Abstract
Type 2 diabetes mellitus (T2DM) is a major risk factor for ischemic stroke accompanied by vascular dysfunction and poor cerebrovascular outcome. Lixisenatide is a glucagon like peptide-1 (GLP-1) analog that is recently used for T2DM treatment with established neuroprotective properties. This study investigated and compared the neuroprotective effect of lixisenatide against glimepiride on diabetic rats subjected to global cerebral ischemia/reperfusion (I/R) injury. T2DM-induced adult male Wistar rats were administered lixisenatide or glimepiride prior to induction of global cerebral I/R-induced injury. Results showed a disturbance in oxidative stress parameters (catalase, reduced glutathione, and malondialdehyde) along with increasing in caspase-3 and tumor necrosis factor-alpha protein expressions in ischemic diabetic brain tissues. An upregulation of protein level of inducible nitric oxide (iNOS) synthase and nicotinamide adenine dinucleotide phosphate (NADPH) oxidase subunit, NOX2 gene expression associated with significant suppression of endothelial nitric oxide synthase (eNOS) protein expression are recorded in carotid arteries of diabetic I/R-injured rats. Apart from ameliorating glucose intolerance and insulin resistance, lixisenatide was found to be superior to glimepiride as protective treatment in terms of enhancing behavioral/neurological functions and suppressing cerebral oxidative stress, inflammation, and apoptosis in cerebral I/R-injured diabetic rats. Unlike glimepiride, lixisenatide relieved carotid endothelial dysfunction by increasing eNOS expression. It also dampened vascular nitrosative/oxidative stress via suppression of iNOS and NADPH oxidase expressions. This study supposed that lixisenatide represents a more suitable anti-diabetic therapy for patients who are at risk of ischemic stroke, and even so, the mechanisms of lixisenatide-mediated vascular protection warrant further experimental and clinical investigations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is a leading cause of disability that is often complicated with one or more co-morbid diseases (Sidney et al. 2016). Type 2 diabetes mellitus (T2DM) is considered one of the most common co-morbid diseases which increases the risk and severity of the ischemic stroke (Luitse et al. 2012). Patients with T2DM have 2- to 6-fold increase in the risk of stroke with greater recurrence and higher mortality rates than non-diabetic patients (Sander and Kearney 2009). T2DM is characterized by hyperglycemia, insulin resistance, oxidative stress, and endothelial dysfunction which significantly exacerbates cerebral injury and worsens stroke outcome through multifactorial pathways (Duarte et al. 2013; Palomares et al. 2012). Cerebral blood flow (CBF) is significantly reduced along with T2DM-induced hyperglycemia due to modulation of vasculature and vasoactive mediators specially endothelium-derived nitric oxide (Gonzalez-Moreno et al. 2014). It is notable that the persistent reduction in CBF contributes to poor outcome and recovery in patient with ischemic stroke (Coucha et al. 2013; Yuh et al. 2017). However, less attention is devoted to elucidate the underlying mechanisms of T2DM-induced vascular dysfunction in stroke.
The evidence that hyperglycemia associated with T2DM exacerbates neuronal death and increases infarct size in stroke patients (Gonzalez-Moreno et al. 2014) leads to the notion that tight glycemic control could protect against those injuries. Indeed, normalization of blood glucose level using insulin had been shown to ameliorate damage in the animal model of global cerebral ischemia (Van den Berghe et al. 2005). Even though the clinical evaluation of insulin therapy in stroke patients showed conflicting results which suggests that the approach of glycemic control via insulin therapy should be revised (Piironen et al. 2012).
Clinically, glucagon-like peptide-1 receptor (GLP-1R) agonists are newly developed anti-T2DM agents with reported efficacy in controlling blood glucose level, improving glucose and lipid metabolism, and decreasing insulin resistance (Lovshin 2017). It was shown that in response to plasma glucose pathologic alteration, glucagon-like peptide 1 (GLP-1) reduces brain glucose level fluctuation by regulating brain vasculature (Gejl et al. 2012). Lixisenatide is a new potent and selective GLP-1R agonist that has been recently released onto the market Sanofi New Drug Application for Lixisenatide Accepted for Review by FDA (2013). In both experimental and clinical researches, lixisenatide is proven to be more potent with rapid onset and sustained duration of action compared with other GLP-1R agonist counterparts (Horowitz et al. 2013; Werner et al. 2010). Once daily lixisenatide improves glycemic control via enhancing insulin biosynthesis and stimulation of β-cell proliferation (Werner et al. 2010). Glimepiride was chosen as therapeutic comparator in this study which is a once-daily sulfonylurea antidiabetic agent that acts through enhancing insulin secretion from β cells by different mechanisms (Kramer et al. 1996). Mechanisms involved either pancreatic via acting on ATP-sensitive potassium (Katp) or extra-pancreatic via increasing glucose transport and glucose transporter expression (GLUT1 and GLUT4) (Langtry and Balfour 1998).
To our knowledge, no previous studies have verified the protective effects of lixisenatide, as a GLP-1R agonist, on global cerebral ischemia-reperfusion (I/R) injury in diabetic rats. Accordingly, the present study aimed to investigate the efficacy of lixisenatide, compared with a standard anti-diabetic drug (glimepiride), in the protection against cerebral I/R-induced injury in diabetic rats.
Materials and methods
Chemicals
Lixisenatide and glimepiride were obtained from Sanofi-Aventis (Germany). Streptozotocin (STZ) and 2,3,5-triphenyltetrazolium chloride, 2-thiobarbituric acid (TTC) stain were purchased from Sigma-Aldrich (St. Louis, MO, USA). Polyclonal rabbit/anti-rat primary antibodies against caspase-3, tumor necrosis factor-alpha (TNF-α), endothelial nitric oxide synthase (eNOS), and inducible nitric oxide synthase (iNOS) were purchased from Thermo Fischer Scientific Inc. /Lab Vision (Fermont, CA, USA).
Animals and T2DM induction
Adult male Wistar rats (8 weeks of age) weighing 200–250 g each were housed under controlled environmental conditions (temperature 27 ± 2 °C and 12-h day/night cycle) and were allowed for an acclimatization period at least 1 week prior to testing. Animals were fed high-fat diet (HFD) for a period of 2 weeks and are permitted free access to tap water. The diet composition is 265-g powdered normal pellet diet, 313 g beef fat (suet), 250 g casein, 10 g cholesterol, 60 g vitamins and mineral mixture, 1 g yeast powder, and 1 g sodium chloride per kg (Srinivasan et al. 2005).
After the 2 weeks of dietary manipulation, rats were injected intraperitoneally with STZ (35 mg/kg). Three days after STZ injection, rats that had blood glucose level (BGL) of ≥ 300 mg/dl were considered diabetic and included in the study. Then, the selected rats were allowed to continue to feed on their respective diets for 4 weeks to induce a late stage of T2DM before drug treatment.
Drug treatments and induction of cerebral I/R injury
Diabetic rats were divided into four groups, each containing eight rats. Prior to induction of cerebral I/R injury, animals received treatment for 14 days in the following regimen; the first group is control and served as sham operated. Group 2 received only vehicle. Group 3 received lixisenatide (1 nmole/kg/day, i.p.). Group 4 received glimepiride (2 mg/kg/day, p.o.). The dose regimens of drug treatment were selected according to our preliminary studies and according to previous studies (McClean and Holscher 2014; Nade et al. 2015).
After 14 days of drug treatment, groups 2, 3, and 4 were subjected to cerebral I/R injury which was induced by bilateral clamping of the common carotid arteries of anesthetized rats (50 mg/kg ketamine and 10 mg/kg xylazine, i.p.) for 30 min using non-traumatic artery clamps. Reperfusion was allowed for 24 h by releasing the clamps and restoration of blood flow in the carotid arteries (Seif-el-Nasr and Fahim 2001).
A mortality of 0–2 rats was observed in each group. All animals’ procedures were performed in accordance Animal Care Community, Minia University, Egypt (Permit Number: MPH-12-015) in strict accordance with the international policies (Guide for Care and Use of Laboratory Animals published by the US National Institute of Health; NIH Publication No. 85-23, revised 1996).
Measurement of glucose tolerance
After treatment completion, before induction of I/R injury, animals were allowed to fast overnight. Glucose (2 g/kg) was given by stomach tube to all animal groups. Blood was drawn from tail vein at 0, 30, 60, and 120 min and assayed for blood glucose level using One-Touch Ultra 2 glucometer. Insulin resistance assessment by homeostatic assay (HOMA-IR) was calculated using the following equation: HOMA-IR = glucose concentration (mmol/L) × insulin (μU/L)/22.5 (Matthews et al. 1985).
Behavioral and neurological outcome measures
The open field test (OFT) was performed at 24 h after induction of cerebral I/R injury to measure spontaneous activity in rats. Briefly, each rat was placed in a wooden box (72 × 72 × 36 cm) whose bottom divided equally into 16 squares. During a period of 3 min, frequency of ambulation (the number of squares crossed with the four paws) and rearing (posture sustained with hind-paw) were recorded by video camera and counted manually (Abdelkader et al. 2017). Moreover, the neurological defect was evaluated by scoring six individual tests which are spontaneous activity, symmetry in the movement of the four limbs, forepaw outstretching, climbing, body proprioception, and response to vibrissae touch. The summation of the neurological score is ranged from 5 to 18 (Garcia et al. 1995).
Blood sampling and tissue preparation
Blood samples were collected via cardiac puncture then centrifuged for 10 min at 3000 rpm. Serum samples (about 2 ml of each animal) were stored at − 80 °C for further analysis.
After rat sacrification, carotid artery segments were excised and deep frozen in liquid nitrogen, then stored at − 80 °C for further analysis. Additionally, whole brains were removed, rinsed with ice-cold saline and divided into two sets. The first set (6–8 brains) were used for analysis of infarct volume. The other set (6–8 brains) was divided sagittally into two halves; one halves were rapid frozen in liquid nitrogen and stored in − 80 °C for biochemical and Western blotting analysis. The other halves were fixed in 4% paraformaldehyde for histopathological analysis.
Biochemical analysis
Serum samples were used for assays of triglycerides (TG) and low density lipoprotein cholesterol (LDL-C), using available commercial kits according to manufacturer instructions purchased from Biodiagnostic (Egypt). The blood level of insulin was measured with insulin enzyme-linked immunosorbent assay (ELISA) kit obtained from Chemux BioScience (San Francisco, USA).
For biochemical measurements, brain tissues were homogenized in 0.05 M phosphate buffer saline (PBS, pH 7.4) and then centrifuged at 10,000 rpm for 10 min at 4 °C. The resulted supernatants were used for the assay of brain malondialdehyde (MDA), reduced glutathione (GSH) contents, and catalase activity using colorimetric kits according to instruction of manufacture (Biodiagnostic, Egypt).
Western blotting analysis
Western blotting analysis was used to detect protein expression of caspase-3 and TNF-α in brain tissues, whereas both iNOS and eNOS protein expressions were detected in carotid arteries. Either brain tissues or carotid arteries were solubilized in RIBA lysis buffer (Bio BASIC INC, Ontario, Canada) for protein extraction. Equal amounts of protein (20 μg/lane) were electrophoresed on 10% sodium dodecyl sulfate poly acrylamide (SDS-PAGE) gel. After electrophoresis, the proteins were transferred into poly vinyl difluoride (PVDF) membrane by a method of semi-dry blotting. Blocking the membrane was performed to prevent non-specific background binding with 5% skim dry milk in PBS in Tris-buffered saline at room temperature for 1 h. Membranes were incubated at 4 °C overnight with primary antibodies TNF-α (1:3000) and caspase-3 (1:500) for brain tissues or iNOS (1:2000) and eNOS (1:1000) for carotid segments. The membrane was washed then incubated with horseradish peroxidase conjugated secondary antibody (Goat anti-rabbit IgG—Novus Biologicals) for 1 h. The blots were developed with chemiluminescent method, and signals were captured using a CCD camera-based imager. Image J software (freeware; rsbweb.nih.gov/ij) was used to read the band intensity of the target proteins. The densities of the target protein bands were normalized to the corresponding density of β-actin band and presented as a ratio of the relative optical density and were calibrated as fold-change value from control.
Real-time quantitative polymerase chain reaction
Total ribonucleic acid (RNA) was extracted from carotid segments using total RNA purification system (Jena Bioscience, Germany). The quality and yield of the total RNA were determined by a UV spectrophotometry at 260 nm. First strand of complementary deoxyribonucleic acid (cDNA) was synthesized from 2 μg of total RNA by reverse transcription using capacity cDNA reverse transcription kit (Fermentas, USA) according to the manufacturer’s instructions. RT-qPCR amplification and analysis were performed by SYBER green using an Applied Biosystem with software version 3.1 (StepOne™, USA). Annealing temperature was optimized to allow qPCR assay of NOX2 mRNA abundance and normalized it to that of β-actin mRNA. The forward NOX2 primer was 5′-GGAAATAGAAAGTTGACTGGCCC-3′ and the reverse primer was 3′-GTATGAGTGCCATCCAGAGCAG-5′. The forward β-actin primer was 5′-ACTGCCGCATCCTCTTCCTC-3′ and the reverse was 3′-ACTCCTGCTTGCTGATCCACAT-5′.
Assessment of cerebral infarct volume
The brains were carefully removed, washed with chilled saline, and frozen for 1–2 h; then, each brain sliced into serial coronal sections of 2 mm thickness. After sectioning, the slices were stained with 2% TTC stain for 15 min at 37 °C then fixed by 10% formaldehyde solution. The infarct volume was calculated by summation of the infarct area in each slice multiplied by its thickness of the slice and presented as percentage of infarct volume (Heeba and El-Hanafy 2012).
Histopathological examination
Brain tissues were fixed for at least 24 h in 10% buffered formalin and then embedded in paraffin blocks. Using microtome, paraffin blocks were sectioned at 4 μm thickness, deparaffinized, and stained with hematoxylin–eosin (H&E) for histological examination by light microscope. The severity of cerebral histopathological changes in terms of nuclear pyknosis and degeneration in neurons, focal gliosis, and encephalomalacia was scored for none, mild, moderate, and sever levels by 0, +, ++, and +++ scores, respectively. During sample analysis, the investigators were blinded to sample identity, where sample coding and decoding were carried out by an independent investigator.
Statistical analysis
Data are represented as mean ± SEM. Differences in statistical significance were evaluated statistically using one-way analysis of variance (one-way ANOVA test) followed by Tukey-Kramer post analysis test for comparing groups. Statistical significance was presented at p < 0.05. Analysis was performed using GraphPad Prism® software (Version 5.0).
Results
Effect on glucose tolerance, insulin resistance, and serum levels of TG and LDL-C
The glucose intolerance which is observed in cerebral I/R-injured and sham diabetic groups was ameliorated in both lixisenatide and glimepiride pretreated groups. Although glimepiride showed a lower level of blood glucose, lixisenatide efficiently lowered postprandial elevation in glucose levels. In the same manner, insulin levels of diabetic rats showed a significant increase upon treatment of lixisenatide and glimepiride when compared with the vehicle-treated group. However, both lixisenatide and glimepiride ameliorated glucose intolerance which was observed in vehicle-treated groups.
This result went along with the observed significant decrease in insulin resistance obtained by treatment of lixisenatide and glimepiride. Both lixisenatide and glimepiride pretreatment showed a decrease of 18 and 29%, respectively, in HOMA-IR index compared with sham diabetic group.
Similar changes were observed in lipid serum levels; TG and LDL-C serum levels in sham diabetic group were 249 ± 5.34 and 200 ± 3.86, respectively. These levels were significantly decreased to 228 ± 6.39 and 180 ± 1.93 for TG and LDL-C levels, respectively, upon pretreatment of lixisenatide. Glimepride pretreatment also showed a comparable result to that of lixisenatide group (Table 1, Fig. 1).
Effect of lixisenatide and glimepiride treatment on blood glucose level of diabetic rats at zero time and at 30, 60, 90, and 120 min after glucose loading during oral glucose tolerance test. Data are represented as mean ± SEM. +,° are significant differences from I/R and lixisenatide-treated groups, respectively, at P ˂ 0.05 where n = 6–8. I/R: Ischemia/reperfusion, Lixi: Lixisenatide, glim: Glimepiride
Effect on neurobehavioral tests
Cerebral I/R-injured diabetic rats showed a significant deterioration in rats’ spontaneous activity and neurological function evident by getting low scores in both open field and Garcia tests compared to sham diabetic group. Both lixsenatide and glimepiride pretreatment protected against deterioration in neurobehavioral analysis observed in cerebral I/R-injured diabetic rats. However, lixisenatide was more efficacious than glimepiride in this regard (Fig. 2).
Effect of lixisenatide and glimepiride treatment on ambulation frequency (a) and rearing frequency (b) as a part of open field behavioral test, and on neurological deficiency (c) as a part of Garcia neurobehavioral test in diabetic rats subjected to global cerebral I/R. Data are represented as mean ± SEM. *, +,° are significant difference from sham, I/R, and lixisenatide-treated groups, respectively, at P ˂ 0.05 where n = 6–8. I/R: Ischemia/reperfusion, Lixi: Lixisenatide, glim: Glimepiride
Effect on oxidative stress markers
Cerebral I/R injury resulted in significant increase (p ˂ 0.05) in brain MDA levels compared with sham-operated group (9.64 ± 0.83 vs. 4.85 ± 0.34 nmol/g protein). Lixisenatide showed a significant protection (p ˂ 0.05) evident by attenuation of the elevated cerebral MDA levels which reached to 4.6 ± 0.47 nmol/g protein. Pretreatment with lixisenatide significantly ameliorated cerebral MDA level comparable to both sham-operated and glimepiride-treated groups (Table 2).
The antioxidant content of both GSH level and catalase activity was significantly decreased in brain tissues upon induction of cerebral I/R injury (15.2 ± 2.86 nmol/mg protein and 1.76 ± 0.39 U/mg protein) compared to sham-operated rats (26.4 ± 3.58 nmol/mg protein and 9.5 ± 0.54 U/mg protein). Lixisenatide as well as glimepiride showed a significant increase in both GSH level and catalase activity compared to cerebral I/R group. It also appeared that the ameliorations of GSH level and catalase activity were significantly higher in lixisenatide-treated group compared with glimepiride-treated group (Table 2).
Effects on the cerebral protein expressions of caspase-3 and TNF-α
The protein expression of caspase-3 and TNF-α was significantly (p < 0.05) increased in ischemic hemisphere compared to sham-operated rats. In rat groups received either lixisenatide or glimepiride pretreatment, the protein expressions of both caspase-3 and TNF-α were significantly attenuated compared to I/R group. However, lixisenatide pretreatment prevented the upregulation of cerebral caspase-3 and TNF-α protein expression more significant than glimepiride pretreatment (Fig. 3).
Representative Western blots analysis of cerebral caspase-3 (a) and TNF-α (b) protein expression showing protein bands of each group (upper panel) and graphs present their densitometric analysis (lower panel). *, +, ° are significant differences from sham, I/R, and lixisenatide-treated groups, respectively, at P ˂ 0.05. Representative Western blots and the bar graph show analysis of four separate experiments (n = 4 rats). I/R: Ischemia/reperfusion, Lixi: Lixisenatide, glim: Glimepiride
Effect on carotid iNOS and eNOS protein expressions
Compared to sham-operated group, cerebral I/R group showed a marked increase in iNOS protein expression with substantial decrease in the expression of eNOS. Lixisenatide pretreatment significantly (p < 0.05) prevented the effect of I/R on both carotid eNOS and iNOS protein expressions. Glimepiride pretreatment showed the same action of lixisenatide on carotid protein expression of iNOS. In addition, the upregulation of eNOS protein expression upon glimepiride treatment was not statistically significant compared with cerebral I/R group (Fig. 4).
Representative Western blot analysis of eNOS (a) and iNOS (b) protein expression of carotid arteries, showing protein bands of each group (upper panel) and graphs present their densitometric analysis (lower panel). *, +, ° are significant differences from sham, I/R, and lixisenatide-treated groups, respectively at P ˂ 0.05. Representative Western blots and the bar graph show analysis of four separate experiments (n = 4 rats). I/R: Ischemia/reperfusion, Lixi: Lixisenatide, glim: Glimepiride
Effects on carotid NOX2 mRNA expression
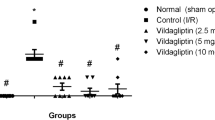
The findings in Fig. 5 indicated a significant increase in carotid NOX2 mRNA expression in cerebral I/R group compared with sham-operated one. Pretreatment of lixisenatide resulted in a marked reduction in the upregulated NOX2 mRNA level. Glimepiride showed a similar effect to lixisenatide on the NOX2 mRNA downregulation. However, pretreatment with lixisenatide exhibited more significant (p < 0.05) downregulation of carotid NOX2 mRNA compared to glimepiride pretreatment.
Representative real-time quantitative polymerase chain reaction (RT-qPCR) of carotid artery NOX2 mRNA expression of each group as normalized to quantity of β-actin mRNA. *, +, ° are significant differences from sham, I/R, and lixisenatide-treated groups, respectively, at P ˂ 0.05 where n = 6–8. I/R: Ischemia/reperfusion, Lixi: Lixisenatide, glim: Glimepiride
Effect on cerebral infarct volume
Brain tissues of diabetic I/R-injured rats showed a significant (P ˂ 0.05) enlargement in infarct volume compared with brains of sham-operated diabetic rats. Lixisenatide-pretreated rats exhibited a significant reduction in infarct volume compared with I/R diabetic rats (4.72 ± 0.46 vs. 23.79 ± 1.74%, respectively). Also, glimepiride showed a reduction of cerebral infarct volume (10.04 ± 0.27%) compared to I/R group (23.79 ± 1.74%). Nevertheless, pretreatment with glimepiride showed higher cerebral infarct volume compared to lixisenatide. Representative images of TTC staining are shown in Fig. 6.
Representative coronal diabetic brain sections showed % of brain infarction in sham group (a), I/R-injured group (b), lixisenatide-treated group (c), and glimepiride-treated group (d). Coronal brain sections (2 mm thick) stained with 2% triphenyl tetrazolium chloride. Dark colored region in the stained sections indicates non-ischemic and pale colored region indicates ischemic portion of brain. The sections were scanned and area of infarction measured using ImageJ analysis software. Quantitative changes in brain infarction are represented as % of infarct volume (E) and data are represented as mean ± SEM. *, +, ° are significant differences from sham, I/R, and lixisenatide-treated groups, respectively, at P ˂ 0.05 where n = 6–8. I/R: Ischemia/reperfusion, Lixi: Lixisenatide, glim: Glimepiride
Effect on histopathological changes in cerebral hemisphere
Histopathological examination of brain tissues from diabetic sham-operated rats showed no histopathological changes with normal neuronal cells. Microscopical examination of brain tissues of cerebral I/R group showed some histopathological alteration in form of nuclear pyknosis in neurons and focal glioss. However, pretreatment with lixisenatide provided amelioration of these abnormalities. Also, glimepiride showed a comparable effect to lixisenatide with less ameliorating effect according to the severity scores of histopathological changes (Fig. 7, Table 3).
Brain tissues of sham operated group (a) showed mild congestion in cerebral cortical blood vessels (hallow arrow head) while, I/R-injured group (b-1, b-2) showed necrosis and pyknosis of neurons (arrow head), focal gliosis (arrow), and focal encephalomalacia in the matrix of striatum (b-3). Lixisenatide-treated group (c) exhibited a marked amelioration in brain tissue with little nuclear pyknosis (arrow head). Glimepiride-treated group (d) showed some focal gliosis (arrow) and pyknosis of neuron degeneration (arrow head) in brain tissues
Discussion
T2DM is the most common epidemic metabolic disease that associated with long-term microvascular complications and a major disorder of insulin regulation (Duarte et al. 2012; Diabetes facts, 2017). Disturbed glucose metabolism and ameliorated level of insulin in brain tissues exacerbate ischemic lesions in stroke patients (Shukla et al. 2017). In this regard, we supposed that tight glycemic control may be a promising strategy for protection against stroke in diabetic rats. In this study, we evaluated the protective effect of a novel anti-T2DM drug, lixisenatide, in comparison with glimepiride (a standard sulfonylurea drug), against global cerebral I/R injury in diabetic rats.
The data of the current study conclusively showed that the pretreatment with lixisenatide had the ability to abrogate insulin resistance and glucose intolerance induced by T2DM along with amelioration of the elevated serum levels of TGs and LDL-C in diabetic rats. On the other hand, pretreatment with glimepiride provided a stronger effect on dampening HOMA-IR index, glucose intolerance, and lipid profile compared to lixisenatide. According to our results, we supposed that pretreatment of glimepiride provided a better glycemic control than lixisentide therapy. Our finding was in contrast to many other clinical studies which supposed that GLP-1R agonists provided sustained improvement in glycemic control than glimepiride in diabetic patients (Garber et al. 2011; Handelsman et al. 2017). However, our results were consistent with Darsalia et al. (2013) who reported that HFD-fed rats showed lower plasma glucose level along with glimepiride treatment than treatment with lingaliptin, a dipeptidyl peptidase-4 inhibitor (Darsalia et al. 2013).
On the other hand, cerebral I/R-injured rats pretreated with lixisenatide showed a significant reduction in cerebral infarct volume and a marked improvement in pathological changes of brain tissues compared to glimepiride protective therapy. In the same way, lixisenatide protective treatment provided higher neurobehavioral amelioration in both Garcia and open field tests in diabetic rats subjected to cerebral I/R injury compared to their counterparts pretreated by glimepiride. These observations suppose that the neuroprotective effect of lixisenatide against global cerebral I/R injury could be beyond its glycemic action. Nevertheless, lixsenatide’s impact on glycaemia may be also considered as a part of its neuroprotective effect.
In diabetic subjects, chronic hyperglycemia leads to excessive production of reactive oxygen spices (ROS) and consequent imbalance in oxidative status in brain tissues (Moreira et al. 2005; Nazaroglu et al. 2009). ROS-induced hyperglycemia can stimulate the production of TNF-α which mediates diabetic neuropathy and enhances cerebral insulin resistance (Celik and Erdogan 2008). Equally important, oxidative stress also could be linked to T2DM-mediated cerebral apoptosis via upregulation of apoptotic markers including caspase-3 (Vincent et al. 2005).
The present study showed that cerebral I/R-induced injury in diabetic rat specifically exacerbated oxidative stress, inflammation, and apoptosis. In line with various reported studies (Mohamed et al. 2014; Zeng et al. 2016), we reported a marked oxidative imbalance in brain tissue of cerebral I/R-injured diabetic rats evident by increased level of MDA with suppressed GSH level and catalase anti-oxidant activity. Additionally, enhanced expressions of cerebral TNF-α and caspase-3 support the concept of inflammatory and apoptotic responses which were observed in diabetic rats with cerebral I/R injury. Glycemic control through pre-treatment of lixisenatide and glimepiride provided protection against oxidative stress, inflammation, and apoptosis in the brain tissues of I/R-injured diabetic rats compared with vehicle-treated counterparts. It is worth noting that, upon comparison of lixisenatide and glimepiride protective therapy, our results showed that lixisenatide was more efficacious than glimepiride against oxidative stress, inflammation, and apoptosis observed in brain tissues of diabetic rats subjected to I/R-induced injury. One possible explanation is that lixisenatide may mediate its neuroprotective effect in diabetic rats through another mechanism besides controlling hyperglycemia.
Lixisenatide is a GLP-1 analog that acts mainly via GLP-1R. GLP-1 is a growth factor in the brain that plays a crucial rule in brain tissue protection and neuronal activity regulation (Holscher 2014). Uniquely, GLP-1 analogs were reported to decrease cerebral pro-inflammatory cytokines and increase the expression of anti-apoptotic genes in ischemic brains besides its ability to protect against oxidative injury in cerebral I/R rat models (Briyal et al. 2014; Teramoto et al. 2011). Hence, we suggest that stimulation of cerebral GLP-1R through lixisenatide provides superior action in terms of protection against cerebral I/R injury aside from its antidiabetic effect.
CBF is tightly regulated by a well-functioning vasculature to optimize supply of the necessary nutrients to brain tissues. Carotid arteries are responsible for delivery of more than 70% of total CBF (Zarrinkoob et al. 2015). Abnormal carotid vasculature and irregular cerebrovascular autoregulation are associated with increased risk of stroke and such abnormality has been identified in diabetic patients (Selvarajah et al. 2016). However, reduced CBF contributes to the progression of neurodegenerative disorders as well as, complicates I/R-induced injury in diabetic subjects (Li et al. 2010; Ohara et al. 2011).
Numerous mechanisms were proposed to explain vascular injury associated with diabetes (Vallurupalli 2017). T2DM is associated with endothelial dysfunction evident by suppression of vascular eNOS activity and upregulation of iNOS and NADPH oxidase expression which subsequently leads to production of cytotoxic peroxynitrite (ONOO−) and aggravates vascular injury (Adel et al. 2014; Li et al. 2007). Endothelial dysfunction and vascular impairment may be exaggerated by interruption of blood flow after occlusion of carotid arteries in model of global cerebral ischemia which has a negative impact on stroke severity and recovery (Coucha et al. 2013). In the current study, we observed that carotid arteries of diabetic rats, subjected to cerebral I/R injury, showed a significant reduction in eNOS protein expression along with increase in protein expression of iNOS and mRNA levels of NOX2 (gp91phox; a critical catalytic component of endothelial NADPH oxidase).
On the other hand, our results revealed that protective treatment by lixisenatide has a strong impact on vascular repair. To illustrate, lixisenatide pretreatment significantly reversed the protein expression in eNOS and suppressed the elevated levels of iNOS protein expression and NOX2 mRNA in carotid arteries of cerebral I/R-injured diabetic rats. Regarding glimepiride pretreatment, no significant improvement was observed in carotids’ eNOS protein expression, but iNOS/NOX2 levels were lowered compared to diabetic rats with cerebral I/R-induced injury. Comparatively, the levels of vascular nitrosative and oxidative mediators (iNOS and NOX2, respectively) were significantly downregulated in cerebral I/R-injured rats by lixisenatide better than glimepiride pretreatment.
Hyperglycemia associated with upregulation of the cytotoxic ONOO− through increasing the levels of both superoxide (O2−) and NO. ONOO− mediates vascular injury through enhanced levels of NADPH oxidase (a vital source of O2− in vessels) and iNOS (a massive NO producer) leading to eNOS uncoupling and decreased NO bioavailability and, as a consequence, endothelial dysfunction (El-Remessy et al. 2010). ONOO− is also generated during cerebral I/R-induced injury (Gursoy-Ozdemir et al. 2004). The data of the present study indicated that both lixisenatide and glimepiride dampened vascular oxidative stress parameters (iNOS, NOX2), in part, through their glycemic control. However, the vascular effect of lixisenatide is superior to that of glimepiride which may be due to its agonist effect on GLP-1R.
Many studies supported the beneficial effects of GLP-1R agonists on vascular dysfunction through different mechanisms which are GLP-1R-dependent. Steven et al. (2015) reported that GLP-1 analog treatment improved vascular inflammation/dysfunction in rats with lipopolysaccharide (LPS)-induced endotoxemia. Accordingly, they observed reduced mRNA levels of iNOS, NADPH oxidase subunit (NOX-2), and TNF-α in aortic tissue of endotoxemic rats (Steven et al. 2015). GLP-1 analogs also improve vascular dysfunction via GLP-1R signaling with downstream phosphorylation of eNOS thus resulting in activation and potentiation of eNOS activity (Hattori et al. 2010). Additionally, GLP-1R agonistic effect suppresses ROS formation and inflammation which mediate endothelial vascular injury (Liu et al. 2014; Selley et al. 2014). Consistently with these findings, our results revealed that lixisenatide protective treatment showed enhanced levels of carotid eNOS protein expression along with significant suppression of iNOS protein expression and NOX2 mRNA levels which ultimately counteracted the endothelial dysfunction observed in diabetic cerebral I/R-injured rats.
Similarly, glimepiride pretreatment showed a slight upregulation in eNOS protein expression of carotid arteries in cerebral I/R-injured rats compared to vehicle-treated ones. However, this elevation is statistically non-significant. Moreover, the upregulation of carotid eNOS protein expression was less significant in glimepiride pretreated group than of lixisenatide protective treatment. Nonetheless, we supposed that glimepiride has some protective effect via suppression of vascular oxidative/nitosative burst evident by dampening NOX2 mRNA levels and iNOS protein expression that may took place in preserving the bioavailability of endothothelial NO. On the contrary, a clinical study of Machado et al. (2012) reported that glimepiride therapy did not affect carotid artery vasodilation in diabetic patients (Machado et al. 2012).
Conclusively, the present study showed that lixisenatide, a GLP-1R agonist, produced protection against cerebral I/R-induced injury in diabetic rats beyond its glycemic control and superior to the standard anti-diabetic sulfonylurea drug, glimepiride. The observed neuroprotective effect of lixisenatide may be mediated through GLP-1R and via mitigation of cerebral oxidative stress, inflammation, and apoptosis.
Abbreviations
- T2DM:
-
Type 2 diabetes mellitus
- eNOS:
-
Endothelial nitric oxide synthase
- GLP-1:
-
Glucagon-like peptide-1
- GLP-1R:
-
Glucagon-like peptide-1 receptor
- I/R:
-
Ischemia-reperfusion
- iNOS:
-
Inducible nitric oxide synthase
- TNF-α:
-
Tumor necrosis factor-alpha
- VEGF:
-
Vascular endothelial growth factor
References
Abdelkader NF, Saad MA, Abdelsalam RM (2017) Neuroprotective effect of nebivolol against cisplatin-associated depressive-like behavior in rats. J Neurochem 141:449–460. https://doi.org/10.1111/jnc.13978
Adel H, Taye A, Khalifa MM (2014) Spironolactone improves endothelial dysfunction in streptozotocin-induced diabetic rats. Naunyn Schmiedeberg's Arch Pharmacol 387:1187–1197. https://doi.org/10.1007/s00210-014-1048-3
Briyal S, Shah S, Gulati A (2014) Neuroprotective and anti-apoptotic effects of liraglutide in the rat brain following focal cerebral ischemia. Neuroscience 281:269–281. https://doi.org/10.1016/j.neuroscience.2014.09.064
Celik S, Erdogan S (2008) Caffeic acid phenethyl ester (CAPE) protects brain against oxidative stress and inflammation induced by diabetes in rats. Mol Cell Biochem 312:39–46. https://doi.org/10.1007/s11010-008-9719-3
Coucha M, Li W, Johnson MH, Fagan SC, Ergul A (2013) Protein nitration impairs the myogenic tone of rat middle cerebral arteries in both ischemic and nonischemic hemispheres after ischemic stroke. Am J Phys Heart Circ Phys 305:H1726–H1735. https://doi.org/10.1152/ajpheart.00535.2013
Darsalia V, Ortsater H, Olverling A, Darlof E, Wolbert P, Nystrom T, Klein T, Sjoholm A, Patrone C (2013) The DPP-4 inhibitor linagliptin counteracts stroke in the normal and diabetic mouse brain: a comparison with glimepiride. Diabetes 62:1289–1296. https://doi.org/10.2337/db12-0988
Diabetes facts (2017) http://www.who.int/mediacentre/factsheets/fs312/en/. Accessed 18 November 2017
Duarte AI, Moreira PI, Oliveira CR (2012) Insulin in central nervous system: more than just a peripheral hormone. J Aging Res 2012:384017–384021. https://doi.org/10.1155/2012/384017
Duarte AI, Candeias E, Correia SC, Santos RX, Carvalho C, Cardoso S, Plácido A, Santos MS, Oliveira CR, Moreira PI (2013) Crosstalk between diabetes and brain: glucagon-like peptide-1 mimetics as a promising therapy against neurodegeneration. Biochim Biophys Acta 1832:527–541. https://doi.org/10.1016/j.bbadis.2013.01.008
El-Remessy AB, Tawfik HE, Matragoon S, Pillai B, Caldwell RB, Caldwell RW (2010) Peroxynitrite mediates diabetes-induced endothelial dysfunction: possible role of rho kinase activation. Exp Diabetes Res 2010:247861. https://doi.org/10.1155/2010/247861
Garber A, Henry RR, Ratner R, Hale P, Chang CT, Bode B, Group L-S (2011) Liraglutide, a once-daily human glucagon-like peptide 1 analogue, provides sustained improvements in glycaemic control and weight for 2 years as monotherapy compared with glimepiride in patients with type 2 diabetes. Diabetes Obes Metab 13:348–356. https://doi.org/10.1111/j.1463-1326.2010.01356.x
Garcia JH, Wagner S, Liu KF, Hu XJ (1995) Neurological deficit and extent of neuronal necrosis attributable to middle cerebral artery occlusion in rats. Statistical validation. Stroke 26:627–634; discussion 635
Gejl M, Egefjord L, Lerche S, Vang K, Bibby BM, Holst JJ, Mengel A, Møller N, Rungby J, Brock B, Gjedde A (2012) Glucagon-like peptide-1 decreases intracerebral glucose content by activating hexokinase and changing glucose clearance during hyperglycemia. J Cereb Blood Flow Metab 32:2146–2152. https://doi.org/10.1038/jcbfm.2012.118
Gonzalez-Moreno EI, Camara-Lemarroy CR, Gonzalez-Gonzalez JG, Gongora-Rivera F (2014) Glycemic variability and acute ischemic stroke: the missing link? Transl Stroke Res 5:638–646. https://doi.org/10.1007/s12975-014-0365-7
Gursoy-Ozdemir Y, Can A, Dalkara T (2004) Reperfusion-induced oxidative/nitrative injury to neurovascular unit after focal cerebral ischemia. Stroke 35:1449–1453. https://doi.org/10.1161/01.STR.0000126044.83777.f4
Handelsman Y, Lauring B, Gantz I, Iredale C, O’Neill EA, Wei Z, Suryawanshi S, Kaufman KD, Engel SS, Lai E (2017) A randomized, double-blind, non-inferiority trial evaluating the efficacy and safety of omarigliptin, a once-weekly DPP-4 inhibitor, or glimepiride in patients with type 2 diabetes inadequately controlled on metformin monotherapy. Curr Med Res Opin 33:1861–1868. https://doi.org/10.1080/03007995.2017.1335638
Hattori Y, Jojima T, Tomizawa A, Satoh H, Hattori S, Kasai K, Hayashi T (2010) A glucagon-like peptide-1 (GLP-1) analogue, liraglutide, upregulates nitric oxide production and exerts anti-inflammatory action in endothelial cells. Diabetologia 53:2256–2263. https://doi.org/10.1007/s00125-010-1831-8
Heeba GH, El-Hanafy AA (2012) Nebivolol regulates eNOS and iNOS expressions and alleviates oxidative stress in cerebral ischemia/reperfusion injury in rats. Life Sci 90:388–395. https://doi.org/10.1016/j.lfs.2011.12.001
Holscher C (2014) Central effects of GLP-1: new opportunities for treatments of neurodegenerative diseases. J Endocrinol 221:T31–T41. https://doi.org/10.1530/JOE-13-022
Horowitz M, Rayner CK, Jones KL (2013) Mechanisms and clinical efficacy of lixisenatide for the management of type 2 diabetes. Adv Ther 30:81–101. https://doi.org/10.1007/s12325-013-0009-4
Kramer W, Muller G, Geisen K (1996) Characterization of the molecular mode of action of the sulfonylurea, glimepiride, at beta-cells. Horm Metab Res = Hormon- und Stoffwechselforschung = Hormones et metabolisme 28:464–468. https://doi.org/10.1055/s-2007-979838
Langtry HD, Balfour JA (1998) Glimepiride. A review of its use in the management of type 2 diabetes mellitus. Drugs 55:563–584
Li R, Wang WQ, Zhang H, Yang X, Fan Q, Christopher TA, Lopez BL, Tao L, Goldstein BJ, Gao F, Ma XL (2007) Adiponectin improves endothelial function in hyperlipidemic rats by reducing oxidative/nitrative stress and differential regulation of eNOS/iNOS activity. Am J Phys Endocrinol Metab 293:E1703–E1708. https://doi.org/10.1152/ajpendo.00462.2007
Li W, Prakash R, Kelly-Cobbs AI, Ogbi S, Kozak A, el-Remessy AB, Schreihofer DA, Fagan SC, Ergul A (2010) Adaptive cerebral neovascularization in a model of type 2 diabetes: relevance to focal cerebral ischemia. Diabetes 59:228–235. https://doi.org/10.2337/db09-0902
Liu L, Liu J, Tian XY, Wong WT, Lau CW, Xu A, Xu G, Ng CF, Yao X, Gao Y, Huang Y (2014) Uncoupling protein-2 mediates DPP-4 inhibitor-induced restoration of endothelial function in hypertension through reducing oxidative stress. Antioxid Redox Signal 21:1571–1581. https://doi.org/10.1089/ars.2013.5519
Lovshin JA (2017) Glucagon-like Peptide-1 receptor agonists: a class update for treating type 2 diabetes. Can J Diabetes 41:524–535. https://doi.org/10.1016/j.jcjd.2017.08.242
Luitse MJ, Biessels GJ, Rutten GE, Kappelle LJ (2012) Diabetes, hyperglycaemia, and acute ischaemic stroke. Lancet Neurol 11:261–271. https://doi.org/10.1016/S1474-4422(12)70005-4
Machado HA, Vieira M, Cunha MR, Correia MRS, Fukui RT, Santos RF, Rocha DM, Wajchenberg BL, Lage SG, Silva MER (2012) Metformin, but not glimepiride, improves carotid artery diameter and blood flow in patients with type 2 diabetes mellitus. Clinics 67:711–717
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
McClean PL, Holscher C (2014) Lixisenatide, a drug developed to treat type 2 diabetes, shows neuroprotective effects in a mouse model of Alzheimer's disease. Neuropharmacology 86:241–258. https://doi.org/10.1016/j.neuropharm.2014.07.015
Mohamed HE, El-Swefy SE, Hasan RA, Hasan AA (2014) Neuroprotective effect of resveratrol in diabetic cerebral ischemic-reperfused rats through regulation of inflammatory and apoptotic events. Diabetol Metab Syndr 6:88. https://doi.org/10.1186/1758-5996-6-88
Moreira PI, Santos MS, Sena C, Seica R, Oliveira CR (2005) Insulin protects against amyloid beta-peptide toxicity in brain mitochondria of diabetic rats. Neurobiol Dis 18:628–637. https://doi.org/10.1016/j.nbd.2004.10.017
Nade VS, Kawale LA, Patel KM (2015) Protective effect of sitagliptin and rosuvastatin combination on vascular endothelial dysfunction in type-2 diabetes. Indian J Pharm Sci 77:96–102
Nazaroglu NK, Sepici-Dincel A, Altan N (2009) The effects of sulfonylurea glyburide on superoxide dismutase, catalase, and glutathione peroxidase activities in the brain tissue of streptozotocin-induced diabetic rat. J Diabetes Complicat 23:209–213. https://doi.org/10.1016/j.jdiacomp.2007.09.001
Ohara T, Doi Y, Ninomiya T, Hirakawa Y, Hata J, Iwaki T, Kanba S, Kiyohara Y (2011) Glucose tolerance status and risk of dementia in the community: the Hisayama study. Neurology 77:1126–1134. https://doi.org/10.1212/WNL.0b013e31822f0435
Palomares SM, Gardner-Morse I, Sweet JG, Cipolla MJ (2012) Peroxynitrite decomposition with FeTMPyP improves plasma-induced vascular dysfunction and infarction during mild but not severe hyperglycemic stroke. J Cereb Blood Flow Metab 32:1035–1045. https://doi.org/10.1038/jcbfm.2012.14
Piironen K, Putaala J, Rosso C, Samson Y (2012) Glucose and acute stroke: evidence for an interlude. Stroke 43:898–902. https://doi.org/10.1161/STROKEAHA.111.631218
Sander D, Kearney MT (2009) Reducing the risk of stroke in type 2 diabetes: pathophysiological and therapeutic perspectives. J Neurol 256:1603–1619. https://doi.org/10.1007/s00415-009-5143-1
Sanofi New Drug Application for Lixisenatide Accepted for Review by FDA (19 February 2013)
Seif-el-Nasr M, Fahim AT (2001) Antioxidant effect of N omega-nitro-L-arginine methyl ester (L-NAME) on global cerebral ischemia in a rat model. Arzneimittelforschung 51:628–632. https://doi.org/10.1055/s-0031-1300092
Selley E et al (2014) Exenatide induces aortic vasodilation increasing hydrogen sulphide, carbon monoxide and nitric oxide production. Cardiovasc Diabetol 13:69. https://doi.org/10.1186/1475-2840-13-69
Selvarajah D, Hughes T, Reeves J, Boland E, Marques J, Gandhi R, Griffiths PD, Tesfaye S, Wilkinson ID (2016) A preliminary study of brain macrovascular reactivity in impaired glucose tolerance and type-2 diabetes: quantitative internal carotid artery blood flow using magnetic resonance phase contrast angiography. Diab Vasc Dis Res 13:367–372. https://doi.org/10.1177/1479164116644404
Shukla V, Shakya AK, Perez-Pinzon MA, Dave KR (2017) Cerebral ischemic damage in diabetes: an inflammatory perspective. J Neuroinflammation 14:21. https://doi.org/10.1186/s12974-016-0774-5
Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Nguyen-Huynh MN, Kushi LH, Go AS, Rana JS (2016) Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol 1:594–599. https://doi.org/10.1001/jamacardio.2016.1326
Srinivasan K, Viswanad B, Asrat L, Kaul CL, Ramarao P (2005) Combination of high-fat diet-fed and low-dose streptozotocin-treated rat: a model for type 2 diabetes and pharmacological screening. Pharmacol Res 52:313–320. https://doi.org/10.1016/j.phrs.2005.05.004
Steven S, Hausding M, Kröller-Schön S, Mader M, Mikhed Y, Stamm P, Zinßius E, Pfeffer A, Welschof P, Agdauletova S, Sudowe S, Li H, Oelze M, Schulz E, Klein T, Münzel T, Daiber A (2015) Gliptin and GLP-1 analog treatment improves survival and vascular inflammation/dysfunction in animals with lipopolysaccharide-induced endotoxemia. Basic Res Cardiol 110:6. https://doi.org/10.1007/s00395-015-0465-x
Teramoto S, Miyamoto N, Yatomi K, Tanaka Y, Oishi H, Arai H, Hattori N, Urabe T (2011) Exendin-4, a glucagon-like peptide-1 receptor agonist, provides neuroprotection in mice transient focal cerebral ischemia. J Cereb Blood Flow Metab 31:1696–1705. https://doi.org/10.1038/jcbfm.2011.51
Vallurupalli SMJL (2017) Vascular remodeling in diabetes mellitus. In: RS KC, Pillai R (eds) Advances in biochemistry in health and disease. https://doi.org/10.1007/978-3-319-60324-7_3
Van den Berghe G, Schoonheydt K, Becx P, Bruyninckx F, Wouters PJ (2005) Insulin therapy protects the central and peripheral nervous system of intensive care patients. Neurology 64:1348–1353. https://doi.org/10.1212/01.WNL.0000158442.08857.FC
Vincent AM, McLean LL, Backus C, Feldman EL (2005) Short-term hyperglycemia produces oxidative damage and apoptosis in neurons. FASEB J 19:638–640. https://doi.org/10.1096/fj.04-2513fje
Werner U, Haschke G, Herling AW, Kramer W (2010) Pharmacological profile of lixisenatide: a new GLP-1 receptor agonist for the treatment of type 2 diabetes. Regul Pept 164:58–64. https://doi.org/10.1016/j.regpep.2010.05.008
Yuh WT, Alexander MD, Ueda T, Maeda M, Taoka T, Yamada K, Beauchamp NJ (2017) Revisiting current golden rules in managing acute ischemic stroke: evaluation of new strategies to further improve treatment selection and outcome. AJR Am J Roentgenol 208:32–41. https://doi.org/10.2214/AJR.16.16557
Zarrinkoob L, Ambarki K, Wahlin A, Birgander R, Eklund A, Malm J (2015) Blood flow distribution in cerebral arteries. J Cereb Blood Flow Metab 35:648–654. https://doi.org/10.1038/jcbfm.2014.241
Zeng X, Wang H, Xing X, Wang Q, Li W (2016) Dexmedetomidine protects against transient global cerebral ischemia/reperfusion induced oxidative stress and inflammation in diabetic rats. PLoS One 11:e0151620. https://doi.org/10.1371/journal.pone.0151620
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
A mortality of 0–2 rats was observed in each group. All animals’ procedures were performed in accordance Animal Care Community, Minia University, Egypt (Permit Number: MPH-12-015).
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Abdel-latif, R.G., Heeba, G.H., Taye, A. et al. Lixisenatide, a novel GLP-1 analog, protects against cerebral ischemia/reperfusion injury in diabetic rats. Naunyn-Schmiedeberg's Arch Pharmacol 391, 705–717 (2018). https://doi.org/10.1007/s00210-018-1497-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1497-1