e The cerebral cortex; f–j the hippocampus; a and f sham-operated group showing the normal histological picture; b control (I/R) group showing a large area of gliosis with marked cellular dissolution and neuronal degeneration with neurophagia; c the vildagliptin (2.5 mg/kg) group showing moderate number of degenerated neuron; d and e vildagliptin (5 and 10 mg/kg) groups showing marked reduction of degenerated neuron and neurophagia; g the control (I/R) group showing massive degeneration and necrosis of pyramidal cells; h the vildagliptin (2.5 mg/kg) group showing moderate reduction to the number of degenerated pyramidal cells; i and j vildagliptin (5 and 10 mg/kg) groups showing a few number of degenerated pyramidal cells
The percentage of the infarct area is represented as ratio of the infarct area to the whole slide area. Statistical analysis was carried out by one-way ANOVA followed by Newman-Keuls Multiple Comparison test.*Significant difference from the normal group at p < 0.05. #Significant difference from the control (I/R) group at p < 0.05
The neuronal cell count
As shown in Fig. 4, the histopathological examination of the cerebral cortex with cresyl violet stain revealed normal neuronal morphology with clear vesicular nucleus of the normal control group. The control (I/R) group showed a large number of shrunken darkly stained cells. The percentage of the intact neurons in different groups was summarized in Fig. 4f. The ischemic brain model showed significant reduction in percentage of intact cells compared to the sham normal group (p < 0.05). The treated groups with vildagliptin showed a significant elevation of the number of intact neuronal cells in a dose-dependent manner compared to the ischemic group.
Cresyl violet staining of different groups (× 400) the intact neuronal cell (black arrow), the degenerated neuronal cell (yellow arrow). a The sham-operated group; b the ischemic model; c the vildagliptin (2.5 mg/kg) group; d the vildagliptin (5 mg/kg) group; e the vildagliptin (10 mg/kg) group; f the scatter plots represents the numbers of intact neurons and necrotic neuronal cells. Results are expressed as mean ± SEM (n = 5). Statistical analysis was carried out by two-way ANOVA followed by the Newman-Keuls Multiple Comparison test.*Significant difference from normal group necrotic cells at p < 0.05. #Significant difference from control (I/R) group necrotic cells at p < 0.05. §Significant difference from normal group intact cells at p < 0.05. †Significant difference from control (I/R) group intact cells at p < 0.05
Immunohistochemistry of caspase-3
The results of immunohistochemical analysis of caspase-3 expression in the normal, control (I/R), and different doses of vildagliptin treated groups were summarized in Fig. 5. Caspase-3 immunostaining pattern was homogenous staining in both the cytoplasm and nucleus of the neurons and glial cells. The percentage of caspase-3 immunopositive cells of the control (I/R) group (Fig. 5b) was significantly higher than the normal group and drug treated groups (p < 0.05). Vildagliptin treated groups (2.5, 5, 10 mg/kg) revealed significant reduction in the percentage of caspase-3 immunopositive cells in a dose-dependent manner compared to the control (I/R) group (Fig. 5c, d, e).
Representative casepase-3 immunohistochemistry in the cerebral cortex of different experimental groups (× 400). a The SHAM-operated group showing weak immunoreactivity; b the MCAO rat model showing intense number of immunopositive cells; c the vildagliptin (2.5 mg/kg) group showing moderate number of immunostained cells; (d) the vildagliptin (5 mg/kg) group; and (e) the vildagliptin (10 mg/kg) group showing marked reduction in casepase-3 immunopositive cells. Statistical analysis was carried out by one-way ANOVA followed by the Newman-Keuls Multiple Comparison test.*Significant difference from the normal group at p < 0.05. #Significant difference from the control (I/R) group at p < 0.05
Discussion
This study imparts novel evidence on the neuroprotective effect of vildagliptin (2.5, 5, 10 mg/kg) in a dose-dependent manner in MCAO rats as manifested in attenuation of the infarct area, neuronal cell loss, and histopathological damage. According to the authors’ knowledge, this is the first research to demonstrate the involvement of neurological deficit scores, behavioral alterations, oxidative stress, PI3K/pAKT/mTOR pathway, apoptosis, and histopathological changes in the neuroprotective effect of vildagliptin in the MCAO rat model.
In this study, body weight change, blood glucose, pulse rate, and systolic and diastolic blood pressure of normal, MCAO, and vildagliptin pretreated rats was stable before and after MCAO, indicating stable physiological function. This finding rolls out any side effect that may interfere with the protective effect of vildagliptin in MCAO rats and suggests that the effect of vildagliptin on blood glucose level is dependent on the diabetic status. In line with this finding, prior study showed that vildagliptin did not alter body weight and metabolic parameters in non-diabetic rats (El Batsh et al. 2015).
Middle carotid artery occlusion as a cerebral I/R model in rats resulted in deficit in neurological score, reduction in the final locomotor activity in the activity cage test, and motor incoordination in rotarod test after 24 h of reperfusion. This finding is in agreement with previous studies (Briyal et al. 2014; Mohamed et al. 2016; Zhao et al. 2016) and reflects severe neurological and motor dysfunctions in MCAO rats. Pretreatment with vildagliptin for 21 days significantly reduced neurological deficit score, increased final locomotor activity, and improved motor coordination as compared to MCAO rats. This finding is in accordance with prior research which showed that vildagliptin exerted neuroprotective effect and improved motor performance in rotenone Parkinson disease in rats (Abdelsalam and Safar 2015). In this work, all rats including MCAO rats and vildagliptin pretreated rats showed a marked reduction in their final locomotor activity compared to their corresponding basal activity, which may have resulted from habituation to the activity cage apparatus.
It is well established that ischemic stroke is associated with oxidative stress due to overproduction of reactive oxygen species (ROS) during ischemia that attacks lipids and proteins and causes DNA damage in ischemic brain tissue (Gong et al. 2014; Wang et al. 2016; Pan et al. 2017). In harmony with prior studies (Liu et al. 2015; Ye et al. 2016), our findings revealed that MCAO rats increased brain MDA content, an end product of lipid peroxidation and subsequently reduced brain GSH content, an endogenous antioxidant enzyme. This implies that oxidative stress mediated neurological dysfunction in MCAO rats. Vildagliptin-pretreated rats significantly reduced MDA and increased GSH brain contents when compared to MCAO rats, indicating that the antioxidant activity of vildagliptin mediated its neuroprotective effect in MCAO rats. Consistent with these findings, vildagliptin exerted a neuroprotective effect in vascular dementia and obese-insulin resistance through its antioxidant effect (Jain and Sharma 2015; Sa-Nguanmoo et al. 2017).
It is well established that PI3K/Akt pathway plays an essential role in mediating the intracellular signal transduction pathway involved in regulation of cellular metabolism, proliferation, inflammation, growth, and survival. Activated PI3K resulted in upregulation of p-Akt which is crucial for neuronal survival and growth (Liu et al. 2012; Kim et al. 2014; Wu et al. 2018). Likewise, mTOR is a major component in the downstream of the PI3K/Akt pathway. It regulates protein synthesis, neuronal regeneration, growth, survival, angiogenesis, and synaptic plasticity (Saxton and Sabatini 2017; Switon et al. 2017).
In this study, MCAO rats showed a significant decrease in PI3K, pAKT, and mTOR brain contents at 48 h after reperfusion. This finding is in harmony with previous studies of Chong et al. (2012)) and Li et al. (2015)) and reveals that cerebral ischemia resulted in inactivation of the PI3K/AKT/mTOR pathway and subsequently neuronal loss and dysfunction.
It has been previously documented that elevation of ROS inhibits phosphorylation of AKT and activation of mTOR (Maiese et al. 2013; Yoshino et al. 2015). Hence, in the current study, elevated oxidative stress may have resulted in inactivation of the PI3K/AKT/mTOR pathway in MCAO rats. Vildagliptin-pretreated rats showed a significant increase in PI3K, pAKT, and mTOR brain contents at 48 h after reperfusion when compared to MCAO rats. This suggests that vildagliptin exerted its neuroprotective effect against cerebral ischemia by activating the PI3K/AKT/mTOR pathway which may be probably via its antioxidant activity. It has been previously reported that vildagliptin attenuated diabetic neuropathy in diabetic rodents by activation of pAKT (Tsuboi et al. 2016). Also, pretreatment with vildagliptin in obese pre-diabetic rats reduced infarct size by activation of the pAKT/PKB pathway (Huisamen et al. 2011).
This study shows that MCAO rats significantly increased caspase-3 protein expression when compared to normal rats, indicating that cell apoptosis mediated neuronal dysfunction and neuronal loss following cerebral ischemia.
In agreement with prior studies, oxidative stress and inactivation of the PI3K/AKT/mTOR pathway resulted in elevated production of the apoptotic marker, caspase-3 following cerebral ischemia (Chen et al. 2012; Huang et al. 2014). Therefore, in the current study, MCAO rats induced cell apoptosis probably via oxidative stress and inactivation of the PI3K/AKT/mTOR pathway. Vildagliptin-pretreated rats showed a significant decrease in protein expression of caspase-3 brain content when compared to MCAO rats. This finding shows that vildagliptin exerted neuroprotection in MCAO rats via its anti-apoptotic effect. Consistent with this finding, it has been reported that vildagliptin exerted neuroprotective effect in rotenone-induced Parkinson’s disease via its anti-apoptotic effect (Abdelsalam and Safar 2015). Also, Chinda et al. (2014) showed that vildagliptin reduces infarct size through decreasing apoptotic Bax, increasing anti-apoptotic Bcl-2 proteins in myocardial infarction.
It has been previously documented that activation of the PI3K/AKT/mTOR pathway results in inhibition of apoptosis via the activation of multiple downstream signaling molecules (Liang et al. 2014; Shen et al. 2017). pAKT inhibits apoptosis via phosphorylation of pro-apoptotic Bcl-2-related protein, BAD, pro-apoptotic protein caspase 9, and forkhead transcription factor FoxO3a that restricts cell growth, and therefore regulate cell survival. (Maiese et al. 2008). All these proteins finally contribute to the decrease in caspase-3 final end product of the apoptotic pathway.
mTOR inhibits apoptosis and is dependent on AKT phosphorylation. Prior study reported that mTOR required pAKT through inhibiting FoxO3a (Guertin et al. 2006). Also, direct inhibition of mTOR by rapamycin elevated caspase-3 leading to neuronal apoptosis in hypoxia ischemia injury (Chen et al. 2012). Therefore, vildagliptin exerted its anti-apoptotic effect in this study probably by its antioxidant effect and activation of the PI3K/AKT/mTOR pathway.
In the current study, MCAO rats showed histopathological changes and significant reduction in infarct area, and number of necrotic neuronal cells compared to sham-operated rats. The Cresyl violet method is a well-known histological method to detect cell damage in the central nervous system (Alvarez-Buylla et al. 1990; Kosaraju et al. 2013). This finding further implies the neuronal cell damage in MCAO rats as manifested in loss in neuronal counts and histopathological alterations and is in harmony with prior studies (Lee et al. 2010; Park et al. 2012).
Pretreatment with vildagliptin in doses of 2.5, 5, and 10 mg/kg showed a dose-dependent reduction in infarct area, preservation in neuronal cell count and histopathological examination. These findings correlate the neuroprotective effect of vildagliptin with its reversal of biochemical and immunohistochemical changes.
Conclusion
It can be concluded that vildagliptin exerted a neuroprotective effect in MCAO rats, evidenced by enhancement of neurological, motor deficits, improvement in the histopathological profile, reduction in infarct area, and preservation of neuronal cell counts which may be probably mediated by its antioxidant effect, activation of the PI3K/AKT/mTOR pathway, and anti-apoptotic activity. Further studies are warranted to deduce the exact molecular mechanisms involved in the neuroprotective effect of vildagliptin in MCAO rats.
References
Abdelsalam RM, Safar MM (2015) Neuroprotective effects of vildagliptin in rat rotenone Parkinson’s disease model: role of RAGE-NFkappaB and Nrf2-antioxidant signaling pathways. J Neurochem 133:700–707
Ahren B, Schweizer A, Dejager S, Villhauer EB, Dunning BE, Foley JE (2011) Mechanisms of action of the dipeptidyl peptidase-4 inhibitor vildagliptin in humans. Diabetes Obes Metab 13:775–783
Alvarez-Buylla A, Ling CY, Kirn JR (1990) Cresyl violet: a red fluorescent Nissl stain. J Neurosci Methods 33:129–133
Bancroft JD, Gamble M (2008) Theory and practice of histological techniques. Elsevier Health Sciences, Oxford
Bederson JB, Pitts LH, Tsuji M, Nishimura MC, Davis RL, Bartkowski H (1986) Rat middle cerebral artery occlusion: evaluation of the model and development of a neurologic examination. Stroke 17:472–476
Briyal S, Shah S, Gulati A (2014) Neuroprotective and anti-apoptotic effects of liraglutide in the rat brain following focal cerebral ischemia. Neuroscience 281:269–281
Bulaj G, Kortemme T, Goldenberg DP (1998) Ionization-reactivity relationships for cysteine thiols in polypeptides. Biochemistry 37:8965–8972
Bustamante A, Garcia-Berrocoso T, Rodriguez N, Llombart V, Ribo M, Molina C, Montaner J (2016) Ischemic stroke outcome: a review of the influence of post-stroke complications within the different scenarios of stroke care. Eur J Intern Med 29:9–21
Chen H, Qu Y, Tang B, Xiong T, Mu D (2012) Role of mammalian target of rapamycin in hypoxic or ischemic brain injury: potential neuroprotection and limitations. Rev Neurosci 23:279–287
Chinda K, Sanit J, Chattipakorn S, Chattipakorn N (2014) Dipeptidyl peptidase-4 inhibitor reduces infarct size and preserves cardiac function via mitochondrial protection in ischaemia-reperfusion rat heart. Diab Vasc Dis Res 11:75–83
Chong ZZ, Shang YC, Wang S, Maiese K (2012) A critical kinase cascade in neurological disorders: PI 3-K, Akt, and mTOR. Future Neurol 7:733–748
Darsalia V, Larsson M, Lietzau G, Nathanson D, Nystrom T, Klein T, Patrone C (2016) Gliptin-mediated neuroprotection against stroke requires chronic pretreatment and is independent of glucagon-like peptide-1 receptor. Diabetes Obes Metab 18:537–541
Donnan GA, Fisher M, Macleod M, Davis SM (2008) Stroke. Lancet 371:1612–1623
Drucker DJ, Nauck MA (2006) The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet 368:1696–1705
El Batsh MM, El Batch MM, Shafik NM, Younos IH (2015) Favorable effects of vildagliptin on metabolic and cognitive dysfunctions in streptozotocin-induced diabetic rats. Eur J Pharmacol 769:297–305
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82:70–77
Gong G, Xiang L, Yuan L, Hu L, Wu W, Cai L, Yin L, Dong H (2014) Protective effect of glycyrrhizin, a direct HMGB1 inhibitor, on focal cerebral ischemia/reperfusion-induced inflammation, oxidative stress, and apoptosis in rats. PLoS One 9:e89450
Guertin DA, Stevens DM, Thoreen CC, Burds AA, Kalaany NY, Moffat J, Brown M, Fitzgerald KJ, Sabatini DM (2006) Ablation in mice of the mTORC components raptor, rictor, or mLST8 reveals that mTORC2 is required for signaling to Akt-FOXO and PKCalpha, but not S6K1. Dev Cell 11:859–871
Huang H, Zhong R, Xia Z, Song J, Feng L (2014) Neuroprotective effects of rhynchophylline against ischemic brain injury via regulation of the Akt/mTOR and TLRs signaling pathways. Molecules 19:11196–11210
Huisamen B, Genis A, Marais E, Lochner A (2011) Pre-treatment with a DPP-4 inhibitor is infarct sparing in hearts from obese, pre-diabetic rats. Cardiovasc Drugs Ther 25:13–20
Iadecola C, Anrather J (2011) The immunology of stroke: from mechanisms to translation. Nat Med 17:796–808
Itou M, Kawaguchi T, Taniguchi E, Sata M (2013) Dipeptidyl peptidase-4: a key player in chronic liver disease. World J Gastroenterol 19:2298–2306
Jain S, Sharma B (2015) Neuroprotective effect of selective DPP-4 inhibitor in experimental vascular dementia. Physiol Behav 152:182–193
Jin R, Liu L, Zhang S, Nanda A, Li G (2013) Role of inflammation and its mediators in acute ischemic stroke. J Cardiovasc Transl Res 6:834–851
Kim M, Shin MS, Lee JM, Cho HS, Kim CJ, Kim YJ, Choi HR, Jeon JW (2014) Inhibitory effects of isoquinoline alkaloid Berberine on ischemia-induced apoptosis via activation of phosphoinositide 3-kinase/protein kinase B signaling pathway. Int Neurourol J 18:115–125
Kosaraju J, Gali CC, Khatwal RB, Dubala A, Chinni S, Holsinger RM, Madhunapantula VS, Muthureddy Nataraj SK, Basavan D (2013) Saxagliptin: a dipeptidyl peptidase-4 inhibitor ameliorates streptozotocin induced Alzheimer's disease. Neuropharmacology 72:291–300
Lakhan SE, Kirchgessner A, Hofer M (2009) Inflammatory mechanisms in ischemic stroke: therapeutic approaches. J Transl Med 7:97
Lee C, Moon S, Yoo K, Choi J, Park O, Hwang I, Sohn Y, Moon J, Cho J, Won M (2010) Long-term changes in neuronal degeneration and microglial activation in the hippocampal CA1 region after experimental transient cerebral ischemic damage. Brain Res Bull 1342:138–149
Li W, Yang Y, Hu Z, Ling S, Fang M (2015) Neuroprotective effects of DAHP and Triptolide in focal cerebral ischemia via apoptosis inhibition and PI3K/Akt/mTOR pathway activation. Front Neuroanat 9:48
Liang K, Ye Y, Wang Y, Zhang J, Li C (2014) Formononetin mediates neuroprotection against cerebral ischemia/reperfusion in rats via downregulation of the Bax/Bcl-2 ratio and upregulation PI3K/Akt signaling pathway. J Neurol Sci 344:100–104
Liu H, Liu X, Wei X, Chen L, Xiang Y, Yi F, Zhang X (2012) Losartan, an angiotensin II type 1 receptor blocker, ameliorates cerebral ischemia-reperfusion injury via PI3K/Akt-mediated eNOS phosphorylation. Brain Res Bull 89:65–70
Liu Y, Zhang L, Liang J (2015) Activation of the Nrf2 defense pathway contributes to neuroprotective effects of phloretin on oxidative stress injury after cerebral ischemia/reperfusion in rats. J Neurol Sci 351:88–92
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 20:84–91
Maiese K, Chong ZZ, Shang YC (2008) OutFOXOing disease and disability: the therapeutic potential of targeting FoxO proteins. Trends Mol Med 14:219–227
Maiese K, Chong ZZ, Shang YC, Wang S (2013) mTOR: on target for novel therapeutic strategies in the nervous system. Trends Mol Med 19:51–60
Mohamed RA, Agha AM, Abdel-Rahman AA, Nassar NN (2016) Role of adenosine A2A receptor in cerebral ischemia reperfusion injury: signaling to phosphorylated extracellular signal-regulated protein kinase (pERK1/2). Neuroscience 314:145–159
Morgan A, Galal MK, Ogaly HA, Ibrahim MA, Abd-Elsalam RM, Noshy P (2017) Tiron ameliorates oxidative stress and inflammation in titanium dioxide nanoparticles induced nephrotoxicity of male rats. Biomed Pharmacother 93:779–787
Pan L, Zhou Y, Li XF, Wan QJ, Yu LH (2017) Preventive treatment of astaxanthin provides neuroprotection through suppression of reactive oxygen species and activation of antioxidant defense pathway after stroke in rats. Brain Res Bull 130:211–220
Park OK, Choi JH, Park JH, Kim IH, Yan BC, Ahn JH, Kwon SH, Lee JC, Kim YS, Kim M, Kang IJ, Kim JD, Lee YL, Won MH (2012) Comparison of neuroprotective effects of five major lipophilic diterpenoids from Danshen extract against experimentally induced transient cerebral ischemic damage. Fitoterapia 83:1666–1674
Paulson OB (1971) Cerebral apoplexy (stroke): pathogenesis, pathophysiology and therapy as illustrated by regional blood flow measurements in the brain. Stroke 2:327–360
Pavic R, Tvrdeic A, Tot OK, Heffer-Lauc M (2007) Activity cage as a method to analyze functional recovery after sciatic nerve injury in mice. Somatosens Mot Res 24:213–219
Pipatpiboon N, Pintana H, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2013) DPP4-inhibitor improves neuronal insulin receptor function, brain mitochondrial function and cognitive function in rats with insulin resistance induced by high-fat diet consumption. Eur J Neurosci 37:839–849
Pongkan W, Pintana H, Jaiwongkam T, Kredphoo S, Sivasinprasasn S, Chattipakorn SC, Chattipakorn N (2016) Vildagliptin reduces cardiac ischemic-reperfusion injury in obese orchiectomized rats. J Endocrinol 231:81–95
Rohnert P, Schmidt W, Emmerlich P, Goihl A, Wrenger S, Bank U, Nordhoff K, Tager M, Ansorge S, Reinhold D, Striggow F (2012) Dipeptidyl peptidase IV, aminopeptidase N and DPIV/APN-like proteases in cerebral ischemia. J Neuroinflammation 9:44
Ruiz-Larrea MB, Leal AM, Liza M, Lacort M, de Groot H (1994) Antioxidant effects of estradiol and 2-hydroxyestradiol on iron-induced lipid peroxidation of rat liver microsomes. Steroids 59:383–388
Sa-Nguanmoo P, Tanajak P, Kerdphoo S, Jaiwongkam T, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2017) SGLT2-inhibitor and DPP-4 inhibitor improve brain function via attenuating mitochondrial dysfunction, insulin resistance, inflammation, and apoptosis in HFD-induced obese rats. Toxicol Appl Pharmacol 333:43–50
Saxton RA, Sabatini DM (2017) mTOR signaling in growth, metabolism, and disease. Cell 168:960–976
Shen M, Wang S, Wen X, Han XR, YJ W, XM Z, MH Z, DM W, YL Z (2017) Dexmedetomidine exerts neuroprotective effect via the activation of the PI3K/Akt/mTOR signaling pathway in rats with traumatic brain injury. Biomed Pharmacother 95:885–893
Sivasinprasasn S, Tanajak P, Pongkan W, Pratchayasakul W, Chattipakorn SC, Chattipakorn N (2017) DPP-4 inhibitor and estrogen share similar efficacy against cardiac ischemic-reperfusion injury in obese-insulin resistant and estrogen-deprived female rats. Sci Rep 7:44306
Switon K, Kotulska K, Janusz-Kaminska A, Zmorzynska J, Jaworski J (2017) Molecular neurobiology of mTOR. Neuroscience 341:112–153
Tsuboi K, Mizukami H, Inaba W, Baba M, Yagihashi S (2016) The dipeptidyl peptidase IV inhibitor vildagliptin suppresses development of neuropathy in diabetic rodents: effects on peripheral sensory nerve function, structure and molecular changes. J Neurochem 136:859–870
Vijitruth R, Liu M, Choi D, Nguyen X, Hunter R, Bing G (2006) Cyclooxygenase-2 mediates microglial activation and secondary dopaminergic cell death in the mouse MPTP model of Parkinson’s disease. J Neuroinflammation 3:6
Wang S, Xu H, Xin Y, Li M, Fu W, Wang Y, Lu Z, Yu X, Sui D (2016) Neuroprotective effects of Kaempferide-7-O-(4″-O-acetylrhamnosyl)-3-O-rutinoside on cerebral ischemia-reperfusion injury in rats. Eur J Pharmacol 788:335–342
Wu J, Wang R, Yang D, Tang W, Chen Z, Sun Q, Liu L, Zang R (2018) Hydrogen postconditioning promotes survival of rat retinal ganglion cells against ischemia/reperfusion injury through the PI3K/Akt pathway. Biochem Biophys Res Commun 495:2462–2468
Yang G, Chan PH, Chen J, Carlson E, Chen SF, Weinstein P, Epstein CJ, Kamii H (1994) Human copper-zinc superoxide dismutase transgenic mice are highly resistant to reperfusion injury after focal cerebral ischemia. Stroke 25:165–170
Yassin N, El-Shenawy S, Mahdy KA, Gouda N, Marrie A, Farrag A, Ibrahim BM (2013) Effect of Boswellia serrata on Alzheimer’s disease induced in rats. J Arab Soc Med Res 8:1–11
Ye Y, Li J, Cao X, Chen Y, Ye C, Chen K (2016) Protective effect of n-butyl alcohol extracts from Rhizoma Pinelliae Pedatisectae against cerebral ischemia-reperfusion injury in rats. J Ethnopharmacol 188:259–265
Yoshino Y, Ishisaka M, Tsujii S, Shimazawa M, Hara H (2015) Glucagon-like peptide-1 protects the murine hippocampus against stressors via Akt and ERK1/2 signaling. Biochem Biophys Res Commun 458:274–279
Yu Z, Cai M, Xiang J, Zhang Z, Zhang J, Song X, Zhang W, Bao J, Li W, Cai D (2016) PI3K/Akt pathway contributes to neuroprotective effect of Tongxinluo against focal cerebral ischemia and reperfusion injury in rats. J Ethnopharmacol 181:8–19
Zhao Q, Cheng X, Wang X, Wang J, Zhu Y, Ma X (2016) Neuroprotective effect and mechanism of Mu-Xiang-You-Fang on cerebral ischemia-reperfusion injury in rats. J Ethnopharmacol 192:140–147
Author information
Authors and Affiliations
Contributions
SA conceived and designed the research. SA and RF conducted pharmacological and biochemical analyses, and RM conducted and observed histopathological and immunohistochemical analyses. SA, RF, and RM wrote the manuscript. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
All animal procedures were approved by the Ethics Committee of the National Research Centre, Egypt (registration number 17/097) and, Institutional Animal Care and Use Committee (IACUC), Cairo University (CU-II-F-9-18).
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
El-Marasy, S.A., Abdel-Rahman, R.F. & Abd-Elsalam, R.M. Neuroprotective effect of vildagliptin against cerebral ischemia in rats. Naunyn-Schmiedeberg's Arch Pharmacol 391, 1133–1145 (2018). https://doi.org/10.1007/s00210-018-1537-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1537-x